Your new post is loading...
 Your new post is loading...

|
Scooped by
Gilbert C FAURE
February 11, 4:11 AM
|
ALLERGIC REACTION
Immunology & Medical Laboratory Science
1. Introduction
An allergic reaction is a common immunological phenomenon encountered in clinical practice. It represents an inappropriate and exaggerated immune response to substances that are ordinarily harmless. While many allergic reactions are mild, some can be severe and life-threatening, emphasizing the importance of understanding their mechanism, diagnosis, and laboratory relevance.
2. Definition
An allergic reaction is an immunologically mediated hypersensitivity response that occurs when a previously sensitized individual is re-exposed to a specific allergen, leading to activation of immune cells and release of inflammatory mediators.
Most allergic reactions are classified as Type I (IgE-mediated) hypersensitivity reactions.
3. Allergens and Routes of Exposure
3.1 Common Allergens
Allergens are substances capable of inducing allergic reactions in susceptible individuals.
•Inhaled allergens: pollen, dust mites, mold spores, animal dander
•Ingested allergens: peanuts, shellfish, eggs, milk, drugs
•Injected allergens: insect stings, injectable drugs, blood products
•Contact allergens: latex, cosmetics, metals (nickel), detergents
3.2 Routes of Entry
•Respiratory tract
•Gastrointestinal tract
•Skin
•Bloodstream
The route of entry influences the clinical presentation.
4. Immunological Mechanism of Allergic Reaction
Allergic reactions occur in two main phases:
4.1 Sensitization Phase (Primary Exposure)
This phase occurs during the first exposure to the allergen and does not produce clinical symptoms.
Steps involved:
1. The allergen enters the body.
2. Antigen-presenting cells (APCs) process the allergen.
3. APCs present the antigen to CD4⁺ T helper (Th2) cells.
4. Th2 cells release cytokines such as IL-4 and IL-13.
5. These cytokines stimulate B cells to produce IgE antibodies.
6. IgE binds to high-affinity FcεRI receptors on mast cells and basophils.
The individual is now sensitized.
4.2 Effector Phase (Re-exposure)
Upon subsequent exposure to the same allergen:
1. The allergen binds to IgE on mast cells.
2. Cross-linking of IgE occurs.
3. Mast cells undergo degranulation.
4. Inflammatory mediators are released, producing clinical symptoms.
5. Chemical Mediators Released
5.1 Pre-formed Mediators
•Histamine: causes vasodilation, itching, edema, and bronchoconstriction
5.2 Newly Synthesized Mediators
•Leukotrienes: bronchoconstriction and mucus secretion
•Prostaglandins: inflammation and pain
•Cytokines: recruit eosinophils and other inflammatory cells
These mediators are responsible for the acute and late-phase reactions.
#MedicalLaboratoryScience
#Immunology
#AllergicReactions
#PatientSafety
#LaboratoryMedicine
#HealthcareEducation
#MLS

