 Your new post is loading...

|
Scooped by
rob halkes
November 6, 2014 12:44 PM
|
Last week I was part of the first community meeting for Data for Health, a program sponsored by the Robert Wood Johnson Foundation. It was held in Philadelphia on October 30 [..]. You can catch up on the #data4health tweets thanks to Symplur — and there were some good ones [..] Once again I was struck by how wide open the definition of “data” can be. I shared the following data points, based on a Pew Research study I led: - 7 in 10 U.S. adults track a health indicator for themselves or someone else.
- Half track regularly, half track when something comes up.
- Technology plays a minor role — about 1 in 5 trackers use a medical device, an app, or any other digital tool.
- 1 in 3 trackers uses paper and pencil to take notes.
- Fully half of trackers say they do so in their heads (and that includes me).
- 1 in 3 trackers share their data with family members or clinicians, but many do not. They are asking secret questions and we must not only respect that, but build it into our planning.
- 45% of U.S. adults live with a chronic health condition; of those, 8 in 10 track some aspect of health.
- Tracking data is not a hobby for this group, but rather a way to see themselves more clearly. This might be true of public health in general — data is a mirror we try to use to make good decisions, based on facts.
[..] My favorite insight of the day came from someone who, when discussing who should be part of the design process for health data systems, said that front desk workers are the ones who know the community best. Read the full blog here ! ALso be sure to see the Pew study here

|
Scooped by
rob halkes
October 1, 2014 4:54 AM
|
From Patient View: Launch of the first-ever toolkit to help people understand and use health apps
©PatientView Ltd 2014
Author: Tony Newbold
Editors: Clive Nead, Dee O’Sullivan, Alexandra Wyke
Designer: Mark Ansell A clear, concise, simple manual to help patients and the public make the best choices and decisions about health apps, “Health Apps—a Toolkit to Help You”, is available in print and online. Launched today, Wednesday, 1st October 2014, at the European Health Forum Gastein 2014, and circulated to the Forum’s 650 delegates (who come from all over Europe and beyond, and who represent the key stakeholders of the European health policy community). This Toolkit is needed to answer the many questions that patients and carers have about health apps
A soon-to-be-published study* by PatientView will reveal that the public are confused by the sheer number of health apps available (100,000), and are not sure that a particular health app will help them. Members of the public may also not trust health apps, because they do not know who makes the apps, or whether their health data would be secure on an app. [*Source: “What do patients and carers want from health apps?” A July-October 2014 global survey of over 1,000 patients, conducted by PatientView in collaboration with Health 2.0. Survey results to be released Monday, 10th November 2014, at the 2014 Health 2.0 conference in London.]
“The myhealthapps’ Toolkit is a good initiative to empower citizens. It is the type of health-literacy project that the European Commission encourages.” —Robert Madelin, Director General, DG CONNECT, European Commission

|
Scooped by
rob halkes
September 9, 2014 8:49 AM
|
Is that an app you're wearing or are you just happy to track your progress? This adulteration of Mae West's classic come-on is most likely justified. Just Just recently, International Data Corporation issue the prediction that wearable device shipments worldwide would rise more than 488.9 percent between 2014 and 2018, rising from 19.0 million to 111.9 million. It’s a rapidly changing marketplace. “There’s been talk recently about the future of notifications on such devices, fashion brands such as Tory Burch and Diane von Furstenberg (DVF) have partnered with tech companies to make wearables more stylish, and GE is testing Google Glass to see how the technology could help boost efficiency in its car factories,” reports eMarketer. So far, it appears that people like using mobile health and fitness apps to get in shape — and that wearables will be the next rung on the ladder. Polling by Makovsky Health and Kelton Research in March documented high interest in wearable health and fitness devices: 81 percent of U.S. internet users said they would use one. Tracking fitness was the top reason, cited by 48 percent. Monitoring personal health issues came in second, and tracking diet and nutrition ranked third. But developers could be waiting a while before the trend becomes widely accepted. A June, 2014 Opera Mediaworks study showed that only 2.5 percent of smartphone users said they used wearable fitness and activity trackers while exercising. Wearables may be the future, but “do-all smartphones are still No. 1 when exercisers need to pump it up,” eMarketer asserts.

|
Scooped by
rob halkes
September 4, 2014 6:47 AM
|
In Sustainia, the most important resource in the sustainable transition is you. In the guide to person-centred care, we have taken a closer look at the world’s healthcare systems and what it takes to make them person-centred. What we understand by healthcare today needs to be redefined so that you become an active partner in creating health. DNV GL and Sustainia are travelling the world this fall to explore how we can co-create healthcare. The mission is to put the person, you, at center of the care. And to do this, we will identify, document and communicate solutions that can inspire a safer, smarter and more sustainable healthcare approach.

|
Scooped by
rob halkes
August 29, 2014 8:26 AM
|
They've been there – and here's what you can learn from their experiences. It’s your body – your tests, your treatment. Your disease. But grasping control of your patient experience, when you’re surrounded by white coats and intimidating medical lingo and scary diagnoses, can be hard. U.S. News talked to 10 people who have a lot of experience being patients – or have advocated for a patient – about the most important lessons they’ve learned about patient empowerment. Their responses: - AnneMarie Ciccarella
- Trisha Torrey
- Alexandra Albin
- Ben Heywood
- Matt Cavallo
- Marisa Zeppieri-Caruana
- Jullia Hallisy
- Dave deBronkart
- Kerry Sparling
- Tiffany M. Peterson
See them all here !

