Your new post is loading...
 Your new post is loading...

|
Scooped by
Gilbert C FAURE
December 2, 2013 9:13 AM
|
A topic dedicated to allergy
ouvert dans le contexte du DESC d'Immunologie clinique et allergologie en France opened for 10 years, > 2800 Highly selected scoops in an evolving and controversial field >14.4 K Views by > 4.4 K viewers

|
Scooped by
Gilbert C FAURE
February 11, 6:28 AM
|
De-Labelling Penicillin Allergies in the Paediatric Emergency Department
"While many children carry a penicillin allergy label, the vast majority do not have a true immunologically mediated allergy, leading to a lifetime risk of avoidable use of broad-spectrum antibiotics, higher healthcare costs, and poorer clinical outcomes."
Most children thought to have a penicillin allergy actually don't.
Giving them an alternative to a penicillin-based antibiotic (because of said "allergy") denies them from receiving the best treatment for their infection.
Any opportunity to remove the incorrect "penicillin allergy" label will help them receive better care.
via Ceri Phillips cc Damian Roland
https://lnkd.in/e5bZiEwr

|
Scooped by
Gilbert C FAURE
February 11, 4:07 AM
|
Is IgE really just the antibody of allergy — or a core pillar of human immunity?
A seminal review in Frontiers in Immunology challenges the idea that IgE is merely pathologic. Instead, it argues that IgE evolved as a protective immune mechanism against multicellular parasites, particularly helminths — with major implications for immune-compromised patients.
Key insights:
• IgE-driven Th2 responses are physiologic in helminth infection, not aberrant
• Most environmental allergens belong to the same protein families targeted during parasitic infection
• Parasite-specific IgE correlates with resistance to reinfection in schistosomiasis, hookworm, and ascariasis
• Helminths actively regulate host immunity, shaping tolerance via IL-10, TGF-β, and IgG4
Why this matters in immune-compromised states
In conditions such as advanced HIV, malignancy, chemotherapy, or immunosuppressive therapy:
• IgE responses may dominate as other immune pathways fail
• Cross-reactive IgE can mimic allergy, malignancy, or autoimmune disease
• Loss of regulatory balance may convert protective IgE into clinically significant inflammation
• Atypical eosinophilia, tissue infiltration, or mass-like immune phenomena may result
This framework helps explain why immune-compromised patients often present with non-classic, confusing inflammatory patterns — and why parasite-derived antigens can be protective in healthy hosts yet harmful in immune-dysregulated ones.
Takeaway:
IgE may represent an ancient survival system that becomes maladaptive only when immune regulation breaks down. Understanding this axis is critical for allergy, parasitology, vaccine development — and modern clinical immunology.
📄 Helminth allergens, parasite-specific IgE, and its protective role in human immunity (Frontiers in Immunology)
Authors:
Colin Matthew Fitzsimmons • Franco Harald Falcone • David William Dunne
(University of Cambridge | University of Nottingham)
#Immunology #IgE #Immunocompromised #ClinicalImmunology #Allergy #Parasitology #TranslationalMedicine #GlobalHealth

|
Scooped by
Gilbert C FAURE
January 16, 10:43 AM
|
On IDSA’s & HIVMA’s Science Speaks blog: Kap Sum Foong, MD, FIDSA, explores how proposed legislation can help close gaps by aligning reimbursement, EHR integration and workforce training to make penicillin allergy delabeling routine across all care settings. https://lnkd.in/eM4tmYTF

|
Scooped by
Gilbert C FAURE
January 14, 7:22 AM
|
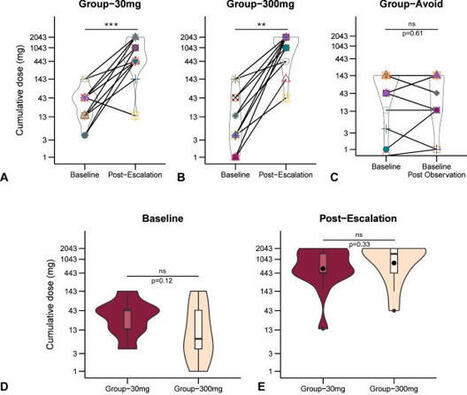
A very low maintenance dose of #peanut #oral #immunotherapy significantly increased tolerated peanut exposure and improved immunologic markers compared with strict avoidance, achieving desensitisation similar to a high dose. https://lnkd.in/dfAtjB2Y

