 Your new post is loading...

|
Scooped by
rob halkes
January 10, 2014 1:43 PM
|
MDU adviser Dr Caroline Fryar answers common GP questions on gaining and recording patient consent GPs can leave themselves vulnerable to criticism if they fail to take proper consent, or fail to properly record the consent process. In order to properly consent to treatment, patients must be given enough information to make an informed choice, so the explanation given to and understood by the patient is crucial. Here we address some of the common questions GPs ask about obtaining valid consent, providing information about risks and getting consent from patients who lack capacity. E.g.: - How can I ensure consent is valid? The GMC makes it clear in its publication Consent: doctors and patients making decisions together (2008) that it is the responsibility of the doctor undertaking the investigation or providing the treatment to discuss it with the patient. This means explaining to patients in non-technical language the nature, purpose and risks of the proposed procedure. If the treatment is difficult to understand, it may be helpful for you to use drawings, diagrams and models. If necessary, an interpreter should be there to make sure the explanation is given in a language the patient understands. You may ask patients to sign a consent form for certain procedures such as minor surgery, but this is of secondary importance to the consent discussion, although it may be useful evidence if a complaint or claim arises. - Do I have to get consent for every procedure? - At what point should I get consent? - Who can obtain consent? - What is the medico-legal definition of consent? - What risks do you need to warn the patient about?
- How can I help patients to make a decision? Should a GP try to make it easier for patients to make decisions for their care, e.g by using simple language?
- HOw can I asess whether the patient has capacity? ... etc.etc...

|
Scooped by
rob halkes
January 7, 2014 5:24 AM
|
Research from European respiraotiry journal 2009, by Koff, P.B. a.o. Abstract Self-management strategies improve a variety of health-related outcomes for patients with chronic obstructive pulmonary disease (COPD). These strategies, however, are primarily designed to improve chronic disease management and have not focused on early detection and early treatment of exacerbations. In COPD, the majority of exacerbations go unreported and treatment is frequently delayed, resulting in worsened outcomes. Therefore, a randomised clinical trial was designed to determine whether integration of self-management education with proactive remote disease monitoring would improve health-related outcomes. A total of 40 Global Initiative for Chronic Obstructive Lung Disease stage 3 or 4 COPD patients were randomised to receive proactive integrated care (PIC) or usual care (UC) over a 3-month period. The primary and secondary outcomes were change in quality of life, measured by the St George’s Respiratory Questionnaire (SGRQ), and change in healthcare costs. PIC dramatically improved SGRQ by 10.3 units, compared to 0.6 units in the UC group. Healthcare costs declined in the PIC group by US$1,401, compared with an increase of US$1,709 in the UC group, but this was not statistically significant. PIC uncovered nine exacerbations, seven of which were unreported. Therefore, proactive integrated care has the potential to improve outcomes in chronic obstructive pulmonary disease patients through effects of self-management, as well as early detection and treatment of exacerbations.

|
Scooped by
rob halkes
November 21, 2013 8:13 AM
|
Das Patientenrechtegesetz: Rechtliche Hinweise und Empfehlungen für Ärzte und Psychotherapeuten Das Patientenrechtegesetz ist seit Februar 2013 in Kraft. Die Einführung der neuen Paragrafen 630a bis 630h des Bürgerlichen Gesetzbuches (BGB) war bundesweit Thema in den Medien. Trotzdem wirft das Gesetz immer wieder Fragen auf: Welche zusätzlichen Pflichten haben niedergelassene Ärzte und Psychotherapeuten jetzt beim Dokumentieren der Behandlung? Dürfen Pati- enten auch außerhalb der Sprechzeiten Einsicht in ihre Akte verlangen? Wie viel kann für eine Kopie in Rechnung gestellt werden? Wer darf die Akte ei- nes verstorbenen Patienten einsehen? – Mit diesen und ähnlichen Anfragen können auch Sie jetzt verstärkt konfrontiert sein.
The Law on Patients' rioghts in Germany: Legal guidelines and advices for physicians and fysiotherapists. The law on patients' rigths is set in force since February 2013. The introduction of new paragraphs 630a to 630h of the citizens rights book has been an issue in the several states of Germany. Nevertheless, the law raises ever new questions: what new obligations are added now to the "niedergelassene" physicians ans physiotherapists regarding documentation of their treatments? Can patients have also right of view/inspection of their records outside of consultation times? How much could one charge for copies of records? Who could see the records of a deceased patient? You could be confronted with such questions as well. ...
Read further, but in German