|
Rescooped by
rob halkes
from Social Media and Healthcare
August 22, 2014 5:58 AM
|
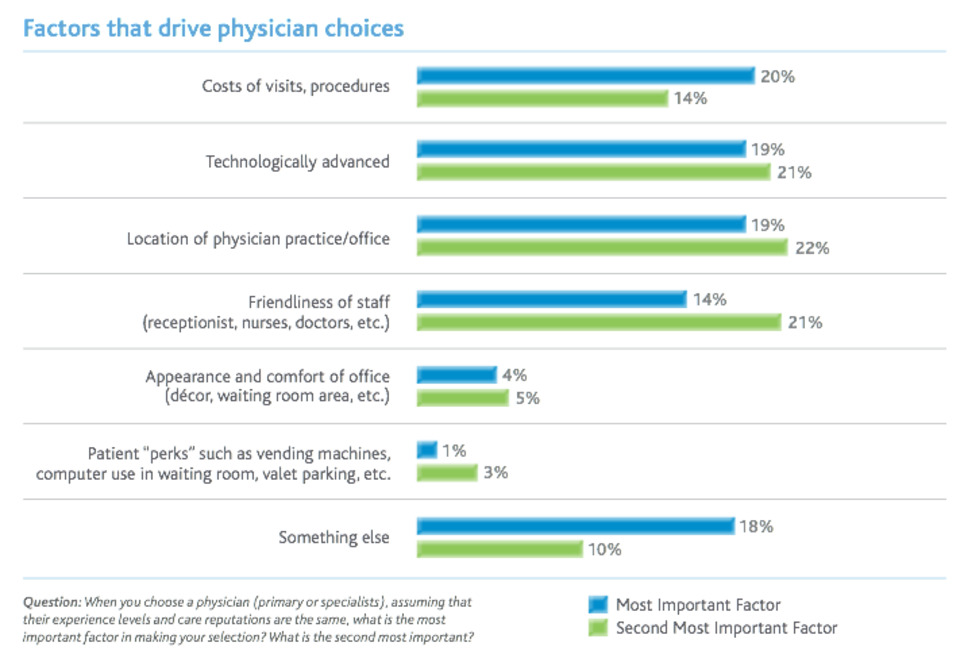
Despite security and privacy concerns, a growing number of physicians are embracing digital technology in their communication with patients. That includes sharing information about services and wellness to a broad audience, and also corresponding directly with patients about their personal health issues. The recent improvements start with physicians revamping their websites. This has allowed doctors to post essential information about which services they offer and to make appointment scheduling easier through patient portals. That includes streamlining the processes of rescheduling and sending reminders electronically instead of over the phone. A common analogy that’s made is making the patient scheduling process similar to picking a seat for a flight through an airline’s website, says James Karpook, principal at The Chartis Group. That mentality is expanding to include information about how to contact physicians directly to follow-up after an office visit. “More and more physicians are communicating with their patients via email so that they don’t have to call in and be waiting on the phone to speak to a nurse or the physician,” says Karpook.
Another area where communications technology is helping doctors is in disease management. For example, patients who have congestive heart failure can use a device at home that links to a processor to capture real-time results. Physicians can then take immediate action when a problem arises. Also, diabetes patients are using mobile apps to log their blood-sugar levels so healthcare providers can monitor them in real-time. Providers are also sending patients text message reminders to check their blood sugar and then have the data sent to the doctor’s office. Social media is another growing digital frontier for physicians. Many are posting articles and sharing their expertise about wellness and healthcare innovation on Facebook, Twitter, and LinkedIn. “Social media is ideal to connect with patients collectively, but not individually,” said Dr. Kevin Pho to The Doctor’s Tablet Blog. Dr. Pho is an advocate of doctors having protected social media time during the workday so they can write blog posts or create videos to be shared. That would force them to get more comfortable with the technology and possibly push ideas to another level. “Replacing a half-day session a week of seeing patients with social media time to create content would be a reasonable goal,” he said. “Healthcare leaders and administrators are the ones who can make that happen.” Still, it’s the one-on-one electronic communication that will set the tone for the future of healthcare. More doctors are corresponding with patients through email and text messaging. Karpook also cites a next wave of physician concierge services that charge a monthly fee to allow patients greater access to physicians through email, instant messaging, or video chat. Making these channels secure and private is the biggest challenge ahead. “We’ll have to continue to find ways to ensure that electronic health information that’s shared is secure,” he says. “There needs to be the IT infrastructure to support it.”
To a great extent, electronic communication between doctors and patients will be driven by consumer preference. As more consumers begin to prefer electronic means for communication, healthcare organizations and physicians will have to adapt to accommodate them. Couple that with the bigger structural healthcare reforms that are promoting better communication between doctors and patients, and it’s likely that we’ll be seeing more progress in this area very soon. “Perhaps in the coming years, when payment isn’t tied to the number of patients seen, communicating with patients can be emphasized, whether it’s through a phone call, email, or social media,” said Dr. Pho.
Via Plus91

|
Scooped by
rob halkes
August 15, 2014 7:54 AM
|
Medication management for patients, as well as their physicians and pharmacists, is going digital. Much of this is driven by the changing demographics of patients and today’s health care providers, says Nancy Green, managing principal, healthcare, of Verizon Enterprise Solutions. “Patients want technology that they are familiar with, and so does the younger generation of physicians,” Green says. “A CEO of a major health care organization recently went to his CIO and said, ‘Whatever IT the doctors or patients want, give it to them. Make it happen. I don’t care how.’” Since doctors provide the billable services for hospitals, and patients (or their insurance companies) pay for them, this scenario is playing out all over the U.S. [...] “Being able to present patient-centered information by way of a web-based graphic interface would likely provide the information and answers that many demand,” says Dr. Mark Leavey, an internist who sees patients at Lutherville Personal Physicians in Lutherville, Md., a satellite of Mercy Medical Center. “Clearly, the paper printout supplied with medications by pharmacies may have all of the information, but it is presented in a form that is a challenge for any but the most well-versed to read.” Scanning a QR code directs users to information portals that display the prescription data in layers, with the most direct and basic facts first, followed by commonly asked questions and a video of proper ways to use the medication. [...] “The system also includes an application that users can download on their phone or tablet for use in helping with chronic conditions by managing their taking of medications or monitoring other health-related tasks they must perform daily,” Hart said....

