“Medicine is not your life. Your identity is more than just being a doctor,” he advises. Every person has a story to tell. “There’s not a story that’s not worth telling,” Zeeshan affirms. It’s worth sharing yours.
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

 Your new post is loading... Your new post is loading...
 Your new post is loading... Your new post is loading...
Visit Crain's Chicago Business for complete business news and analysis including healthcare, real estate, manufacturing, government, sports and more.
Studies indicate people with chronic conditions want to use mHealth devices at home for care management, but the devices and apps they’re trying are too complex or confusing. More than 100,000 (health) applications are now available in the leading app stores, and the assortment is constantly growing,” says a BAEK study that was discussed at the congress. But only a fraction of the programs are certified as medical products.Mobile health apps for smartphones and tablet computers are especially popular with young people. And demand is rising. There’s a caveat, though. An app can never replace a doctor – at best it can only supplement one, but the problem is that too many patients may be relying on apps that have not been medically tested. The other problem is that many mobile app developers are lax when it comes to data privacy. Users should be careful not to thoughtlessly share personal information. Chronic Conditions…A report from digital health analyst Parks Associates indicates 27 percent of those surveyed with a chronic condition want a mobile health device that tracks their condition – yet significant numbers also report that the devices they now have are too complicated to use or don’t work properly. A lot of patients simply do not have a good grasp on health metrics – meaning they either don’t know what their current health metrics are, or they do not know what they should be, the survey noted. Plus, even when patients do know their numbers, it is not guaranteed that they understand what those numbers mean. To make sense of health metrics and chronic disease management, patients need support from their healthcare providers. Accuracy Issues?An independent study of 18 popular mHealth sensors used by people with diabetes finds that two-thirds aren’t meeting standards for accuracy, potentially putting those users at risk. The analysis of 18 FDA-approved blood glucose monitoring systems (BGMSs) by the Diabetes Technology Society found that only six meters recorded blood glucose levels within 15 percent of mg/dl of the laboratory value in at least 95 percent of the tests. In layman’s terms, this means a person with diabetes can be confident that a blood glucose reading is accurate 19 times out of 20. Compared with the traditional method of in-office visits, does self-monitoring of blood glucose (SMBG) via digital tools result in better health and wellness for people with non-insulin-treated type 2 diabetes? In the case of a 450-person cohort studied at 15 primary care practices across the University of North Carolina, Chapel Hill health system, the answer was a flat “No.” The patients were randomized into three different groups. Two groups were given the Telcare connected blood glucose monitor, with one of those groups simply checking in with the device and the other doing the same plus receiving “enhanced patient feedback” (in the form of automated, one-way messages delivered directly on the meter). The third group did not receive a device. After the patients were randomized into groups, their primary care clinicians worked with them to manage their conditions, with those whose patients were using the Telcare devices receiving a summary of the data via their electronic health records. Researchers were measuring outcomes based on hemoglobin A1c levels and health-related quality of life. Over a year’s time, there were no significant differences in hemoglobin A1c levels nor health-related quality of life over all three groups. “Incorporating technology into self-management activities has been touted as potentially transformative for patients, and to date some smaller studies support this notion. However, our findings do not,” the researchers wrote in an article published by the Journal of the American Medical Association. Pharma may have the solutionCan you imagine a mHealth app developed by pharma that had been clinically tested to show that it provided both accurate data and improved patient outcomes? It would ne recommended by physicians and insurers alike and I’m sure widely adopted. mHealth developers need to work closely with pharma R&D people yo better understand the clinical trial process. Via Plus91, Giuseppe Fattori
The benefits of virtual-working are plentiful. The following strategies look at motivating virtual teams on a team and personal level. Via COUCH Medcomms
The use cases of artificial intelligence (AI) and machine learning could create more personalized engagement for mental healthcare.
While social media use in healthcare has the potential to bring value to patient-provider relationships, it is not without its ethical and professional challenges. This presentation looks at those challenges and suggests ways to deal with them. Via Marie Ennis-O'Connor, Tanja Juslin, Giuseppe Fattori
Early signs from the FDA point to an agency that seems motivated to move quickly and, ultimately, reinvent itself in the eyes of entrepreneurs, investors, and industry stakeholders.
As telemedicine and virtual care become more ubiquitous in healthcare, providers that occupy the traditional brick-and-mortar model of providing care will have to learn to strike a balance with new digital entrants aimed at improving consumer access, similar to the way Amazon changed the dynamics of the retail industry.
Artificial intelligence, wearable sensors, virtual reality, medical robots are changing the way patients and doctors think and act about healthcare.
A team of researchers from Stanford University, working with cardiac monitoring company iRhythm, have created an AI algorithm that, in a small proof-of-concept trial, outperformed board-certified cardiologists at identifying various types of arrhythmias from ECGs.
