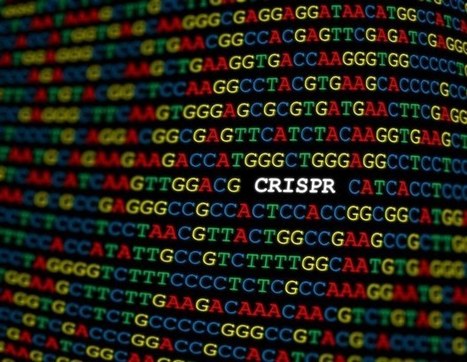
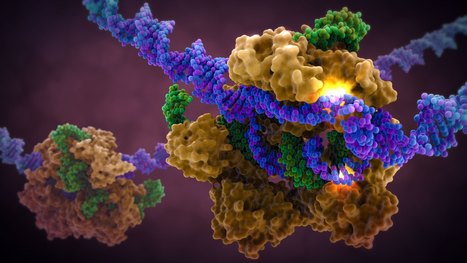
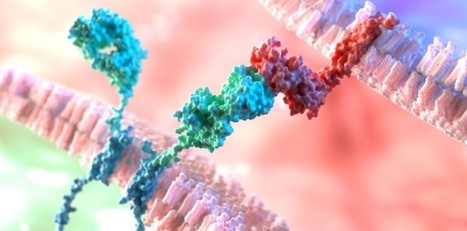
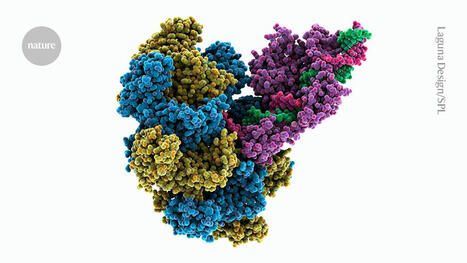
A landmark study published in Cell has shown that prime editing, a cutting-edge form of gene editing, can correct mutations causing Alternating Hemiplegia of Childhood (AHC) with a single in-brain injection. The research team fixed the most prevalent ATP1A3 gene mutations in mouse models, reducing symptoms and more than doubling survival, a first-of-its-kind success in treating a neurological disease directly in the brain. CRISPR-based gene editing was delivered through an harmless adeno-associated virus called AAV9. In parallel, patient-derived cells (iPSCs) responded similarly, reinforcing the method’s promise for human translation. Importantly, this success opens the door to targeting other genetic brain disorders previously deemed untreatable. Although results are preliminary, this study provides robust proof‑of‑concept for personalized gene editing in the brain and opens doors toward potential treatments for other intractable genetic neurological disorders.





 Your new post is loading...
Your new post is loading...



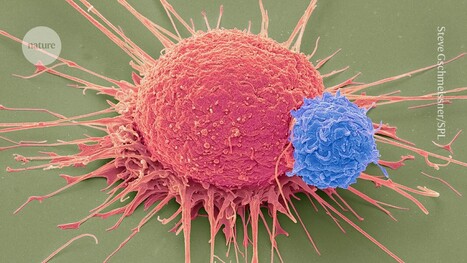







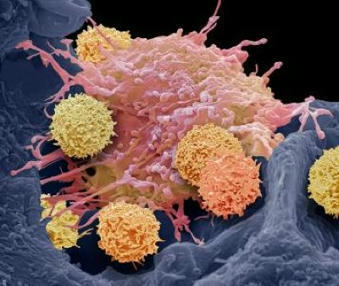


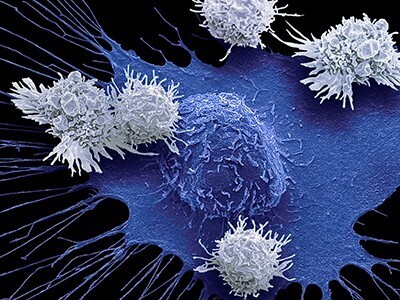






A study published in Blood Advances reveals that magnetic resonance imaging (MRI) and lumbar puncture (LP) may not be systematically necessary in the diagnosis and management of severe cases of neurotoxicity linked to CAR T cell therapy. Instead, electroencephalogram (EEG), a non-invasive test, has proved useful in the management of these complications. The researchers examined the usefulness of these tests in 190 patients treated with CAR-T at Rennes University Hospital, where during treatment around 48% of patients developed immune effector cell-associated neurotoxicity syndrome (ICANS). The researchers assessed how the different tests affected patient treatment, such as how medications, e.g. antibiotics and anti-epileptic treatments, were prescribed based on abnormal results, and how these treatments altered patient outcomes. The results ultimately revealed that abnormal findings were more common in patients with more severe ICANS. MRI findings were often normal, and although LP and EEG often showed abnormalities, they were more common in more severe cases of ICANS. When it came to therapeutic decisions, MRI rarely led to changes, LP sometimes led to unnecessary treatments in cases of suspected infections, and EEG often resulted in adjustments to antiepileptic drugs.