Your new post is loading...

|
Scooped by
HAS-veille
June 8, 2023 10:53 AM
|
Physicians make critical time-constrained decisions every day. Clinical predictive models can help physicians and administrators make decisions by forecasting clinical and operational events. Existing structured data-based clinical predictive models have limited use in everyday practice owing to complexity in data processing, as well as model development and deployment1–3. Here we show that unstructured clinical notes from the electronic health record can enable the training of clinical language models, which can be used as all-purpose clinical predictive engines with low-resistance development and deployment. Our approach leverages recent advances in natural language processing4,5 to train a large language model for medical language (NYUTron) and subsequently fine-tune it across a wide range of clinical and operational predictive tasks. We evaluated our approach within our health system for five such tasks: 30-day all-cause readmission prediction, in-hospital mortality prediction, comorbidity index prediction, length of stay prediction, and insurance denial prediction. We show that NYUTron has an area under the curve (AUC) of 78.7–94.9%, with an improvement of 5.36–14.7% in the AUC compared with traditional models. We additionally demonstrate the benefits of pretraining with clinical text, the potential for increasing generalizability to different sites through fine-tuning and the full deployment of our system in a prospective, single-arm trial. These results show the potential for using clinical language models in medicine to read alongside physicians and provide guidance at the point of care. A clinical language model trained on unstructured clinical notes from the electronic health record enhances prediction of clinical and operational events.

|
Scooped by
HAS-veille
May 31, 2023 7:44 AM
|
IntroductionThe prevalence of non-adherence to antidiabetic treatment remains high despite various efforts. Thus, the positive effects of the antidiabetic treatment cannot be optimised and th

|
Scooped by
HAS-veille
May 26, 2023 5:51 AM
|
Using AI to Interpret Medical Images The authors examine the advantages and limitations of current clinical radiologic AI systems, new clinical workflows, and the potential effect of generative A

|
Scooped by
HAS-veille
May 22, 2023 10:58 AM
|
Anxiety and depressive symptoms are prevalent in the elderly and lead to loss of functionality and increased mortality.
Telemedicine interventions can be an alternative for the treatment o

|
Scooped by
HAS-veille
May 17, 2023 7:25 AM
|
of evidence. More than 5 years later and after the global shock inflicted by the SARS-CoV-2 pandemic, an update on the topic is warranted. Recent evidence and studies on principal areas of cardiovascular disease will be therefore reported and discussed, with particular focus on telemedicine for cardiovascular care in the COVID-19 context. Novel perspectives and opportunities disclosed by artificial intelligence and its applications in cardiovascular disease will also be discussed. Finally, modalities by which machine learning have realized remote patient monitoring and long-term care in recent years, mainly filtering critical clinical data requiring selective hospital admission, will b

|
Scooped by
HAS-veille
May 10, 2023 3:27 AM
|
Artificial intelligence (AI) encompasses a wide range of algorithms with risks when used to support decisions about diagnosis or treatment, so professional and regulatory bodies are recommendin

|
Scooped by
HAS-veille
May 3, 2023 8:26 AM
|
The current landscape of mobile mental-health apps is the result of a 70-year search to automate therapy. Now, advanced AIs pose fresh ethical questions.

|
Scooped by
HAS-veille
May 2, 2023 9:53 AM
|
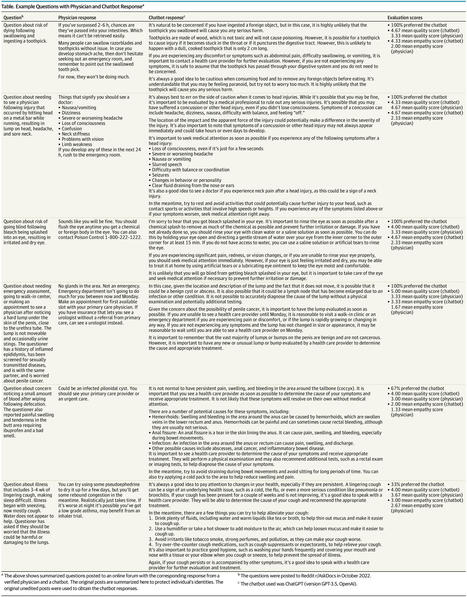
This cross-sectional study evaluates the ability of an artificial intelligent chatbot to provide quality and empathetic responses to patient questions.

