Testing in mice suggests that rejuvenating T cells could make vaccines and some cancer therapies more effective.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

 Your new post is loading... Your new post is loading...
 Your new post is loading... Your new post is loading...
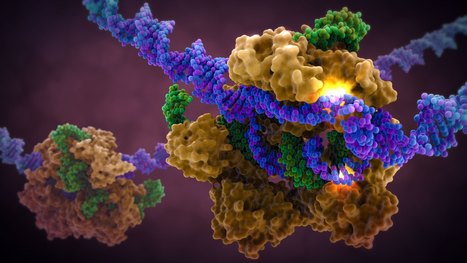
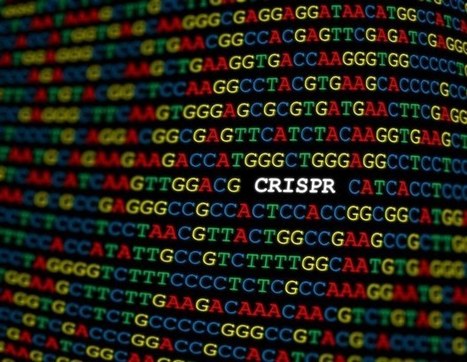
A new generation of CRISPR technology developed at UNSW Sydney offers a safer path to treating genetic diseases like Sickle Cell, while also proving beyond doubt that chemical tags on DNA - often thought to be little more than genetic cobwebs - actively silence genes.
BigField GEG Tech's insight:
For decades, scientists have debated whether methyl groups are simply debris that accumulates in the genome where genes are turned off, or the actual cause of gene repression. Now, researchers have shown in a recent paper published in Nature Communications that removing these tags can reactivate genes, confirming that methylation is not only correlated with silencing, but directly responsible for it. A third generation of CRISPR, called epigenetic editing, examines the surface of genes present in the nucleus of every cell in the body. Rather than cutting strands of DNA to remove or modify defective genes, this method removes the methyl groups attached to inhibited or suppressed genes. This new generation of CRISPR technology offers a safer way to treat genetic diseases such as sickle cell anemia.
Preliminary results from a small trial offer the clearest evidence yet that the brain disease’s progression can be slowed.
BigField GEG Tech's insight:
Preliminary results from a small trial offer the clearest evidence yet that the brain disease’s progression can be slowed.
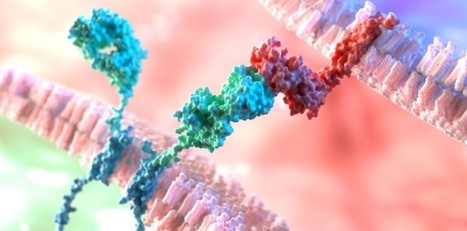
A landmark study published in Cell has shown that prime editing, a cutting-edge form of gene editing, can correct mutations causing Alternating Hemiplegia of Childhood (AHC) with a single in-brain injection. The research team fixed the most prevalent ATP1A3 gene mutations in mouse models, reducing symptoms and more than doubling survival, a first-of-its-kind success in treating a neurological disease directly in the brain. CRISPR-based gene editing was delivered through an harmless adeno-associated virus called AAV9. In parallel, patient-derived cells (iPSCs) responded similarly, reinforcing the method’s promise for human translation. Importantly, this success opens the door to targeting other genetic brain disorders previously deemed untreatable. Although results are preliminary, this study provides robust proof‑of‑concept for personalized gene editing in the brain and opens doors toward potential treatments for other intractable genetic neurological disorders.
BigField GEG Tech's insight:
A landmark study published in Cell has shown that prime editing, a cutting-edge form of gene editing, can correct mutations causing Alternating Hemiplegia of Childhood (AHC) with a single in-brain injection. The research team fixed the most prevalent ATP1A3 gene mutations in mouse models, reducing symptoms and more than doubling survival, a first-of-its-kind success in treating a neurological disease directly in the brain. CRISPR-based gene editing was delivered through an harmless adeno-associated virus called AAV9. In parallel, patient-derived cells (iPSCs) responded similarly, reinforcing the method’s promise for human translation. Importantly, this success opens the door to targeting other genetic brain disorders previously deemed untreatable. Although results are preliminary, this study provides robust proof‑of‑concept for personalized gene editing in the brain and opens doors toward potential treatments for other intractable genetic neurological disorders.
