Your new post is loading...
 Your new post is loading...

|
Rescooped by
Gilbert C FAURE
from Immunology and Biotherapies
March 17, 2019 10:23 AM
|
Abstract
While allergen immunotherapy (AIT) for IgE-mediated diseases holds curative potential, the considerable heterogeneity in clinical outcomes may relate to the complex mechanisms of tolerance. The regulation of humoral immunity by AIT contributes to the suppression of allergic responses. Recent findings have revealed novel roles for IgA and IgG antibodies in the induction of tolerance. These mechanisms synergize with their ability to block allergen-IgE binding and mediate inhibitory signaling of effector cells of the allergic response. In addition, the regulatory activity of B cells in AIT extends beyond IL-10 secretion and induction of IgG4. Here, we review the evolution of the B cell response during AIT with special emphasis on the novel protective mechanisms entailing humoral immunity.
Keywords
B cell immunity Allergen immunotherapy Blocking IgG antibodies IgA response B regulatory cells Allergy
Via Krishan Maggon

|
Suggested by
Société Francaise d'Immunologie
February 20, 2019 4:02 AM
|
Abstract A 60‐year‐old female with severe bronchial asthma developed persistent dyspnoea and an abnormal lung shadow. High‐resolution computed tomography (HRCT) demonstrated patchy ground‐glass opacities and diffuse, small nodular shadows. Elevated percentages of eosinophils were observed in the blood and bronchoalveolar lavage fluid. These results collectively indicated that her asthma was accompanied by eosinophilic pneumonia and eosinophilic bronchiolitis. Although previous, rare case reports suggest that systemic steroid therapy is necessary and effective for the control of eosinophilic bronchiolitis, we chose to treat her with an anti‐interleukin 5 antibody, mepolizumab. Her asthma, eosinophilic pneumonia, and eosinophilic bronchiolitis each improved in response to mepolizumab as assessed from her symptoms, pulmonary function tests, and HRCT. Mepolizumab might be effective not only for asthma and eosinophilic pneumonia but also for eosinophilic bronchiolitis. Introduction There have been a few case reports of eosinophilic bronchiolitis that is characterized by radiographic findings showing diffuse bronchiolitis plus massive accumulation of eosinophils in the airways 1-4. It has been suggested that systemic steroid therapy is effective for this disorder, although the precise pathogenesis in unknown. Here, we report a case of severe asthma complicated with eosinophilic pneumonia and eosinophilic bronchiolitis, all of which were alleviated by anti‐interleukin 5 (IL‐5) antibody. Case Report A 60‐year‐old female was referred to the outpatient clinic of Teikyo University Hospital for evaluation of persistent dyspnoea and an abnormal lung shadow. She had been diagnosed with bronchial asthma 10 years earlier. Although she continued to use medium‐ or high‐dose inhaled corticosteroid (ICS) plus a long‐actingβ2 agonist (LABA), leukotriene receptor antagonist (LTRA), and sustained‐release theophylline, the asthma frequently flared up, and short‐term oral corticosteroid bursts were needed. One year before referral, diffuse small nodular shadows were seen on chest X‐rays, suggesting the possibility of bronchiolitis. On the day of her first visit to our clinic, she complained of persistent dyspnoea both at rest and on exertion and presented expiratory wheezes. Her fractional exhaled nitric oxide (FeNO) was clearly elevated (72 ppb). Blood tests showed eosinophilia (790/μL), elevated serum total IgE (1280 IU/mL), and positivity for specific IgEs against house dust mites and aspergillus. Serum autoantibodies, including myeloperoxidase–anti‐neutrophil cytoplasmic antibody (ANCA) and proteinase 3‐ANCA, were negative. A chest X‐ray showed diffuse small nodular shadows and irregular pulmonary infiltration shadows (Fig. 1A). High‐resolution computed tomography (HRCT) images demonstrated a tree‐in‐bud appearance and patchy ground‐glass opacity (GGO) in both lung fields (Fig. 1B), suggesting the presence of bronchiolitis and pneumonia. Sinus computed tomography (CT) showed non‐specific mild maxillary sinusitis but no ethmoid sinusitis. After starting inhalation of tiotropium, a muscarinic antagonist, her asthma symptoms improved slightly, although a pulmonary function test clearly indicated airflow obstruction (Fig. 1C). Bronchoscopic examination found that the bronchial mucosa was oedematous, and the bronchoalveolar lavage (BAL) fluid showed an elevated percentage of eosinophils (28.5%) but not neutrophils. A biopsy specimen of the right B8 distal bronchial mucosa showed massive infiltration of eosinophils, detachment of airway epithelial cells, and thickening of subepithelial fibrosis, but no Charcot‐Leyden crystals were observed (Fig. 1D). These findings resulted in a diagnosis of bronchial asthma, eosinophilic pneumonia, and eosinophilic bronchiolitis. As her symptoms persisted, we decided to start treatment with mepolizumab, an anti‐IL‐5 antibody, two months after her first visit to our hospital. Her dyspnoea gradually improved, and her blood eosinophil counts were controlled at low levels, although FeNO remained high (Fig. 2A). HRCT images indicated that GGO had disappeared, and the thickening of the bronchial mucosa observed in the initial HRCT images had become milder (Fig. 2B, C). The tree‐in‐bud appearance and thickening of centrilobular shadows, suggesting bronchiolitis, were also alleviated. A spirogram showed improvement in both restrictive abnormality (percent vital capacity (%VC): 70.9% before mepolizumab; 94.8% after introduction of mepolizumab) and obstructive impairment (forced expiratory volume in 1 second (FEV1): 0.99 L before mepolizumab; 1.45 L after introduction of mepolizumab) (Fig. 2A). The residual volume/total lung capacity (RV/TLC), a useful index of air trapping in relation to small airway involvement, was initially as high as 46.9% (two months after mepolizumab was started), but it gradually improved with time to 44.4% (after four months on mepolizumab) and then 40.4% (after 10 months).Oral steroid bursts were not necessary during treatment with mepolizumab. Discussion Eosinophilic bronchiolitis is a relatively new disorder, first reported in 2001 1. So far, around 10 cases of this disorder have been reported; all of them displayed chronic progression of respiratory symptoms including cough, sputa, and dyspnoea at rest and exertion. This disorder is characterized by unique radiological findings, i.e. diffuse micronodular shadows and a tree‐in‐bud appearance, suggesting bronchiolitis and eosinophilia in both blood and pulmonary examinations 1-4. The clinical features of our case are in line with those findings for eosinophilic bronchiolitis. Thus, we believe that the diagnosis of eosinophilic bronchiolitis is correct for the present case. Accumulating evidence suggests that eosinophilic bronchiolitis is often accompanied by various other eosinophilic disorders 2, 5. Bronchial asthma is the most commonly reported disease accompanying eosinophilic bronchiolitis, as seen in our case, who also had eosinophilic pneumonia. In this patient, the findings of diffuse bronchiolitis on CT images were dominant and very striking, and we felt that they could not be regarded as features of bronchial asthma. The patient was thus diagnosed with a combination of asthma and eosinophilic bronchiolitis. We suppose that her asthma, eosinophilic pneumonia, and eosinophilic bronchiolitis might be mutually related, and these disorders collectively gave rise to cough, dyspnoea, and clear impairment of pulmonary function. It is important to note that BAL analysis may not be useful for distinguishing eosinophilic bronchiolitis as other disorders also demonstrate a similar increase in eosinophils. The previous case reports on eosinophilic bronchiolitis suggested that oral corticosteroid was an effective and standard therapy, whereas ICS was not. Importantly, discontinuation of oral corticosteroid was difficult, and long‐term administration of systemic steroid was thus unavoidable 1, 3, 4. For our patient, however, we chose a new anti‐IL‐5 antibody, mepolizumab, as her asthma was severe, and she strongly requested an additional effective anti‐asthma drug other than systemic steroid. As a result, not only her asthma but also her eosinophilic pneumonia and eosinophilic bronchiolitis responded to mepolizumab: her symptoms improved, as did the findings of lung function and imaging studies. Her clinical course suggests that IL‐5 may have been critically involved in the pathogenesis of all of her eosinophilic disorders, including eosinophilic bronchiolitis. As there have not been many reports of eosinophilic bronchiolitis, we have limited evidence regarding the pathogenesis and standard therapy for this disorder. In view of recent robust progress in the field of allergology, further accumulation of basic and clinical information on eosinophilic bronchiolitis is anticipated. That information will contribute to the further confirmation of this clinical entity, e.g. whether eosinophilic bronchiolitis is a unique disorder or just a continuum of the pathological process of asthma and the therapeutic strategy for it, and to our overall understanding of eosinophilic lung diseases. Disclosure Statement Appropriate written informed consent was obtained for publication of this case report and accompanying images. Acknowledgments We thank Ms Yasuko Asada for her excellent secretarial work. References