|
Scooped by
Gilbert C FAURE
January 8, 4:58 AM
|
💡 𝐖𝐡𝐚𝐭 𝐢𝐟 𝐰𝐞 𝐜𝐨𝐮𝐥𝐝 𝐭𝐞𝐚𝐜𝐡 𝐁 𝐜𝐞𝐥𝐥𝐬 𝐭𝐨 "𝐟𝐨𝐫𝐠𝐞𝐭" 𝐈𝐠𝐄??
📖 In a recent Science Immunology study, long-term allergic memory was mapped 𝐧𝐨𝐭 𝐭𝐨 𝐈𝐠𝐄 cells, but mainly to 𝐈𝐠𝐆𝟏⁺ 𝐦𝐞𝐦𝐨𝐫𝐲 𝐁 𝐜𝐞𝐥𝐥𝐬 with a type-2 imprint, primed to change from IgG1 to IgE when the allergen returns (recall).
🧬 𝐃𝐢𝐬𝐜𝐨𝐯𝐞𝐫𝐢𝐧𝐠 𝐓-𝐩𝐨𝐰𝐞𝐫
🔁 𝐓-𝐜𝐞𝐥𝐥 𝐜𝐲𝐭𝐨𝐤𝐢𝐧𝐞𝐬 as gatekeepers: 𝐈𝐋-𝟒/𝐈𝐋-𝟏𝟑 drive this switch at recall; dampen those cues and IgE recall drops. Notably, exposing these memory B cells to allergen without IL-4 can make them “𝐟𝐨𝐫𝐠𝐞𝐭” 𝐭𝐡𝐞 𝐈𝐠𝐄 𝐩𝐫𝐨𝐠𝐫𝐚𝐦 and default to 𝐈𝐠𝐆, even when IL-4 reappears later.
🧪 𝐋𝐞𝐭’𝐬 𝐥𝐞𝐚𝐫𝐧 (𝐧𝐞𝐮𝐫𝐨)𝐈𝐦𝐦𝐮𝐧𝐨𝐥𝐨𝐠𝐲 — 𝐀𝐥𝐥𝐞𝐫𝐠𝐲 𝐛𝐚𝐬𝐢𝐜𝐬
• 𝐀𝐥𝐥𝐞𝐫𝐠𝐲 = an excessive immune response to a 𝐡𝐚𝐫𝐦𝐥𝐞𝐬𝐬 𝐚𝐧𝐭𝐢𝐠𝐞𝐧 (𝐚𝐥𝐥𝐞𝐫𝐠𝐞𝐧) recognized by 𝐈𝐠𝐄 𝐚𝐧𝐭𝐢𝐛𝐨𝐝𝐢𝐞𝐬.
• 𝐈𝐠𝐄 binds to its high-affinity receptor (𝐅𝐜ε𝐑𝐈) on 𝐦𝐚𝐬𝐭 𝐜𝐞𝐥𝐥𝐬 and 𝐛𝐚𝐬𝐨𝐩𝐡𝐢𝐥𝐬; upon re-exposure, the allergen cross-links IgE → 𝐝𝐞𝐠𝐫𝐚𝐧𝐮𝐥𝐚𝐭𝐢𝐨𝐧 (histamine release…) → hives, wheezing, anaphylaxis.
• 𝐈𝐠𝐆𝟏⁺ 𝐦𝐞𝐦𝐨𝐫𝐲 𝐁 𝐜𝐞𝐥𝐥𝐬 store the “recipe”; with 𝐈𝐋-𝟒/𝐈𝐋-𝟏𝟑 they can 𝐜𝐥𝐚𝐬𝐬-𝐬𝐰𝐢𝐭𝐜𝐡 𝐛𝐚𝐜𝐤 𝐭𝐨 𝐈𝐠𝐄, helping explain relapses.
🧬 𝐂𝐡𝐚𝐥𝐥𝐞𝐧𝐠𝐢𝐧𝐠 𝐭𝐡𝐞 𝐩𝐚𝐫𝐚𝐝𝐢𝐠𝐦: the immune system is not a defense system… it is much more than that.
🔗 𝐑𝐞𝐚𝐝 𝐭𝐡𝐞 𝐩𝐚𝐩𝐞𝐫 𝐢𝐧 𝐒𝐜𝐢𝐞𝐧𝐜𝐞 𝐈𝐦𝐦𝐮𝐧𝐨𝐥𝐨𝐠𝐲: https://lnkd.in/d5zeXDDX
🔖 Save for later. 🔁 Share with your science-curious friends.
#immunology #allergy #IgE #Bcells #IL4 #IL13 #mastcells #ScienceImmunology #ChallengingTheParadigm

