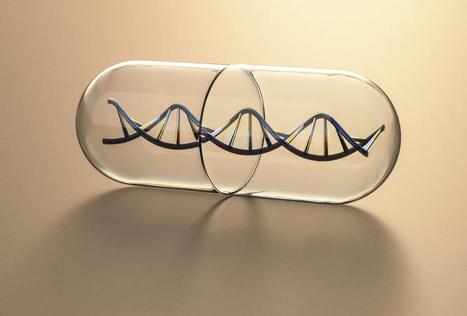
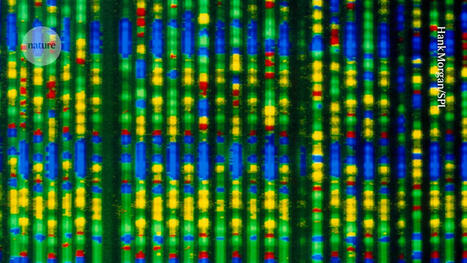
The Human Genome Project was an ambitious initiative to sequence every piece of human DNA. The project drew together collaborators from research institutions around the world, including Whitehead Institute, and was finally completed in 2003.

|
Scooped by
BigField GEG Tech
onto Genetic Engineering in the Press by GEG June 20, 2022 6:32 AM
|




 Your new post is loading...
Your new post is loading...
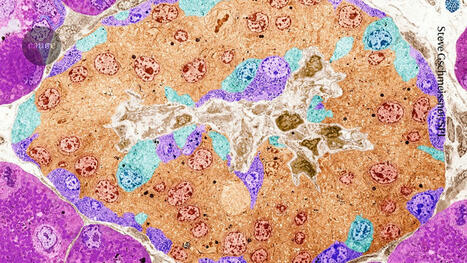










Jonathan Weissman, a member of the Whitehead Institute, and his colleagues have produced the first comprehensive functional map of genes expressed in human cells. The data from this project, published online on 9 June in Cell, associates each gene with its work in the cell. For this project, the researchers used the Perturb-seq method, which uses CRISPR/Cas9 genome editing to introduce genetic modifications into cells, and then uses single-cell RNA sequencing to capture information about the expressed RNAs resulting from a given genetic modification. Since RNAs control all aspects of cell behavior, this method can help decipher the many cellular effects of genetic modifications. Using human blood cancer cell lines as well as non-cancerous retina-derived cells, the researchers performed a Perturb-seq on over 2.5 million cells and used the data to create a comprehensive map linking genotypes to phenotypes. Once completed, the researchers decided to use their new dataset and examine some biological questions. In the future, the researchers hope to use Perturb-seq on different cell types in addition to the cancer cell line they started with. They also hope to continue exploring their map of gene functions and hope that others will do the same.