|
Scooped by
Gilbert C FAURE
January 26, 2019 1:30 PM
|

|
Scooped by
Gilbert C FAURE
December 18, 2018 1:07 PM
|
Abstract The potential of precision medicine in allergy and asthma has only started to be explored. A significant clarification in the pathophysiology of rhinitis, chronic rhinosinusitis, asthma, food allergy and drug hypersensitivity was made in the last decade. This improved understanding led to a better classification of the distinct phenotypes and to the discovery of new drugs such as biologicals, targeting phenotype‐specific mechanisms. Nevertheless, many conditions remain poorly understood such as non‐eosinophilic airway diseases or non‐IgE–mediated food allergy. Moreover, there is a need to predict the response to specific therapies and the outcome of drug and food provocations. The identification of patients at risk of progression towards severity is also an unmet need in order to establish adequate preventive or therapeutic measures. The implementation of precision medicine in the clinical practice requires the identification of phenotype‐specific markers measurable in biological matrices. To become useful, these biomarkers need to be quantifiable by reliable systems, and in samples obtained in an easy, rapid and cost‐efficient way. In the last years, significant research resources have been put in the identification of valid biomarkers for asthma and allergic diseases. This review summarizes these recent advances with focus on the biomarkers with higher clinical applicability. Highlights The implementation of precision medicine in allergic diseases requires a further clarification of disease phenotypes and endotypes allowing the identification of valid biomarkers. Many of the biomarkers of allergic diseases identified to date still require validation in larger cohorts and distinct geographical areas. Multidimensional approaches have a greater potential to identify valid biomarkers for allergic and chronic respiratory diseases. 1 INTRODUCTION Precision medicine for allergic diseases requires a deep understanding of immunopathology and phenotype heterogeneity in relation to clinically significant outcomes.1 Precision medicine could also help to limit the socio‐economic burden imposed by allergic and chronic respiratory diseases.2 According to the National Institutes of Health (NIH), precision medicine is an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment and lifestyle for each person. In this regard, asthma and allergic conditions are ideally suited, as they represent umbrella entities comprising different diseases partially sharing immune mechanisms (endotypes) and presenting similar visible properties (phenotypes), but requiring individualized approaches for a better risk prediction and the identification of treatment responders.3 The implementation of precision medicine demands measurable indicators of biological conditions usually termed biomarkers. A valid biomarker should be quantifiable in an analytical system with well‐defined performance and need to be supported by a body of evidence which sufficiently clarifies the pathological and clinical significance of the test results.4 Moreover, the identification of novel biomarkers applicable in daily practice requires clear clinical models with well‐established extreme phenotypes, allowing a better understanding of the disease progression along its severity. Another aspect influencing the clinical applicability is the biological matrix (“sample type”) where biomarkers are measured (Table 1). Appropriate matrices should be easy to obtain, store and manipulate in standardized and reproducible measuring protocols at a reasonable cost. Moreover, in most cases a single biomarker will not adequately represent the complexity of mechanisms underlying multifactorial diseases. In this regard, the generation of multidimensional biomarker panels displays a greater potential to identify valid markers.5 The ideal biomarker Supported by a body of evidence clarifying its biological significance Quantifiable in a cost‐efficient analytical system with well‐defined performance Detectable in a biological matrix obtained in an easy, rapid and cost‐efficient way The research efforts in asthma and allergic diseases during the last decades have focused on the identification of biomarkers applicable in clinical practice. Although several markers of allergic inflammation (e.g, IgE, eosinophilia, fractional exhaled nitric oxide [FENO]) have been described, their utility in diagnosis, prognosis and therapy is still controversial.6-8 Different types of molecules (genes, metabolites, etc.) have been also proposed as biomarkers for allergic and chronic respiratory conditions. Some of them display good analytical properties, but overall, they are insufficiently robust to be extrapolated to clinical practice. This fact partially arises from a paucity of clinical models for allergic diseases, which clearly constitutes a limiting factor in the search for biomarkers. This review will summarize the biomarkers identified to date for allergic and chronic respiratory conditions, with special focus on those with higher clinical applicability. 2 NEW METHODS TO IDENTIFY BIOMARKERS: THE OMICS The different omics characterize and quantify biological molecules, which share a common feature and which provide information about the structure and function of organisms. Omics are significantly contributing to the definition of disease endotypes and phenotypes and to the identification of therapeutic targets. Recent technological advances have pushed the omics field forward by allowing higher throughputs, improving detection limits and providing software tools to analyse and visualize the data. Genomics, transcriptomics and epigenetics have been used to identify genes, RNA sub‐types and DNA modifications, respectively. Nevertheless, the validation of these observations requires the investigation of their functional consequences (e.g, the effect in transcription or splicing variants or in the functionality of proteins). Only this step permits valid conclusions for the underlying mechanisms of disease phenotypes (Figure 1). Metabolomics investigates the nature and concentration of the metabolites generated in living systems and is among the most recent approaches applied to allergy research. Metabolomics displays a high degree of versatility, as it is applicable to a great variety of matrices, whose nature can be tailored to the disease of interest.4, 7 In chronic respiratory diseases, the metabolic analysis of exhaled breath condensate seems a promising matrix for biomarker identification. Other approaches which could help phenotype chronic airway conditions include electronic nose (eNose) or nuclear magnetic resonance–based metabolomics.7 Nevertheless, the lack of standardized procedures for breath sampling, the effect of pH on some metabolites and the low concentrations are well‐established limiting factors. Individual omics display both strengths and weaknesses which overall define the validity and robustness of the results. The development of multi‐omics and multi‐matrix platforms in integrated approaches will probably provide a more holistic picture of biological situations, including allergic and chronic respiratory diseases. Nevertheless, the implementation of these advances in clinical practice requires the identification of biomarkers measurable in biological fluids obtained in an easy, rapid and cost‐efficient way. 3 UPPER AND LOWER AIRWAY DISEASES 3.1 Rhinitis Chronic rhinitis is generally divided into allergic rhinitis (AR) and non‐allergic rhinitis (NAR).9 The NAR category comprises a heterogeneous group of diseases mediated by immune or neurogenic mechanisms.10 Conversely, AR is a relatively homogeneous entity arising from IgE‐mediated inflammation.11 Local allergic rhinitis (LAR) is a disease phenotype not fitting into the AR‐NAR dichotomy.12 The skin prick test (SPT) and/or serum allergen–specific (s)IgE and the nasal allergen challenge (NAC) positively identify AR patients. Subjects with LAR are defined by a positive NAC with negative SPT and serum sIgE, whereas NAR patients test negative for the three biomarkers. Several inflammatory cells and mediators may also serve as diagnostic biomarkers for AR. Eosinophils, IL‐5, IL‐6, IL‐13 and macrophage inflammatory protein (MIP)‐1β increase in the nasal lavage of AR patients following NAC,13 while elevated nasal endothelin (ET)‐1 and CCL17 at baseline discriminate AR from NAR individuals.14 Compared to healthy controls, subjects with house dust mite (HDM)–induced AR have increased circulating group 2 innate lymphoid cells (ILC2), which also correlate with serum IL‐13 and symptom scores.15 Allergen immunotherapy (AIT) is an effective treatment for AR16 and LAR17, 18 but involves considerable time and cost. Biomarkers assisting the selection of patients most likely to respond to AIT have recently been summarized.16 A proportion of sIgE to total IgE >16.2% predicted AIT success with 97.2% sensitivity and 88.1% specificity.19 In children, low serum osteopontin identifies responders to sublingual immunotherapy.20 Serum osteopontin and basophil reactivity increase after NAC21 and diminish following successful AIT.16 Moreover, subcutaneous immunotherapy with HDM armed peripheral T regulatory cells with the ability to inhibit Th2 and Th9 proliferation.22 3.2 Chronic rhinosinusitis Chronic rhinosinusitis (CRS) is defined by nasal and sinus mucosal inflammation. Phenotyping of CRS is typically based on the presence (CRSwNP) or absence (CRSsNP) of nasal polyps on endoscopy or CT scan, whereas examination of nasal samples facilitates the endotyping (Figure 2). In Caucasian populations, nasal polyps generally show an eosinophilic infiltrate, whereas fewer than 50% of Asian patients display eosinophilic polyps.23, 24 One study identified ten CRS clusters, of which six exhibited a type 2 inflammatory profile with raised IL‐5 and eosinophilia. Type 2 clusters displayed a higher risk of nasal polyps and asthma.25 The CRSwNP phenotype has been also associated with increased ILC2 at both the tissue level and peripheral blood.26, 27 Several matrices have been used to predict CRS prognosis. Blood and tissue eosinophilia correlates with severity as measured by endoscopy and CT scan28 and can predict recurrence following endoscopic sinus surgery.23 In addition, a small study observed that programmed cell death‐1 (PD‐1) mRNA expression in nasal polyp tissue correlated with disease severity on CT scan,29 while tissue gene expression of the eosinophil marker—Charcot‐Leyden crystal protein—was associated with higher olfactory impairment.30 The level of IL‐5 and P‐glycoprotein in nasal secretions helped to predict the olfactory and the CT scan scores, respectively.31 Nasal nitric oxide (nNO) inversely correlated with CT scan‐graded severity and increased after sinus surgery.32 3.3 Asthma Asthma phenotypes are classified into those displaying dominant type 2 inflammation, and those without significant type 2 inflammation,33 with each group comprising a number of different diseases (Figure 3). Several biomarkers measurable in different matrices have been described for these asthma phenotypes. The relevance of asthma endotyping is perfectly illustrated by the case of the anti‐IL‐5 monoclonal antibody (mAb) mepolizumab whose initial lacklustre performance in unclassified asthma34 was followed by excellent outcomes when administered to patients with eosinophilic asthma.35 In any individual, the disease expression may be driven by complex endotypes with numerous mechanistic pathways3; therefore, multidimensional biomarker assessment may be required. Unsupervised statistical analyses examining various blood inflammatory mediators identified unique clusters with different clinical and pathological features. Cluster analysis using sputum mediators at exacerbation also identified distinct biologic clusters with differences in host microbiome. The subsequent paragraphs describe individual biomarkers according to their biological matrices in more detail. 3.4 Diagnostic biomarkers 3.4.1 Blood cells Peripheral blood eosinophilia and neutrophilia in asthma have been associated with different clinical characteristics, with neutrophilia indicating increased sputum production.36 In asthma, neutrophilia is also more prevalent among patients with a smoking history and persistent airflow limitation compared to non‐smoking asthma patients (4.5 × 109 vs 3.6 × 109 cells/L),37 suggesting that neutrophilia may differentiate between patients with asthma alone from those with features of asthma‐chronic obstructive pulmonary disease (COPD) overlap (ACO) syndrome. Several genes regulating immune cells such as B lymphocytes, T lymphocytes and granulocytes were up‐ or down‐regulated in severe asthma compared to healthy controls.38 In a paediatric asthma cohort, the expression of five selected genes on CD4 lymphocytes (SRM, HDAC2, SLC33A1, P2RY10 and ADD3) predicted the atopic status with 100% sensitivity and 81.3% specificity,39 while in another paediatric study, a fourteen‐gene signature (MCEMP1, AQP9, PGLYRP1, S100P, RNASE2, OLFM4, CAMP, CEACAM8, LCN2, MPO, DEFA4, ELANE, BPI, DEFA1B, CTSG, HBD, ALAS2, RPS4Y2 and RPS4Y1) was unique to a neutrophilic phenotypic cluster.40 In a recent pilot study, circulating blood microRNA profile (expressed as miRNA ratios) showed promise in differentiating allergic asthma from healthy controls.41 Lipidomic profile and gene expression after low molecular weight hyaluronic acid stimulation of peripheral blood mononuclear cells were also shown to be different in severe asthma compared to mild asthma and healthy controls.42 Peripheral differential cell counts can also serve as surrogate markers of airway inflammation. In a meta‐analysis of 14 studies, the ability of blood eosinophils to predict airway eosinophilia showed an area under the curve (AUC) of 0.78.43 Enumeration of peripheral ILC2 has a similar utility for predicting sputum eosinophilia.44 Conversely, blood neutrophilia is less indicative of sputum neutrophilia, with an AUC of only 0.6.45 The ex vivo response of blood neutrophils and eosinophils to stimulation with N‐formyl‐methionyl‐leucyl‐phenylalanine (fMLP), in combination with relevant clinical parameters, is also able to predict sputum eosinophilia.46 3.4.2 Serum mediators The chitinase‐like protein YKL‐40 distinguished asthma from COPD and healthy controls.47 Neutrophil expression of Siglec‐9 is increased in patients with COPD and may have future potential to diagnose asthma.48 Serum (soluble‐cleaved) urokinase plasminogen–activated receptor (scuPAR) was found to be higher in severe, non‐atopic asthma in a single study49 and requires confirmation in further studies. Blood mediators can also predict airway inflammation. Overall, serum periostin moderately correlated with sputum eosinophilia.50, 51 Eosinophilic cationic protein (ECP) is more predictive of sputum eosinophilia than serum IgE,39 whereas C‐reactive protein (CRP) is weakly associated with sputum neutrophilia.52 3.4.3 Sputum cells and mediators Sputum quantitative cell count is a reference standard for airway inflammation in asthma. Four inflammatory phenotypes have been described—eosinophilic, neutrophilic, mixed granulocytic and paucigranulocytic. The neutrophilic subtype has been associated with the obese female asthma non‐type 2 phenotype.52 The Unbiased Biomarkers for the Prediction of Respiratory Disease Outcomes (UBIOPRED) study is a multicentre prospective cohort study recruiting patients with severe asthma in various European countries. Sputum analysis of the UBIOPRED cohort identified 3 transcriptome‐associated clusters (gene clusters), corresponding to eosinophilic, neutrophilic and paucigranulocytic phenotypes, respectively.53 A six‐gene signature (CLC, CPA3, DNASE1L3, IL1B, ALPL and CXCR2) can differentiate asthma patients from controls and distinguish between eosinophilic from neutrophilic asthma.54 This method has a practical advantage over sputum differential cell counts, as frozen samples can be batched for processing. Neutrophil myeloperoxidase in sputum has the potential to differentiate ACO from asthma.55 Specific microRNAs can discriminate neutrophilic from eosinophilic asthma.56 Sputum eosinophil peroxidase (EPX) correlates with sputum eosinophilia,57 as does nasal and pharyngeal EPX.58 Importantly, nasal sampling may be particularly useful for patients in whom sputum induction is unsafe or not possible. 