|
Scooped by
Gilbert C FAURE
October 2, 2025 2:42 AM
|
✨✨✨ Nous sommes très heureux d’annoncer la publication des résultats de #AllergenChipChallenge dans la prestigieuse revue Journal of Allergy and Clinical Immunology https://lnkd.in/e_Mn4c73
Ce projet est le fruit d’un travail collectif remarquable, qui a rassemblé cliniciens, biologistes, data scientists et chercheurs autour d’un objectif commun : mieux comprendre et interpréter les données issues des puces à allergènes et de générer par #MachineLearning un #algorithme de prédiction des #allergies à partir d'un profil d'IgE et de données cliniques.
La base de données et l'algorithme sont en libre accès au bénéfice de la recherche et des patients allergiques.
Un grand merci 🙏 à Joana Vitte et Pascal Demoly pour avoir initié ce passionnant projet, la Société Française d'Allergologie - SFA, AllergoBioNet, Health Data Hub et Bpifrance pour leur soutien déterminant, ainsi qu’à toutes celles et ceux qui ont contribué à rendre cette aventure possible Guillaume Martinroche Amir Guemari Pol André APOIL Isabella Annesi-Maesano Eric Fromentin @Laurent Guilleminault Davide Caimmi Caroline Klingebiel @Céline Beauvillain Alain Didier Jeremy Corriger Lauriane Armand Agathe Delaune Trustii.io Naama BAK CHU de Bordeaux.
➡️ Ces avancées montrent la puissance de la collaboration et de l’ouverture des données pour faire progresser la recherche en allergologie et au-delà. Le projet continue.
#OpenData #Database #Allergie #Allergologie #Allergy #Immunologie #Recherche #IA #MachineLearning #SFA #GTESIA

|
Scooped by
Gilbert C FAURE
July 19, 2025 8:06 AM
|

|
Scooped by
Gilbert C FAURE
July 7, 2025 5:48 AM
|
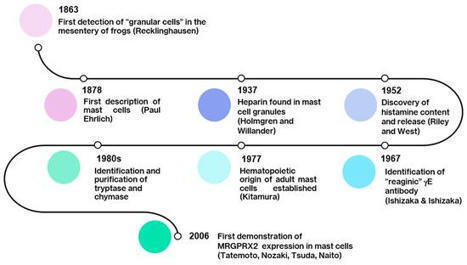
🔬 Et si on arrêtait de réduire les mastocytes à l’IgE ?
Pendant des décennies, la triade « mastocyte - IgE - allergie » a structuré notre compréhension des réactions d’hypersensibilité immédiate.
Mais aujourd’hui, nous savons que cette vision est incomplète.
📌 L’article-clé paru en janvier 2025 (Int J Mol Sci. 26(3):927) montre que les mastocytes (MC) disposent d’un répertoire de récepteurs bien plus vaste que FcεRI, et que leur activation peut suivre des voies non-IgE, dites "pseudoallergiques", via des récepteurs comme MRGPRX2.
💥 Résultat ?
➡️ Des réactions cliniques rapides, sans sensibilisation préalable ni IgE spécifique détectable.
➡️ Une dégranulation induite par des médicaments (fluoroquinolones, vancomycine, morphine...), des neuropeptides (substance P), ou des stimuli physiques.
➡️ Une inflammation neurogène amplifiée par l’interaction étroite entre MC et terminaisons nerveuses périphériques.
🧠 Les implications dépassent largement le champ allergologique classique :
- Urticaire chronique, dermatite atopique, prurit rebelle
- Syndrome d’activation mastocytaire (MCAS)
- Rosacée, asthme non contrôlé, inflammation cérébrale...
💡Comprendre MRGPRX2, c’est élargir notre cadre diagnostique et thérapeutique.
👉 De nouveaux traitements ciblent déjà cette voie : antagonistes de MRGPRX2, cannabinoïdes non-psychoactifs (PEA, CBD), anticorps anti-Siglec-8...
🧬 Les mastocytes sont bien plus que des effecteurs allergiques.
Ils sont au carrefour de l’immunité, du système nerveux et des interfaces barrière.
Et si l’on actualisait nos réflexes cliniques ?
Source : https://lnkd.in/etTeyKBh
Dr Lucie WETCHOKO

|
Scooped by
Gilbert C FAURE
October 16, 2024 10:11 AM
|
Comparable production of IL-4 by both TFR and TFH cells. A helper role for TFR cells in food allergy was previously demonstrated with the use of TFR cell–deficient Foxp3CreBcl6fl/fl (Bcl6FC) mice (18).