The promise of genome editing to help understand human diseases and create new therapies is vast, but technological limitations have limited advancement of the field.
BigField GEG Tech's insight:
Conventional gene-editing technologies, such as CRISPR Cas9, have been limited by the generation of DNA double-strand breaks, which introduce unwanted modifications into the genome. While the development of base editors has enabled the direct chemical modification of target DNA nucleotides, allowing researchers to avoid double-strand breaks, base editing technology has been limited by the number and precision of individual base modifications achievable. However, in a new study, the research team used a CRISPR-associated protein, Cas12, and guide RNAs (gRNAs). Fused with an enzyme, Cas12 can perform targeted chemical modifications on DNA at locations determined by the gRNA sequence. The team chose Cas12 for its innate ability to process an RNA template containing numerous gRNAs. To improve editing precision, the team modified the gRNAs by shortening the gRNA sequence or modifying the RNA bases. They then used the new system to successfully edit gene sequences with greater precision at 15 different sites in human cells, three times as many locations as previously designed. This improvement will not only enable the roots of complex genetic diseases, such as cancer, to be assessed, but will also guide the development of new synthetic drugs.
Cancer therapies called checkpoint inhibitor drugs, which ratchet up the immune system, work better when this bacterium is around.
BigField GEG Tech's insight:
Cancer therapies called checkpoint inhibitor drugs, which ratchet up the immune system, work better when this bacterium is around.
Experimental treatment could offer a safer, cheaper alternative to CAR-T-cell therapies for disorders such as lupus.
BigField GEG Tech's insight:
Experimental treatment could offer a safer, cheaper alternative to CAR-T-cell therapies for disorders such as lupus.
After treatment with CAR-T cells - immune cells engineered to attack cancer - patients sometimes tell their doctors they feel like they have "brain fog," or forgetfulness and difficulty concentrating.
BigField GEG Tech's insight:
A recent study published in Cell by Stanford Medicine researchers reveals that CAR-T cell therapy, while transformative for cancer treatment, may lead to mild cognitive impairments, commonly referred to as "brain fog." This condition encompasses symptoms like forgetfulness and difficulty concentrating and appears to occur independently of other treatments such as chemotherapy. The study, conducted primarily in mice, identified mechanisms similar to those observed in cognitive impairments following chemotherapy and infections like COVID-19. Once activated by the immune response, brain’s immune cells, called microglia, release inflammatory molecules that damage oligodendrocytes (responsible for myelin production), thereby impairing neural signal transmission. Importantly, the researchers discovered potential strategies to reverse these effects using compounds akin to existing medications, suggesting that treatments could be developed relatively quickly. These findings underscore the importance of monitoring cognitive health in patients undergoing CAR-T therapy and developing interventions to mitigate such side effects and enhance quality of life.
Investigators from Mass General Brigham and Beth Israel Deaconess Medical Center have developed STITCHR, a new gene editing tool that can insert therapeutic genes into specific locations without causing unwanted mutations.
BigField GEG Tech's insight:
American researchers have unveiled STITCHR in Nature, a novel gene-editing tool that enables the precise insertion of entire therapeutic genes into specific genomic locations without introducing unwanted mutations. Unlike traditional CRISPR systems, which typically correct single mutations and often face targeting limitations, STITCHR offers a "one-and-done" solution by inserting full genes. It may be a game-changing approach for treating diseases caused by a wide range of mutations, such as cystic fibrosis. STITCHR, short for Specific Target-Primed Insertion Through Targeted CRISPR Homing of Retroelements, harnesses enzymes derived from retrotransposons, genetic elements also known as "jumping genes", to guide gene integration with high specificity. Notably, the system can be delivered entirely in RNA form, simplifying logistics compared to approaches that require both RNA and DNA components. This advancement marks a major step forward in gene therapy, offering a promising strategy to treat diverse genetic disorders by replacing faulty genes in their entirety.