|
Scooped by
rob halkes
July 8, 2014 6:19 AM
|
Wolters Kluwer is a market-leading global information services and publishing company focused on professionals. (December 12, 2012) — Philadelphia, PA (December 12, 2012) – According to a new Wolters Kluwer Health survey, 80 percent of consumers believe the greater “consumerization” of healthcare – or the trend of individuals taking a greater and more active role in their own healthcare – is positive for Americans. Survey data suggests many Americans feel that a greater role in their care is not only good, but necessary, with 86 percent of consumers reporting that they feel they have to take a more proactive role in managing their own healthcare in order to ensure better quality of care. Most consumers also say they feel prepared to take on a greater role in managing their own healthcare, with 76 percent reporting that they have the information and tools to take a more proactive role in healthcare decisions ranging from choosing healthcare providers to researching treatment options. Despite feeling prepared, only 19 percent report that they have their own electronic Personal Health Record (PHR). [..] “With greater responsibility placed on patients to take a role in their own care, it’s essential that consumers have access to evidence-based tools and resources to make informed decisions about their care in partnership with their healthcare providers,” said Dr. Linda Peitzman, Chief Medical Officer, Wolters Kluwer Health. “Access to research-based medical information not only can positively impact quality of care, but it also can lead to improved doctor-patient communication and relationships.” Survey findings showed that the notion of the “patient experience” is also gaining significance for many Americans. Three in ten adults (30 percent) want their patient experience to be the same as any other customer experience they have – such as shopping, hotel and travel experiences – complete with choices and control. [..]
See report here

|
Scooped by
rob halkes
June 14, 2014 6:41 AM
|
The term "patient engagement" is at risk of becoming a vague buzzterm, as it lacks a shared definition. This paper aims to pinpoint the key conceptualizations of "patient engagement" from recent academic literature, in order to deepen understanding of the term.

|
Scooped by
rob halkes
May 30, 2014 9:47 AM
|
Experience co-creation in health care is an effective method to innovate value to patients in a personalized way, in collaboration with all relevant stakeholders.
It is intended to benefit patient...

|
Scooped by
rob halkes
March 25, 2014 5:34 AM
|
"How "Flipped" is your health practice?" Flip the Clinic is a new Robert Wood Johnson Foundation project to re-imagine the medical encounter between patients and care providers. What Exactly is Flip the Clinic?Our goal is not only to create a specific set of practices that will improve the medical encounter, but also to inspire others to invent new ways to get more out of the clinic visit, too. The first batch of resources for patients and providers launched in early 2014. But we’re not stopping there. The future of Flip the Clinic will be built from patient, care provider, and administrator input and ideas; it will be built from the advice of those willing to try something bold. We hope that FliptheClinic.org will serve as a hub for innovative ideas already happening as well as a clearinghouse for what works and what doesn’t in the doctor-patient encounter. Flip the Clinic is an ongoing conversation, powered by your participation.
The traditional doctor’s visit is ripe for reinvention—both because it is such a valuable interaction, and because we know there are ways to make it better. We believe that new tools, technologies, and strategies can empower people to be more informed and more engaged when they walk into the doctor’s office and better equipped to improve their health when they walk out the door. And we believe that doctors, nurses, and other care providers can improve the ways they communicate and engage with patients during visits. We believe they can take advantage of new tools for monitoring, supporting, and connecting with their patients outside of the office, too. We think that by tapping into these strategies, we could to turn the provider-patient interaction on its head—and promote better, more meaningful relationships while doing so.

|
Scooped by
rob halkes
March 20, 2014 10:47 AM
|
Patient Education and Counseling, Volume 95, Issue 1, Pages 111-117, April 2014, Authors:Omolola E. Adepoju; Jane N. Bolin; Charles D. Phillips; Hongwei Zhao; Robert L. Ohsfeldt; Darcy K. McMaughan; Janet W. Helduser; Samuel N. Forjuoh Abstract ObjectiveThis study compared time-to-hospitalization among subjects enrolled in different diabetes self-management programs (DSMP). We sought to determine whether the interventions delayed the occurrence of any acute event necessitating hospitalization. MethodsElectronic medical records (EMR) were obtained for 376 adults enrolled in a randomized controlled trial (RCT) of Type 2 diabetes (T2DM) self-management programs. All study participants had uncontrolled diabetes and were randomized into either: personal digital assistant (PDA), Chronic Disease Self-Management Program (CDSMP), combined PDA and CDSMP (COM), or usual care (UC) groups. Subjects were followed for a maximum of two years. Time-to-hospitalization was measured as the interval between study enrollment and the occurrence of a diabetes-related hospitalization. ResultsSubjects enrolled in the CDSMP-only arm had significantly prolonged time-to-hospitalization (Hazard ratio: 0.10; p=0.002) when compared to subjects in the control arm. Subjects in the PDA-only and combined PDA and CDSMP arms showed no improvements in comparison to the control arm. ConclusionCDSMP can be effective in delaying time-to-hospitalization among patients with T2DM. Practice implicationsReducing unnecessary healthcare utilization, particularly inpatient hospitalization is a key strategy to improving the quality of health care and lowering associated health care costs. The CDSMP offers the potential to reduce time-to-hospitalization among T2DM patients.

