The genetic mutation underlying a severe immune system deficiency can be corrected
by adenine base editing of human patient stem cells, restoring the ability of these
cells to develop into functional T cells in model systems, and paving the path for
future treatment of CD3δ SCID in patients.

|
Scooped by
BigField GEG Tech
onto Genetic Engineering Publications - GEG Tech top picks April 6, 2023 7:15 AM
|





 Your new post is loading...
Your new post is loading...



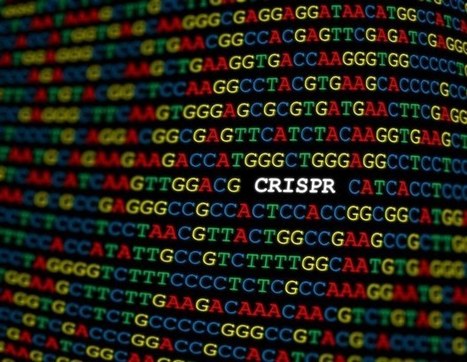
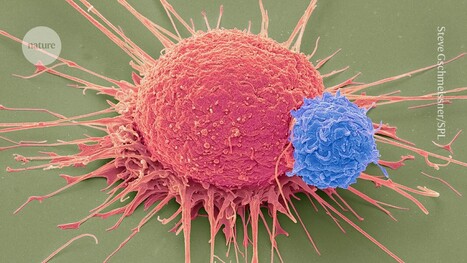



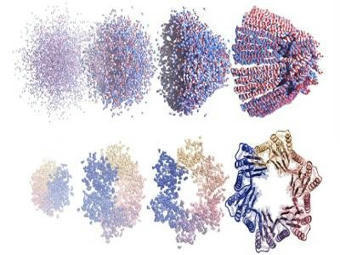
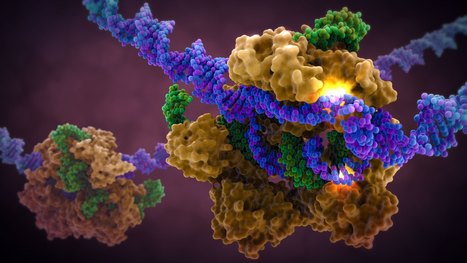




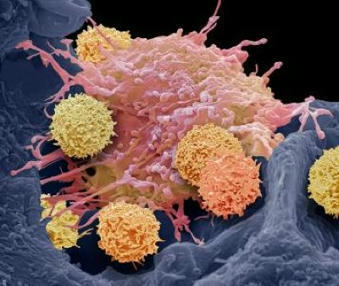


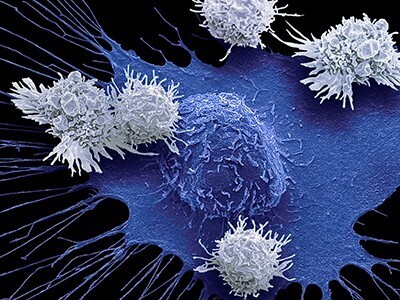
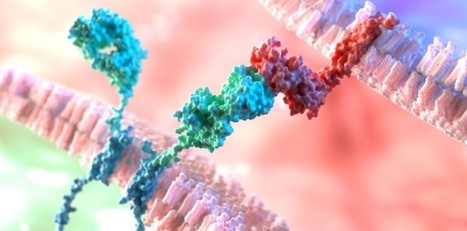
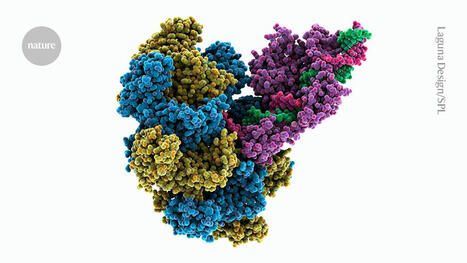






The rare and fatal genetic disease CD3 delta severe combined immunodeficiency, also known as CD3 delta SCID, is caused by a mutation in the CD3D gene, which prevents the production of the CD3 delta protein needed for normal T cell development from blood stem cells. Currently, bone marrow transplantation is the only treatment available, but the procedure carries significant risks. In a study published in Cell, researchers showed that a new genome editing technique called base editing can correct the mutation that causes CD3 delta SCID in blood stem cells and restore their ability to produce T cells. The basic editor corrected an average of nearly 71 percent of the patient's stem cells in three experiments. The researchers then tested whether the corrected cells could give rise to T cells. When the corrected blood stem cells were introduced into artificial thymic organoids, they produced fully functional and mature T cells. The corrected cells remained four months after transplantation, indicating that the basic editing had corrected the mutation in the true self-renewing blood stem cells. The results suggest that the corrected blood stem cells could persist over the long term and produce the T cells that patients would need to lead healthy lives.