BigField GEG Tech's insight:
Manufacturing CAR T cells in the laboratory is expensive and time-consuming. An in vivo approach could get the powerful therapy to more people.
Imagine a super-charged immune cell that can launch a focused attack on stubborn solid tumors - a smart fighter that destroys cancer cells for days without tiring.
BigField GEG Tech's insight:
Researchers have introduced a next-generation CAR T-cell therapy, called EchoBack CAR T-cells, in a study published in Cell. Designed to address key limitations of current immunotherapies for solid tumors, including off-tumor toxicity, T-cell exhaustion, and limited persistence, this platform uses sonogenetic engineering to remotely activate CAR T-cells via focused ultrasound (FUS). It employs an ultrasensitive heat-shock promoter, selected from a screened library and integrated with a positive feedback loop from CAR signaling. This setup enables sustained CAR expression after ultrasound stimulation, maintaining antitumor activity for up to five days, versus less than 24 hours for standard CAR T-cells. In preclinical models, EchoBack CAR T-cells eliminated glioblastoma (GBM) cells in 3D cultures and mice, outperforming conventional CAR T-cells. Single-cell RNA sequencing showed enhanced cytotoxicity and reduced exhaustion. The system was also adapted to target prostate-specific membrane antigen (PSMA), showing prolonged tumor control in prostate cancer models. EchoBack CAR T-cells represent a versatile, precise, and safer therapeutic approach, a major advance for treating hard-to-target solid tumors.
‘Directed’ evolution in the laboratory creates an editing tool that outperforms classic CRISPR systems.
BigField GEG Tech's insight:
An innovative genome-editing tool promises to do what original CRISPR systems have struggled to achieve: insert entire genes, precisely and efficiently, into human DNA.‘ Described recently in Science, the method could pave the way for gene-correction therapies that would be given once, and work regardless of the specific mutation causing an individual’s disease. It could also accelerate the development of engineered cell therapies for cancer and simplify the creation of genetic models for research. “It could really be a big part of the future,” says study co-author David Liu, a chemical biologist at the Broad Institute in Cambridge, Massachusetts
From
www
diagnosis of severe carbamoyl-phosphate synthetase 1 deficiency
BigField GEG Tech's insight:
World’s First Patient Treated with Personalized base editing system !
This proof of principle paves the way for precision gene therapy administered directly in vivo. In addition to having a significant therapeutic effect, this trial will allow the collection of critical data for designing tomorrow's precision gene therapies, both in terms of efficacy and biosafety. We know that the liver, a target organ in this pathology, is a prime target for in vivo gene therapy because after systemic injection, vectors accumulate there without a specific targeting system and liver cells multiply rapidly, allowing rapid colonization of cured cells. Consequently, these results support the idea that the field of vectorology is key to harnessing the power of new genome editors such as base editing systems, prime editing systems. The design of vectors that can target the desired cell populations, without compromising efficacy and biosafety, is the next critical step to enable precision gene therapy for a large number of genetic pathologies. |
Chimeric antigen receptor (CAR) T cell therapy, which uses a patient's own immune cells to fight cancer, has emerged as a powerful way to treat lymphoma and other blood cancers.
BigField GEG Tech's insight:
CAR-T cell therapy has proven to be an effective treatment for lymphoma and other blood cancers. However, researchers are struggling to adapt this treatment to solid tumors, including prostate, breast, lung, and ovarian cancers, which account for about 90% of cancer cases. A research team has discovered a promising solution. The researchers genetically modified CAR-T cells to produce a fusion of two proteins: interleukin 12 (IL-12), a cytokine that stimulates immune activity, and a PD-L1 (programmed death ligand 1) inhibitor, an immune checkpoint inhibitor that prevents cancer cells from deactivating the immune response. In mouse models of prostate and ovarian cancer, the modified CAR-T cells triggered a localized attack, reducing the tumor without causing toxicity in other parts of the body. These findings have just been published in the journal Nature Biomedical Engineering.