|
Scooped by
Gilbert C FAURE
January 8, 4:58 AM
|
💡 𝐖𝐡𝐚𝐭 𝐢𝐟 𝐰𝐞 𝐜𝐨𝐮𝐥𝐝 𝐭𝐞𝐚𝐜𝐡 𝐁 𝐜𝐞𝐥𝐥𝐬 𝐭𝐨 "𝐟𝐨𝐫𝐠𝐞𝐭" 𝐈𝐠𝐄??
📖 In a recent Science Immunology study, long-term allergic memory was mapped 𝐧𝐨𝐭 𝐭𝐨 𝐈𝐠𝐄 cells, but mainly to 𝐈𝐠𝐆𝟏⁺ 𝐦𝐞𝐦𝐨𝐫𝐲 𝐁 𝐜𝐞𝐥𝐥𝐬 with a type-2 imprint, primed to change from IgG1 to IgE when the allergen returns (recall).
🧬 𝐃𝐢𝐬𝐜𝐨𝐯𝐞𝐫𝐢𝐧𝐠 𝐓-𝐩𝐨𝐰𝐞𝐫
🔁 𝐓-𝐜𝐞𝐥𝐥 𝐜𝐲𝐭𝐨𝐤𝐢𝐧𝐞𝐬 as gatekeepers: 𝐈𝐋-𝟒/𝐈𝐋-𝟏𝟑 drive this switch at recall; dampen those cues and IgE recall drops. Notably, exposing these memory B cells to allergen without IL-4 can make them “𝐟𝐨𝐫𝐠𝐞𝐭” 𝐭𝐡𝐞 𝐈𝐠𝐄 𝐩𝐫𝐨𝐠𝐫𝐚𝐦 and default to 𝐈𝐠𝐆, even when IL-4 reappears later.
🧪 𝐋𝐞𝐭’𝐬 𝐥𝐞𝐚𝐫𝐧 (𝐧𝐞𝐮𝐫𝐨)𝐈𝐦𝐦𝐮𝐧𝐨𝐥𝐨𝐠𝐲 — 𝐀𝐥𝐥𝐞𝐫𝐠𝐲 𝐛𝐚𝐬𝐢𝐜𝐬
• 𝐀𝐥𝐥𝐞𝐫𝐠𝐲 = an excessive immune response to a 𝐡𝐚𝐫𝐦𝐥𝐞𝐬𝐬 𝐚𝐧𝐭𝐢𝐠𝐞𝐧 (𝐚𝐥𝐥𝐞𝐫𝐠𝐞𝐧) recognized by 𝐈𝐠𝐄 𝐚𝐧𝐭𝐢𝐛𝐨𝐝𝐢𝐞𝐬.
• 𝐈𝐠𝐄 binds to its high-affinity receptor (𝐅𝐜ε𝐑𝐈) on 𝐦𝐚𝐬𝐭 𝐜𝐞𝐥𝐥𝐬 and 𝐛𝐚𝐬𝐨𝐩𝐡𝐢𝐥𝐬; upon re-exposure, the allergen cross-links IgE → 𝐝𝐞𝐠𝐫𝐚𝐧𝐮𝐥𝐚𝐭𝐢𝐨𝐧 (histamine release…) → hives, wheezing, anaphylaxis.
• 𝐈𝐠𝐆𝟏⁺ 𝐦𝐞𝐦𝐨𝐫𝐲 𝐁 𝐜𝐞𝐥𝐥𝐬 store the “recipe”; with 𝐈𝐋-𝟒/𝐈𝐋-𝟏𝟑 they can 𝐜𝐥𝐚𝐬𝐬-𝐬𝐰𝐢𝐭𝐜𝐡 𝐛𝐚𝐜𝐤 𝐭𝐨 𝐈𝐠𝐄, helping explain relapses.
🧬 𝐂𝐡𝐚𝐥𝐥𝐞𝐧𝐠𝐢𝐧𝐠 𝐭𝐡𝐞 𝐩𝐚𝐫𝐚𝐝𝐢𝐠𝐦: the immune system is not a defense system… it is much more than that.
🔗 𝐑𝐞𝐚𝐝 𝐭𝐡𝐞 𝐩𝐚𝐩𝐞𝐫 𝐢𝐧 𝐒𝐜𝐢𝐞𝐧𝐜𝐞 𝐈𝐦𝐦𝐮𝐧𝐨𝐥𝐨𝐠𝐲: https://lnkd.in/d5zeXDDX
🔖 Save for later. 🔁 Share with your science-curious friends.
#immunology #allergy #IgE #Bcells #IL4 #IL13 #mastcells #ScienceImmunology #ChallengingTheParadigm