3.4.4 Cellular bronchial samples Patients in the UBIOPRED cohort could be divided into four groups based on the expression of nine gene sets in bronchial cells, each with mixed inflammatory patterns including one with concomitant Th2 and Th17 markers.53 Interestingly, a different study found that Th2 and Th17 gene expression signatures were mutually exclusive in asthmatic airway tissue.59 The authors suggested that suppression of Th2 activity by corticosteroids may accentuate Th17 activity. Different gene signatures for Th2 and Th17 activities were used in the two studies, possibly limiting direct comparisons. The interplay between Th2 and Th17 cells is also likely to be complex, and the exact relationship between the two is still uncertain.60 3.4.5 Exhaled breath The FENO displays an AUC of 0.8 for asthma diagnosis.2 Of note, very high or low cut‐offs for FENO can, respectively, rule‐in or rule‐out asthma.27 Conversely, FENO has limited utility to predict sputum eosinophilia,43 as it is confounded by corticosteroid treatment, atopy and smoking status. Volatile organic compounds (VOCs) in exhaled breath can be readily measured using eNose devices. Building on previous work which discriminates between COPD and asthma, eNose has identified label‐free clinical and inflammatory clusters among asthma and COPD patients.61 VOCs and other metabolites in exhaled breath can also differentiate asthma from healthy controls in adults and children.62-65 In a paediatric study, metabolomic analysis using nuclear magnetic resonance (NMR) of exhaled breath condensate identified three clusters with different inflammatory profiles based on global spectral patterns of NMR.66 3.4.6 Urine Urine metabolite analysis can accurately discriminate between asthma and COPD67 and also correlates with FENO and blood eosinophilia.68 3.5 Prognostic biomarkers 3.5.1 Blood cells Raised blood eosinophils strongly predict the risk of asthma exacerbations in both adults and children.69, 70 Blood eosinophilia also predicts longitudinal lung function decline, irrespective of smoking status.71 Blood neutrophilia is linked with airway infections in asthma11 as well as poor symptom control and increased exacerbations.72 Circulating blood fibrocytes correlate with asthma severity.73 3.5.2 Serum mediators The stability of serum periostin over disease progression facilitates its use as a biomarker.74 Elevated levels are associated with fixed and more severe airflow obstruction75, 76 and greater longitudinal lung function decline.77 Total serum IgE in children is associated with atopy, airway hyperresponsiveness (AHR) and bronchial wall thickening in CT scan.69 In both adults and children, YKL‐40 level correlates with severe asthma and poor lung function.78, 79 The expression of ten selected microRNAs (HS_108.1, HS_112, HS_182.1, HS_240, HS_261.1, HS_3, HS_55.1, HS_91.1, hsa‐miR‐604 and hsa‐miR‐638) was higher in children with severe asthma.80 3.5.3 Sputum cells and mediators Sputum neutrophilia and ILC2 27 are associated with asthma severity.81, 82 Changes in sputum eosinophilia reflect fluctuations in clinical asthma control.83 Human tumour necrosis factor–like weak inducer of apoptosis (TWEAK) is an inflammatory mediator whose level in sputum correlated with higher severity, poor symptom control and decreased lung function in children with non‐eosinophilic asthma.84 3.5.4 Cellular bronchial samples Bronchial neutrophilia is present in severe (compared to non‐severe) asthma, independent of oral corticosteroid (OCS) intake.85 Gene signatures analysed in endobronchial brushing and biopsy specimens predicted persistent airflow limitation in the UBIOPRED cohort.86 In bronchoalveolar lavage samples, elevated CD4+ cells expressing both IL‐4 and IL‐17 predicted greater asthma severity.69, 87 3.5.5 Exhaled breath In both children and adults, FENO correlates with greater AHR, airway obstruction and exacerbations.69, 88 Patients with FENO >45 ppb are at greater risk for suffering >2 asthma exacerbations/year.89 Electronic nose‐measured VOCs predicted the loss of asthma control upon withdrawal of inhaled corticosteroids (ICS).90 Reactive oxygen species (ROS) can also be detected in exhaled breath condensates of patients with asthma and has been shown to be suppressed by anti‐inflammatory agents.91 3.5.6 Functional imaging of lungs Functional imaging with hyperpolarized gas magnetic resonance of the lung can predict asthma outcomes; persistent ventilation defects were associated with poorer asthma control.92 Greater ventilation defects are also observed in patients with uncontrolled eosinophilic inflammation.93 3.6 Biomarkers for therapeutic response prediction and measurement 3.6.1 Blood cells Blood eosinophilia identifies asthma patients responding to therapies targeting type 2 inflammation. The post hoc analyses of randomized controlled trials with the anti‐IgE mAb omalizumab identified blood eosinophilia (≥300 cells/μL) as a predictor of greater response.94, 95 Nevertheless, this finding was not reproduced in a real‐life study.96 There is a direct correlation between blood eosinophilia and the response to mepolizumab,97 the anti‐IL‐5 receptor mAb benralizumab98 and the anti‐IL‐4 receptor mAb dupilumab.99 Blood eosinophilia may also predict and monitor the response to corticosteroids. Atopic children with eosinophilia ≥300 cells/μL respond better to ICS.100 A decrease in peripheral eosinophilia is observed with the up‐dosing of ICS,101 while titration of OCS to maintain blood eosinophilia <200 cells/μL improved asthma control.102 3.6.2 Serum mediators Elevated serum periostin predicts the response to omalizumab.75, 103 Interestingly, total serum IgE does not predict the response to omalizumab, despite this molecule being not only the drug target, but also the basis for its dose calculation.104 On the other hand, a reduction in serum‐free IgE after 16‐32 weeks on omalizumab is associated with a decrease in exacerbations over two years.81 3.6.3 Sputum Sputum eosinophilia ≥3% predicts response to corticosteroids105 and mepolizumab.35 Sputum eosinophilia as a guide for ICS therapy reduced exacerbations with no associated increase in the total ICS dose.106, 107 3.6.4 Exhaled breath In patients with symptoms suggestive of AHR, elevated FENO predicts response to ICS.108 A systematic review concluded that using FENO to guide ICS therapy in adults reduced the mild but not the severe exacerbations.109 Among children, FENO also showed unclear benefits on asthma outcomes.110 A FENO level >19.5 ppb also correlated with response to omalizumab.75 3.6.5 Urine Urine bromotyrosine correlates with corticosteroid responsiveness, and the predictive accuracy further improves when combined with high FENO levels.94 Despite the previous enumeration being made in a matrix‐related fashion, the complexity of most asthma phenotypes will require multidimensional approaches to identify valid biomarkers (Table 2). This aspect is exemplified by the greatest benefit from dupilumab being observed in asthma patients exhibiting both elevated peripheral eosinophilia and FENO.99 Diagnosis Prognosis Response prediction and monitoring Blood cells Distinguish asthma from COPD Blood neutrophil Distinguish asthma from healthy controls Gene expression Inflammatory phenotyping Blood eosinophils Blood neutrophils Responsiveness of blood neutrophils and eosinophils to fMLF Exacerbations Eosinophils Neutrophils Symptoms Neutrophils Lung function Eosinophils Asthma severity Fibrocytes Predict response to anti‐IL‐5 Eosinophils Predict response to ICS Eosinophils Monitor response to corticosteroids Eosinophils Blood mediators Distinguish asthma from COPD YKL‐40 Siglec‐9 Determine atopy status scuPAR Inflammatory phenotyping ECP CRP Lung function Periostin YKL‐40 Airway remodelling IgE Asthma severity IgE MicroRNA YKL‐40 Predict response to omalizumab Periostin Reduction in serum‐free IgE Sputum cells Inflammatory phenotyping Quantitative cell count Gene signature Lung function Neutrophils Asthma severity ILC2 Loss of asthma control Eosinophils Predict response to mepolizumab Eosinophils Predict response to corticosteroids Eosinophils Guide ICS titration Eosinophils Sputum mediators Distinguish asthma from COPD MPO Inflammatory phenotyping MicroRNA Sputum/nasal/pharyngeal EPX Asthma severity TWEAK Bronchial tissue Inflammatory phenotyping Gene expression Lung function Gene signatures Asthma severity Neutrophils Exhaled breath Asthma diagnosis FENO VOC Metabolites Inflammatory phenotyping eNose Exacerbations FENO Lung function FENO Loss of asthma control eNose Predict response to ICS FENO Guide ICS therapy FENO (in adults) Urine Distinguish asthma from COPD Metabolites Inflammatory phenotyping Urine metabolites Predict response to corticosteroids Urine bromotyrosine COPD, chronic obstructive pulmonary disease; CRP, C‐reactive protein; ECP, eosinophilic cationic protein; eNose, electronic Nose; EPX, eosinophil peroxidase; FENO, fractional exhaled nitric oxide; fMLF, N‐formyl‐methionyl‐leucyl‐phenylalanine; ICS, inhaled corticosteroid; IgE, immunoglobulin E; IL‐5, interleukin‐5; ILC2, group 2 innate lymphoid cell; LTE4, leukotriene 4; MPO, myeloperoxidase; NERD, aspirin‐exacerbated respiratory disease; scuPAR, serum soluble‐cleaved form of the urokinase plasminogen–activated receptor; Siglec‐9, sialic acid–binding immunoglobulin‐type lectins‐9; TWEAK, tumour necrosis factor–like weak inducer of apoptosis; VOC, volatile organic compounds. 4 FOOD ALLERGY AND ANAPHYLAXIS The food allergy (FA) phenotypes differ on their IgE dependence and prognosis (Figure 4).111 Given this heterogeneity, the search for FA biomarkers has gained significant attention.112 4.1 IgE‐mediated food allergy The identification of children at risk of developing FA might help establish preventive strategies.112 The balance between type 2 and type 1 chemokines in cord blood influenced the sensitization to food allergens at the age of 3 years in children from Taiwan.113 Atopic individuals often display skin prick test (SPT) positivity to foods they tolerate.112 Indoleamine 2,3‐dioxygenase (IDO) is a tryptophan‐catabolizing enzyme expressed by antigen‐presenting cells.114 A high IDO activity was associated with unresponsiveness to food allergens in sensitized children from Turkey.114 Molecular allergology is a useful tool to identify clinically relevant IgE sensitization.2, 112 Specific (s)IgE to the storage proteins Cor a 14 from hazelnut or Ana o 1, 2 or 3 from cashew, correlated with clinically relevant sensitization in children from Denmark115 and the Netherlands,116 respectively. These observations might facilitate the management of patients with FA by limiting the number of oral food challenges (OFC) necessary for diagnosis.64, 112 Interestingly, a score based on the value of sIgE to Ana o 3, the SPT wheal size and the gender of the patient was proposed to predict the outcome of cashew OFC in Dutch patients.117 Basophil activation test (BAT) might also correlate with the OFC outcome in food‐dependent NSAID‐induced anaphylaxis.118 Anaphylaxis is the most severe phenotype of IgE‐mediated hypersensitivity, and the increase in serum tryptase is a helpful biomarker in most cases.119 In Canadian children, milk was the food most likely to increase serum tryptase levels.119 Interestingly, the combination of the serum levels of apolipoprotein A1 and the prostaglandin D2 metabolite 9α,11β‐PGF2, displayed a good diagnostic performance for food‐induced anaphylaxis in German patients.120 Oral immunotherapy (OIT) is a promising tool for persistent forms of IgE‐mediated FA.111, 121-123 In anaphylactic children from the United States, successful milkOIT induced the increase in peripheral invariant natural killer T (iNKT) cells and skewed milk‐stimulated iNKT cells from a type 2 to a type 1 profile.124 Furthermore, successful OIT reduced blood eosinophils and increased several mediators functionally related to type 1 immunity (adipokines, leptin or resistin) in milk‐allergic children from Finland.125 A higher baseline sIgA and a rapid increase in sIgG1 after OIT initiation identified good responder egg‐allergic children from Japan.126 The adverse reactions (AdR) during OIT limit its use in the clinics.123 In children undergoing peanutOIT, the presence of allergic rhinitis and the SPT wheal size were associated with systemic and gastrointestinal AdR.127 Adjuvant therapy with omalizumab might reduce AdR during OIT,123 and the combination of basophil reactivity and sIgE/total IgE ratio at baseline could identify patients more likely to benefit from omalizumab during milkOIT.128 Beyond the oral route, other administration routes are under investigation for severe FA.123 Sublingual immunotherapy with Pru p 3, the lipid transfer protein from peach, induced anti‐inflammatory PDL‐1+ dendritic cells and IL‐10+ T regulatory cells in responder patients from Spain.129, 130 4.2 Other types of food allergy The diagnosis of eosinophilic esophagitis requires the demonstration of >15 eosinophils/high‐power field in the oesophagus of individuals with suggestive symptoms.131 Oesophageal eosinophilia correlated with male gender and the number of positive food sIgE tests in American children.132 This observation might help to limit the number of endoscopies required for diagnosis.131 The management of food protein‐induced enterocolitis syndrome (FPIE) patients involves consecutive OFCs to asses for disease resolution.133 In Japanese children with FPIES, the OFCs induced the activation of intestinal and peripheral eosinophils.134 Interestingly, the peripheral level of C‐reactive protein and of eosinophilia correlated with a poor and good prognosis, respectively, in Japanese patients with FPIES.135 Despite the progress made in recent years, most biomarkers remain to be validated in larger populations and distinct geographical areas. Moreover, growing evidence suggests that airway allergy influences many of the parameters identified as FA biomarkers.136, 137 In this regard, the clarification of atopic phenotypes and their relationship with FA will improve the interpretation of biomarkers.68, 138 5 DRUG HYPERSENSITIVITY A summary of the different drug hypersensitivity phenotypes can be seen in Figure 5. 5.1 Cross‐intolerance to NSAIDs Non‐steroidal anti‐inflammatory drugs (NSAIDs) are the most common triggers of drug hypersensitivity reactions, and in most cases, these reactions are not mediated by immunological mechanisms.139 In non‐selective or cross‐intolerant reactions, NSAIDs from different groups provoke skin or respiratory symptoms.140 In these cases, the reaction‐inducing potential does not rely on the chemical structure of the drug, but on its COX‐1 inhibitory activity.140 Aspirin‐ or NSAID‐exacerbated respiratory disease (AERD and NERD, respectively) is the most studied phenotype of cross‐intolerance. This entity is defined by the onset of respiratory symptoms upon intake of NSAIDs and is related to a dysregulation of arachidonic acid (AA) metabolism with overproduction of leukotrienes (LT) and prostaglandins (PG).141 Many NERD subjects have concomitant CRS and asthma.141 In a Korean study, NERD patients were divided into four sub‐phenotypes based on the presence of CRS, urticaria and atopy.142 Interestingly, significant differences existed in asthma severity, total serum IgE, sputum and peripheral eosinophilia, and urinary LTE4 (uLTE4).142 In American patients, uLTE4 helped to identify aspirin sensitivity in patients with different nasal inflammatory conditions.143 A recent meta‐analysis reported that the sensitivity and specificity of uLTE4 for identifying aspirin sensitivity in asthma ranged from 0.55 to 0.81 and from 0.77 to 0.82, respectively, depending on the detection method.144 Serum LTE4 in combination with LTE4/PGF2α ratio might help to detect NERD among other asthma phenotypes.145 Aspirin provocation increased 8‐iso‐PGE2 in the exhaled breath condensate of NERD patients and correlated with uLTE4.146 Platelet activation was also associated with overproduction of AA metabolites and to a reduced lung function in NERD patients.147 Other biomarkers beyond AA metabolites have been related to NERD. The serum sphingosine‐1‐phosphate was higher in NERD patients than in other asthmatics.148 American patients with NERD displayed higher activation of mast cells, basophils and platelets measured in nasal microparticles than other CRS individuals.149 Overall, these biomarkers might facilitate the diagnosis of NSAID hypersensitivity by decreasing the need for drug provocations. Some cross‐intolerance phenotypes resolve over time,150 and these biomarkers might help determine the most adequate timing to test for aspirin tolerance. 5.2 Immune‐mediated reactions These conditions can be divided into immediate and non‐immediate reactions arising from IgE‐ and T cell–mediated mechanisms, respectively (Figure 5).112 5.3 Immediate reactions Betalactams (BL) and fluoroquinolones (FQ) are the most common drugs involved in immediate reactions.139 5.3.1 Betalactams Skin testing displays a diagnostic sensitivity of up to 70%.151 Available in vitro tests include immunoassays to quantify serum BL‐sIgE, including the commercial ImmunoCAP© (Thermo‐Fisher, Uppsala, Sweden).151 Its sensitivity shows a high variability (0%‐50%),152 depending on the reaction severity and the time gap at the moment of measurement.153 Moreover, ImmunoCAP© can induce false‐positive results when testing for Penicillin‐V.154 Increased serum tryptase during the acute phase of reactions can confirm mast cell activation 112 and correlates with the severity.155 The sensitivity of BAT for BL allergy ranges from 22% to 55% with a specificity of up to 96%.156, 157 5.3.2 Fluoroquinolones Skin testing is not useful for the diagnosis of FQ allergy,158 and there are no available immunoassays. The CD63‐based BAT displayed 83.3% sensitivity and 88.9% specificity for ciprofloxacin allergy.159 Surprisingly, CD203c outperforms CD63 as BAT‐activation marker for moxifloxacin allergy, yet its sensitivity was low (36.4%).159, 160 These data question the role of basophils in moxifloxacin allergy, but identify BAT as a promising tool for ciprofloxacin allergy. 5.4 Non‐immediate reactions Patch testing and intradermal test with delayed reading are useful in vivo biomarkers. The sensitivity of the in vitro lymphocyte transformation test (LTT) is lower than that of BAT for immediate reactions.63, 155 A combination of granzyme B and granulysin expression in blood cells can detect lymphocyte activation in the setting of severe cutaneous reactions like Stevens‐Johnson syndrome.161 The screening for HLAB*57:01 before abacavir prescription is recommended by regulatory agencies,162 as it showed 100% of negative predictive value for immunologically confirmed abacavir hypersensitivity.163 The screening for HLAB*15:02 is also recommended before carbamazepine treatment in patients at high risk (Han Chinese, Vietnamese, Cambodians, etc.).164, 165 6 CONCLUSIONS The potential of precision medicine in the fields of allergy and chronic respiratory diseases has only started to be explored. A better definition of disease phenotypes and endotypes based on treatable traits and other clinically significant aspects is a prerequisite to progress in individualized therapies. In the last decade, we have seen an improvement in the definition of allergic respiratory disease, and we have gained insights into other eosinophilic phenotypes of rhinitis, CRS and asthma. This knowledge has translated into a significant broadening of therapeutic options, including (but not limited to) new biologicals. Because precision medicine needs to be performed in a cost‐efficient way, there is a need to identify responder patients to these new drugs. On the other hand, the available therapies for NAR and non‐eosinophilic CRS and asthma are much more limited, reflecting the important knowledge gaps in the pathophysiology of those phenotypes. Similarly, there is a need to progress in the definition of EoE and FPIES in order to improve the clinical management of the patients. The clarification of the disease mechanisms behind IgE‐mediated food allergy and drug hypersensitivity will help identify patients at risk of developing allergic reactions, limit the number of required provocations and establish preventive strategies. Nevertheless, the clarification of disease phenotypes per se does not guarantee the implementation of precision medicine in the clinical practice, as this step requires the detection of valid biomarkers. This search will be a long and resource‐consuming path requiring large population cohorts. Among the different disciplines applied to biomarker identification, metabolomics appears as a promising tool, yet growing evidence indicates that valid biomarkers will be detected by multidimensional strategies. Valid biomarkers do not only need to accurately reflect the phenotype‐specific disease mechanisms, but also to be quantifiable in a rapid, easy and cost‐efficient way. Only under these premises, the research in biomarker identification will be able to impact the clinical practice and translate into an improved diagnosis, management, and treatment of patients with allergic and chronic respiratory diseases. ACKNOWLEDGMENTS The present work has been supported by the Institute of Health “Carlos III” of the Spanish Ministry of Economy and Competitiveness (grants cofunded by the European Regional Development Fund (ERDF): thematic network and cooperative research centres ARADyAL RD16/0006/0001 and RD16/0006/0015, and research projects PI15/02256, PI16/00249, PI17/01318. This article has been also supported by research grants provided by the Regional Ministry of Health of Andalusia: PI‐0346‐2016 and PC‐0278‐2017. I Eguiluz‐Gracia holds a Rio Hortega research contract (CM17/00140) of the Institute of Health “Carlos III,” Spanish Ministry of Economy and Competitiveness (cofounded by the European Social Fund, ESF). CONFLICT OF INTEREST None of the authors have any conflict of interest in relation to this article. REFERENCES