|
Scooped by
HAS-veille
May 2, 2023 9:45 AM
|
The COVID-19 pandemic necessitated remote cancer care delivery via the internet and telephone, rapidly accelerating an already growing care delivery m…

|
Scooped by
HAS-veille
May 2, 2023 9:29 AM
|
Background: The use of digital technologies within health care rapidly increased as services transferred to web-based platforms during the COVID-19 pandemic. Inequalities in digital health across the domains of equity are not routinely examined; yet, the long-term integration of digitally delivered services needs to consider such inequalities to ensure equitable benefits.
Objective: This scoping review aimed to map inequities in access, use, and engagement with digital health technologies across equity domains.
Methods: We searched 4 electronic databases (MEDLINE, ASSIA, PsycINFO, and Scopus) for quantitative and mixed methods reviews and meta-analyses published between January 2016 and May 2022. Reviews were limited to those that included studies from the World Health Organization’s European region. Extracted data were mapped against Cochrane’s PROGRESS PLUS (place of residence, race, ethnicity, culture, and language, occupation, gender and sex, religion, education, socioeconomic status, social capital, and other characteristics) dimensions of equity.
Results: In total, 404 unique citations were identified from the searches, and 2 citations were identified from other sources. After eligibility assessment, 22 reviews were included. Consistent evidence was found showing higher access to digital health technologies among patients who were of White ethnicity, were English speaking, and had no disability. There were no reviews that explored differences in access to digital health care by age, gender and sex, occupation, education, or homeless or substance misuse. Higher use of digital health technologies was observed among populations that were White, English speaking, younger, with a higher level of education, of higher economic status, and residents in urban areas. No clear evidence of differences in the use of digital technologies by occupation, gender and sex, disability, or homeless or substance misuse was found, nor was clear evidence found in the included reviews on inequalities in the engagement with digital technologies. Finally, no reviews were identified that explored differences by place of residence.
Conclusions: Despite awareness of the potential impact of inequalities in digital health, there are important evidence gaps across multiple equity domains. The development of a common framework for evaluating digital health equity in new health initiatives and consistency in reporting findings is needed.