|
Scooped by
Gilbert C FAURE
January 4, 5:04 AM
|
L’intelligence artificielle s’impose progressivement dans les salles de consultation. À l’UZ Leuven, l’IA a récemment commencé à aider à l’interprétation des tests d’allergie. Selon une étude internationale, elle pourrait être plus rapide, plus cohérente et plus fiable que l’analyse humaine. Un journaliste de Het Laatste Nieuws, Steven Swinnen, a réalisé un de ces tests 2.0 et a obtenu un résultat surprenant.

|
Scooped by
Gilbert C FAURE
December 29, 2025 11:13 AM
|
Key lung immune cells can intensify allergic reactions
“Alveolar macrophages have long been seen as peacekeepers in the lung,” said the first author of the study. “Our results show that during allergic responses, they can do the opposite and actually help drive inflammation.”
Using an advanced mouse model that allowed the researchers to precisely track and manipulate these lung cells, the team discovered that allergen exposure causes alveolar macrophages to send out signals that attract other immune cells into the lung. This influx amplifies inflammation and worsens allergic reactions. Remarkably, the macrophages were also found to fuse together into large ‘giant cells’ that change the structure of the lung tissue during allergy.
Mechanistically, upon allergen exposure, interleukin-33-activated innate type 2 lymphoid cells (ILC2s) produced interleukin-13, which reprogrammed trAMs through induction of the transcription factor interferon regulatory factor 4 (IRF4).
IRF4 suppressed the expression of the transcription factor peroxisome proliferator-activated receptor gamma (PPARγ) and dismantled the PPARγ-dependent homeostatic regulon that defines trAM identity, while initiating a transcriptional program driving chemokine production and cell fusion. This resulted in the recruitment of granulocytes, ILC2s, and regulatory T cells, as well as the formation of multinucleated giant cells in the alveolar niche.
These findings challenge the long-standing view that alveolar macrophages are stable cells that resist change. Instead, the study reveals that they are surprisingly flexible and can be reprogrammed by their environment, sometimes with harmful consequences.
#ScienceMission #sciencenewshighlights
https://lnkd.in/gMDVj3Rq

|
Scooped by
Gilbert C FAURE
December 24, 2025 4:21 AM
|
🐾 Allergie aux chats : un enjeu de santé publique sous-estimé !
En Europe, près d’1 personne allergique sur 4 est sensibilisée aux allergènes de chat. En France, ce chiffre atteint 10 à 15 % des adultes, et jusqu’à 67 % chez les personnes asthmatiques selon les études. L’exposition, même modérée, peut suffire à induire une sensibilisation dès l’enfance.
🔬 Des conséquences majeures :
Près de la moitié des patients allergiques aux chats souffrent d’asthme, avec un risque accru d’exacerbation à chaque contact.
La sensibilisation aux allergènes de chat est associée à des formes plus sévères d’asthme, soulignant l’importance de cette exposition dans la gravité de la maladie.
🚫 L’éviction totale des chats reste très difficile, voire impossible.
💡 Des solutions existent ! Une étude en vie réelle menée chez des patients désensibilisés montre que l’immunothérapie sublinguale, prescrite principalement pour l’asthme allergique (61,9 %) et la rhinite allergique (54,8 %), apporte des résultats très encourageants.
👉 L’immunothérapie sublinguale s’impose comme une option thérapeutique efficace pour améliorer la qualité de vie des patients allergiques aux chats.
#Allergie #Asthme #Immunothérapie #Santé #Chat #InnovationMédicale
👉 Merci à nos auteurs, Nhân Pham-Thi, Julien Goret, Luc Colas, Laurent Guilleminault, Silvia Scurati, Laurence Girard
👉Bravo et merci au JAHD et à Luciana Tanno de soutenir les publications françaises dans l’Allergologie.