|
Scooped by
Gilbert C FAURE
November 24, 2018 4:00 AM
|
Based on immunologic phenotypes underlying asthma, use of monoclonal antibody based therapies is becoming the new standard of care for severe, corticosteroid refractory clinical symptoms. Patients may qualify for one or more of these targeted treatments, based on clinical characteristics and approved indications. However, the statistics are not well characterized, particularly in the Canadian population. The objective of this observational study was to identify and describe the proportion of patients with severe asthma who were eligible for targeting IgE, IL-5, or both pathways of immunomodulation. We reviewed a cross-sectional cohort of patients in a Canadian Allergy and Immunology referral practice. We also compared demographic and clinical characteristics of each group. Of the 128 patients with severe asthma, 84 (66%) were eligible for omalizumab, 100 (78%) for mepolizumab, 52 (41%) for reslizumab, and 68 (53%) for benralizumab. Overlap in treatment eligibility varied; 68 (53%) patients were eligible for both omalizumab and mepolizumab, 47 (37%) were eligible for omalizumab and benralizumab, and 37 (29%) were eligible for all four medications. Patient demographics and clinical characteristics were similar, and levels of serum biomarkers varied based on locally approved prescribing criteria. In this severe asthma population from a Canadian Allergist’s practice, one-third of individuals qualified for all currently available biologics. 41–78% were eligible for at least one mAb. Patients were most likely to be eligible for mepolizumab. Objective assessments to determine asthma phenotype, along with further characterization of safety profiles will lead to further advances in asthma management.

|
Rescooped by
Gilbert C FAURE
from Mucosal Immunity
November 13, 2018 4:28 AM
|
In most industrialized countries, allergies have increased in frequency quite dramatically during the past 50 years. Estimates show that 20–30% of the populations are affected. Allergies have thereby become one of the major medical challenges ...

|
Scooped by
Gilbert C FAURE
November 6, 2018 6:43 AM
|
The clinical benefit of allergen-specific immunotherapy (AIT) involves induction of blocking antibodies. It is not clear if these antibodies function via steric hindrance alone or a combination of levels, avidities, and epitope specificities, and clinical outcome cannot be predicted. We aim to in-depth characterize serum antibody profiles during birch pollen AIT, investigate therapy-induced antibodies for their capacity to block IgE binding to Bet v 1 and correlate data with clinical outcomes. Immune responses of five birch pollen allergic patients were monitored during the first year of AIT by nasal provocation tests (NPTs), ImmunoCAP, immunoblots, direct and avidity enzyme-linked immunosorbent assays, mediator release assays, facilitated antigen binding (FAB) assays, and inhibition mediator release assays. There was no correlation between NPT results and therapy-induced changes in levels (IgE, IgG, IgA, IgM), avidities, or mediator release potency of Bet v 1-specific antibodies. In FAB assays, blocking antibodies initiated upon AIT were shown to prevent formation of Bet v 1-IgE complexes of an indicator serum pool and significantly correlated with clinical readout. Inhibition mediator release assays using patient-specific IgE for passive sensitization revealed therapy-induced blocking capacities with very good correlation to NPT results. Notably, this assay was the only one to detect a non-responder during treatment in this pilot study. Clinical outcome of AIT depends on induction of blocking antibodies able to prevent the patient’s own IgE from allergen binding. Monitoring of clinical efficacy seems to be best achieved using the inhibition mediator release assay, as development of relevant blocking antibodies can be verified in a patient-tailored manner.

|
Scooped by
Gilbert C FAURE
October 30, 2018 3:18 PM
|
<b><i>Background:</i></b> Allergic sensitisation towards cashew nut often happens without a clear history of eating cashew nut.IgE cross-reactivity between cashew and pistachio nut is well described;...

|
Scooped by
Gilbert C FAURE
October 16, 2018 1:52 AM
|
Allergen-specific immunotherapy (ASIT) has the potential to modify allergic diseases, and it is also considered a potential therapy for allergic asthma. House dust mite (HDM) allergens, a common source of airborne allergen in human diseases, have been developed as an immunotherapy for patients with allergic asthma via the subcutaneous and sublingual routes. Oral immunotherapy with repeated allergen ingestion is emerging as another potential modality of ASIT. The aim of this study was to evaluate the therapeutic efficacy of the oral ingestion of HDM extracts in a murine model of allergic asthma. BABL/c mice were sensitized twice by intraperitoneal injection of HDM extracts and Al(OH)3 on day 1 and day 8. Then, the mice received challenge to induce airway inflammation by intratracheal instillation of HDM extracts on days 29–31. The treatment group received immunotherapy with oral HDM extracts ingestion before the challenge. All the mice were sacrificed on day 32 for bronchoalveolar inflammatory cytokines, mediastinal lymph node T cells, lung histology, and serum HDM-specific immunoglobulins analyses. Upon HDM sensitization and following challenge, a robust Th2 cell response and eosinophilic airway inflammation were observed in mice of the positive control group. The mice treated with HDM extracts ingestion had decreased eosinophilic airway inflammation, suppressed HDM-specific Th2 cell responses in the mediastinal lymph nodes, and attenuated serum HDM-specific IgE levels. Oral immunotherapy with HDM extracts ingestion was demonstrated to have a partial therapeutic effect in the murine model of allergic asthma. This study may serve as the basis for the further development of oral immunotherapy with HDM extracts in allergic asthma.

|
Scooped by
Gilbert C FAURE
October 4, 2018 8:14 AM
|
Back to listingNews Scientists develop a new test to safely and accurately diagnose peanut allergies 3 May 2018 MRC scientists have developed a new laboratory test to diagnose peanut allergy. The test has 98% specificity and, unlike current options, it doesn’t run the risk of false-positives or causing allergic reactions such as anaphylactic shock. The simple blood test is five times more cost-efficient compared to the oral food challenge (OFC) – the standard food allergy test – and could be adapted to test for other food allergies. Peanut allergies are among the most common food allergies in children*. Currently, doctors diagnose peanut allergy using a skin-prick test or specific IgE test but this may result in over-diagnosis or false-positives and it cannot differentiate between sensitivity and true food allergy. When skin-prick and IgE test results are unclear, allergists rely on an OFC, which consists of feeding peanut in incrementally larger doses to a patient in a highly-controlled setting in hospital to confirm allergy to the food. While the test is the gold-standard for diagnosing food allergies, there is risk of causing severe allergic reactions. Now, the researchers have developed a safer, accurate blood test in the lab. The new test, called the mast activation test (MAT), could act as a second line tool when skin-prick test results are inconclusive and before referring children and their families to specialists for an OFC, according to researchers from the MRC & Asthma UK Centre in Allergic Mechanisms of Asthma. Their new study was published in the Journal of Allergy and Clinical Immunology. Dr Alexandra Santos, an MRC Clinician Scientist at King’s College London, paediatric allergist and study lead author, said: “The current tests are not ideal. If we relied on them alone, we’d be over diagnosing food allergies – only 22% of school-aged children in the UK with a positive test to peanuts are actually allergic when they’re fed the food in a monitored setting.” Dr Santos continued: “The new test is specific in confirming the diagnosis so when it’s positive, we can be very sure it means allergy. We would reduce by two-thirds the number of expensive, stressful oral food challenges conducted, as well as saving children from experiencing allergic reactions.” Food allergy symptoms are triggered when allergens interact with an antibody called immunoglobulin E (or IgE). The food allergens activate IgE antibodies, triggering symptoms such as skin reactions, itching or constricting of the mouth, throat and airways, and digestive problems (such as stomach cramps, nausea or vomiting). The current skin-prick test and IgE test, which have been in use for decades, measure the presence of IgE antibodies. The new test focuses on mast cells, which play a crucial role in triggering allergic reactions. Mast cells activate by recognising the IgE in plasma and, in allergic patients, produce biomarkers associated with allergic reactions, which can be detected in the lab. Using blood samples from 174 children participating in allergy testing – 73 peanut allergic and 101 peanut-tolerant – the scientists added peanut protein to mast cells to screen for IgE-mediated activation. The MAT accurately identified peanut allergy with 98 specificity. (Specificity is a statistical measure in determining efficacy for diagnosis. The MAT test rarely gives positive results in non-allergic patients.) The researchers also found the test reflected the severity of peanut allergy – patients with more severe reactions have a higher number of activated mast cells. The MAT test is five times cheaper to conduct than the OFC, which requires an allergist and specialist nurses on hand to monitor for adverse reactions and provide medical support if symptoms arise. Dr Santos said: “We are adapting this test to other foods, such as milk, eggs, sesame and tree nuts. This test will be useful as we are seeing more and more children who have never been exposed to these foods because they have severe eczema or have siblings with allergies. Parents are often afraid to feed them a food that is known to cause allergic reactions.” The researchers believe the MAT test may have other uses, for example, in the food industry to detect the presence of allergens in products. Pharmaceutical companies could use it to monitor patients’ allergic response to drugs being evaluated during clinical trials. The scientists plan to transition the biomarker test out of the laboratory and into a clinical setting. They will be testing blood samples from patients with suspected allergies to further validate its utility. 5 to 8% of UK children have a food allergy with up to one in 55 children having a peanut allergy, according to Food Standards Agency estimates. Current UK guidelines recommend avoiding giving your child peanuts and foods containing peanuts before the age of six months. Other countries, such as Canada and the United States, have updated their recommendations – a move that is in the works in the UK. The researchers say updated guidelines may result in a rise in requests for peanut allergy diagnosing. This paper is available on Europe PMC. Categories Categories: Research Health categories: Blood, Inflammatory, Respiratory, Generic Strategic objectives: Lifestyles affecting health, Environment and health, Securing impact from medical research, Aim: Picking research that delivers, Aim: Research to people, Aim: Supporting scientists Locations: London Type: News article