|
Scooped by
rob halkes
March 20, 2014 10:10 AM
|
Patient Education and Counseling, Volume 95, Issue 1, Pages 76-82, April 2014, Authors:Jamie A. Green; Alda Maria Gonzaga; Elan D. Cohen; Carla L. Spagnoletti
Abstract Objective To develop, pilot, and test the effectiveness of a clear health communication curriculum to improve resident knowledge, attitudes, and skills regarding health literacy. Methods Thirty-one internal medicine residents participated in a small group curriculum that included didactic teaching, practice with a standardized patient, and individualized feedback on videotaped encounters with real patients. Outcomes were assessed using a pre-post survey and a communication skills checklist.
Results Mean knowledge scores increased significantly from 60.3% to 77.6% (p<0.001). Residents also reported increased familiarity with the concept of health literacy (mean response 3.2 vs. 4.5 on a 5 point scale), importance placed on health literacy (4.2 vs. 4.9), frequency of considering health literacy in patient care (3.3 vs. 4.0), and confidence in communicating with low literacy patients (3.3 vs. 4.1) (all p<0.001). Use of plain language increased significantly from 33% to 86% (p=0.023). There were nonsignificant increases in the use of teach-back (0–36%, p=0.116) and encouraging questions (0–14%, p=0.502).
Conclusion Training in clear health communication improves resident knowledge, attitudes, and skills regarding health literacy. Practice implications The increased use of clear health communication techniques can significantly improve the care and outcomes of vulnerable patients with limited health literacy.

|
Scooped by
rob halkes
March 19, 2014 2:54 PM
|
Web 2.0 Chronic Disease Self-Management for Older Adults: A Systematic Review
Background: Participatory Web 2.0 interventions promote collaboration to support chronic disease self-management. Growth in Web 2.0 interventions has led to the emergence of e-patient communication tools that enable older adults to (1) locate and share disease management information and (2) receive interactive healthcare advice. The evolution of older e-patients contributing to Web 2.0 health and medical forums has led to greater opportunities for achieving better chronic disease outcomes. To date, there are no review articles investigating the planning, implementation, and evaluation of Web 2.0 chronic disease self-management interventions for older adults.
Objective: To review the planning, implementation, and overall effectiveness of Web 2.0 self-management interventions for older adults (mean age ≥ 50) with one or more chronic disease(s).
Methods: A systematic literature search was conducted using six popular health science databases. The RE-AIM (Reach, Efficacy, Adoption, Implementation and Maintenance) model was used to organize findings and compute a study quality score (SQS) for 15 reviewed articles.
Results: Most interventions were adopted for delivery by multidisciplinary healthcare teams and tested among small samples of white females with diabetes. Studies indicated that Web 2.0 participants felt greater self-efficacy for managing their disease(s) and benefitted from communicating with health care providers and/or website moderators to receive feedback and social support. Participants noted asynchronous communication tools (eg, email, discussion boards) and progress tracking features (eg, graphical displays of uploaded personal data) as being particularly useful for self-management support. Despite high attrition being noted as problematic, this review suggests that greater Web 2.0 engagement may be associated with improvements in health behaviors (eg, physical activity) and health status (eg, HRQoL). However, few studies indicated statistically significant improvements in medication adherence, biological outcomes, or health care utilization. Mean SQS scores were notably low (mean=63%, SD 18%). Studies were judged to be weakest on the Maintenance dimension of RE-AIM; 13 reviewed studies (87%) did not describe any measures taken to sustain Web 2.0 effects past designated study time periods. Detailed process and impact evaluation frameworks were also missing in almost half (n=7) of the reviewed interventions.
Conclusions: There is need for a greater understanding of the costs and benefits associated with using patient-centered Web 2.0 technologies for chronic disease self-management. More research is needed to determine whether the long-term effectiveness of these programs is sustainable among larger, more diverse samples of chronically ill patients. The effective translation of new knowledge, social technologies, and engagement techniques will likely result in novel approaches for empowering, engaging, and educating older adults with c

|
Scooped by
rob halkes
March 19, 2014 12:32 PM
|
As the number of self-tracking health and fitness tools available to consumers continues to climb, a persistent question has been whether the data they collect might be useful to health researchers. Along with that: Are people who self-track comfortable sharing their data with researchers? A new, must-read report from San Diego’s California Institute for Telecommunications and Information Technology (Calit2), funded by the Robert Wood Johnson Foundation, explores these and other questions. Based on a survey with hundreds of self-trackers, a majority — 57 percent — said one critical assurance they would need before agreeing to make their self-tracked, personal health data available to researchers was that their privacy would be protected. More than 90 percent also said it was important that their data remained anonymous. Respondents said they’d be more comfortable sharing data if they knew it was only going to be used for “public good” research. ..
One open-ended survey that the report’s researchers posed to self-trackers found that 13 percent of respondents specifically mentioned an aversion to commercial or profit-making use of their data, according to the report. One respondent wrote: “It depends who gets it. Research using these data will be instrumental in the future of personal predictive services, but also for that reason are likely to be exploited by marketers and the politically short-sighted. Thus I would like transparency for who has access to my data.” Among the almost 100 health researchers interviewed for the report, 46 percent said that they had already used self-tracking data in their research previously. Some 23 percent reported that they had already worked with digital health companies that offer apps or devices to consumers to track their health. Overall, the researchers interviewed for the report were “generally enthusiastic” about the prospect of using self-tracking data in the future — 89 percent agreed or strongly agreed that such data would prove useful to their research efforts. Almost all of those researchers surveyed said that kind of data could answer questions that other data could not. ..