|
Scooped by
rob halkes
November 14, 2013 7:38 AM
|
I can’t think of any strategic initiative in recent time with more potential to engage and active patients, improve patient health outcomes and enhance patient experiences than the call by the Institute of Medicine in Crossing the Quality Chasmfor providers to become more patient-centered. Specifically, more patient-centered in the way they communicate with patients. Having spent years working in the field, I am continually amazed at the rich body of evidence documenting the wide range of strategic benefits of engaging patients in conversations about their health goals, beliefs, motivations and expectations. I am also amazed at how slow health plans, hospitals systems and the like have been to leverage the benefits of patient-centered communications within their provider networks. A 2011 article in BMJ’s journal Quality and Safety highlight the present state of affairs with respect to patient-centered communications in the U.S. The study looked at how often physicians employed the most essential and defining patient-centered communication skill – asking patients about what they expected from their health encounter. In the case of the study, asking patients what they expected from a required hospital stay…although the finding could just as easily come from a study of physician office visits.
Why Is Understanding The Patient’s Expectations Important?
The basic premise of patient-centered care is that, where practicable, the clinician should honor the patient’s beliefs, motivations fears and expectations in the course of treating them. Obviously before you can “honor” the patient’s “perspective” you first need to understand what they are. The clinician needs to ask the patient.
And there’s the rub. Turns out that only 16% of physicians in the study (residents and attending physicians) admitted to routinely asking their patients about their health care-related expectations. ...
Read on!

|
Rescooped by
rob halkes
from Health Care Business
October 16, 2013 6:52 AM
|
Publication Date: August 12, 2009 In its new research brief, "Thinking Outside the Pillbox," NEHI addresses the root causes of poor patient medication adherence - a significant contributor to overall health care waste - and offers promising solutions to improve adherence, particularly among chronic disease patients. See pdf of full report

|
Scooped by
rob halkes
October 14, 2013 12:19 PM
|
Health engagement online deepening at a time when consumers are expected to take a greater role in their care October 10, 2013, New York, NY – Consumers have long used health websites and other online tools to gather information about conditions and treatments. Now they are broadening their health activity online, using Internet resources to support healthcare decision-making and to manage conditions, a new study shows. Forty-five percent of online U.S. adults with a chronic condition say that the Internet is essential to managing their disease or condition, according to the Cybercitizen Health® U.S. 2013 study from healthcare market research and advisory firm Manhattan Research. “We’ve hit an inflection point in the way consumers use the internet for health,” said Rory Stanton, Consumer Insights Analyst at Manhattan Research. “They are going beyond seeking-information to using tools and services to manage the day-to-day aspects of care. That’s good news in this post–healthcare reform environment, in which digital engagement of consumers for example via patient portals and telehealth will be a key to success.” The study also found that online content and services influence how consumers approach health management for themselves and their dependents, with 44 percent of online consumers agreeing that the Internet is essential for their health and medical decision-making. These and other study findings highlight key opportunities for various health stakeholders, such as pharmaceutical companies, provider networks, and payers, to provide technology-based value added services and empower deeper engagement from end users.