|
Scooped by
Gilbert C FAURE
September 18, 2018 12:01 PM
|
Welcome To 5 Strands® Affordable Testing 5 Strands® Affordable Testing provides a simple HAIR analysis test that measures food and environmental substances that cause non-IgE mediated reactions, known as INTOLERANCES. Reactions have a delayed onset with symptoms appearing several hours or days after ingestion or exposure and lasting a longer period of time. Common symptoms include eczema, bloating, diarrhea, constipation, and in more severe cases, pain, inflammation or weight problems. Our simple, non-invasive testing can quickly identify if your body is intolerant to over 650 food and environmental items. We can also test for metal/minerals and nutritional deficiencies. Our list of items tested is the most comprehensive of any test on the U.S. market today. This screening tool can help you make the dietary, environmental and lifestyle changes necessary to allow your symptoms to improve. 5 Strands® Affordable Testing scans your hair sample (10-15 strands) using bio -resonance technology and provides an extensive, easy-to-understand report. You can expect to receive your results within 5 – 7 days after the sample arrives at the processing center. Be aware that IgE (Immunoglobulin E) allergies, which are caused by the body’s immune system, are NOT measured by 5 Strands® Affordable Testing. This type of reaction, which represents only 2% of all allergic reactions, occurs within minutes of ingestion or exposure. Common symptoms range from hives, rash and swelling of the lips or face to swelling of the throat, wheezing, sudden shortness of breath and other potentially life-threatening reactions. IgE-mediated allergies are diagnosed through a blood test or skin prick test by healthcare professionals.

|
Scooped by
Gilbert C FAURE
August 21, 2018 6:36 AM
|
Immunoglobulin E (IgE)-mediated food allergy is a major issue that affects 2–10% of infants. Here the authors study the epigenetic regulation of the naive CD4+ T cell activation response among children with IgE-mediated food allergy finding epigenetic dysregulation in the early stages of signal transduction through the T cell receptor complex.

|
Scooped by
Gilbert C FAURE
June 24, 2018 5:12 AM
|
Immediate hypersensitivity reactions are induced by the interaction of allergens with specific IgE antibodies bound FcεRI to mast cells and basophils. W...
|

|
Scooped by
Gilbert C FAURE
March 9, 2019 1:31 PM
|

|
Rescooped by
Gilbert C FAURE
from Immunology and Biotherapies
February 18, 2019 2:03 AM
|
IgE‐mediated food allergy (FA) is a potentially life‐threatening condition with a negative impact on quality of life and an increasing prevalence in westernized countries in the recent two decades. A strict avoidance of the triggering food(s) represents the current standard approach. However, an elimination diet may be difficult and frustrating, in particular for common foods, (e.g. milk, egg, and peanut). Food allergy immunotherapy (FA‐AIT) may provide an active treatment that enables to increase the amount of food that the patient can intake without reaction during treatment (i.e. desensitization), and reduces the risk of potential life‐threatening allergic reaction in the event of accidental ingestion. However, several gaps need still to be filled. A memorable Latin orator stated: “Est modus in rebus” (Horace, Sermones I, 1, 106‐07). This sentence remembers that there is a measure in everything to a proper proportion of therapy. The common sense of measure should find application in each stage of treatment. A personalized approaching should consider the specific willing and features of each patient. Efforts are devoted to improve the efficacy, the safety but also the quality of life of patients suffering from FA. In the near future it will be important to clarify immunological pathways of FA‐AIT, and to identify reliable biomarkers in order to recognize the most suitable candidates to FA‐AIT and algorithms for treatments tailored on well‐characterized subpopulations of patients. This article is protected by copyright. All rights reserved.
Via Krishan Maggon

|
Scooped by
Gilbert C FAURE
December 30, 2018 1:54 PM
|
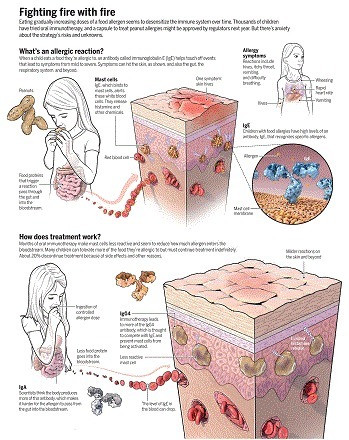
Changes in the human environment and activities over the past few decades have caused an epidemic of food allergies ([ 1 ][1]). People suffering from allergies often feel that they live on a cliff edge, as the allergens to which they react are potentially fatal ([ 2 ][2]). For example, tiny amounts of peanut picked up on skin or contaminating other foods can be dangerous to peanut-sensitized individuals ([ 2 ][2]–[ 4 ][3]). Immunoglobulin E (IgE) antibodies mediate the allergic response. They bind to specific receptors on inflammatory immune cells: mast cells in mucosal tissues lining body surfaces and cavities, and basophils in the circulation. These cells mediate allergic responses triggered by specific antigens (allergens) that are recognized by IgE. B cells expressing IgG antibodies have long served as the paradigm for the development of B cells into antibody-secreting plasma cells in the immune response. Until recently, the far less abundant IgE-expressing B cells have proved to be elusive. On page 1306 of this issue, Croote et al. ([ 5 ][4]) have analyzed single B cells from six individuals with peanut allergy, which enabled the identification of the natural Ig heavy- and light-chain pairs from IgE-expressing B cells that are responsible for peanut allergy. With this information they produced recombinant antibodies, identified the peanut allergen–specific antibodies, and used site-directed mutagenesis to suppress their activity. The mutated antibodies could be used to treat peanut allergy.
![Figure][5]
From sensitization to peanut allergy
Dendritic cells in the skin pick up peanut allergens and present them to peanut allergen–specific T helper 2 (TH2) cells, which in turn present them to B cells. Interaction between peanut allergen–specific TH2 cells and B cells solicits help from TH2 cells for B cell proliferation, somatic hypermutation and affinity maturation, class switching to IgE, and plasma cell differentiation. Allergen-specific IgE secreted by plasma cells binds to resident mast cells in the gut, so the ingestion of peanuts triggers an allergic reaction.
GRAPHIC: N. DESAI/ SCIENCE
Whole-exome sequencing of single B cells from peanut-allergic individuals yielded two principal components of gene expression, representing naïve or memory B cells and plasmablasts (the circulating precursors of plasma cells). The majority of Ig-Eexpressing cells were plasmablasts, whereas the majority of cells expressing IgG or IgA (the more abundant antibody classes) were naïve or memory B cells. It has previously been observed that IgE-expressing B cells tend to develop into the plasma cell lineage as opposed to the memory cell lineage. The IgE plasma cells inherit their antigen specificity from B cells of other antibody classes, which have undergone affinity maturation. This is advantageous for their biological function in immediate hypersensitivity to antigens as it cuts out the time that would be required for affinity maturation of IgE memory B cells ([ 6 ][6], [ 7 ][7]).
In immune responses, antigens bind to specific B cells expressing a membrane-bound form of the antibody [the B cell receptor (BCR)], which stimulates B cell maturation through the processes of somatic hypermutation (mutations affecting the antibody affinity for antigen) and affinity maturation (the selection of cells expressing BCRs with the highest affinity for antigen). The cells may also undergo class switching (from IgM to IgG, IgA, or IgE) to the most effective antibody class for a particular location in the body. IgE expression is needed for protection from parasites at barriers to the environment (airways, gut, skin). The cost of this elaborate immune mechanism is frequently the lack of normal tolerance to harmless allergens, causing allergy.
There is compelling clinical and experimental evidence that both IgE class switching and somatic hypermutation in humans occur transiently in the respiratory tract upon allergen stimulation ([ 8 ][8]–[ 10 ][9]). Whether primary contact with peanuts through the skin ([ 3 ][10], [ 4 ][3]) is followed by local class switching to IgE in the aerodigestive tract in food allergy remains to be investigated. Immediate hypersensitivity that is characteristic of allergic reactions mediated by IgE occurs in the gut as it does in the airways (see the figure). The IgE-expressing B cells isolated from blood by Croote et al. may represent peanut-specific cells that have migrated out of the tissue to other sites in the body where they continue to function ([ 10 ][9], [ 11 ][11]).
The authors focused on B cells that were of interest because the variable region sequences in six B cells from two of the six individuals studied were similar. Such similarity between individuals is highly improbable (one in 1014 potential sequences in the far fewer number of B cells that occur in each individual). The similarities suggest that the antigen-binding sequences are convergent or “public” sequences (inherited sequences that are conserved in evolution). Convergent sequences have been observed in infectious disease and in vaccination studies. A rationale is to hand: The relatively small germline gene repertoire encoding the Ig variable region sequences, compared to the repertoire resulting from somatic hypermutation and affinity maturation of the B cells, may have evolved in our ancestors to protect them against commonly encountered pathogens. Whether the conserved sequences serve the same purpose now or allergens are mistaken for the pathogens that affected our ancestors is unclear ([ 12 ][12]).
The six convergent clones were expressed as recombinant antibodies. This revealed high levels of somatic hypermutation, reflecting affinity maturation in the B cells specific for the three most common and clinically relevant peanut allergens, Ara h 1, Ara h 2, and Ara h 3. The coincidence of convergence and peanut specificity here is remarkable. Genetic mutagenesis gave insight into the crucial residues for activity, and this could be further understood through high-resolution crystal structure determination of the allergen-antibody complexes ([ 13 ][13]). One other B cell was shown to express an Ara h 3–specific IgE antibody. This cell was especially interesting because the IgE was related to an IgG4 (an IgG subclass) in the same cell. This confirms previous reports of related IgG4 and IgEs in allergy ([ 10 ][9]). IgG4 is an antibody class that confers tolerance to allergens by competing with IgE for specific antigens ([ 14 ][14], [ 15 ][15]) and is dramatically increased in specific allergen immunotherapy. It is reassuring that the immune system itself can operate a mechanism to prevent or ameliorate allergy, which can be exploited in the clinic.
Further research on these antibodies could lead to modified antibodies or antibody fragments that compete with IgE for allergen binding and prevent the allergic response. Future use of whole-exome sequencing, perhaps comparing the development of IgE-expressing plasma cells with those expressing other antibody classes, may identify genes that regulate IgE plasma cell development and survival that could be counteracted. The work of Croote et al. exemplifies a concerted approach to understanding and potentially intervening in allergic disease.