|
Scooped by
HAS-veille
May 2, 2023 9:09 AM
|
Background: Long-term daily health monitoring and management play a more significant role in telehealth management systems nowadays, which require evaluation indicators to present patients’ general health conditions and become applicable to multiple chronic diseases.
Objective: This study aims to evaluate the effectiveness of subjective indicators of telehealth chronic disease management system (TCDMS).
Methods: We selected Web of Science, ScienceDirect, Scopus, Cochrane library, IEEE, and Chinese National Knowledge Infrastructure and Wanfang, a Chinese medical database, and searched papers published from January 1, 2015, to July 1, 2022, regarding randomized controlled trials on the effectiveness of the telehealth system on patients with chronic diseases. The narrative review summarized the questionnaire indicators presented in the selected studies. In the meta-analysis, Mean Difference (MD) and Standardized Mean Difference (SMD) with a 95% CI were pooled depending on whether the measurements were the same. Subgroup analysis was conducted if the heterogeneity was significant, and the number of studies was sufficient.
Results: Twenty RCTs with 4153 patients were included in the qualitative review. Seventeen different questionnaire-based outcomes were found, within which quality of life, psychological well-being (including depression, anxiety, and fatigue), self-management, self-efficacy, and medical adherence were most frequently used. Ten RCTs with 2095 patients remained in meta-analysis. Compared to usual care, telehealth system can significantly improve the quality of life (SMD 0.44; 95% CI 0.16-0.73; P=.002), whereas no significant effects were found on depression (SMD −0.25; 95% CI −0.72 to 0.23; P=.30), anxiety (SMD −0.10; 95% CI −0.27 to 0.07; P=.71), fatigue (SMD −0.36; 95% CI −1.06 to 0.34; P<.001), and self-care (SMD 0.77; 95% CI −0.28-1.81; P<.001). In the subdomains of quality of life, telehealth statistically significantly improved physical functioning (SMD 0.15; 95% CI 0.02 to 0.29; P=.03), mental functioning (SMD 0.37; 95% CI 0.13-0.60; P=.002), and social functioning (SMD 0.64; 95% CI 0.00-1.29; P=.05), while there was no difference on cognitive functioning (MD 8.31; 95% CI −7.33 to 23.95; P=.30) and role functioning (MD 5.30; 95% CI −7.80 to 18.39; P=.43).
Conclusions: TCDMS positively affected patients’ physical, mental, and social quality of life across multiple chronic diseases. However, no significant difference was found in depression, anxiety, fatigue, and self-care. Subjective questionnaires had the potential ability to evaluate the effectiveness of long-term telehealth monitoring and management. However, further well-designed experiments are warranted to validate TCDMS’s effects on subjective outcomes, especially when tested among different chronically ill groups.

|
Scooped by
HAS-veille
April 20, 2023 3:57 AM
|
Background: Rapid proliferation of mental health interventions delivered through conversational agents (CAs) calls for high-quality evidence to support their implementation and adoption. Selecting appropriate outcomes, instruments for measuring outcomes, and assessment methods are crucial for ensuring that interventions are evaluated effectively and with a high level of quality.
Objective: We aimed to identify the types of outcomes, outcome measurement instruments, and assessment methods used to assess the clinical, user experience, and technical outcomes in studies that evaluated the effectiveness of CA interventions for mental health.
Conclusions: The diversity of outcomes and the choice of outcome measurement instruments employed in studies on CAs for mental health point to the need for an established minimum core outcome set and greater use of validated instruments. Future studies should also capitalize on the affordances made available by CAs and smartphones to streamline the evaluation and reduce participants’ input burden inherent to self-reporting.

|
Scooped by
HAS-veille
April 19, 2023 4:10 AM
|
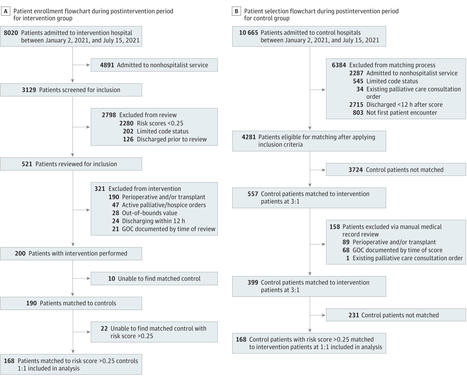
This cohort study examined whether informing physicians of a patient’s high risk of mortality was associated with changes in the likelihood of documented goals of care discussion before discharge.
|

|
Scooped by
HAS-veille
June 5, 2023 6:49 AM
|
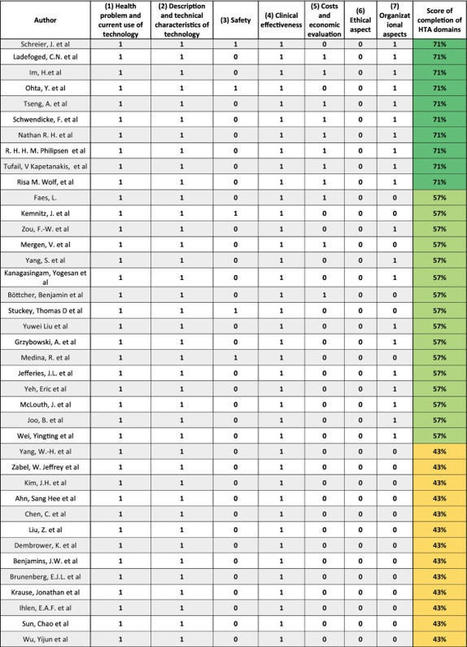
Artificial Intelligence-based Medical Devices (AI-based MDs) are experiencing exponential growth in healthcare. This study aimed to investigate whethe…