|
Scooped by
rob halkes
October 8, 2013 12:40 PM
|
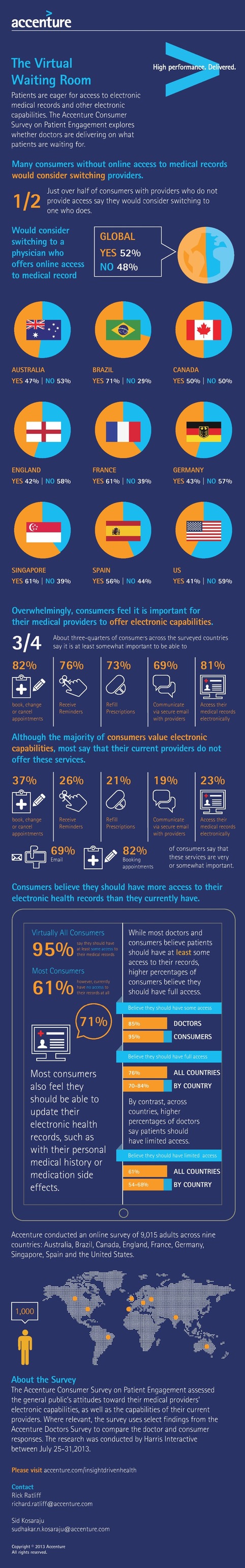
84 percent of US consumers believe they should have full access to their electronic medical records while only a third of physicians (34 percent) share this belief, according to an Accenture survey.

|
Scooped by
rob halkes
September 12, 2013 4:43 AM
|
A story from blogger Leslie, pointing out what consequences a bad policy of caregivers about their giving access to patietns' records. Thier image will suffer. While, patients as in most countries in Europe and in the US do have the principle right to view what's in them; See also here: http://epatientdave.com/2013/07/19/you-can-ask-to-see-or-get-a-copy-of-your-medical-record-other-health-information/#comment-261333 Here's her story: What Happens When Your Medical Records Aren’t Yours?You get a bill for $361.26. I almost had a heart attack. And then I burst into tears. And then I got pretty freakin’ pissed off. For that price, I could pay for 18 appointment co-pays with my current insurance.I could do a lot with that kind of money, but I cannot afford to pay that for my medical records. I wanted my medical records because I am moving. And how was I supposed to know that my medical records over the past five years would be six inches thick, more than 1,000 pages? When I got home one night a few weeks ago and saw a box from a health company in Atlanta, I figured surely that couldn’t be my medical records. Then I picked up the box and it was heavy to the point where I knew it probably was. And before I even saw the bill, I had a sinking feeling in my stomach. I feel like I am being punished because I have a complicated medical history. It’s insane to me that these people look at this six-inch thick medical record of a 27-year-old, and rather than wonder what my life might be like as it is, they stick it to me even more.And I was under the impression that if I was going to be charged more than $50, I would be contacted before they went ahead with processing my request. That never happened. Because if it had, I wouldn’t have been willing or able to pay that much. The other thing is that I poured through every page and found nearly 350 pages that were blank, only had the hospital logo on them, or only had the line about “electronic mail not being secure”. There were 1,202 pages at 0.23 each. I accounted for those, which included the 350 garbage ones I just mentioned. But then there were 20 pages at $1.16 each and 30 pages at 0.58 each. I couldn’t account for those. But the real question is, besides how I was going to pay the bill is how can I be a responsible patient if my medical records are in Michigan and I’m in New York? How is it possible that I have to pay for my own medical record?....
Using Focus Groups and Feedback Sessions to Develop an Interactive, Web-Based Self-Management Intervention for Chronic Pain Marie Ennis-O'Connor added in her scoopit: The results of this study suggest the potential value of self-management for chronic pain patients and the potential acceptability of web-based delivery of intervention content. Focus group and feedback methodologies highlight the usefulness of including potential program users in intervention development.
Via Marie Ennis-O'Connor