|
Scooped by
Gilbert C FAURE
December 4, 2018 4:09 AM
|
Abstract All body surfaces are exposed to a wide variety of microbes, which significantly influence immune reactivity within the host. This review provides an update on some of the critical novel findings that have been published on the influence of the microbiome on atopic dermatitis, food allergy and asthma. Microbial dysbiosis has consistently been observed in the skin, gut and lungs of patients with atopic dermatitis, food allergy and asthma, respectively, and the role of specific microbes in allergic disorders is being intensively investigated. However, many of these discoveries have yet to be translated into routine clinical practice. Abbreviations AAI allergic airway inflammation AD atopic dermatitis AHR airway hyper‐responsiveness AMP antimicrobial peptides COPD chronic obstructive pulmonary disease CRS chronic rhinosinusitis GCS glucocorticoids HDM house dust mite HMOs human milk oligosaccharides ICSs inhaled corticosteroids LABAs long‐acting β2 adrenergic receptor agonists OIT oral immunotherapy PARs protease‐activated receptors PSMs phenol‐soluble modulins RSV respiratory syncytial virus SCFAs short‐chain fatty acids TLR Toll‐like receptor 1 INTRODUCTION An enormous variety of microbes colonize the skin and mucosal body surfaces. These microbes are organized within complex community structures, utilizing nutrients from other microbes, host secretions and the diet. The microbiome is defined as the sum of these microbes, their genomic elements and interactions in a given ecological niche. In addition to bacteria, viruses are also considered to be an important component of the microbiome (virome). The composition of the microbiome is dependent on the specific body site examined, resulting in a series of unique habitats within and between individuals that can change substantially over time.1 This presents significant challenges to the local immune system, which should tolerate the presence of these microbes to avoid damaging host tissue while retaining the ability to respond appropriately to pathogens. The mechanisms that mediate host‐microbe communication are highly sophisticated and need to be constantly coordinated.2 Indeed, disrupted communication between the microbiome and the host due to altered microbiome composition and/or metabolism is thought to negatively influence immune homeostatic networks and may play a role in immune hypersensitivity to environmental exposures, such as allergens.3-5 For several years, epidemiological studies have suggested associations between the migration from traditional farming to urban environments, increase in processed food intake, lack of contact with animals and excessive hygiene practices with the increased incidence of asthma, atopic dermatitis and food allergy. However, it is only relatively recently that the importance of the gut, lung and skin microbiomes in regulation of immune tolerance and its aberrations in a variety of human diseases including allergy and asthma has been recognized.6, 7 In particular, early‐life events such as mode of delivery, breastfeeding, mother's diet and health status, antibiotics and other drug usage in pregnancy and early childhood, early‐life environment (ie, siblings, pets at home, proximity to farm animals and green areas) significantly influence the timing of bacterial colonization and establishment, which modify the risk of developing allergies and asthma, as summarized in Figure 1.8-17 In this review, we will highlight some of the recent advances in our knowledge regarding the influence of the microbiome on immune reactivity in the skin, gut and lungs of patients with atopic dermatitis, food allergy and asthma. In addition, we will discuss the potential translation and challenges associated with microbial‐based therapies in patients with these allergic disorders. 2 MICROBIOME IN ATOPIC DERMATITIS The skin microbiome is comprised of bacteria, fungi, viruses and archaeal communities, with bacteria being the most widely studied.18 The skin microbiome is influenced by age, gender, ethnicity, climate, UV exposure and lifestyle factors.19 16S ribosomal RNA (rRNA) sequencing has demonstrated that significantly diverse bacterial phyla exist on healthy skin with site‐specific differences in composition. This is primarily driven by the physiology of a skin niche. Propionibacterium species are predominantly found in sebaceous sites, with Corynebacterium and Staphylococcus species occurring in moist microenvironments. Malassezia represents the predominant fungal flora on human skin.20 Figure 2 illustrates the interactions between the skin microbiome and host cells. Atopic dermatitis (AD) is characterized by epidermal barrier dysfunction resulting from a synergistic decrease in epidermal barrier structural proteins, alteration in lipid composition and skin pH, activation of local and systemic inflammatory responses and decrease in skin microbiome diversity.19 Staphylococcus aureus overgrowth is consistently linked with AD pathogenesis and correlates with disease severity and eczematous flares.1, 21 High IL‐4 and IL‐13 levels within AD skin can deplete keratinocyte‐produced antimicrobial peptides (AMPs), cathelicidin LL‐37, human beta defensin hBD‐2 and hBD‐3, necessary for controlling pathogenic organisms.22 Defective TLR‐2 expression in Langerhans cells of AD skin has also been observed, which may contribute to the impairment in effective immune recognition and clearance of pathogenic bacteria such as S. aureus.23 Epidermal lipid composition strongly correlates with bacterial diversity and composition at typical sites for AD lesions. For example, S. aureus dominance was associated with elevated levels of ceramide AS.21 Staphylococcus aureus overgrowth with concomitant decline in Staphylococcus epidermidis is a general feature of AD and is not restricted to eczematous lesions.19, 21 Staphylococcus aureus colonization is evident in 90% of AD cases,24 associates with AD severity and increased allergen sensitization.25 Intervention studies with antimicrobials targeting S. aureus can reduce AD severity. Restoration of the epithelial barrier with anti‐inflammatory and emollient use is able to increase microbial diversity of lesional skin.1, 24 Patients with severe AD can be colonized with a single S. aureus strain, which persists even post‐eczematous flare albeit at a lower relative abundance. In contrast, S. epidermidis strains were more heterogeneous. Interestingly, patients with more severe AD were colonized with methicillin‐sensitive staphylococci, whereas less severe AD was more frequently associated with methicillin‐resistant strains. This observation may have significant treatment implications, particularly when methicillin‐sensitive S. aureus and methicillin‐resistant S. epidermidis strains are present.26 In a recent study, the skin microbiome of infants with AD showed a consistent absence of S. aureus sequences at multiple time points on lesional skin contrary to reported finding in patients with established AD. The most prevalent species were S. epidermidis and S. cohnii. However, those who developed AD at 12 months had significantly lower levels of these commensal staphylococci detectable at 2 months of age.27 This study suggests that S. aureus colonization may not always predate clinical AD and highlights the need for longitudinal studies to investigate the transition to microbial dysbiosis in AD. Commensal S. epidermidis strains can also increase during disease flares.24 Coagulase‐negative staphylococci (CoNS), which include S. epidermidis, S. hominis and S. lugdunensis, can secrete antimicrobials that limit S. aureus overgrowth and biofilm formation.1, 28 In addition, S. epidermidis activates TLR2, thereby promoting tight junction protein expression and inducing keratinocyte‐derived antimicrobial peptide secretion. Early occupation of the neonatal human skin by S. epidermidis is associated with induction of S. epidermidis‐specific FOXP3+ Treg cells that regulate local activation of host immune responses.29 Other members of the healthy skin microbiota, such as Propionibacterium, Streptococcus, Acinetobacter, Corynebacterium, Prevotella and Proteobacteria, are frequently reduced in AD patients.28, 30 Staphylococcus aureus can contribute to epidermal barrier disruption in a number of ways. Staphylococcus aureus downregulates terminal differentiation proteins such as filaggrin and loricrin, while secretion of proteases contributes to the disruption of the epidermal integrity via direct proteolytic activity or activation of protease‐activated receptors (PARs). Superantigens such as staphylococcal enterotoxins A and B or toxic shock syndrome toxin‐1 trigger a cytokine response that further disrupts the epidermal barrier. These enterotoxins also act as allergens, and toxin‐specific IgE contributes to cutaneous inflammation.28, 31 Staphylococcus aureus expresses exotoxins such as cytolytic α‐toxin, which damage keratinocytes, while β‐, γ‐ and δ‐toxins stimulate mast cell degranulation.28, 32 Phenol‐soluble modulins (PSMs) induce keratinocyte damage and secretion of the alarmins IL‐1α and IL‐36α, which further exaggerate skin inflammation.33 An impaired skin barrier results in increased exposure of the immune system to microbial components, resulting in a progressive cycle of inflammatory responses and tissue damage. It was recently suggested that reactivity to S. aureus can be facilitated via allergen co‐exposure and vice versa since patients with sensitization to house dust mite also show significantly more IgE reactivity to S. aureus and Escherichia coli, two abundant species in the house dust mite microbiome.34 A subset of AD patients is susceptible to eczema herpeticum (EH), and S. aureus may contribute to EH susceptibility as it has been shown to secrete products that enhance viral replication.1 Despite Malassezia species having a commensal role in healthy skin, in AD Malassezia may contribute to disease pathogenesis. Malassezia DNA has been detected in 90% of AD skin lesions, and colonization increases with disease severity.35 In addition, different Malassezia strains were found in AD and healthy individuals suggesting the existence of key pathogenic strains in AD.36 Higher levels of IgE sensitization to Malassezia have been detected in adult AD compared to healthy individuals and childhood AD.22, 36 Malassezia could contribute to AD pathogenesis by secreting immunogenic proteins that induce proinflammatory cytokines, expression of TLR2 and TLR4 on keratinocytes and induction of auto‐reactive T cells.22 Atopic dermatitis is considered a first step in the atopic diathesis, facilitated in part by the defective epidermal barrier of AD. The IL‐4/IL‐13 axis in AD is also thought to upregulate the pore‐forming claudin‐2 expression in the gut leading to barrier defects.19 In addition to the skin microbiota, AD has been associated with changes in the gut microbiota. Patients with AD have lower levels of Bifidobacterium in the gut compared to healthy controls, and Bifidobacterium levels were inversely correlated with AD disease severity.37 Several studies have shown that alterations in gut microbiota composition can precede the development of AD. Early gut colonization with C. difficile was associated with AD development,38 and low gut microbiota diversity and specifically low Bacteroidetes diversity at 1 month were associated with AD development at 2 years of age.35, 39 A recent whole‐metagenome analysis demonstrated a lower abundance of key metabolic pathways in AD children associated with depletion of mucin‐degrading bacteria such as Akkermansia muciniphila, Ruminococcus gnavus and Lachnospiraceae.40 These bacteria not only are able to influence immune development through directly influencing signalling pathways and antigen processing but also can lead to a reduced microbial diversity as these bacteria are able to degrade complex polysaccharides into short‐chain fatty acids (SCFAs)—nutrient sources that allow for gut colonization by other microbes.40 Dog exposure at birth was associated with a dose‐related reduced risk of AD in early life, suggesting that exposure to an environment rich in microbial components may be protective.41 In contrast, antibiotic exposure during the first 2 years of life is associated with an increased risk of AD.42 Infants with high faecal calprotectin levels (an antimicrobial protein used as a biomarker of intestinal inflammation) measured at 2 months of age had an increased risk of AD and asthma by 6 years of age. High faecal calprotectin was also shown to be inversely correlated with levels of E. coli. Reduced early colonization with E. coli was shown to impair IL‐10 regulation.43 3 MICROBIOME IN FOOD ALLERGY The human gut microbiome is increasingly being considered as a crucial factor in the development of food allergy, with a strong interrelation between the human gut microbiota, environmental factors, human genetics and gastrointestinal atopy.4, 44 In particular, the composition and metabolic activity of the gut microbiota are intimately linked with the development of oral tolerance.45, 46 Therefore, disturbed microbial homeostasis, especially early in life, appears to significantly influence allergic disease susceptibility. Figure 3 illustrates some of the known interactions between the gut microbiome and host mucosal cells. Recently, the oral bacterial composition in saliva samples from healthy and allergic children up to 7 years of age was described. The result confirmed that early changes in oral microbial composition seem to associate with immune maturation and allergy development.47 Milk‐allergic infants have higher total bacteria and anaerobic bacterial counts compared with healthy control children after 6 months of differential formula intake. In addition, higher proportions of Lactobacilli and lower proportions of Enterobacteria and Bifidobacteria were observed in 46 milk‐allergic infants.48 The spontaneous resolution of milk allergy in infants was associated with a specific gut microbiota composition.49 Bunyavanich et al showed that Clostridia and Firmicutes were enriched in the infant gut microbiome of subjects whose milk allergy spontaneously resolved. This result suggested that early infant gut microbiota may shape food allergy outcomes in childhood and bacterial taxa within Clostridia and Firmicutes species could be further investigated as probiotic candidates for milk allergy therapy.49 An additional study examining the gut microbiome of 141 children with egg allergy and healthy controls found that genera from Lachnospiraceae and Ruminococcaceae were associated with egg sensitization; however, there was no association between early‐life gut microbiota and egg allergy resolution by age 8 years.50 A prospective microbiome association study in 14 children with food allergy and 87 children with food sensitization showed that the genera Haemophilus, Dialister, Dorea and Clostridium were underrepresented among subjects with food sensitization, whereas the genera Citrobacter, Oscillospira, Lactococcus and Dorea were underrepresented among subjects with food allergy.51 An additional prospective study identified both temporal variation and long‐term variation in the differential abundance of specific bacterial genera in children developing IgE‐associated allergic disease, with Faecalibacterium correlating with IL‐10 and Foxp3 mRNA levels.52 Human milk oligosaccharides (HMOs) have been shown to be important in supporting the establishment of the infant gut microbiome as they are selective substrates for protective microbes such as Bifidobacteria.53 Two recent studies have described differences in HMO composition that are associated with cow's milk allergy or food sensitization.54, 55 One potential mechanism for this association is that different HMO profiles may support the establishment of different microbes early in life, thereby indirectly influencing immune maturation and education. In conclusion, a number of human studies now suggest that food allergy could be associated with changes in microbial exposures in early life, which modifies the development of host immunity and results in pathologic immune responses to food allergens. 4 MICROBIOME IN ASTHMA Composition of the microbiome at all mucosal sites changes dynamically in the first days, months and years of life. If the process of “healthy” and timely colonization is disrupted, the early‐life dysbiosis of the gut and lung becomes an important risk factor for atopy, allergy and asthma. In the Canadian Healthy Infant Longitudinal Development (CHILD) study, the lower relative abundance of the bacterial genera Lachnospira, Veillonella, Faecalibacterium and Rothia in the gut was associated with the development of asthma later in life and mechanistically linked with the reduced levels of faecal SCFAs.56 Another recent study also showed that high levels of SCFAs early in life were protective against later life sensitization and asthma.57 In a US birth cohort, lower relative abundance of Bifidobacterium, Akkermansia and Faecalibacterium, with higher relative abundance of Candida and Rhodotorula, in the gut of neonates significantly increased the risk of developing multisensitized atopy and asthma later in life.58 Interestingly, the faecal metabolome of those children at increased risk contained increased levels of pro‐inflammatory metabolites, among which 12, 13‐DiHOME was able to induce IL‐4 production in CD4+ T cells and decreased the abundance of Tregs.58 Increased abundance of nasopharyngeal Lactobacillus species during acute respiratory infection with respiratory syncytial virus (RSV) in infancy was associated with reduced risk of wheezing at 2 years of age.59 Colonization of the airways with Streptococcus, Moraxella or Haemophilus within the first 2 months of life was associated with virus‐induced acute respiratory infections in the first 60 weeks of life as well as increased risk of asthma later in life.60 Colonization of the hypopharynx within the first month of life with Moraxella catarrhalis, Haemophilus influenzae or Streptococcus pneumoniae was associated with low‐grade systemic inflammation as assessed by serum CRP, TNF‐alpha and IL‐6 levels.61 In addition, a positive association was observed between RSV infection and hospitalization in children with nasopharyngeal colonization with H. influenzae and Streptococcus.62, 63 Importantly, the relative nasopharyngeal abundance of Streptococcus and Staphylococcus negatively correlated with FEV1 and PC20 in children.64 Children who were breastfed and those who had low rates of respiratory infections in the first 2 years of life were colonized early within the upper respiratory tract with Staphylococcus species, followed by Corynebacterium, Dolosigranulum and Moraxella.65-67 However, the most impressive data regarding asthma protection have been observed in relation to traditional farming environments, associated with a high endotoxin and bacterial‐containing dust within the home.5, 15, 17, 68-71 Adult asthma patients treated with inhaled corticosteroids (ICSs) have greater upper and lower airway microbiota diversity compared to control subjects, especially enriched in the phylum Proteobacteria, which include Haemophilus, Comamonadaceae, Sphingomonadaceae, Nitrosomonadaceae, Oxalobacteraceae and Pseudomonadaceae families.72-76 The phylum Proteobacteria is also associated with worse asthma control, whereas Actinobacteria correlates with improvement or no change in asthma control.77 Interestingly, neutrophilic exacerbations of asthma and chronic obstructive pulmonary disease (COPD) correlated with the presence of Proteobacteria in the sputum, whereas eosinophilic exacerbations correlated with the presence of Bacteroidetes.78 Mycoplasma pneumoniae and Chlamydophila pneumoniae are also often found in the airways of the severe asthmatic.79 Macrolide antibiotic treatment may be useful in this subgroup of patients, but patients should be carefully selected.80 Both clarithromycin and azithromycin have been shown to reduce airway hyper‐responsiveness and decrease the abundance of Pseudomonas, Haemophilus and Staphylococcus,73, 81 while increasing the relative abundance of Streptococci.82 However, it is currently not clear how significant a role asthma medications play in directly influencing the composition of the airway microbiota. It has been reported that combination of ICS and oral glucocorticoids (GCS) correlates positively with the increased abundance of Proteobacteria, specifically Pseudomonas, and with a decreased abundance of Bacteroidetes, Fusobacteria and Prevotella.83 In corticosteroid‐resistant patients, Neisseria‐Haemophilus, Campylobacter and Leptotrichia species are present in the lower airways.75 Interestingly, treatment of COPD patients with ICS and long‐acting β2 adrenergic receptor agonists (LABAs), compared to LABA alone, significantly increased the bacterial load, increased bacterial diversity and changed composition of the microbiome in the airways.84 However, prospective longitudinal studies involving corticosteroid‐naïve asthma patients are still needed to address the issue of medication effects on the airway microbiome. The mechanisms responsible for changes in the airway microbiome are also not well understood, and in addition to medications, it is possible that the type of inflammatory response (ie, eosinophil vs neutrophil), changes in host secretions (eg, lipids85, 86) and cellular metabolism might influence microbial colonization and growth within the airways. Figure 4 illustrates the immune responses in the airways that can be influenced by the respiratory microbiome. In addition to asthma, the potential for microbes to play a role in the initial aetiology of rhinitis, or in exacerbations and progression to more severe inflammatory sequelae (such as asthma) is currently being examined. The phylum Proteobacteria is enriched in children with rhinitis, which may be clinically important given the Proteobacteria‐related asthma associations described above.69 Dysbiosis of the inferior turbinate mucosa microbiota, particularly an increase in S. aureus and a decrease in P. acnes, was associated with high total IgE levels in adults with allergic rhinitis.87 In adults with chronic rhinosinusitis (CRS), the genus Corynebacterium was depleted, accompanied by increased relative abundance of genera from the phyla Firmicutes (including Staphylococcus and Streptococcus), Proteobacteria (including Haemophilus, Pseudomonas and Moraxella) or Fusobacteria. This trend was particularly evident in subjects with comorbidities such as asthma and cystic fibrosis.88 Similarly, another study reported that middle meatus samples from CRS patients without nasal polyps were enriched in Streptococcus, Haemophilus and Fusobacterium but exhibited loss of diversity compared to healthy, CRS with nasal polyps and allergic rhinitis subject samples.89 5 LEARNING FROM ANIMAL MODELS Despite the compelling observations and associations in humans that link changes in the microbiota with allergic diseases, very often the causal relationship is not clear. Microbial dysbiosis can be the reason for the disease but can also be the consequence of inappropriate immune reactivity. Animal models have been used to better understand the role of microbes in directly influencing allergic diseases and to elucidate the molecular mechanisms underpinning host‐microbe crosstalk. 