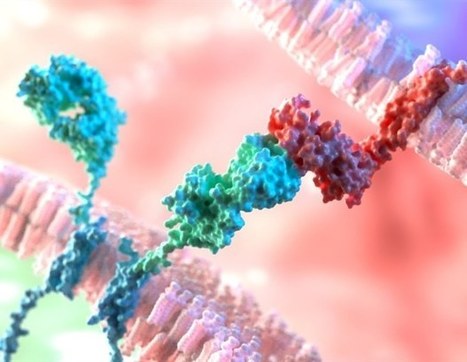
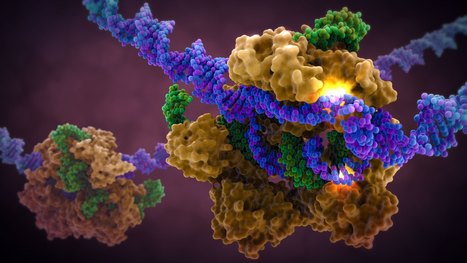
A landmark study published in Cell has shown that prime editing, a cutting-edge form of gene editing, can correct mutations causing Alternating Hemiplegia of Childhood (AHC) with a single in-brain injection. The research team fixed the most prevalent ATP1A3 gene mutations in mouse models, reducing symptoms and more than doubling survival, a first-of-its-kind success in treating a neurological disease directly in the brain. CRISPR-based gene editing was delivered through an harmless adeno-associated virus called AAV9. In parallel, patient-derived cells (iPSCs) responded similarly, reinforcing the method’s promise for human translation. Importantly, this success opens the door to targeting other genetic brain disorders previously deemed untreatable. Although results are preliminary, this study provides robust proof‑of‑concept for personalized gene editing in the brain and opens doors toward potential treatments for other intractable genetic neurological disorders.





 Your new post is loading...
Your new post is loading...





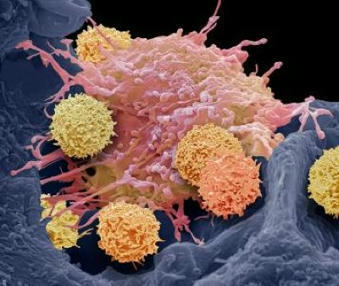


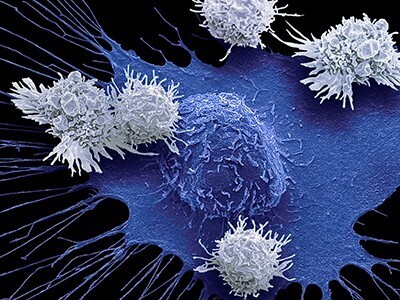
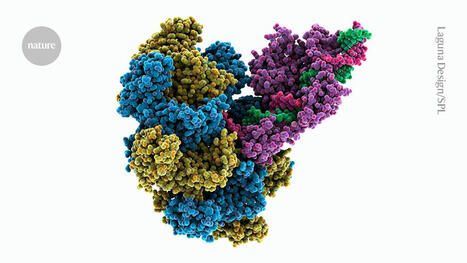




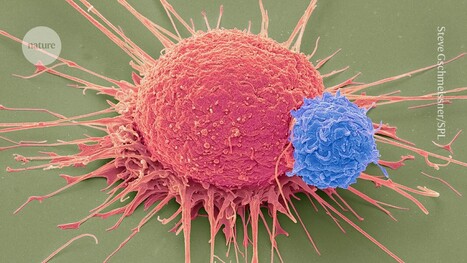








While CAR-T cells have been successful in treating certain blood cancers, they have not been as effective in treating solid and brain tumors. One reason for this is that cancer cells do not uniformly express the same proteins. Thus, CAR-T cells targeting a single antigen may miss malignant cells that do not express that protein, leading to tumor recurrence and difficult-to-treat relapse. For this reason, scientists have attempted to create CARs that target two proteins at once. However, they encountered problems, including low CAR expression on the surface of T cells and suboptimal anti-cancer capacity. To address this, the researchers developed a computational method to screen many theoretical models of tandem CARs and rank the best candidates for further optimization and validation. The researchers generated and experimentally validated the highest-ranked tandem CAR candidates against selected targets, demonstrating that computationally optimized CARs overcame previous difficulties and performed better in treating animal models of cancer.