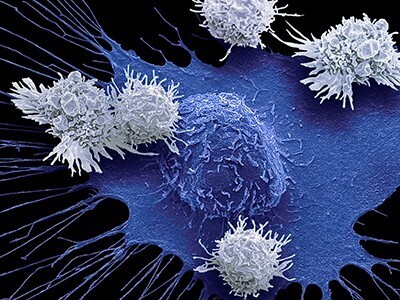
A computational approach by St. Jude Children's Research Hospital scientists promises to make designing T cell-based immunotherapies that target two cancer-related antigens at the same time far easier and faster.
BigField GEG Tech's insight:
While CAR-T cells have been successful in treating certain blood cancers, they have not been as effective in treating solid and brain tumors. One reason for this is that cancer cells do not uniformly express the same proteins. Thus, CAR-T cells targeting a single antigen may miss malignant cells that do not express that protein, leading to tumor recurrence and difficult-to-treat relapse. For this reason, scientists have attempted to create CARs that target two proteins at once. However, they encountered problems, including low CAR expression on the surface of T cells and suboptimal anti-cancer capacity. To address this, the researchers developed a computational method to screen many theoretical models of tandem CARs and rank the best candidates for further optimization and validation. The researchers generated and experimentally validated the highest-ranked tandem CAR candidates against selected targets, demonstrating that computationally optimized CARs overcame previous difficulties and performed better in treating animal models of cancer.
A new study, led by researchers at Children's Hospital of Philadelphia (CHOP), identified tiny pieces of messenger RNA that are missing in pediatric high-grade glioma tumors but not in normal brain tissues.
BigField GEG Tech's insight:
Adoptive immunotherapies based on CAR-T cells show promise against cancer; however, they often also target healthy cells, which share most surface proteins with cancer cells. While this collateral damage may be tolerable in patients with certain blood cancers, the destruction of healthy neurons in the brain is unacceptable. However, alternative splicing could be a potential avenue for discovering new therapeutic targets for brain tumors. By studying microexons in detail, the researchers discovered that the shortened version of NRCAM generated by microexon skipping was essential for cancer cell migration and invasion in Petri dishes, as well as for tumor growth in a preclinical mouse model implanted with glioma cells. This makes the glioma-specific version of NRCAM a particularly attractive target for immunotherapy, as tumors will not be able to easily disable it. Because the omission of NRCAM microexons profoundly alters the conformation of the protein, the researchers were able to develop a murine monoclonal antibody that marks cells for destruction by T cells equipped with an immune receptor for mouse antibodies.
Researchers at MUSC Hollings Cancer Center have identified a signaling loop involved in the growth and persistence of leukemia cells – and developed a novel immunotherapy that can disrupt that loop to boost immune function and improve survival.
BigField GEG Tech's insight:
Acute myeloid leukemia (AML) is one of the most aggressive blood cancers, with poor response to chemotherapy or CAR-T cell therapy. This is notably due to a self-sustaining signaling loop that allows leukemia stem cells to grow and evade treatment. A study published in Nature Communications has just outlined a groundbreaking bispecific antibody that disrupts this mechanism. The novel antibody tackles leukemia on two fronts : it blocks the IL-33/IL1RL1 protective feedback loop, while recruiting T-cells that target IL1RL1-expressing leukemia cells. In preclinical models, this dual-action strategy eradicated the shielded cancer cells, enhanced immune response, reduced relapse, and improved survival, all without significant toxicity. While Phase I trials are to follow, this approach may be replicated for cancers where IL1RL1 is also expressed in the tumor microenvironement.
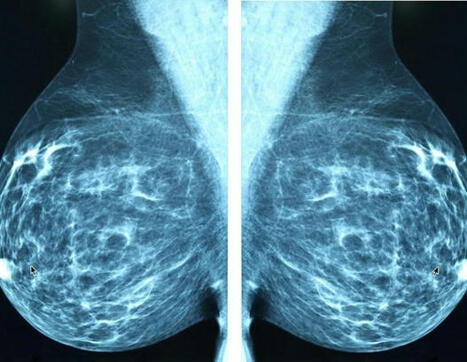
The Calibr-Skaggs Institute for Innovative Medicines, the drug development division of Scripps Research, today announced a milestone in cancer treatment with the dosing of the first patient in a phase 1 trial (NCT06878248) evaluating CLBR001 + ABBV-461, a modular, switchable chimeric antigen receptor T cell (sCAR-T) therapy in patients with advanced or metastatic breast cancer who have no suitable treatment options.