|
Scooped by
rob halkes
July 22, 2013 4:52 AM
|
Pharmacy data show great variations in the rates at which people stick to drug regimens for diabetes, depression and other illnesses. The degree to which Americans with chronic conditions take their medications as prescribed differs widely according to the state where they live, the conditions they have and their type of insurance coverage. Those are the findings of a recent report based on 2012 data from the 60 million customers of CVS Caremark Corp.'s pharmacy benefit management program, which serves consumers covered by self-insured employers, private health plans and Medicare Part D. The CVS report breaks down drug adherence by state, condition and coverage on metrics such as medication possession ratio, which is based on dispensing records to show what percentage of a yearlong period patients had their prescriptions on hand to take. The data show wide variations in drug adherence.. Experts define an 80% medication possession ratio as optimal in terms of ensuring that patients are able to get the adequate clinical effect from their medicines. The report found similarly big gaps in the overall rates of adherence according to that definition. Drug noncompliance not only contributes to worse health outcomes, but raises costs. The central question is how to make a significant dent in drug noncompliance, a puzzle that has challenged physicians, pharmacists and researchers for years. Earlier research has found that time-squeezed physicians have trouble spotting noncompliant patients, educating them about the impact of adherence on outcomes and helping them overcome barriers such as high out-of-pocket costs and low health literacy....

|
Scooped by
rob halkes
July 22, 2013 4:03 AM
|
I am a big fan of Infographics. They are a great for turning otherwise complex data into practical information. Here's an Infographic I built to describe the "disconnect" that often occurs between physicians and patients and the impact of adherence...

|
Scooped by
rob halkes
May 21, 2013 3:27 PM
|
Vervloet, M.
Have you taken your medication yet? The effectiveness of electronic reminders = Heeft u uw medicijnen al ingenomen? De effectiviteit van elektronische herinneringen. Utrecht, NIVEL, 2013 Dutch article of recent published thesis by M. Vervloet. The medication Box automatically monitors when a drug is taken: RTMM: Real Time Medication Monitoring, through a central server. The patient can be remembered about his/her medication through severla methods; texting etc. They appear to like this (although there was a small number of patients). But this is a great step to knwo how we can help/support patients. The (Dutch/ English) summary of the thesis can be downloaded at the same site page. Research enabled by the Dutch ministry.
The Empowered Patient® Decision Support web app is a series of ten questions that help identify areas in which patients may need help and support when making health care decisions. The app produces a streamlined pdf report of areas where the patient feels confident and decisive – and areas in which the patient may need information and guidance.
Via Marie Ennis-O'Connor

|
Scooped by
rob halkes
May 7, 2013 3:40 AM
|
Most patients are interrupted by their physicians after 18 seconds… yes 18 seconds. Well, that isn’t going to cut it anymore. Patients are individuals. They have differing ideologies, values, goals, pain thresholds, lifestyles, and few patients react the same way to the same disease process. Enter the days of Informed Decision Making … Poor communication and poor listening skills are likely at the heart of this emerging high tech-low touch method of treating patients these days. In these days of medical data overload, it is becoming far too easy to order and treat a lab test or MRI, as opposed to treating a patient as a person. Each injury has its own “personality”. That means that an ACL tear in a couch potato who slipped picking up their newspaper probably needs to be treated differently than a patient of the same age who exercises twice a day and plays every sports under the sun. Yet, of all the second opinions I am seeing that doesn’t seem to be the case. In most cases patients are being told – “your MRI showed this and you need that”… Incorporating the art of informed decision making into your daily workflow means you need to listen to your patient. You need to dive deep into their own ideologies, values and goals that will shape their decision when presented with the alternatives available. Your are a coach, you are part of a team that will arrive at the right choice for that patient at this particular time. You will need to listen for more than 18 seconds … and you will need to learn to treat patients as people and not as a disease state or an MRI finding. Physicians feel rushed because they’re trying to maintain their income as their reimbursements decline and they need to spend more time filling out reams of paperwork to justify many of their requests or actions. We need to adjust to this new reality without putting our patients health at risk… or without recommending a procedure that someone clearly doesn’t need. In a recent NY Times piece.. The author, Seth Horowitz points out .. Listening is a skill that we’re in danger of losing in a world of digital distraction and information overload. “You never listen” is not just the complaint of a problematic relationship, it has also become an epidemic in a world that is exchanging convenience for content, speed for meaning. The richness of life doesn’t lie in the loudness and the beat, but in the timbres and the variations that you can discern if you simply pay attention. Embracing the art of listening will lead to better treatment decisions, better resource utilization, fewer medical errors, a happier more engaged patient base and hopefully a physician who once again can enjoy the non-monetary rewards of a career in medicine.
The Centre for Patient Leadership (CPL) provides learning and support for a new generation of healthcare leaders – Patient Leaders. Now more than ever, the NHS needs new leaders and innovative solutions. But patients, service users and carers are seen as part of the problem and remain a huge untapped asset. It’s time to shift our thinking. When patients lead and manage their own health and well-being and when they develop the confidence and skills to lead and influence others, something special takes place! Positive change happens, new solutions arrive and collaborative systems of healthcare emerge.
Via Giuseppe Fattori, Géraldine GOULINET FITE, Lionel Reichardt / le Pharmageek