|
Scooped by
rob halkes
March 18, 2014 6:25 AM
|
Conclusions of the first ever cross-stakeholder, pan-european seminar on health apps, held at the King's Fund on 28 October 2013. The five key messages: 1. Overhauling healthcare systems–making them patient-centric 2. Engaging doctors in the prescribing of health apps
3. Overseeing quality standards for health apps
4. Ensuring that health apps remain of a high standard throughout their lifetime
5. Considerations for policymakers wishing to oversee health apps

|
Rescooped by
rob halkes
from PATIENT EMPOWERMENT & E-PATIENT
March 6, 2014 4:49 AM
|
The evidence is clear that a patient-centered approach -- not a paternalistic, “we know best” approach -- is linked to increased patient engagement, better outcomes, more adherent patients, lower utilization and better patient experiences. .. The setting was a presentation last week at HIMSS 2014. The presenter was Chanin Wendling, the Director of eHealth at Geisinger Health System. Channing was talking about Geisinger’s often cited HIT-driven patient engagement efforts which includes their patient portal, health apps and recent foray into “Open Notes.” What struck me was Chanin’s description of philosophical approach and communication style employed by Geisinger in the course of developing the content for theses engagement tools... Here’s what she said. “We tend to think in a paternalistic way: this is what the patient needs, versus thinking ‘What will work best for the patient?’ and ‘How will the patient relate to whatever we’re prescribing?’ And that’s extremely important because at the end of the day, if you can’t get the patient to help, if they don’t take their meds, if they don’t lose the weight, if they don’t do their exercises, there’s nothing you as a clinician can do. You need the patient to help you.” Here are two things that jumped out at me from Chanin’s comments; 1. Geinsinger’s patient communication style is paternalistic and physician-directed…meaning it is the direct opposite of a patient-centered philosophical approach and communication style. A patient-centered style begins with an understanding of the very things Chanin says Geisinger ignores – what will work best for the patient and how patients will relate to a proposed intervention. The evidence is clear that a patient-centered approach -- not a paternalistic, “we know best” approach -- is linked to increased patient engagement, better outcomes, more adherent patients, lower utilization and better patient experiences. 2. Geisinger’s attitude that patients are inherently unengaged, e.g., won’t help clinicians unless told by clinicians what they need to do, is why so many heath care providers are having difficulty engaging patients at all levels of the organization, including patient portals. Think about it: 82% of U.S. adults visit their doctor at least once a year because “they” think it’s the right thing to do…and Geisinger thinks they are “not willing to help”? Are you kidding me? The problem today is not that patients are unengaged…but that many providers aren’t very engaging. Sure 50% of patient re non-adherent…but 20% of patient non-adherence has been attributed to poor communications on the physician’s part, e.g., paternalistic, physician-directed communications. Sure less than 10% of patients visit the average patient portal in a year…but when portal contents and functionality treat one like an uncooperative child why would one expect a higher level of adoption?
Via Chanfimao, Lionel Reichardt / le Pharmageek

|
Scooped by
rob halkes
February 11, 2014 8:30 AM
|
Who would have thought that this tiny aperture -- a mere 140 characters -- could connect me with so many smart, feisty people? ... Since 1992, I have advocated for all of us to have the information, support and guidance we need to act to improve our health and get the most from our health care. I believe — and there is evidence to back me up — that we do better when we participate in our care to the extent we are able with as much knowledge about what might work that we can absorb. As someone who has been/is being treated for five different types of cancer, I am familiar with many of the challenges we face in getting the most out of our health care. We not only need to know about our specific diseases and treatments and what we can do about them, but we also need to know something about how our care is organized and about changes in general health knowledge and medical practice that affect how we make use of the resources and services available to us. Then we have to act on our own behalf or on behalf of our child, partner, spouse or parent. The organization I direct, the Center for Advancing Health, has mapped out the tasks that are now ours — the many actions we must take to find good health care and benefit from it. Every weekday, I tweet a carefully chosen stream of new evidence, analysis and commentary that covers all the health and health care angles that we — sick or well — might need to know about. I tweet material from major news outlets, peer-reviewed literature, blogs and magazines in the belief that thoughtful consideration of emerging information and understandings about health and health care will serve us well. Here’s why I tweet what I tweet: - It has never been more important for us to be well-informed about so many aspects of health care — not just our complaint of the moment. Otherwise, when we are passive recipients of care, we risk being on the receiving end of medical errors, spending money on unnecessary tests, receiving suboptimal care or simply not knowing how we can best help ourselves. I aim to tweet what we need to know.
- Evidence has never been more important. Especially considering media reports that much of the care we receive may not be consistent with evidence of what is currently deemed most effective. Combined with the rapid pace of new findings, understanding the facts relevant to your situation can be intimidating to patients and health professionals alike. Plus, it’s time-consuming for us to sort out solid information from broad assertions and slick advertisements, so I aim to tweet evidence worth noting, with the understanding that next week’s evidence may reverse what we know today.
- Finding high-quality analysis and commentary that is relevant to the decisions we must make about our health and care every day is a bear. I know. I wouldn’t be traipsing through 40+ different sites every day in search of the best pieces if they were located in one place. I aim to tweet links to useful, diverse analyses and findings.
- Understanding health and health care is not just a matter of digesting new facts. It also includes considering implications of those facts and different perspectives on policies so that the facts have context and meaning. I aim to include articles that tweak easy assumptions, shed light in dark corners and sometimes make me smile.
- Lastly, it’s funner than heck to do this. I have an insatiable taste for gossip, a fascination with trying to figure out what we really need to know to care for ourselves, a long memory for ineffective-but-nevertheless-repeated health care foibles and an impulse toward snarkiness that occasionally breaks through. Spending a couple of hours each day trawling online for new findings, blogs, articles and essays that I think you might find interesting is a great way to start the day. ...