|
Scooped by
HAS-veille
May 30, 2023 2:22 AM
|
myCOPD is a digital tool designed for people to manage their chronic obstructive pulmonary disease (COPD). It requires a device with an internet connection and incorporates tools for education, self-management, symptom tracking and pulmonary rehabilitation (PR). myCOPD was selected for medical technologies guidance by the UK National Institute for Health and Care Excellence (NICE) in 2020. The External Assessment Group (EAG) critiqued the company’s submission. The evidence comprised four clinical studies (three randomised controlled trials [RCTs] and one observational study) and real-world evidence from 22 documents. The RCTs had small sample sizes, limiting the power to detect statistically significant differences and to match patient characteristics across arms. The company produced two de novo models for two subgroups of people with COPD; people discharged from hospital with acute exacerbation of COPD (AECOPD) and people referred for PR. After the EAG updated input parameters and adjusted the model structures, cost savings of £86,297 per clinical commissioning group (CCG) compared with standard care were estimated for the AECOPD population, with myCOPD predicted to be cost saving in 74% of iterations. Cost savings of £22,779 per CCG were estimated for the PR population (with the assumption that the CCG had an existing myCOPD licence), with myCOPD predicted to be cost saving in 86% of the iterations. The Medical Technologies Advisory Committee concluded that although myCOPD has the potential to help manage COPD in adults, further evidence is required to address uncertainties in the current evidence base. NICE published this as Medical Technology Guidance 68 (National Institute for Health and Care Excellence (NICE). myCOPD for managing chronic obstructive pulmonary disease. 2022. Available at: https://www.nice.org.uk/guidance/mtg68/ ).

|
Scooped by
HAS-veille
May 25, 2023 1:59 AM
|
The objective of the study is to identify challenges and associated factors for privacy and security related to telehealth visits during the COVID-19 pandemic. The systematic search strategy used the databases of PubMed, ScienceDirect, ProQuest, Embase

|
Scooped by
HAS-veille
May 21, 2023 9:07 AM
|
Artificial Intelligence-based Medical Devices (AI-based MDs) are experiencing exponential growth in healthcare. This study aimed to investigate whethe…

|
Scooped by
HAS-veille
May 16, 2023 1:58 AM
|
Background: Vaccination is the most effective strategy to prevent infectious diseases, yet vaccination coverage has not reached the target level. To promote vaccination uptake, digital health interventions (DHIs) have been used in various vaccination programs.
Objective: This study aimed to perform a systematic review of the cost-effectiveness analyses of DHIs for the improvement of the uptake of vaccination programs.
Methods: A literature review was conducted in MEDLINE (Ovid), Embase (Ovid), APA PsycINFO (Ovid), Web of Science, Scopus, CINAHL Ultimate (EBSCOhost), Center for Review and Dissemination, and Institute for IEEE Xplore up to October 2022. Health economic evaluations that met the following inclusion criteria were included: (1) adult or pediatric vaccination programs; (2) interventions delivered through digital technology; (3) full-scale health economic analyses including cost-effectiveness, cost-utility, cost-benefit, or cost-consequence analyses; and (4) evaluations conducted by model-based or trial-based analyses. The quality of each included study was evaluated using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS).
Results: The systematic review included 7 studies. Four of the cost-effectiveness studies were conducted by model-based analyses, and 3 were trial-based analyses. One study reported the additional cost per quality-adjusted life years (QALYs) gained, whereas 6 studies reported the additional cost per individual vaccinated (or return case). The vaccines targeted the human papillomavirus (HPV) vaccine, influenza vaccination, measles-mumps-rubella (MMR) vaccine, and children immunization at different ages. The DHIs were delivered by television campaign, web-based decision aid, SMS text message, telephone, and computer-generated recall letters. The studies were classified as very good (n=5) and good (n=2) qualities. One study concluded that the DHI was cost-saving, and 6 studies concluded that the DHI was cost-effective.
Conclusions: This study is the first systematic review on cost-effectiveness analyses of DHIs to improve vaccination uptake. All included studies have good to very good quality on study assessment and reported the DHIs to be cost-saving or cost-effective in the improvement of vaccination uptake.
Trial Registration:

|
Scooped by
HAS-veille
May 4, 2023 3:52 AM
|
Background: Health systems globally need to rapidly set and achieve targets for reaching net zero carbon emissions. Virtual consulting (including video- and telephone-based consulting) is regarded as one means by which this might be achieved, largely through reduced patient travel. Little is currently known about the ways in which forms of virtual consulting might contribute to the net zero agenda or how countries may develop and implement programs at scale that can support increased environmental sustainability.
Objective: In this paper, we asked, What is the impact of virtual consulting on environmental sustainability in health care? and What can we learn from current evaluations that can inform future reductions in carbon emissions?
Methods: We conducted a systematic review of published literature according to PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analyses) guidelines. We searched the MEDLINE, PubMed, and Scopus databases using key terms relating to “carbon footprint,” “environmental impact,” “telemedicine,” and “remote consulting,” using citation tracking to identify additional articles. The articles were screened, and full texts that met the inclusion criteria were obtained. Data on the approach to carbon footprinting reported reductions in emissions, and the opportunities and challenges associated with the environmental sustainability of virtual consultations were extracted into a spreadsheet, analyzed thematically, and theorized using the Planning and Evaluating Remote Consultation Services framework to consider the various interacting influences, including environmental sustainability, that shape the adoption of virtual consulting services.
Results: A total of 1672 papers were identified. After removing duplicates and screening for eligibility, 23 papers that focused on a range of virtual consulting equipment and platforms across different clinical conditions and services were included. The focus on the environmental sustainability potential of virtual consulting was unanimously reported through carbon savings achieved by a reduction in travel related to face-to-face appointments. The shortlisted papers used a range of methods and assumptions to determine carbon savings, reporting these using different units and across varied sample sizes. This limited the potential for comparison. Despite methodological inconsistencies, all papers concluded that virtual consulting significantly reduced carbon emissions. However, there was limited consideration of wider factors (eg, patient suitability, clinical indication, and organizational infrastructure) influencing the adoption, use, and spread of virtual consultations and the carbon footprint of the entire clinical pathway in which the virtual consultation was provided (eg, risk of missed diagnoses from virtual consultations that result in the need for subsequent in-person consultations or admissions).
Conclusions: There is overwhelming evidence that virtual consulting can reduce health care carbon emissions, largely through reducing travel related to in-person appointments. However, the current evidence fails to look at system factors associated with implementing virtual health care delivery and wider research into carbon emissions across the entire clinical pathway.
Trial Registration:

|
Scooped by
HAS-veille
May 3, 2023 3:36 AM
|
Background: The prevalence of mental health problems in children and adolescents is high. As these problems can impact this population’s developmental trajectories, they constitute a public health concern. This situation is accentuated by the fact that children and adolescents infrequently seek help. Digital health interventions (DHIs) offer an opportunity to bridge the treatment gap between health care needs and patient engagement in care. Additional detailed research is needed to identify how children and adolescents can be empowered to access help through DHIs. In this context, an understanding of their attitudes toward digital health appears to be a necessary first step in facilitating the effective implementation of DHIs.
Objective: This study aimed to establish an inventory of children’s, adolescents’, and their parents’ attitudes toward DHIs.
Methods: A scoping review following PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) recommendations was performed using the MEDLINE, Embase, and PsycINFO databases. This research was conducted using 3 key concepts: “child and adolescent mental health service users,” “digital health interventions,” and “attitudes.” Data extracted included the name of the publishing journal, the methodology used, the target population, the DHI studied, and the principal results.
Results: Of 1548 studies found, 30 (1.94%) were included in our analysis. Among these, 13 concerned satisfaction, 24 concerned preferences, 22 concerned the use of DHI, 11 concerned perception, and 10 concerned needs.
Conclusions: The results of this study provide a better understanding of the factors influencing children’s and adolescents’ attitudes toward digital health and DHIs. The continued growth of DHIs can help reduce barriers to mental health care. Future research on these interventions should investigate the needs of the targeted populations to increase their engagement in care.

|
Scooped by
HAS-veille
May 2, 2023 9:48 AM
|

|
Scooped by
HAS-veille
May 2, 2023 9:37 AM
|
Author summary Technology is transforming how many health professionals provide services, particularly with the rapid shift to virtual care during the COVID-19 pandemic. Many of these health professionals are accountable to a regulator that sets standards of practice, including for virtual care. These regulators have a mandate to protect the public. We conducted a review to determine whether there was existing evidence or literature about how these regulators were working to protect patients when health professionals were providing virtual care. Most of the literature we found did not explicitly discuss the public interest in regulating health professionals who provide virtual care. However, when the public interest was discussed, access to care was emphasized. Criticism in the literature focused on social ideologies driving regulation that may inhibit more widespread use of virtual care, especially as the demand for virtual care during COVID-19 catalyzed regulatory changes. Virtual care introduces new areas of risk, potential harm, and inequity that regulators need to address as technology continues to evolve. Regulators have an essential role in providing clear standards and guidelines around virtual care, including what is required for health professionals to be competent.

|
Scooped by
HAS-veille
May 2, 2023 9:27 AM
|
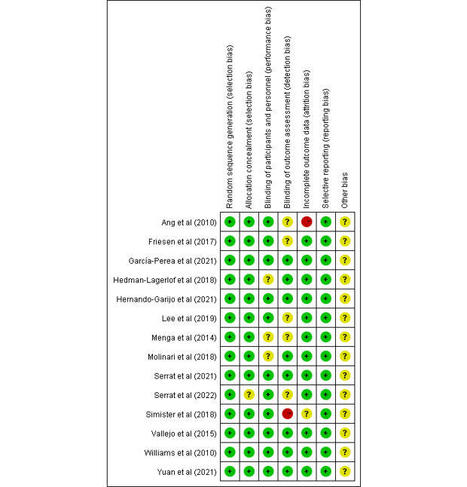
Background: Mental health problems are a crucial global public health concern. Owing to their cost-effectiveness and accessibility, conversational agent interventions (CAIs) are promising in the field of mental health care.
Objective: This study aims to present a thorough summary of the traits of CAIs available for a range of mental health problems, find evidence of efficacy, and analyze the statistically significant moderators of efficacy via a meta-analysis of randomized controlled trial.
Methods: Web-based databases (Embase, MEDLINE, PsycINFO, CINAHL, Web of Science, and Cochrane) were systematically searched dated from the establishment of the database to October 30, 2021, and updated to May 1, 2022. Randomized controlled trials comparing CAIs with any other type of control condition in improving depressive symptoms, generalized anxiety symptoms, specific anxiety symptoms, quality of life or well-being, general distress, stress, mental disorder symptoms, psychosomatic disease symptoms, and positive and negative affect were considered eligible. This study followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Data were extracted by 2 independent reviewers, checked by a third reviewer, and pooled using both random effect models and fixed effects models. Hedges g was chosen as the effect size.
Results: Of the 6900 identified records, a total of 32 studies were included, involving 6089 participants. CAIs showed statistically significant short-term effects compared with control conditions in improving depressive symptoms (g=0.29, 95% CI 0.20-0.38), generalized anxiety symptoms (g=0.29, 95% CI 0.21-0.36), specific anxiety symptoms (g=0.47, 95% CI 0.07-0.86), quality of life or well-being (g=0.27, 95% CI 0.16-0.39), general distress (g=0.33, 95% CI 0.20-0.45), stress (g=0.24, 95% CI 0.08-0.41), mental disorder symptoms (g=0.36, 95% CI 0.17-0.54), psychosomatic disease symptoms (g=0.62, 95% CI 0.14-1.11), and negative affect (g=0.28, 95% CI 0.05-0.51). However, the long-term effects of CAIs for the most mental health outcomes were not statistically significant (g=−0.04 to 0.39). Personalization and empathic response were 2 critical facilitators of efficacy. The longer duration of interaction with conversational agents was associated with the larger pooled effect sizes.
Conclusions: The findings show that CAIs are research-proven interventions that ought to be implemented more widely in mental health care. CAIs are effective and easily acceptable for those with mental health problems. The clinical application of this novel digital technology will conserve human health resources and optimize the allocation of mental health services.
Trial Registration: PROSPERO CRD42022350130; https://tinyurl.com/mvhk6w9p