|
Scooped by
rob halkes
May 3, 2013 1:00 PM
|
The boundaries between the physician – patient relationship have always been difficult as the relationship is based on trust, intimacy and the ability to share information from both sides of the desk. This relationship has grown more complex due to the rise of social media engagement. Physicians are being friend-ed, followed and reviewed across the digital channel like crazy, placing the doctors that care for them in difficult positions regarding the confidentiality of their patients who often don’t think about the impact of their digital-buddy request. Similarly, due to the ease of digital communications, the commonly time-stretched doctor also faces temptation to use quick communication methods to reach their audience, in lieu of a more professional path. No-one really wants their test results Tweeted to them! These examples of digital doctoring to be avoided are covered in the guidance. Protecting patient privacy and confidentiality is stressed as the main area for focus when using social media. In order to help doctors better understand digital communication best practices and to fill a gap than many medical practice management efforts have neglected, about a week ago, the American College of Physicians (ACP) and Federation of State Medical Boards (FSMB) published a policy paper entitled“Online Medical Professionalism: Patient and Public Relationships.” Some of the highlights from this publication can be found in this helpful table

|
Scooped by
rob halkes
May 1, 2013 4:15 PM
|
The “digital exhaust” from your mobile phones and other devices could give doctors a valuable window into your wellbeing. Big data may be a rising star in health care but small data can play a powerful role, too. At the TEDMED conference on Wednesday, Deborah Estrin, a computer science professor at New York City’s Cornell Tech, gave a compelling case for how your “digital exhaust,” including location data, searches and social media posts, could provide a valuable window into your wellbeing. “We’re continuously generating digital breadcrumbs from the services we interact with,” she said. But “there are no existing vehicles that package that data about me in a format that’s useful for me and that make it accessible to me. [And] there should be because there’s a lot that I can learn about my personal health from my digital behavior.”... But Estrin wants to encourage an entire ecosystem of apps. And, along with colleagues at the mobile health non-profit OpenM Health and Cornell Tech, she’s beginning to build prototypes that demonstrate the benefits of using small data for personal health, as well as create the architecture for service providers, app developers and others to create additional small data health apps and algorithms. (You can learn more about Cornell’s small data initiative here.) “We need an open architecture, so that a rich market of apps and services can grow up around that data just like http created the World Wide Web and led to the rich array of internet services,” she said.

|
Scooped by
rob halkes
April 26, 2013 1:49 PM
|
Prior to a discussion about the use of social media by nurses and midwives, thoughts on where the lines should be drawn. Maintaining clear and appropriate boundaries in the world of social media can be a real challenge for patients and the health professionals who care for them. Advice from the Nursing and Midwifery Council issued last year warned that nurses and midwives must not overstep those boundaries by sharing confidential information, distributing images taken in clinical environments or pursuing personal relationships with patients online. Similar advice for doctors followed, and other regulators are taking action on a subject that concerns patients, health professionals and their employers. But while this advice has been helpful in clarifying expectations of appropriate behaviour, and allowing regulators to take action when boundaries are breached, it may have left health professionals with the impression that any online engagement with their patients is simply wrong. An event run by the NMC as part of this year's social media week brings together bloggers, tweeters and digital enthusiasts from both sides of the patient-professional divide, to see where the boundaries should be drawn