|
Scooped by
Gilbert C FAURE
April 18, 2023 12:06 PM
|
Basophils bind IgE via FceRI-alpha beta gamma 2, which they uniquely share only with mast cells. In doing so, they can rapidly release mediators that are hallmark of allergic disease. This fundamental similarity, along with some morphological features shared by the two cell types, has long brought into question the biological significance that basophils mediate beyond that of mast cells. Unlike mast cells, which mature and reside in tissues, basophils are released into circulation from the bone marrow (constituting 1% of leukocytes), only to infiltrate tissues under specific inflammatory conditions. Evidence is emerging that basophils mediate non-redundant roles in allergic disease and, unsuspectingly, are implicated in a variety of other pathologies [e.g., myocardial infarction, autoimmunity, chronic obstructive pulmonary disease, fibrosis, cancer, etc.]. Recent findings strengthen the notion that these cells mediate protection from parasitic infections, whereas related studies implicate basophils promoting wound healing. Central to these functions is the substantial evidence that human and mouse basophils are increasingly implicated as important sources of IL-4 and IL-13. Nonetheless, much remains unclear regarding the role of basophils in pathology vs. homeostasis. In this review, we discuss the dichotomous (protective and/or harmful) roles of basophils in a wide spectrum of non-allergic disorders.

|
Scooped by
Gilbert C FAURE
October 12, 2022 10:44 AM
|
In this study, researchers identified significant practice variations in management & diagnosis of FPIAP among pediatric gastroenterologists and immunologists.

|
Scooped by
Gilbert C FAURE
February 1, 2022 5:28 AM
|
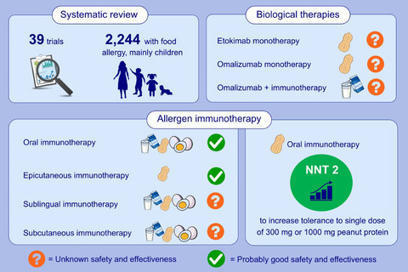
We systematically reviewed 39 randomized controlled trials about allergen-specific immunotherapy and/or biologicals in 2244 people with IgE-mediated food allergy, mostly children. We found that ora

|
Scooped by
Gilbert C FAURE
July 12, 2021 1:38 PM
|
The first molecular structures of allergens were identified more than 30 years ago, and characterised recombinant allergens became available. We evaluate the current state of the art in molecular AIT with the purpose of understanding why progress in this field has been modest, despite the fact that there is enormous promise for treatment and allergen-specific prevention. Several AIT techniques have been developed and are being tested in clinical trials based on allergen structures. In clinical AIT trials, promising results were obtained with recombinant and synthetic allergen derivatives inducing allergen-specific IgG antibodies, which interfered with allergen recognition by IgE, whereas clinical efficacy for approaches targeting only allergen-specific T-cell responses could not yet be demonstrated. According to the available research, molecular AIT techniques have significant advantages over allergen extract-based AIT. Clinical trials show that recombinant allergen-based AIT vaccines that outperform existing allergen extract-based AIT vaccines for respiratory, food, and venom allergy can be created. Allergen-specific preventative techniques based on recombinant allergen-based vaccine methods and T-cell tolerance induction are on the horizon and hold the promise of allergy prevention. However, progress is hampered by a shortage of resources for clinical trials, which are required for the development of these novel therapies. For latest news and updates By signing up, you will receive emails about Physician's Weekly products and you agree to our Terms & Conditions and Privacy Policy. Reference: https://journals.lww.com/co-allergy/Fulltext/2019/08000/Recombinant_allergens_for_immunotherapy__state_of.20.aspx

|
Scooped by
Gilbert C FAURE
December 13, 2020 2:17 PM
|
The term anaphylaxis refers to a systemic immediate hypersensitivity reaction caused
by the rapid, IgE-mediated immune release of potent mediators from tissue mast cells
and peripheral blood basophils.