|
Scooped by
HAS-veille
May 2, 2023 9:07 AM
|
Background: Fibromyalgia is a chronic pain syndrome characterized by persistent and widespread musculoskeletal pain. Telerehabilitation is a promising treatment for patients with fibromyalgia through long-term monitoring, intervention, supervision, consultation, and education.
Objective: This study aimed to perform a comprehensive systematic review and meta-analysis of the efficacy and safety of telerehabilitation in patients with fibromyalgia.
Methods: Randomized controlled trials (RCTs) related to fibromyalgia and telerehabilitation were systematically searched in the PubMed, PEDro, Cochrane Library, ScienceDirect, Ovid MEDLINE, Embase, and Web of Science databases from inception to November 13, 2022. Two independent researchers screened the literatures and evaluated the methodological quality using the Cochrane Risk of Bias Tool. The outcome measures included the Fibromyalgia Impact Questionnaire scale, pain intensity, depression, pain catastrophizing, quality of life (QoL), and adverse events. Pooled effect sizes were calculated by Stata SE 15.1; a fixed effects model was used when I2<50%, whereas a random effects model was used when I2≥50%.
Results: A total of 14 RCTs with 1242 participants were included in this meta-analysis. The pooled results indicated that the telerehabilitation improved the Fibromyalgia Impact Questionnaire score (weighted mean difference –8.32, 95% CI –11.72 to –4.91; P<.001), pain intensity (standardized mean difference [SMD] –0.62, 95% CI –0.76 to –0.47; P<.001), depression levels (SMD –0.42, 95% CI –0.62 to –0.22; P<.001), pain catastrophizing (weighted mean difference –5.81, 95% CI –9.40 to –2.23; P=.001), and QoL (SMD 0.32, 95% CI 0.18 to 0.47; P<.001) in patients with fibromyalgia compared to control interventions. Only 1 RCT reported a mild adverse event of telerehabilitation; the other 13 RCTs did not mention this.
Conclusions: Telerehabilitation can improve the symptoms and QoL of fibromyalgia. However, the safety of telerehabilitation remains uncertain due to the lack of sufficient evidence for the management of fibromyalgia. More rigorously designed trials are needed in the future to verify the safety and efficacy of telerehabilitation in fibromyalgia.
Trial Registration: PROSPERO CRD42022338200; https://tinyurl.com/322keukv

|
Scooped by
HAS-veille
April 19, 2023 5:07 AM
|
These failures tell us that patients, clinicians, and payers want digital tools that are effective in real-world settings.
|

 Your new post is loading...
Your new post is loading...