|
Scooped by
rob halkes
April 9, 2013 5:08 AM
|
Obtaining and documenting informed patient consent prior to surgery is of vital importance, but both the process and documentation of consent can be inadequate. Today at the annual meeting of the American Association of Neurological Surgeons in San Francisco, physicians from the University of Pittsburgh Medical Center reported on a study of a procedure-based consent form they have developed to enhance and improve this process. “Appropriate physician conduct in medical/legal matters begins with the informed consent process. This leads to an understanding of the patient’s diagnosis, the planned procedure, the therapeutic alternatives – both medical and surgical, and the inherent procedural risks,” reported Douglas Kondziolka, M.D., Peter J. Jannetta Professor and vice-chairman of neurological surgery, and professor of radiation oncology at the University of Pittsburgh School of Medicine. “It has been argued that most surgeons do not devote appropriate importance to informed consent in their daily duties. The patient consent procedure we developed facilitates patient discussion and we validated this process by surveying our patients on various elements of the consent process.” In the study, 120 consecutive patients were evaluated.... .. “The practice-specific consent form we developed is modular and simple to use. Because it is written as a check list, it aids the surgeon in discussing each issue with the patient so that all of the important topics are covered,” Dr. Kondziolka said. “Our study involved questions asked in an open-ended format, but the patients had a finite list of items to recall. A secretary, with no medical background or pretenses, administered the questionnaire. In this way, we avoided the potential pitfall of having a physician misrepresent any portion of the informed consent process. We believe this method to obtain and document informed consent should be considered for use by physicians.”

|
Scooped by
rob halkes
April 9, 2013 4:16 AM
|
Our new set of infographics considers how patients and service users will use technology and data to become more active in their care.
These infographics are for you to use and share – please just mention The King's Fund when you do so.

|
Scooped by
rob halkes
April 9, 2013 4:00 AM
|
12 Ways to Improve the Healthcare User Experience ( Industry Verticals ) Technology is a great way to engage patients in managing their health, but poor design--whether it's a bad interface or an app that doesn't meet patients' needs--often stands in the way. These 12 tips will help designers and developers improve the user experience for patients who want to improve their health. At the recent Healthcare Experience Designconference, of which Cueva is the chairwoman, attendees learned 12 strategies for improving the healthcare user experience. - Understand the Problem You're Trying to Solve - Participatory Design: It's All About Empathy - Focus on the Underserved - Eliminate the Source of the Problem - Focus on What Users Need, Not What They Want - Remember That Millennials Are Brats - Don't Confuse Web Literacy and Health Literacy - Don't Forget That Typography Matters - Target the Ready and the Willing - Learn From Video Games - Support Measurement-Based Medicine - Bring a Sword ..

|
Scooped by
rob halkes
April 9, 2013 3:47 AM
|
By Ashley Gold The key to health information security is in data security, and not necessarily the devices in which data is stored, according to Barbara Bartley, executive director of IT operations and information security officer at Montgomery, Ala.-based Baptist Health. Bartley, in a recent interview with Health IT Security, says that too often, people get "lost" in trying to protect data by focusing on devices. Bartley thinks that her approach can help CIOs and CISOs focus on the "most important part" of managing a large healthcare system's security framework.
In describing Baptist Health's technical safeguards, Bartley says, "The biggest security impact, in my mind as a security officer, is our end users having knowledge of the privacy and security expectations and how breaches happen. Education, monitoring and auditing are our life from a security standpoint."
All mobile devices issued to end users--such as iPads, iPhones and Androids--are physically encrypted with multi-factor authentication to reduce access to protected health information, according to Bartley. When it comes to BYOD, she says, employees must follow ground rules, which means having a remote wipe enabled.
As FierceMobileHealthcare recently reported, nearly 89 percent of U.S. healthcare workers use their personal smartphones for work purposes, according to a Cisco partner network study. When it comes to security, the study found that 41 percent of healthcare employees' personal devices are not password protected.