|
Scooped by
Gilbert C FAURE
December 22, 2025 6:47 AM
|
This is one paper to bookmark. This group is the international leader in antimicrobial allergy stewardship. Structured approach to delabeling and/or referral combined with simple and effective tools.

|
Scooped by
Gilbert C FAURE
December 13, 2025 9:05 AM
|
The era of avoidance is over. Dr William Basco explains why early exposure is the new prevention and offers a protocol for introducing allergens at the 4- to 6-month mark.

|
Scooped by
Gilbert C FAURE
December 7, 2025 3:54 AM
|
An anti-allergy vaccine protects mice from anaphylaxis for as long as one year, mRNA-ferrying nanoparticles treat fatty liver disease in animals and potentiate immunotherapy against liver tumors, and more this week in #ScienceTranslationalMedicine.
https://scim.ag/4pitecZ

|
Scooped by
Gilbert C FAURE
November 18, 2025 4:27 AM
|
📢 Des algorithmes décisionnels sont disponibles dans votre espace ressources !
Pour accompagner les professionnels de santé dans leurs pratiques, nous mettons à disposition des algorithmes destinés à faciliter les démarches diagnostiques et thérapeutiques. Ces outils sont accessibles au fur et à mesure, enrichissant progressivement notre sélection.
En tant que membres de la SFA, n’hésitez pas à les consulter régulièrement. Pour profiter de ces ressources pratiques, rendez-vous sur notre site internet : https://lnkd.in/dwSN_Fqe
🔐 Pas encore membre ? Rejoignez la communauté pour bénéficier de l’ensemble des contenus : https://lnkd.in/d6-Hqdmr
#allergologie #allergies #algorithmes #adhesion
|

|
Scooped by
Gilbert C FAURE
February 11, 11:28 AM
|
🔔 Read our latest paper published "Scope, Features, and Utility of Australian Penicillin Allergy Delabelling Protocols: A Descriptive Analysis" by Prof. Dr. Sandra M Salter et al.
🔗 Link: https://brnw.ch/21wZQJI
🎓 These findings emphasise the complexity of clinical decision-making around penicillin allergy and suggest a need for standardisation of PADL-Ps to maximise delabelling benefits and safety across Australian healthcare settings.
#PenicillinAllergy #PenicillinAllergyDelabelling #PADL #AntimicrobialStewardship #PatientSafety #HealthcareQuality #ClinicalGuidelines #ASCIA #AllergyManagement #MedicationSafety #HealthcareResearch #ClinicalDecisionMaking #StandardisationInHealthcare #AustralianHealthcare #PaediatricCare #AdultMedicine #EvidenceBasedPractice #HealthPolicy #InfectiousDiseases #QualityImprovement