|
Scooped by
rob halkes
February 11, 2014 4:22 AM
|
A British company, Camntech, has received FDA clearancefor a motion-tracking wristband and a wristworn electronic diary, likely for use in clinical trials. The devices are called the MotionWatch 8 and PRO-Diary. According to the filing, the devices ”are intended for the acquisition and analysis of the physical activity of the body during daily living and sleep.” The devices upload data to a PC via a USB cord.

|
Scooped by
rob halkes
January 31, 2014 1:42 AM
|
by Molly Gamble - [ See my comment, if you want it quickly read - but that would be a shame ;-) ]
Patient-centered care is a cornerstone of any accountable care organization, but creating or joining one doesn't necessarily make patient engagement any easier. In the world of healthcare business, patient engagement may sound like a "soft" concept, but its difficulty is nothing to underestimate.
David Muhlestein, PhD, director of research at Leavitt Partners in Salt Lake City, says a minority of patients want to be engaged with their care teams in actively managing their healthcare. The high majority — likely approaching 70 percent — want to turn their care over to their physician and have them take the reigns. The rest of patients do not want to share decisions about their healthcare with physicians at all — they prefer to decide on their own.
"ACOs are finding it's really hard to get people engaged," says Dr. Muhlestein. "Some are proactive or are really trying to engage patients in different ways, but they're not particularly seeing more success than anyone else."
What is working for ACOs' patient engagement? What are the biggest roadblocks? As it turns out, there are several definitions of patient responsibility, high-deductible health plans are bad news for accountable care and no ACO provider will be successful on a high horse.
Seven degrees of engagement
There are numerous buzzwords for patient responsibility — patient engagement, accountability, skin in the game. It's easy to lump these ideas together as synonymous, but Dr. Muhlestein says there are some nuances.
For example, patients and physicians may arrive with different expectations for patient engagement. Patients see it as shared decision-making, or talking to a physician before a decision is made about their treatment to learn about the pros and cons, then making the ultimate decision in conjunction with the physician. It's a behavior largely reserved for the visit to the physician.
Physicians, on the other hand, see engagement as active condition management. This includes lifestyle changes, adherence to medications and regular dialogue with the care team to ensure the care plan is going smoothly. Essentially, this version of patient engagement involves the patient taking on more responsibilities that traditionally belonged to clinicians and carrying them out between physician visits.
People who have used accountants to complete income taxes may see where patients are coming from. Instead of doing a few tasks on a daily basis, many people find it easier to drop off their financial paperwork and receipts at the end of the year and let someone else do the math. The same is often true for patients' expectations for healthcare.
"You want to say, 'Here, you deal with this. I'll come back next month and you'll tell me how to change the doses of my meds,'" says Dr. Muhlestein.
How having "skin in the game" could muddle accountable care
There's another shade of patient responsibility, one that is a little greener in hue. More patients are taking on more financial responsibility for their healthcare. Recent years have brought a boom of high-deductible health plans, which cut businesses' health benefit costs by shifting more responsibility onto their employees. This is not the best news for people trying to advance accountable care. Some ACO leaders simply call these health plans outrageous, even immoral.
"It's something we're concerned about," says Marcia Delk, MD, chief quality officer with Marietta, Ga.-based WellStar Health System, a five-hospital system participating in the Medicare Shared Savings Program. Dr. Delk spoke about the trend more generally, as high deductibles don't pertain to Medicare beneficiaries. "Those individuals with more of a responsibility to their bills are very price sensitive to whatever healthcare they're buying." And this sensitivity extends to basic preventive care — a huge component of population health — that is covered by their plans.
A 2012 study conducted by Rand Corp., Towers Watson and the University of Southern California examined families' use of care in the first year after switching from traditional plans to high-deductible health plans. These families spent, on average, about 14 percent less on their healthcare than those enrolled in traditional plans. But they also cut back on beneficial preventive services — such as cervical and colorectal cancer screenings, mammograms, and blood tests for glucose and lipids — even though most of these preventive services are covered under consumer-directed plans…
Much like the financial case providers must make for investments in population health management — linking initial costs to long-term gains — physicians and care teams may need to take a similar approach with their patients. Robust communication and patient education can help them understand the value of their vaccinations, mammograms and other preventive measures, and how these are not the measures to skimp on.
"If we engage patients properly and work with them to understand the benefit of taking care of a chronic condition, or getting a colonoscopy, and how that will reduce costs later on, it can work," says Dr. Delk.
Reaching instead of preaching
That seems to be the main job description for ACOs today — finding what works.
…
Conclusion
The normal fee-for-service environment does not have financial rewards for patient care coordination or care management programs. Even though ACOs are one of the most progressive steps toward pay-for-performance reimbursement, joining one doesn't necessarily provide direct reimbursement for patient education and engagement.

|
Scooped by
rob halkes
January 23, 2014 11:00 AM
|
Patient Education and Counseling, Volume 94, Issue 2, Pages 187-192, February 2014, Authors:Eva Boström; Ulf Isaksson; Berit Lundman; Ulla H. Graneheim; Åsa Hörnsten Objective The aim of this study was to explore the interaction between diabetes specialist nurses (DSNs) and patients with type 2 diabetes (T2D) during group sessions about self-management. Methods Ten DSNs and 44 patients were observed during group sessions about self-management, and thereafter the observations were analyzed using qualitative content analysis. Results The interaction was characterized by three themes: becoming empowered, approaching each other from different perspectives, and struggling for authority. The interaction was not a linear process, but rather a dynamic process with distinct episodes that characterized the content of the sessions. Conclusion It is important to achieve an interaction that is patient-centered, where the DSN is aware of each patient's individual needs and avoids responding to patients in a normative way. A satisfying interaction may strengthen patients’ self-management, and also may strengthen the DSNs in their professional performance. Practice implications Authority struggles between patients and DSNs could be a prerequisite for patients to become autonomous and decisive in self-management. DSNs might benefit from an increased awareness about this issue, because they can better support patients if they do not perceive authority struggles as threats to their professional role.