|
Scooped by
rob halkes
March 8, 2013 3:15 AM
|
Editorial Patients in context: Recognizing the companion as part of a patient- centered team
Marla L. Clayman, Megan A. Morris Reviews Physician–patient–companion communication and decision-making: A systematic review of triadic medical consultations
R.C. Laidsaar-Powell, P.N. Butow, S. Bu, C. Charles, A. Gafni, W.W.T. Lam, J. Jansen, K.J. McCaffery, H.L. Shepherd, M.H.N. Tattersall, I. Juraskova Effects of remote feedback in home-based physical activity interventions for older adults: A systematic review
Hilde Geraedts, Agnes Zijlstra, Sjoerd K. Bulstra, Martin Stevens, Wiebren Zijlstra Assessments Validation of the English version of the Trust in Oncologist Scale (TiOS) Marij A. Hillen, Phyllis N. Butow, Martin H.N. Tattersall, George Hruby, Frances M. Boyle, Janette Vardy, Bellinda L. Kallimanis-King, Hanneke C.J.M. de Haes, Ellen M.A. Smets How to ask: Older adults’ preferred tools in health outcome prioritization Siobhan M. Case, Terri R. Fried, John O’Leary Cross-cultural validation of the Patient–Practitioner Orientation Scale (PPOS)
Cláudia M.A.S. Pereira, Carlos F.S. Amaral, Maria M.F. Ribeiro, Helena B.M.S. Paro, Rogério M.C. Pinto, Lara E.T. Reis, Carlos H.M. Silva, Edward Krupat Communication Studies Stimulating client involvement and client–provider dialog through participatory video: Deliberations on long-term care in a psychiatric The perception of shared medical decision making of expert and lay people: Effects of observing a movie clip depicting a medical consultation

|
Scooped by
rob halkes
March 5, 2013 3:51 AM
|
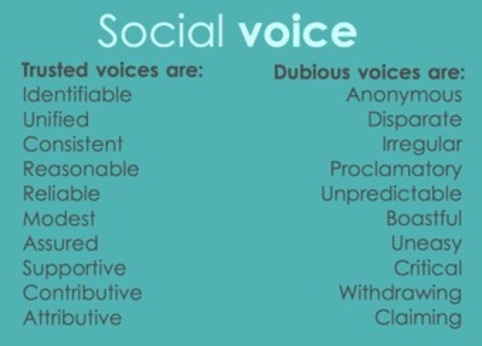
Many articles have been written about what in recent times has come to be known as 'content strategy' -- the reassuring, if not always entirely accurate, notion that we are in control of all the resources available to us, can marshal them with precision, and present them optimally. Rather less has been said about the manner in which we present these materials, presumably because it is a given that by default we will do so in the most sympathetic and productive manner possible. However, the critical eye does not have to wander too far across the topographies of social environments to appreciate that this is frequently not the case. ...

|
Scooped by
rob halkes
February 21, 2013 1:05 PM
|
In a recent study, 77 percent of physicians believed patients understood their diagnosis, but only 57 percent of patients could correctly state their diagnosis. Limited or poor communication channe... Go direct to summary of the refered research: http://www.ncbi.nlm.nih.gov/pubmed/20696951
|



 Your new post is loading...
Your new post is loading...





























Is "patient consent" enough to state that doctor and patient make joint decisions? (Compare with this phrasing: "when the patient has consented to a certain procedure or activity, are doctor and patients making shared decisions?")
Is patient's consent satisfactory to conclude an optimal relationship between doctor and patient is present conducive to optimal health outcomes?
This is all well intended, of course. Still: although it is, as is written, about doctors and patients making decisions together. But in the initating of these Q&A's, isn't there something odd?
Are legal interests of doctors being put above patients's interests for well taken care? Is development of an optimal relationship between caregiver and -taker paved by the concept of consent? is it that easy?
OMG, we are still far away, aren't we? Or do youthink differently?