|
Scooped by
Gilbert C FAURE
September 16, 2020 1:30 AM
|
Alpha-gal Syndrome (AGS) is a unique allergy to non-primate mammalian meat (and derived-products) that is associated with tick bites and is due to a specific IgE antibody to the oligosaccharide gal...

|
Scooped by
Gilbert C FAURE
May 24, 2020 11:57 AM
|
Abstract Background A few studies have investigated the antecedents and outcomes of infants who demonstrate IgE sensitization to foods that they clinically tolerate. Improved understanding of this ...
|

|
Scooped by
Gilbert C FAURE
February 11, 4:07 AM
|
Is IgE really just the antibody of allergy — or a core pillar of human immunity?
A seminal review in Frontiers in Immunology challenges the idea that IgE is merely pathologic. Instead, it argues that IgE evolved as a protective immune mechanism against multicellular parasites, particularly helminths — with major implications for immune-compromised patients.
Key insights:
• IgE-driven Th2 responses are physiologic in helminth infection, not aberrant
• Most environmental allergens belong to the same protein families targeted during parasitic infection
• Parasite-specific IgE correlates with resistance to reinfection in schistosomiasis, hookworm, and ascariasis
• Helminths actively regulate host immunity, shaping tolerance via IL-10, TGF-β, and IgG4
Why this matters in immune-compromised states
In conditions such as advanced HIV, malignancy, chemotherapy, or immunosuppressive therapy:
• IgE responses may dominate as other immune pathways fail
• Cross-reactive IgE can mimic allergy, malignancy, or autoimmune disease
• Loss of regulatory balance may convert protective IgE into clinically significant inflammation
• Atypical eosinophilia, tissue infiltration, or mass-like immune phenomena may result
This framework helps explain why immune-compromised patients often present with non-classic, confusing inflammatory patterns — and why parasite-derived antigens can be protective in healthy hosts yet harmful in immune-dysregulated ones.
Takeaway:
IgE may represent an ancient survival system that becomes maladaptive only when immune regulation breaks down. Understanding this axis is critical for allergy, parasitology, vaccine development — and modern clinical immunology.
📄 Helminth allergens, parasite-specific IgE, and its protective role in human immunity (Frontiers in Immunology)
Authors:
Colin Matthew Fitzsimmons • Franco Harald Falcone • David William Dunne
(University of Cambridge | University of Nottingham)
#Immunology #IgE #Immunocompromised #ClinicalImmunology #Allergy #Parasitology #TranslationalMedicine #GlobalHealth

|
Scooped by
Gilbert C FAURE
January 4, 12:57 PM
|
Allergies alimentaires : de grandes disparités à l’échelle mondiale
L’article proposé par la WAO Sur un projet international mené auprès de 150 centres dans 50 pays met en évidence de grandes différences dans la prise en charge des allergies alimentaires selon les pays,que ce soit dans les possibilités diagnostiques ou le prix des traitements d’urgence .
-Le test cutané est utilisé mais certaines régions d’Afrique et d’Asie y ont un accès inégal .
- les IgE spécifiques, souvent utilisées en alternative.
-L’immunothérapie orale est surtout pratiquée en Europe occidentale, puis en Amérique du Nord, en Europe du Sud et en Europe du Nord. L’omalizumab est également utilisé notamment en Europe occidentale, en Amérique du Nord, en Asie de l’Est et en Océanie.
-La sévérité des réactions varie fortement selon les zones géographiques.
L’utilisation d’adrénaline va de 3 % en Asie du Sud à 50 % en Afrique australe, avec des taux importants en Asie de l’Est, en Asie occidentale, en Europe du Sud et en Amérique du Nord. La disponibilité de l’adrénaline elle-même est très variable selon les pays, et certains n’y ont pas accès aux auto‑injecteurs,
Allergènes :Avant 5 ans, le lait et l’œuf sont les allergènes les plus fréquents. Entre 5 et 11 ans, l’œuf >du lait, >l’arachide et des fruits à coque. Chez les adolescents, l’arachide le plus courant au niveau mondial, suivie des noix et des crustacés. Chez les adultes, les crustacés, les noix, l’arachide et le poisson sont les allergènes les plus souvent rapportés,
Ces résultats montrent que les allergies alimentaires représentent un enjeu mondial majeur, influencé par l’accès aux diagnostics, aux traitements, aux auto‑injecteurs d’adrénaline et aux soins d’urgence. Selon l’outil DEFASE, environ 3 % des patients pourraient être classés comme souffrant d’allergies alimentaires sévères, un taux comparable à celui observé dans l’asthme sévère réfractaire.
https://lnkd.in/ebF3d252
Cet article est très intéressant et engage à comparer les prix dans différents pays :
les tarifs hors assurance sont d’environ 1 000 à 3 000 dollars pour une admission aux urgences aux États‑Unis et 3 000 à 10 000 dollars pour une journée en soins intensifs, alors qu’en Thaïlande une journée de soins intensifs coûte hors assurance 900 à 2 700 euros, tandis qu’en France les coûts hospitaliers sont beaucoup plus faibles grâce à la prise en charge publique, mais peuvent devenir élevés pour les personnes sans aucune assurance
Aux USA les prix vont de 199 dollars pour le nouveau spray nasal d’adrenaline à près de 300 dollars pour le système parlant injectable. Et 600 euros pour le plus connu ( tarifs hors assurance ) En France il faut compter entre environ 62 et 91 euros pour deux dispositifs . , l’Assurance maladie rembourse 65 % du prix des auto‑injecteurs d’adrénaline et, dans la plupart des cas, les complémentaires santé prennent en charge le reste du coût.