BigField GEG Tech's insight:
CAR-T therapy has revolutionized the treatment of patients with hematological malignancies who have failed many previous therapies. However, conventional CAR-T therapies have yet to achieve similar success in patients with solid tumors. This is precisely the challenge that Calibr-Skaggs' switchable CAR-T cell therapy platform aims to address. The sCAR-T platform developed by Calibr-Skaggs aims to improve the precision and safety of CAR-T therapies. It has shown promising preliminary results in a Phase 1 clinical trial in hematological malignancies. In addition, early results have demonstrated that CLBR001 sCAR-T cells can multiply in the body in significantly higher numbers than conventional CAR-T cells, offering a better chance of penetrating the hostile solid tumor microenvironment. In addition, this change offers the added benefit of allowing the cells to “rest”, potentially preventing CAR-T cell exhaustion.
Chimeric Antigen Receptor (CAR)-T cells are a promising cancer therapy that are made from the patient's own T cells, which are reprogrammed to fight their cancer. One of the limitations of CAR-T cell therapy is the ability of these cells to survive long enough to target the entire tumor.
BigField GEG Tech's insight:
Chimeric Antigen Receptor (CAR)-T cells have revolutionized cancer therapy, by reprogramming the patient’s own T cells to fight their cancer. Yet, one current limitation is that CAR-T cells don’t survive long enough to target the whole tumor. To that effect, researchers from Massachusetts General Hospital have introduced a novel approach to enhance CAR T-cell therapy for solid tumors by improving T-cell survival and persistence. They engineered CAR T-cells to be resistant to interferon-gamma (IFN-γ) signaling by knocking out the IFN-γ receptor (IFNGR) using CRISPR-Cas9. This modification allows the cells to maintain their tumor-killing capabilities, enabled by IFN-γ, while reducing activation-induced cell death, leading to prolonged survival and expansion. In preclinical murine models, these IFNGR-deficient CAR T-cells demonstrated enhanced efficacy against solid tumors without compromising safety. This advancement addresses a significant hurdle in solid tumor immunotherapy, offering a promising strategy to improve the durability and effectiveness of CAR T-cell treatments.
When a neuron in our body gets damaged, segments of RNA produce proteins that can help repair the injury.
BigField GEG Tech's insight:
When a neuron is damaged, segments of RNA produce proteins that help repair the lesion. However, in neurological disorders such as ALS and spinal muscular atrophy, or following damage to the spinal cord, the mechanisms for transporting life-sustaining RNA to damaged sites in the cell fail. As a result, RNA molecules are unable to reach their target, and damage becomes permanent. Stanford researchers have developed a technology dubbed CRISPR-TO, to transport RNA to specific areas of a neuron, where it can repair and even regenerate parts of the cell. The researchers used a version of CRISPR, called CRISPR-Cas13, to target individual RNA fragments. The researchers associated Cas13 with specific localization signals that act as addresses, telling Cas13 where to deliver the RNA. Each location in the cell has its own address molecule, so the researchers can direct RNA to different locations by adding different molecules to the cell. Their work, supported by the National Institutes of Health, forms the basis of a new class of therapies which the researchers call “RNA space medicine”, and which they hope will pave the way for the treatment of neurological diseases and trauma.
Renier Brentjens, MD, PhD, discusses the current landscape of CAR T-cell agents in patients with solid tumors.