|
Scooped by
rob halkes
January 21, 2014 9:49 AM
|
As I sat next to him, and now in a voice confident and ringing with anticipation, Mr A explained in painstaking detail how he determined which approach shot to hit to the 2nd green on the Black Course at Bethpage State Park. Only 10 minutes earlier when Mr A and I first met he was weary, his face was drawn, and the sound of the aortic balloon pump keeping him alive made it nearly impossible to hear him. Sitting down, which would seem like one of the simplest things to do, is the least practiced of five communication skills for doctors that Lenore would have endorsed and that research has shown can make a big difference in patient satisfaction. “5 Simple Habit to Help Doctors Connect with Their Patients” When my grandmother was caring for my ill grandfather — she expressed neverending confidence in his physician. As a physician in training I was very interested about the qualities she saw in him that made her so confident that he was in fact the best doctor for her husband. He talks to us. He sits with us. He takes time out of his busy day to let us know that he cares… My grandfather passed away not too long after that discussion. Sadly it was likely that very same physicians fault. But no one needed to now that… my grandmother’s confidence didn’t wane through his last dying days. (read on at the original blog by Howard..!)

|
Scooped by
rob halkes
January 14, 2014 9:44 AM
|
The health records of everyone in the NHS will be pooled in a vast database which can be accessed by researchers and pharmaceutical companies. But campaigners warn it could breach privacy.But campaigners warn it could breach privacy. By Sarah Knapton, Science Correspondent he medical notes of every NHS patient are to be pooled in a vast database to improve research. In the coming days every household in Britain will receive a letter advising them that, from April, their medical histories will be shared with researchers and pharmaceutical companies unless they opt out. Today leading charities including Cancer Research UK, Diabetes UK and the British Heart Foundation launch a campaign to highlight the importance of allowing the notes to be accessed for the advancement of medical science. They say the database will help them understand the causes of disease, spot side-effects to new drugs and detect outbreaks of infectious diseases. Doctors have promised that patients will remain anonymous. But data protection campaigners have warned that individuals risk being identified and that the notes may be inaccurate. Health professionals have admitted the ‘care.data’ database could be vulnerable to targets from hackers and criminal networks, but say it is necessary to improve the health service..... [ Read the full blog! Specifically quotes from experts for and against this registration }

|
Scooped by
rob halkes
January 14, 2014 9:25 AM
|
Patients now often enter a physician’s office with preconceived notions. All the parties involved are cognizant of one thing: time is limited. The patient is hoping their issue is addressed he patient is hoping their issue is addressed (hopefully, the provider often fears it is not more than one), the physician hoping that the right targeted information is provided. These desires are commonly not met by either side. Should there be ‘sides’ to healthcare? How did this inherently adversarial relationship develop before the parties have even met? In an earlier postI discuss the importance about navigating the healthcare system. I would like to discuss here some observations I have made both in practice and as a caregiver for my mother on the initial office visit. They address my sensitivity to issues which are viewed by others who are resigned to a new status quo and accept them as part of healthcare. Perhaps digital health technologies facilitating communication among patients and providers will help in these regards. 1. Patients see answering their questions as a value added service. I am amazed at “Is it OK if I ask a question?” To their amazement, my pat answer is “This is what I am here for.” Every encounter is concluded by asking “Do you have any (or other) questions?” The look of satisfaction after that is the only thing I need to propel me to my next patient with a sense of satisfaction and purpose. 2. Patients think they need to provide a diagnosis instead of seeking one. I have heard countless patients seeking my help (either via referral by another physician or self-referred) that they are sorry they don’t know a diagnosis for the complaints which have prompted my visit. My philosophy is that a patient is only responsible for describing symptoms. Most physicians are familiar with Sir William Osler, a great pioneer in medicine, who said “Most times it is the patient who will furnish the diagnosis.” What he meant was that the patient’s narrative, NOT a specific diagnosis would provide adequate information to make said diagnosis. While it is not as easy today, given significant therapeutic implications not present in Osler’s time, the patient’s story remains critical to focusing future investigation and questioning. I allow the patient to furnish the whole story without interruption. In the case of no specific diagnosis found for a non-serious condition, I emphasize that it is just as important in knowing what it ISN’T as what it is, and that this is not a denial of their symptoms. I encounter this often facing patients with palpitations. 3. Patients smile when I tell them that I dispense medications and suggest tests on a minimal basis. Most patients, contrary to many providers’ impression, do not seek or desire a pill, tests or procedures. Certainly they cannot be avoided in all circumstances. Initially, they want to know if the condition is (or potentially) serious, and why each therapy, test, or procedure is prescribed. Explanations go a long way. Often communication with other providers (especially regarding side effects of meds prescribed by others) is critical. I tell patients that my goal is to decrease medication use, not to increase it. I find that relatively healthy 90 year olds are on minimal medications and tell them that it is in part for this reason that they are doing relatively well. Ordering tests for defensive medicine purposes is largely unnecessary and many do not fall into accepted practice guidelines. Good patient relationships are fundamental to decreasing liability concerns. Minimizing interventions are both important in this regard and appreciated by patients as a sign of patient advocacy. 4. Patients are relieved when I acknowledge the importance and intent of caregivers. Many patients are embarrassed when significant others or other caregivers accompanying them to either ask questions, take notes or corroborate the narrative. I take time to dispel any doubt about the importance of that person. I first ask for the relationship of the person and if it is OK to share all of my thoughts with that person. The extent of caregiver support might very well affect the type of treatment plan I recommend or the need to contact that person to discuss the shared decision plan. 5. Patients are surprised when I tell them that old age is not a diagnosis. While many diseases are diseases of old age, a patient’s age itself is not a disease. Someone presenting with fatigue due to anemia should certainly not be written off as having ‘anemia of old age.’ I am not advocating exhaustive workup of elderly patients, merely stating that a discussion regarding shared treatment decisions needs to take place. Discussions surrounding advanced directives should also include how far one would like to go in testing and therapeutic procedures. This might not preclude an otherwise healthy elderly patient from undergoing a workup for a problem impairing quality of life.