|
Scooped by
Gilbert C FAURE
February 11, 4:11 AM
|
ALLERGIC REACTION
Immunology & Medical Laboratory Science
1. Introduction
An allergic reaction is a common immunological phenomenon encountered in clinical practice. It represents an inappropriate and exaggerated immune response to substances that are ordinarily harmless. While many allergic reactions are mild, some can be severe and life-threatening, emphasizing the importance of understanding their mechanism, diagnosis, and laboratory relevance.
2. Definition
An allergic reaction is an immunologically mediated hypersensitivity response that occurs when a previously sensitized individual is re-exposed to a specific allergen, leading to activation of immune cells and release of inflammatory mediators.
Most allergic reactions are classified as Type I (IgE-mediated) hypersensitivity reactions.
3. Allergens and Routes of Exposure
3.1 Common Allergens
Allergens are substances capable of inducing allergic reactions in susceptible individuals.
•Inhaled allergens: pollen, dust mites, mold spores, animal dander
•Ingested allergens: peanuts, shellfish, eggs, milk, drugs
•Injected allergens: insect stings, injectable drugs, blood products
•Contact allergens: latex, cosmetics, metals (nickel), detergents
3.2 Routes of Entry
•Respiratory tract
•Gastrointestinal tract
•Skin
•Bloodstream
The route of entry influences the clinical presentation.
4. Immunological Mechanism of Allergic Reaction
Allergic reactions occur in two main phases:
4.1 Sensitization Phase (Primary Exposure)
This phase occurs during the first exposure to the allergen and does not produce clinical symptoms.
Steps involved:
1. The allergen enters the body.
2. Antigen-presenting cells (APCs) process the allergen.
3. APCs present the antigen to CD4⁺ T helper (Th2) cells.
4. Th2 cells release cytokines such as IL-4 and IL-13.
5. These cytokines stimulate B cells to produce IgE antibodies.
6. IgE binds to high-affinity FcεRI receptors on mast cells and basophils.
The individual is now sensitized.
4.2 Effector Phase (Re-exposure)
Upon subsequent exposure to the same allergen:
1. The allergen binds to IgE on mast cells.
2. Cross-linking of IgE occurs.
3. Mast cells undergo degranulation.
4. Inflammatory mediators are released, producing clinical symptoms.
5. Chemical Mediators Released
5.1 Pre-formed Mediators
•Histamine: causes vasodilation, itching, edema, and bronchoconstriction
5.2 Newly Synthesized Mediators
•Leukotrienes: bronchoconstriction and mucus secretion
•Prostaglandins: inflammation and pain
•Cytokines: recruit eosinophils and other inflammatory cells
These mediators are responsible for the acute and late-phase reactions.
#MedicalLaboratoryScience
#Immunology
#AllergicReactions
#PatientSafety
#LaboratoryMedicine
#HealthcareEducation
#MLS

|
Scooped by
Gilbert C FAURE
February 2, 3:28 AM
|
What Your IgG Test Results Mean (and Don’t Mean)
TL;DR: IgG sensitivity tests can’t tell you what foods you're sensitive to.
IgG sensitivity tests claim to work by measuring levels of IgG antibodies in your blood against specific foods. Some test up to 100 foods, and the idea is that if your body makes a lot of IgG to a certain food, it means your immune system sees that food as a “problem.” Companies that make these tests say this immune response may be linked to symptoms like bloating, fatigue, headaches, or skin issues. Based on the results, they recommend avoiding foods that show high IgG levels.
However, these tests measuring IgG antibodies, aren't scientifically proven. Experts, including the American Academy of Allergy, Asthma, and Immunology (AAAAI), say IgG antibodies actually show normal exposure and tolerance to a food. Meaning that your body tolerates those foods, not that you're sensitive to them!
These tests are expensive and can lead to unnecessary food restrictions and can cause anxiety, nutrient deficiencies, and a bad relationship with food.
✅ An elimination diet, done with a healthcare professional, is still the best way to pinpoint food sensitivities. It takes time, but it’s the most trusted method!
https://lnkd.in/dBhYfZf2
https://lnkd.in/dYJ47Wjh
#Debunked #FoodSensitivity #GutHealth #EliminationDiet

|
Scooped by
Gilbert C FAURE
January 15, 3:54 AM
|
We are proud to share a new review published in #Allergy, the leading journal in the field of allergy research. Authored by an international team including Dr. Annette Kuehn from the Department of Infection & Immunity at the Luxembourg Institute of Health and Prof. Thomas Eiwegger of Karl Landsteiner University in Austria 👏
The paper synthesizes key insights into the immune mechanisms underlying #food allergies.
By linking current research with open questions, it provides a solid foundation for future advances in allergy research and ultimately improved care for patients 🤍🚀
Coauthors: Noémi Anna Nagy, Diana Schnoegl, Vikki Houghton, Liam O'Mahony, Alexandra Santos, MD PhD , Edward Knol

|
Scooped by
Gilbert C FAURE
January 12, 8:48 AM
|
#eaccmeaccredited
Dr. Andreas Horn / Fortbildungen und Beratungen
#eaccme
#cme
#liveevents
#allergology

