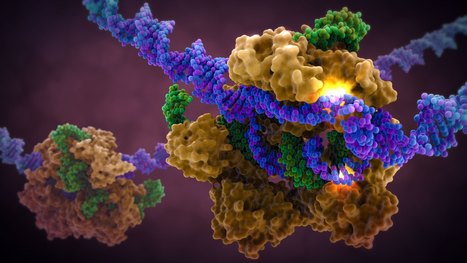
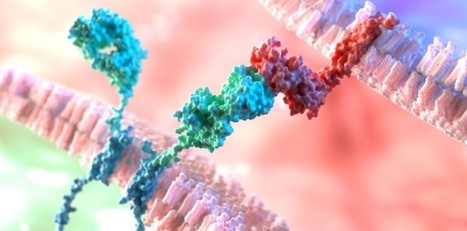
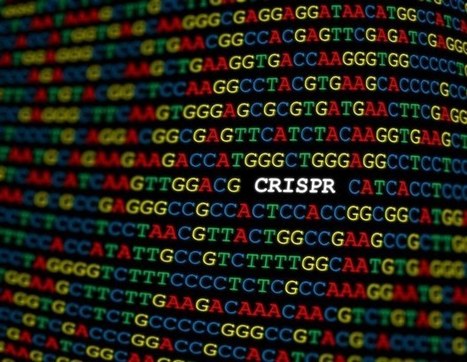
A landmark study published in Cell has shown that prime editing, a cutting-edge form of gene editing, can correct mutations causing Alternating Hemiplegia of Childhood (AHC) with a single in-brain injection. The research team fixed the most prevalent ATP1A3 gene mutations in mouse models, reducing symptoms and more than doubling survival, a first-of-its-kind success in treating a neurological disease directly in the brain. CRISPR-based gene editing was delivered through an harmless adeno-associated virus called AAV9. In parallel, patient-derived cells (iPSCs) responded similarly, reinforcing the method’s promise for human translation. Importantly, this success opens the door to targeting other genetic brain disorders previously deemed untreatable. Although results are preliminary, this study provides robust proof‑of‑concept for personalized gene editing in the brain and opens doors toward potential treatments for other intractable genetic neurological disorders.






 Your new post is loading...
Your new post is loading...




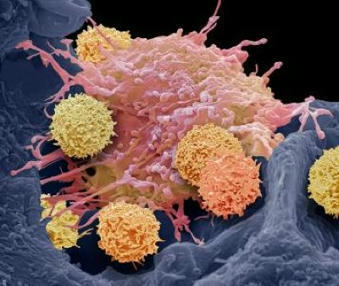


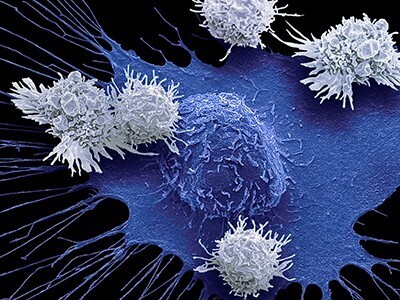



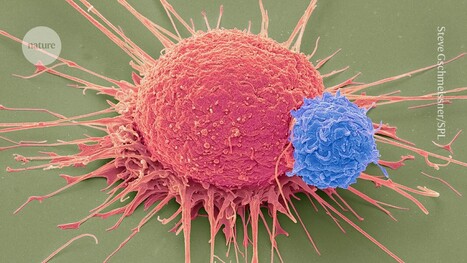








Adoptive immunotherapies based on CAR-T cells show promise against cancer; however, they often also target healthy cells, which share most surface proteins with cancer cells. While this collateral damage may be tolerable in patients with certain blood cancers, the destruction of healthy neurons in the brain is unacceptable. However, alternative splicing could be a potential avenue for discovering new therapeutic targets for brain tumors. By studying microexons in detail, the researchers discovered that the shortened version of NRCAM generated by microexon skipping was essential for cancer cell migration and invasion in Petri dishes, as well as for tumor growth in a preclinical mouse model implanted with glioma cells. This makes the glioma-specific version of NRCAM a particularly attractive target for immunotherapy, as tumors will not be able to easily disable it. Because the omission of NRCAM microexons profoundly alters the conformation of the protein, the researchers were able to develop a murine monoclonal antibody that marks cells for destruction by T cells equipped with an immune receptor for mouse antibodies.