5.1 Atopic dermatitis Similar to humans, dogs naturally develop AD and associated allergen sensitization. Canine AD is associated with reduced bacterial diversity, with increased abundance of Staphylococcus pseudintermedius and Corynebacterium species.90 Canine AD lesions improve with antimicrobial treatment and a reduction in Staphylococcus species coincided with restoration of bacterial diversity.30 Filaggrin‐deficient flaky tail mice carry a loss‐of‐function filaggrin mutation, which is associated with a defective epidermal barrier, epidermal hydration and flexibility. Staphylococcus aureus abundance on the skin of these mice correlates with Th2 cytokine levels.91 Inbred DS‐Ng mice develop spontaneous dermatitis, and the skin lesions have been shown to be heavily colonized by S. aureus.29 Staphylococcus aureus triggered cutaneous inflammation involve the accessory gene regulatory (Agr) virulence systems of S. aureus and induced δ‐toxin molecules, which initiate Th2 type skin inflammation. Targeted S. aureus and Corynebacterium bovis antimicrobial therapy improved eczematous lesions and increased bacterial diversity in Adam 17 (a transmembrane metalloproteinase)‐deficient mice. Withdrawal of targeted antimicrobials resulted in a recurrence of eczema and microbial dysbiosis.30 In a mouse itch model, IL‐17A and IL‐22 drive neutrophils to limit the overgrowth of S. aureus on injured skin.25 C5aR‐deficient mice develop reduced microbial diversity, suggesting that the complement system may also regulate the skin microbiota.29 A mouse model of AD showed that application of a Vitreoscilla filiformis bacterial lysate reduced the inflammatory manifestations following allergen application.24 Studies in mice during the neonatal period suggest that tolerance to skin commensals such as S. epidermidis is preferentially established early in life. This supports the hypothesis that exposure to certain microbes at a critical window early in life is required for normal development of the immune system.30 5.2 Food allergy The potential role of the gut microbiome in food allergy has been studied in multiple murine models. Rodriguez et al92 demonstrated that intestinal colonization with Staphylococcus protects against oral sensitization and allergic responses. The microbiota of allergen‐sensitized IL‐4raF709 mice differentially promoted OVA‐specific IgE responses and anaphylaxis when reconstituted in wild‐type germ‐free mice, which could play a role in food allergy.93 The disease‐susceptible IL‐4raF709 mice display enhanced signalling through the interleukin‐4 receptor (IL‐4R) and exhibit STAT6‐dependent impaired generation and function of mucosal allergen‐specific Treg cells, which failed to suppress mast cell activation and expansion.94 Interestingly, STAT6 gene variants are also implicated in the pathophysiology of food allergy in humans.95 The gut microbiota can also regulate Th2 responses through the induction of RORγt Treg cells and Th17 cells.96 Certain bacterial strains such as Bifidobacterium longum 35624, Lactobacillus rhamnosus JB‐1, Clostridia species and Bacteroides fragilis can induce intestinal Treg cells that are able to suppress food allergy and colitis.97, 98 Pattern‐recognition receptor activation on DCs is a potential mechanism by which intestinal microbes may promote Treg cell differentiation.99 5.3 Asthma Important insights regarding the role of the microbiota in the pathogenesis of airway inflammation have come from mouse models. Neonatal mice are more susceptible to develop house dust mite (HDM)‐induced allergic airway inflammation (AAI) and airway hyper‐responsiveness (AHR) than mature mice.100 This phenomenon was associated with a shift from Gammaproteobacteria and Firmicutes towards a Bacteroidetes‐dominated microbiota and the development of PDL‐1–dependent Helios‐ Treg cells.100 Mice housed under germ‐free conditions display significantly more pronounced type 2 inflammation and AHR as compared to conventionally colonized mice. Recolonization, especially early in life, can reverse many of these immunological defects.101 Similarly, antibiotic‐driven dysbiosis in neonatal mice leads to impaired maturation of Tregs and enhanced Th2 responses and promotes proinflammatory colonic iNKT cells.80, 102-105 Conversely, specific bacterial strains, their components or metabolites can successfully induce a variety of anti‐inflammatory responses in the gut and in the lung. L. rhamnosus decreased AAI and AHR induced by Bet v 1 in mice.106 Bacterial strains isolated from neonatal mouse lungs and then administered intranasally very early in life (starting at day 2 after birth) can protect or worsen HDM‐induced airway inflammation, depending which cytokine profile they induced in vitro on precision‐cut lung slices.107 Intramuscular treatment with a DNA plasmid encoding a M. leprae 65 kDa heat‐shock protein (DNA‐HSP65) or subcutaneous injections with proteins from M. tuberculosis delivered in the presence of the TLR9 agonist CpG were able to significantly inhibit development of Der p 1‐induced AAI and AHR in MyD88‐ or Fas‐dependent manner.108 In addition, an exopolysaccharide from B. longum subsp. longum 35624 was shown to protect against colitis and AAI in murine models, which was dependent on TLR2‐induced IL‐10 secretion.109, 110 SCFAs or dietary fibres that are metabolized to SCFAs potently reduced experimental asthma, as well as increased the levels of colonic Bacteroidetes and Actinobacteria species, while decreasing the levels of Firmicutes and Proteobacteria.111, 112 Importantly, the beneficial effects of SCFAs or a high‐fibre diet were transferred to the offspring after treatment of pregnant mice via epigenetic mechanisms.112, 113 Mechanistically, SCFAs have been repeatedly shown to increase Treg numbers and effectiveness.114, 115 In addition, SCFAs influence bone marrow haematopoiesis,111 reduce effector T‐cell activity,116 improve epithelial barrier117, 118 and inhibit mast cell and ILC2 activation.119, 120 Other bacterial metabolites, such as histamine, can induce a wide and complex spectrum of regulatory mechanisms.121, 122 Increased numbers of histamine‐secreting bacteria were observed in adult patients with asthma and correlated with asthma severity.123 Histamine signalling through the H2R is involved in AAI,124 while the use of H2R antagonists in children during their first 6 months of life is associated with significantly increased risk of allergic diseases and asthma.10 6 THERAPEUTIC TARGETING OF THE MICROBIOME Despite the growing number of studies that associate changes in the microbiota with allergic and immune‐related outcomes, only a relatively small number of studies have shown clinical benefits and there are no microbe‐based therapies that are currently universally accepted for the prevention or treatment of allergies or asthma. A number of reasons can be suggested for this, which may include the poor choice of therapeutic microbes to begin with. It is likely that many confounding factors do influence the success of a microbiome therapeutic, such as diet, age, obesity, ethnicity and other environmental exposures. These need to be taken into account and controlled for. In addition, given the explosion in knowledge regarding disease endotypes, it is possible that specific microbes will need to be carefully selected to mechanistically fit with specific disease endotypes and it is likely that one intervention will not work for everyone. Certain interventions such as faecal transplantation may be too crude an approach, and until critical safety concerns are resolved, this type of intervention should not be considered outside the setting of carefully monitored clinical trials. 6.1 Atopic dermatitis Early intervention aimed at protecting the skin barrier may ameliorate progression of the atopic march in a subset of patients.19 Skin microbiome manipulation may offer novel therapeutic opportunities, as has been seen with the emollients supplemented with a Vitreoscilla filiformis lysate.125 Similarly, topically administration of Roseomonas mucosa improved clinical severity scores in adults and children with AD.125 Autologous microbiome transplant (AMT) of S. hominis and S. epidermidis showed efficacy in controlling S. aureus overgrowth.126 In addition to topical bacterial treatments, oral administration of probiotics has also been examined. Prenatal and post‐natal treatment with Lactobacillus and Bifidobacterium strains can reduce risk of AD development in infants,35, 127, 128 which may associate with changes in T cell–mediated responses.129 A mixture of probiotic strains was recently shown to reduce SCORAD index and topical steroid use in children with AD.130 Little has been reported on probiotic treatment of adults with AD, but administration of B. longum 35624 to adults with psoriasis resulted in reduced circulating CRP, TNF and IL‐17 levels, possibly due to increased numbers of Tregs, which suggests that bacteria in the gut can influence skin inflammatory activity in adults.131, 132 Taken together, supplementation with specific probiotic strains may modulate the gut bacteria in a way that influences inflammation within the skin and may protect some children against AD development.35 6.2 Food allergy The use of probiotics in food allergy treatment and prevention has been examined. Supplementation of cow's milk‐allergic children with Lactobacillus casei and Bifidobacterium lactis did not accelerate cow's milk allergy resolution.133 However, the combination of L. rhamnosus GG and extensively hydrolysed casein formula did accelerate milk allergy resolution after 6 and 12 months when compared to the formula‐only control group.134 The combination of L. rhamnosus supplementation and peanut oral immunotherapy (OIT) was evaluated in peanut‐allergic children for 18 months. The combination was effective in inducing possible sustained unresponsiveness and immune changes that suggested modulation of the peanut‐specific immune response.135 In addition, a sustained beneficial effect on psychosocial impact of food allergy at 3 and 12 months after end of treatment was recently reported.136 However, the major limitation of this study is that further work is required to determine the relative contributions of the probiotic vs OIT due to the lack of an OIT and L. rhamnosus supplementation control groups in this trial. 6.3 Asthma A significant number of studies have examined the effect of probiotic supplementation on asthma‐related outcomes. A recent systematic review of probiotic studies in children with asthma identified eleven studies eligible with a total of 910 children. The proportion of children with fewer episodes of asthma was significantly higher in the probiotic group than in the control group, but no statistical significance was observed in childhood asthma control test, asthmatic symptom in the day and night, the number of symptom‐free days, forced expiratory volume in the first second predicted and peak expiratory flow.137 In the future, it will be interesting to evaluate microbial administration directly to the airways, in addition to the gut.138 7 CONCLUSIONS Significant advances have been made in recent years in describing the composition of the microbiome in the gut, airways and skin. The changes in bacterial communities that associate with, or sometimes precede, atopic dermatitis, food allergy and asthma are being identified (summarized in Table 1). Accumulating evidence suggests that microbial exposures might be most effective at preventing atopic disorders during the first 1‐2 years of life. However, substantial gaps in our knowledge on the microbiome still exist. In particular, the field has been slow to translate potentially effective microbiome‐associated therapies into the clinic via appropriate clinical trials performed to high standards and showing meaningful clinical responses that are superior to current avoidance approaches. While the critical role of the microbiota in cancer immunotherapy has been established, there are currently no published data on the potential role of the microbiota in influencing the success of immunotherapy or biologics in allergy or asthma.139 In addition, novel probiotics and not just the traditional probiotic strains need to be clinically tested. Furthermore, microbial components or their metabolites should also be examined; in particular, the application of these novel microbial drugs to the diseased site (eg, the airways) must be explored. Lastly, there are no microbial therapeutics currently approved for routine clinical practice, and significant effort and investment are still required to identify the optimal microbial interventions for allergy and asthma. Location Phyll (Genus) Effect Reference Oral cavity ↑ Gemella haemolysans ↓ Lactobacillus gasseri, Lactobacillus crispatus Increased risk of allergic diseases 47 Intestine ↑ Staphylococcus species Protection against oral sensitization and allergic responses 92 Intestine ↑ Clostridia, Firmicutes Milk allergy resolution 49 Intestine ↑ Lachnospiraceae, Ruminococcaceae Associated with egg allergy 50 Intestine ↓ Haemophilus, Dialister, Dorea, Clostridium Associated with food sensitization 51 Intestine ↓ Citrobacter, Oscillospira, Lactococcus, Dorea Associated with food allergy 51 Intestine ↓ Escherichia coli High faecal calprotectin, impaired IL‐10 activation, increased risk of AD and asthma 43 Intestine ↓ Bifidobacterium Correlates with AD severity 37 Intestine Early colonization with C. difficile Associated with AD development 38 Intestine ↓ Bacteroidetes diversity Associated with AD development 39 Intestine ↓ Akkermansia muciniphila, Ruminococcus gnavus and Lachnospiraceae Associated with AD development 40 Intestine ↓ Lachnospira, Veillonella, Faecalibacterium, Rothia Reduced levels of faecal SCFAs, increased risk of asthma 56 Intestine ↓ Bifidobacterium, Akkermansia, Faecalibacterium ↑ Candida, Rhodotorula Increased risk of developing multisensitized atopy, increased circulating proinflammatory metabolites 58 Upper airways Early colonization with Staphylococcus species, Corynebacterium, Dolosigranulum, Moraxella Associated with lower rate of respiratory infections in the first 2 years of life 65-67 Upper airways Early colonization with Streptococcus, Moraxella, Haemophilus Increased risk of virus‐induced acute respiratory infections and increased risk of asthma 60 Upper airways ↑ Proteobacteria Associated with rhinitis in children 69 Nasopharynx ↑ Haemophilus influenzae, Streptococcus species Increased risk of hospitalization during RSV infection 62 Nasopharynx Colonization with Staphylococcus aureus Decreased risk of hospitalization during RSV infection 63 Nasopharynx ↑ Streptococcus, Staphylococcus Abnormalities in functional tests of the respiratory system 64 Nasopharynx ↑ Staphylococcus aureus ↓ P. acnes Associated with high IgE levels 87 Nasopharynx ↑ Firmicutes (Staphylococcus & Streptococcus), Proteobacteria (Haemophilus, Pseudomonas & Moraxella), Fusobacteria ↓ Corynebacterium Associated with CRS in adults 88 Nasopharynx ↑ Streptococcus, Haemophilus, Fusobacteria ↓ Diversity Associated with CRS without nasal polyps in adults 89 Nasopharynx ↑ Lactobacillus during acute respiratory infection with RSV Reduced risk of wheezing 59 Hypopharynx Colonization with Moraxella catarrhalis, Haemophilus influenzae, Streptococcus pneumoniae Low‐grade systemic inflammation 61 Lower airways ↑ Proteobacterium (Klebsiella species) (Mycoplasma pneumoniae, Chlamydophila pneumoniae) Associated with severe asthma 77, 79 Lower airways ↑ Actinobacteria Improvement in asthma control 77 Lower airways ↑ Neisseria, Haemophilus, Campylobacter, Leptotrichia Associated with resistance to corticosteroids in asthma 75 Sputum ↑ Proteobacteria Associated with neutrophilic asthma exacerbations 78 Sputum ↑ Bacteroidetes Associated with eosinophilic asthma exacerbations 78 Skin ↑ Staphylococcus aureus Epidermal barrier dysfunction, cutaneous inflammation, formation of AD skin lesions, associated with AD severity and allergen sensitization, associated with susceptibility to eczema herpeticum among AD patients 19, 21, 23 Skin Colonization with single clonal Staphylococcus aureus strains Associated with AD severity 26 Skin ↑ Malassezia species. Associated with AD severity 35 Skin ↑ Corynebacterium, Proteobacterium Associated with AD severity 21 Skin ↑ coagulase‐negative staphylococci: (Staphylococcus epidermidis, S. hominis, S. lugdunensis) Limits Staphylococcus aureus overgrowth 28 Skin Colonization with S. epidermidis TLR2 activation, epidermal barrier maintenance 1 Skin ↓ Proteobacteria (Propionibacterium, Streptococcus, Acinetobacter, Corynebacterium, Prevotella) Associated with AD 28, 30 Skin Early colonization with S. epidermidis Local activation of the host immune response through induction of S. epidermidis‐specific FOXP3 Treg cells 29 Skin ↑ in resident skin bacteria Associated with AD flares 24 This table summarizes the bacterial changes that have been associated with atopic dermatitis, food allergy or asthma. CONFLICTS OF INTEREST LOM is a consultant to Alimentary Health Ltd and has received research funding from GSK. NL, PS, ZL, MS and TE have no conflict of interest in relation to this work. AUTHOR CONTRIBUTIONS NL, PS, ZL, MS, TE and LOM contributed to drafting the manuscript. All authors read, reviewed and agreed the final version of this manuscript. REFERENCES Notes : This table summarizes the bacterial changes that have been associated with atopic dermatitis, food allergy or asthma.