|
Scooped by
Gilbert C FAURE
August 7, 2025 3:35 AM
|
"A blog about allergy, asthma & immunology"

|
Scooped by
Gilbert C FAURE
July 8, 2025 8:34 AM
|
8th July is World Allergy Day.
This article in Times Of India mentioned about our old study: Allergic diseases have significant impact on the quality-of-life, social life, and economy. Inadequate knowledge about allergic testing further add on to the burden of the disease. Reposting this for awareness about harmonisation of allergens testing.
The clinical suspicion of allergic sensitization can be confirmed by demonstrating the presence of allergen specific immunoglobulin-E (IgE) antibodies in vivo (skin prick test) or in vitro methods (Blood tests: FEIA, ELISA, CRD etc). There is a lack of well-defined protocols and guidelines for the diagnosis of respiratory allergy testing in India. Therefore, the evidence-based guidelines is the need of the hour.

|
Scooped by
Gilbert C FAURE
June 12, 2025 11:14 AM
|
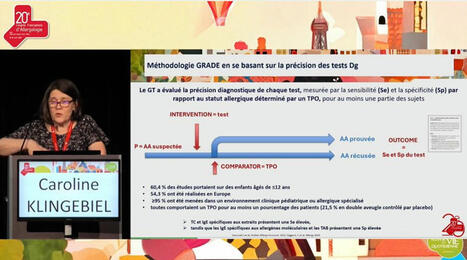
On behalf of the Allergy Diagnosis Working Group Of the French Society of Allergology (GTBA – SFA), I’m proud to have contributed to the dissemination of the EAACI guidelines on the diagnosis of IgE-mediated Food Allergy within the French-speaking medical community:
- French translation of the food allergy guidelines on diagnosis for a special issue of the French Allergy Journal (RFA) dedicated to Food Allergy: https://lnkd.in/dBAxRQXC
- Plenary presentation at the French National Congress of Allergology (CFA 2025) in Paris with a focus on methodology based on the accuracy of diagnostic tests to understand the recommended diagnostic approach: https://lnkd.in/dGAEc7PK
- Presentation at a workshop/controversy at the 30th National Congress of AMAFORCAL in Rabat, Morocco
Julien Goret, Joana Vitte, Alexandra Santos, MD PhD, Société Française d'Allergologie - SFA, European Academy of Allergy and Clinical Immunology - EAACI, @GTBA, Youness EL GUEDDARI, Elleni-Sofia Vaia

|
Scooped by
Gilbert C FAURE
September 8, 2024 11:47 AM
|

|
Scooped by
Gilbert C FAURE
March 9, 2023 7:53 AM
|
Un consortium international (*), comprenant le laboratoire de génétique humaine des maladies infectieuses, à l’Institut Imagine (Inserm, APHP, Université Paris Cité), vient de publier une nouvelle étude dans la revue Journal of Experimental Medicine. Les médecins et chercheurs ont identifié un nouveau gène en cause dans le syndrome « hyper IgE », responsable d’allergies et d’eczéma sévères.

