A new type of immunotherapy that targets aggressive blood cancers shows promising results alongside manageable side effects, according to the results of an international phase 1/2 clinical trial led by researchers at Washington University School of Medicine in St. Louis.

|
Scooped by
BigField GEG Tech
onto Genetic Engineering in the Press by GEG June 24, 2025 10:01 AM
|





 Your new post is loading...
Your new post is loading...
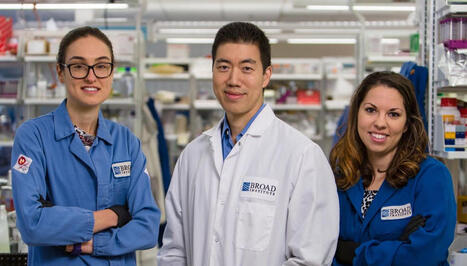
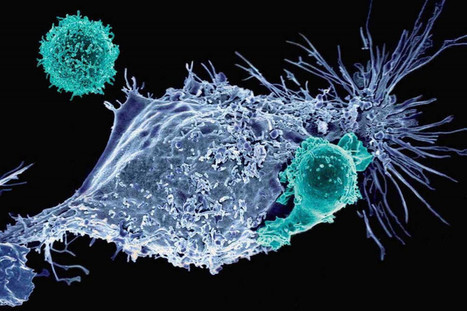


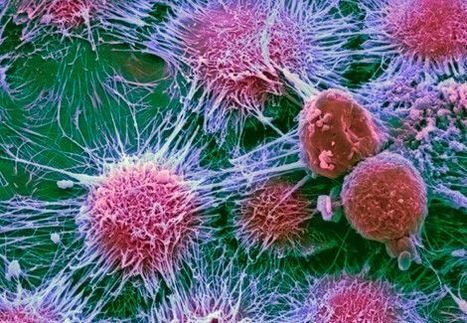
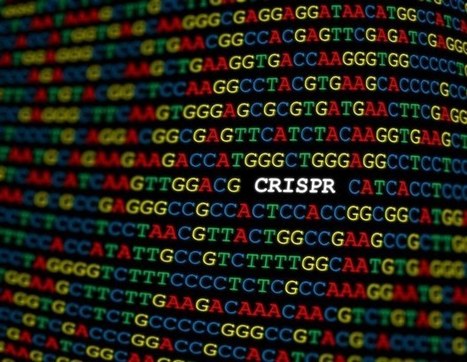
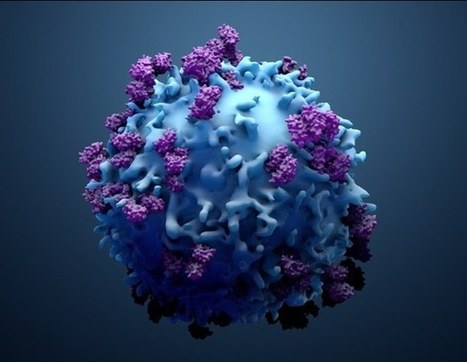

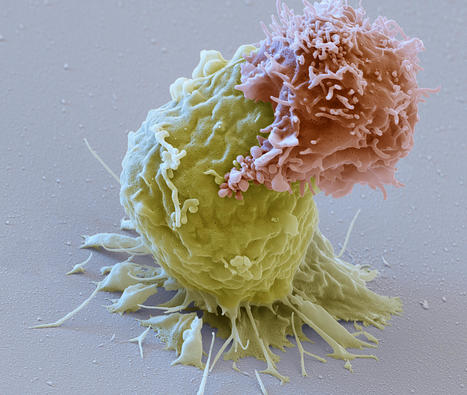
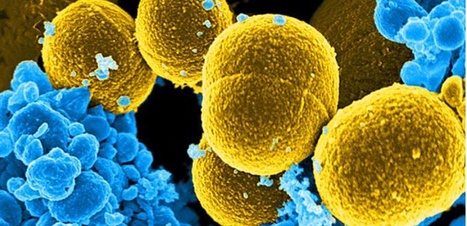






A new type of immunotherapy, called WU-CART-007, targeting aggressive blood cancers is showing promising results as well as manageable side effects, according to the results of an international phase 1/2 clinical trial conducted by researchers. Participants in the trial had been diagnosed with a rare cancer: T-cell acute lymphoblastic leukemia or T-cell lymphoblastic lymphoma, and had run out of treatment options as standard therapy had proved ineffective. In the process of its production, CRISPR deletes the T-cell receptor from donor cells, thereby considerably reducing the risk of graft-versus-host disease, in which donor T cells attack healthy tissue. Deletion of another key antigen also prevents CAR-T cells from attacking each other. After using CRISPR gene editing to modify CAR-T cells to prevent these harmful side effects, the cells are then modified to target a protein called CD7 on the surface of cancer T cells to destroy the cancer. The clinical trial evaluated the safety and efficacy of an innovative CAR-T cell-based immunotherapy, specifically designed to attack cancer T cells. Thanks to this new immunotherapy, most patients in the study who received the full dose of cells achieved complete remission of their cancer.