|
Scooped by
Gilbert C FAURE
January 4, 12:57 PM
|
Allergies alimentaires : de grandes disparités à l’échelle mondiale
L’article proposé par la WAO Sur un projet international mené auprès de 150 centres dans 50 pays met en évidence de grandes différences dans la prise en charge des allergies alimentaires selon les pays,que ce soit dans les possibilités diagnostiques ou le prix des traitements d’urgence .
-Le test cutané est utilisé mais certaines régions d’Afrique et d’Asie y ont un accès inégal .
- les IgE spécifiques, souvent utilisées en alternative.
-L’immunothérapie orale est surtout pratiquée en Europe occidentale, puis en Amérique du Nord, en Europe du Sud et en Europe du Nord. L’omalizumab est également utilisé notamment en Europe occidentale, en Amérique du Nord, en Asie de l’Est et en Océanie.
-La sévérité des réactions varie fortement selon les zones géographiques.
L’utilisation d’adrénaline va de 3 % en Asie du Sud à 50 % en Afrique australe, avec des taux importants en Asie de l’Est, en Asie occidentale, en Europe du Sud et en Amérique du Nord. La disponibilité de l’adrénaline elle-même est très variable selon les pays, et certains n’y ont pas accès aux auto‑injecteurs,
Allergènes :Avant 5 ans, le lait et l’œuf sont les allergènes les plus fréquents. Entre 5 et 11 ans, l’œuf >du lait, >l’arachide et des fruits à coque. Chez les adolescents, l’arachide le plus courant au niveau mondial, suivie des noix et des crustacés. Chez les adultes, les crustacés, les noix, l’arachide et le poisson sont les allergènes les plus souvent rapportés,
Ces résultats montrent que les allergies alimentaires représentent un enjeu mondial majeur, influencé par l’accès aux diagnostics, aux traitements, aux auto‑injecteurs d’adrénaline et aux soins d’urgence. Selon l’outil DEFASE, environ 3 % des patients pourraient être classés comme souffrant d’allergies alimentaires sévères, un taux comparable à celui observé dans l’asthme sévère réfractaire.
https://lnkd.in/ebF3d252
Cet article est très intéressant et engage à comparer les prix dans différents pays :
les tarifs hors assurance sont d’environ 1 000 à 3 000 dollars pour une admission aux urgences aux États‑Unis et 3 000 à 10 000 dollars pour une journée en soins intensifs, alors qu’en Thaïlande une journée de soins intensifs coûte hors assurance 900 à 2 700 euros, tandis qu’en France les coûts hospitaliers sont beaucoup plus faibles grâce à la prise en charge publique, mais peuvent devenir élevés pour les personnes sans aucune assurance
Aux USA les prix vont de 199 dollars pour le nouveau spray nasal d’adrenaline à près de 300 dollars pour le système parlant injectable. Et 600 euros pour le plus connu ( tarifs hors assurance ) En France il faut compter entre environ 62 et 91 euros pour deux dispositifs . , l’Assurance maladie rembourse 65 % du prix des auto‑injecteurs d’adrénaline et, dans la plupart des cas, les complémentaires santé prennent en charge le reste du coût.

|
Scooped by
Gilbert C FAURE
December 30, 2025 9:56 AM
|
New Guidance Sets Standard for Paediatric Antibiotic Allergy Testing: in a new report, investigators USDAR-Peds introduce unified, evidence-informed protocols designed to guide clinicians in evaluating suspected antibiotic hypersensitivity in children. https://lnkd.in/dpV7Cb-S

|
Scooped by
Gilbert C FAURE
December 28, 2025 5:34 AM
|
Bronchiectasis and asthma can co-exist in the same patient, and the characteristics may be different from bronchiectasis alone. Here the authors characterise the function of ILC3 cells and how IL-17C potentiates IL-17A expression promoting a neutrophil dominated asthma endotype in mouse...

|
Scooped by
Gilbert C FAURE
December 23, 2025 1:24 PM
|

|
Scooped by
Gilbert C FAURE
December 18, 2025 4:33 AM
|
In this week’s podcast, Voices in Health and Wellness, I speak with Loren Isakson, on how to build a modern allergy and immunology practice without losing focus on the patient.
We talk about launching lean with telemedicine, shifting to in person care, and using comprehensive testing, immunotherapy, and biologics to reduce ER visits and improve stability.
We also discuss where technology helps, where it slows clinicians down, and why systems should protect time for listening and observation.
If you care about patient first allergy care, smart use of health tech, or building a sustainable medical practice, this episode offers clear and practical insight.
#AllergyCare #Immunology #HealthcareEntrepreneurship #HealthTechnology #VoicesInHealthAndWellness #AndrewGreenland