|
Scooped by
Gilbert C FAURE
July 25, 2022 8:38 AM
|
All shrimp oral challenge test (OCT)-positive patients were positive for IgE against Der p 10.The level of anti-Der p 10 IgE >1.2 kUA/mL had the best diagnostic performance (sensitivity 100%, specificity 65%) Conclusion: Anti-Der p 10 IgE is useful for predicting shrimp allergy diagnosis and cou ...

|
Scooped by
Gilbert C FAURE
December 27, 2021 10:47 AM
|
The introduction of novel food products could expose the population to new dietary proteins. Assessing the potential allergenicity of these proteins is essential to their safe introduction, but remains a challenge.The activity is focusing on establishing the way different types of methodologies can be deployed to achieve a quantitative or semi-quantitative assessment of the risk posed by protein sources. The recently developed Adverse Outcome Pathway for IgE-mediated sensitisation in particular, is considered.

|
Scooped by
Gilbert C FAURE
May 24, 2021 11:20 AM
|
Abstract Background Atopic diseases are an increasing problem that involve both immediate hypersensitivity reactions mediated by IgE and unique cellular inflammation. Many forms of specific immunot...

|
Scooped by
Gilbert C FAURE
December 13, 2020 2:17 PM
|
Our study suggests that the mast cell activation test can be used to diagnose IgE/FcεRI-dependent immediate drug hypersensitivity reactions.It also shows potential to assess the clinical relevance of drug-specific IgE antibodies in their ability to elicit mast cell degranulation, and therefore disc...

|
Scooped by
Gilbert C FAURE
September 12, 2020 4:20 AM
|
Morning Session Morning Chair: Dr Tom Marrs 09:00 Welcome and Introduction Dr Tom Marrs Consultant in Paediatric Allergy St Thomas' Hospital, London 09:10 Remote managment of eczema and urticaria in primary care Dr Alya Abdul-Wahab Consultant Dermatologist St George's Hospital, London 09:50 How to fix common gastro-intestinal symptoms in children Dr Rakesh Vora Paediatric Gastroenterology Consultant St Thomas' Hospital, London 10:35 << BREAK >> 11:00 How to manage IgE and non-IgE food allergies Dr Tom Marrs Consultant in Paediatric Allergy St Thomas' Hospital, London 11:40 How to recomment avoidance of egg and nuts Rebecca Brocklehurst Paediatric Allergy Dietitian St Thomas' Hospital, London 12:20 << LUNCH >> Afternoon Session Afternoon Chair: Dr Rosy Wells 13:00 Preventing food allergy: what to tell parents Dr Michael Perkin Consultant Allergist and Reader in Clinical Epidemiology St George's Hospital, London 13:30 Priorities to Tell Families Living With Food Allergy Professor Adam Fox Professor in Paediatric Allergy St Thomas' Hospital, London 14:00 QUICK FIRE: Adrenaline auto-injector guide IN PRACTICE: Spare pens in schools Alia Boardman Clinical Nurse Specialst in Paediatric Allergy St George's Hospital, London 14:30 << BREAK >> 15:00 Managing Long-Term Asthma in a Virtual World Dr Richard Iles Paediatric Respirology Consultant St Thomas' Hospital, London 15:40 How to recognise and treat allergic rhinitis Dr Anne Chsitopher Consultant Paediatrician and Allergist St George's Hospital, London 16:10 New inhalers and nasal sprays Katherine Knight Clinical Nurse Specialist in Paediatric Allergy St Thomas' Hospital, London 16:40 Webinar feedback and Close of meeting
|




 Your new post is loading...
Your new post is loading...