Via Olivier Delannoy
A study by researchers at the Dartmouth-Hitchcock Medical Center in New Hampshire, US found that 72% of fresh urology graduates had public Facebook profiles of which 40% contained “potentially objectionable” content. Many have examined the implications of HCPs utilising social media
Maintaining a healthy work-personal life balance
Via Plus91, Marie Ennis-O'Connor
Why Wellness Is the New Way to Look, Feel, and Act Rich
Oscar Health will partner with the Cleveland Clinic to offer individual coverage in Ohio on the public exchange under the Affordable Care Act. |
July 11, 2017 - Patient experience and patient satisfaction are healthcare terms that are too often used interchangeably. Although they appear to be synonymous – a patient’s hospital experience should be satisfactory, one might assume – they are in fact separate terms that have entirely different meanings to healthcare professionals. Via Lionel Reichardt / le Pharmageek
From
hbr
They need focused strategies and operational discipline.
Ethnographical studies can help in generating patient insights that allow pharma and HCPs to fill the gap between treatment and improved patient outcomes. Via COUCH Medcomms
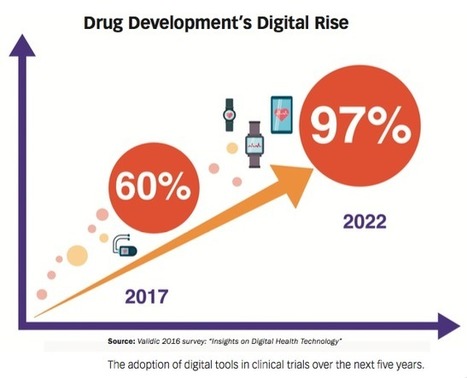
Outlining the four core elements pharma companies need to lay the foundation for a solid digital health infrastructure.
Low-income individuals with high BP were less likely to take their medication when their physician did not ask them about social issues or did not engage in collaborative communication, according to recent findings. “Despite advances in treatments for [CV] risk factors such as hypertension, poorly controlled BP continues to be a significant public health problem in the United States,” Via Richard Meyer
A drop of blood analyzed by a telemedicine tool means that patients will soon track the development of their pathology and stay connected to their doctor for better healthcare and a more personalized treatment.
Via Philippe Marchal
The Pediatric Insider © 2017 Roy Benaroch, MD Competition often works. Competing dry cleaners or donut shops must either improve the quality of their product or keep their prices low, or customers will go somewhere else for their cruller fix. In time, the better businesses – the ones that provide tastier pastries at a lower…
Hospitals remain high profile and high value targets for ransomware attacks. We’re not a cyber security company, but clients are concerned about safety.
NewYork-Presbyterian is expanding its telemedicine reach. It has launched Pediatric Urgent Care, a new telehealth offering that's part of NYP OnDemand.
Physicians have practiced precision medicine, defined as the tailoring of medical treatment by taking into account individual differences in people’s genes, environments and lifestyles, for decades. The main difference today is that technological advances have given us greater power to combine comprehensive data collected over time about an individual tohelp provide appropriate care.
Further reading: Here's how physicians can impact healthcare policies
The precision medicine initiative, now known as the All of Us Research Program, launched by the National Institutes of Health, is an ambitious effort to gather data for over a million people living in the U.S. It will likely accelerate precision medicine research with the goal of eventually benefiting everyone by providing information that healthcare providers can use in the clinic. However, there are aspects of precision medicine that have emerged, or are beginning to emerge, in different clinics across the country and are being used to benefit patients today. Pharmacogenomics (PGx), the study of genetic variations that cause individuals to respond differently to medications, is the most widely used form of precision medicine today. Virtually all of us harbor at least one genetic change that predisposes us to metabolize a common medication differently than the average person. A PGx panel with multiple genes can provide gene-drug guidelines for dozens of medications, including common ones like Warfarin, Clopidogrel or various antidepressants.
Trending on our site: Waiting on Congress to fix healthcare could be hazardous to physicians
Via Giuseppe Fattori
Data has become a valuable tool and a foundation for healthcare to build its services and products. PSFK’s new Future of Health report identifies six
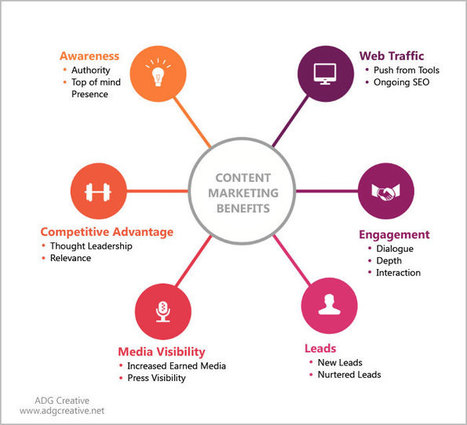
Modern times demand modern rules. And healthcare marketing is no exception. The market is constantly evolving, leading to a seismic shift in healthcare marketing trends. Here are a few |