BigField GEG Tech's insight:
The first CAR T-cell therapy was approved for pediatric acute lymphoblastic leukemia back in 2017. CAR T-cell therapies are now advancing beyond hematologic malignancies, showing early efficacy in solid tumors. Agents like satricabtagene autoleucel (satri-cel) and ALLO-316 have demonstrated promising activity in gastrointestinal cancer and renal cell carcinoma, respectively. They have received FDA designations such as fast track and regenerative medicine advanced therapy (RMAT). Solid tumors present unique challenges, including antigen heterogeneity, immunosuppressive microenvironments, and fibrotic structures that hinder CAR T-cell infiltration and function. To address these, researchers are exploring combination strategies, such as pairing CAR T-cells with immune checkpoint inhibitors, to enhance efficacy. These developments suggest a promising future for CAR T-cell therapies in treating solid tumors, with ongoing research focused on improving targeting precision and reducing toxicity. The field is moving toward more effective and safer treatments for patients with solid malignancies.
Trial in China is one of the first times the immune therapy has worked against solid tumours.
BigField GEG Tech's insight:
Trial in China is one of the first times the immune therapy has worked against solid tumours.
A new review outlines genetic engineering strategies, including CRISPR, to enhance the therapeutic potential of innate immune cells in cancer immunotherapy. The authors evaluate preclinical studies and emerging clinical data on how these cells can be retooled to overcome the limitations of conventional CAR T cell therapy.
BigField GEG Tech's insight:
Gene editing is redefining the potential of cancer immunotherapy, not only by enhancing precision, but also by extending its reach beyond T cells. A recent Nature Biotechnology review highlights how CRISPR is being used to reprogram innate immune cells, including Natural Killer (NK) cells, macrophages, and γδ T cells, to enhance their tumor-fighting abilities. By knocking out inhibitory genes, NK cells become more resilient, metabolically robust, and cytotoxic. Macrophages, typically immunosuppressive within the tumor microenvironment, are now being engineered with CARs and cytokines to adopt proinflammatory, anti-tumor roles. γδ T cells, which combine innate and adaptive immune features, are also being explored for CAR-based therapies thanks to their stress-sensing T-cell receptors and natural cytotoxicity. Early trials across multiple tumor types suggest these engineered cells could drive a new wave of more effective and versatile cancer immunotherapies.
BigField GEG Tech's insight:
A new class of molecules capable of killing the cancer cells that are refractory to standard treatments and responsible for recurrence has just been developed by scientists at Institut Curie, the CNRS, and Inserm. This crucial advance in the fight against metastatic cancer is based on identifying the cellular site for ferroptosis initiation, a natural process, catalysed by iron, that sparks the oxidative degradation of cell membranes. These promising preclinical results will be published in the journal Nature on 7 May 2025.
Genome editing has advanced at a rapid pace with promising results for treating genetic conditions-but there is always room for improvement.
BigField GEG Tech's insight:
One of the key elements in the use of CRISPR-Cas9 technologies lies in the need for enzymes to locate and bind to a short DNA sequence called the adjacent proto-spacer motif (PAM). The researchers used a machine-learning algorithm, called PAMmla, to predict the PAMs of millions of Cas9 enzymes, thereby identifying a set of novel Cas9 enzymes designed to exhibit the best targeted activity and specificity. The researchers conducted proof-of-concept experiments on human cells and a mouse model of retinitis pigmentosa, and found that the tailored enzymes exhibited greater specificity. This work could help reduce off-target effects, improve the safety and efficacy of editing, and enable researchers to predict customized enzymes for new therapeutic targets. |









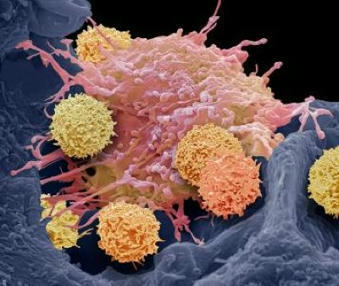






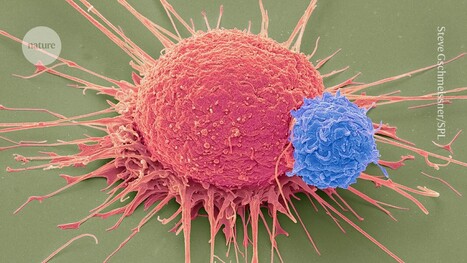








Testing in mice suggests that rejuvenating T cells could make vaccines and some cancer therapies more effective.