|
Scooped by
Gilbert C FAURE
December 11, 2025 4:05 AM
|
🤖 L'IA révolutionne les tests d'allergie !
🔬 Une étude récente dévoile que l'intelligence artificielle améliore considérablement le diagnostic allergologique. À l'UZ Leuven, le dispositif SPAT, développé par Hippo Dx, administre automatiquement des réactifs allergènes et utilise un algorithme d'IA pour analyser les réactions cutanées avec une précision de 99,5 %, accélérant le diagnostic près de quatre fois par rapport aux méthodes traditionnelles.
🏥 La professeure Laura Van Gerven souligne que cette avancée ne remplace pas les cliniciens, mais optimise le processus diagnostique tout en libérant du temps pour le soin des patients. Cette technologie est désormais en service dans plusieurs hôpitaux, tant en Belgique qu’à l’étranger.
Découvrez l'article complet sur Le journal du Médecin : https://lnkd.in/eG7xU-xx

|
Scooped by
Gilbert C FAURE
November 25, 2025 1:23 PM
|
I'm privileged to have spearheaded the scientific content of Thermo Fisher Scientific’s Allergen Encyclopedia over the past years, working closely with leading experts in allergen research.
The latest updates include integration of 300 allergen-specific codes from the WHO International Classification of Diseases 11th Revision (ICD-11) into the Allergen Encyclopedia. This enhancement significantly expands its utility as a resource for allergen-related clinical information.
Grateful to the World Allergy Organization for helping raise awareness of this valuable, continually updated resource.
Luciana Tanno

|
Scooped by
Gilbert C FAURE
November 12, 2025 5:08 AM
|
Very proud to present our November issue. Drug #hypersensitivity reactions (DHRs) constitute a major concern in clinical practice, as they compromise patient safety and restrict the use of essential medications. These immune-mediated adverse drug reactions occur after exposure to therapeutic doses and can manifest with a broad clinical spectrum, ranging from mild cutaneous reactions to severe, potentially fatal conditions.
This issue opens with an editorial by Li et al., highlighting the inaugural EAACI Hong Kong Allergy School where global experts in drug allergy gathered under the theme “East Meets West” to call for harmonized international definitions of drug hypersensitivity and standardized criteria for identifying low-risk penicillin allergy, underscoring the urgent need to reduce mislabelling and advance safe, evidence-based delabelling practices worldwide. Leonardi et al. provide a comprehensive overview of the clinical presentations, diagnostic approaches, and treatment strategies for drug-induced ocular adverse events. Cortellini et al. present data and recommendations on the characteristics of hypersensitivity reactions to antiplatelet drugs and the associated diagnostic procedures, to maximize their safety and effectiveness. Gelincik et al. review current knowledge on the pathomechanisms of hypersensitivity reactions to quinolones, including diagnostic tests and cross-reactivities, and propose a practical diagnostic approach for clinicians. Hutten et al. highlight significant discrepancies between studies on cross-allergy to beta-lactam antibiotics, particularly concerning recommendations for safe alternatives. Labella et al. investigate the utility of direct single-dose drug provocation testing without prior skin testing in adult European patients at low risk of penicillin allergy. Bilgic-Eltan et al. analyze the discrepancies between suspected and confirmed drug hypersensitivity in a well-defined cohort of patients with inborn errors of immunity. Helevä et al. evaluate the benefits of aspirin treatment after desensitization in patients with chronic rhinosinusitis with nasal polyps, asthma, and N-ERD. Goh et al. explore haptenated ligands presented by HLA-A*02:01, characterize the T cell repertoire involved in penicillin-induced reactions in a hypersensitive patient, and investigate whether a dominant penicillin-specific T cell receptor clonotype recognizes haptenated HLA peptides. Bertolotti et al. present the thoroughly documented case of a patient with delayed cross-reactivity to all seven available iodinated contrast media. Cho, Jo, and Park et al. leverage the WHO global pharmacovigilance database to identify the ten drugs most frequently associated with severe cutaneous adverse reactions, providing large-scale epidemiological insights into delayed drug hypersensitivities and contributing to global drug safety. Céspedes and Pérez-Moreno et al. demonstrate that IgG removal enhances…………..
journalallergy.com
|






 Your new post is loading...
Your new post is loading...