|
Rescooped by
rob halkes
from Social Health on line
January 13, 2014 11:25 AM
|
When John "Chuck" Lenferink was being readied to fly from Campbell County Memorial Hospital to Denver in August, he turned to Angela Roesler and said, "This is going to kill me, isn't it? The nurse looked at her 68-year-old chronically ill patient and told him "yes." If he didn't make some big changes, and soon, his chronic obstructive pulmonary disease (COPD) and congestive heart failure would be the death of him. At the time, Lenferink was averaging one hospital stay and at least two emergency room visits per month. If he wasn't in the hospital for heart failure, it was for COPD. He was overweight, he couldn't breathe without oxygen and things were only getting worse. Lenferink is stubborn. He'll be the first to say he doesn't like being told what to do. But faced with his own mortality, he knew he needed to listen to his favorite nurse. "When he came home, he was a changed man," Roesler said. Roesler loves being a nurse, and she also loves to teach. When the hospital decided to create a transition care program in May, she was ecstatic. "It's the best of both worlds," she said. Roesler had been an acute care nurse in the medical surgical department since 2009, but the change to a transition care nurse was easy. "It's about the people," she said. "I love my patients, and I love this job." ... participating patients must be 65 or older and have one of the 10 most common diagnoses for readmitted patients, which are: congestive heart failure, COPD, coronary artery disease, diabetes mellitus, stroke, hip fracture, peripheral vascular disease, pulmonary embolism, chronic back pain and cardiac arrhythmia. The nurses meet with at-risk patients while they're still in the hospital and then do a home visit once they are discharged. "We don't do any acute assessments. We don't take blood pressures. We don't do what public health and home health agencies do," Roesler said. "We don't compete with them. We're kind of an adjunct to them." The nurses act as a liaison between the patient, their doctors and the hospital. Their main goal is education and empowerment. During the first home visit, the transition care nurses go over the discharge information that the hospital gave the patient and come up with an action plan. The biggest challenge during the first visit is medication reconciliation, Roesler said. The nurse and patient go through all the patient's medications together and outline which pills the patient should be taking, how often and why. ... "This is a great program. I'm very thankful the hospital decided to do it," Roesler said. "It's definitely made a difference in the lives of real people." ... It's not a time-driven program, so you get time with your patients, and you get to invest in them and in their success," she said. Patients are taking control of their health, and the hospital is seeing its readmission rates go down for patients 65 and older. "I think it's a good fit for every community, honestly," Roesler said. "It probably works well here because we are a community-focused hospital. We're it. So when people go to the hospital, they're going to come here, and when they go home they're going to look back to us to help them succeed at home." ... The hospital doesn't charge patients to use the service, and it's not getting reimbursed for it. The hope is that the program will work so well that the hospital will continue to provide the service once the grant stops paying the nurses' salaries. "It's the right thing to do for the patients, and that's what I love," Roesler said. "If it's the right thing to do, then let's keep doing it."
Read more here: http://www.kansascity.com/2014/01/09/4739811/nurse-helps-patients-take-control.html#storylink=cpy
|



 Your new post is loading...
Your new post is loading...

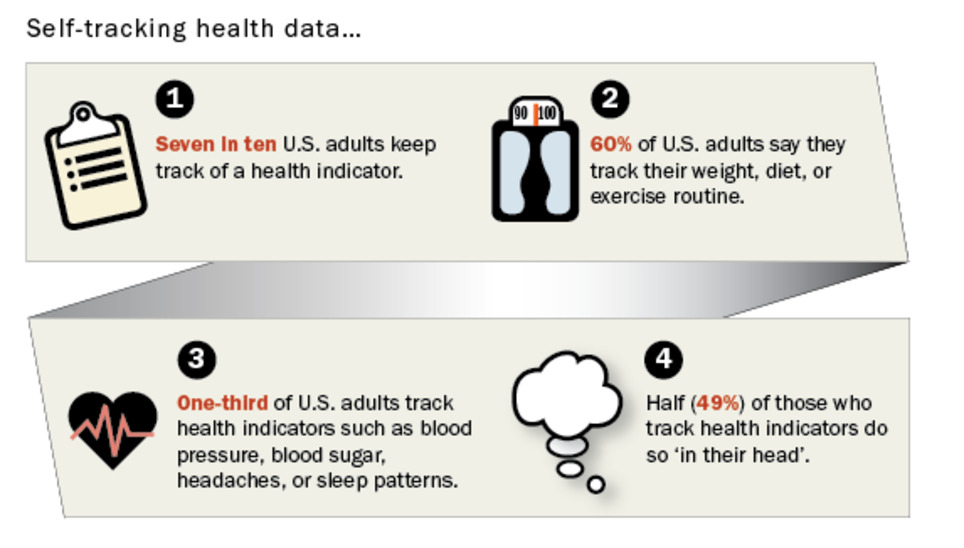
































Indeed, so many people do track some health parameters themselves: the "ground" for many interest in health apps. But when it comes to relate with these data to their "formal" health care providers, .. we get into a complete other realm. It seems even to be so that patients try to avoid this exchange. .. So many things need to be accommodated at the site of the ...
indeed, the providers, of course.
One of the implications of ehealth.
(see for instance here )