|
Scooped by
Gilbert C FAURE
November 15, 2018 5:24 AM
|
Adnan Custovic and colleagues demonstrate that combinations of allergen sensitivities in children can be used to predict concurrent asthma diagnosis.

|
Scooped by
Gilbert C FAURE
November 12, 2018 2:35 PM
|
Abstract Background Patients with mastocytosis are at increased risk of anaphylaxis. The use of nonsteroidal anti‐inflammatory drugs (NSAIDs) is often discouraged because of this reason. However, the actual prevalence and severity of NSAID‐related hypersensitivity among patients with mastocytosis is unknown. Methods A double‐blind, placebo‐controlled acetylsalicylic acid (ASA) challenge up to a cumulative dose of 520 mg was performed among adult patients with mastocytosis. In addition, a retrospective search of the entire outpatient cohort was performed to obtain “real‐life” data on NSAID hypersensitivity. Results Fifty patients underwent an ASA challenge. Seventy percent had indolent systemic mastocytosis, 18% had mastocytosis in the skin, and 12% had advanced mastocytosis. The ASA challenge was positive in 1 patient who developed urticaria. The additional retrospective chart review revealed that 8 of 191 patients had a history of NSAID‐related hypersensitivity reaction(s), of whom 3 reported severe systemic reactions. All 8 patients had already experienced NSAID‐related hypersensitivity reactions before mastocytosis was diagnosed. Conclusions The frequency of ASA hypersensitivity was 2% in a prospective challenge study and 4.1% in a retrospective chart review of 191 patients with mastocytosis. NSAIDs can be administered safely to most patients with mastocytosis. Extra caution should be taken in patients with a history of hypersensitivity reactions to other drugs, or traditional risk factors for NSAID hypersensitivity. 1 INTRODUCTION Mastocytosis is a disease in which aberrant mast cells accumulate. The WHO recognizes different subtypes of SM.1, 2 The prevalence of anaphylaxis is higher in patients with mastocytosis compared to healthy persons.3, 4 A wide variety of stimuli can trigger mast cell degranulation and thereby lead to anaphylaxis.5 Historically, the use of certain medications that could theoretically trigger mast cell degranulation is discouraged in patients with mastocytosis. Among these are radiocontrast media, general anesthetics, opioid analgesics, and nonsteroidal anti‐inflammatory drugs (NSAIDs).3 For general anesthetics and radiocontrast media, case reports on severe (and sometimes lethal) anaphylaxis in patients with mastocytosis are available, although the absolute risk still appears low.6-8 The prevalence and severity of anaphylaxis due to NSAIDs in patients with mastocytosis is actually not known. Anxiety for NSAID‐related hypersensitivity reactions leads to confusion among both physicians and patients, and different advices between practices. The use of NSAIDs is therefore often avoided, resulting in the risk of mistreatment of patients with mastocytosis for several reasons. Firstly, these patients are at increased risk of cardiovascular morbidity, which often necessitates acetylsalicylic acid (ASA) for secondary prevention.4, 9 Secondly, ASA is a well‐known treatment for flushing in mastocytosis.10, 11 Thirdly, patients with mastocytosis relatively often suffer from various types of pain for which analgesics might be necessary.12, 13 Currently, they are often advised to only take acetaminophen which is not always sufficient. In our practice, we noted that many patients used NSAIDs uneventfully, until they received were diagnosed to have mastocytosis. Furthermore, previously performed NSAID challenges were always negative. We therefore hypothesized that the frequency and severity of NSAID‐related hypersensitivity is overestimated in patients with mastocytosis. For drug hypersensitivity in general, drug challenge tests are the gold standard diagnostic procedure.14 ASA is often used to test for general NSAID hypersensitivity because of its strong COX‐1‐inhibiting properties.15 Therefore, we designed a study using standardized drug challenge tests with ASA to investigate the exact prevalence and severity of NSAID hypersensitivity reactions in patients with mastocytosis. 2 METHODS 2.1 Patient eligibility Patients were recruited from the Mastocytosis Outpatient Clinic of the Erasmus University Medical center. All adult patients with biopsy‐proven cutaneous or systemic mastocytosis were eligible. Patients were excluded if they had a history of a prior NSAID‐related hypersensitivity reaction(s), uncontrolled asthma, rhinosinusitis, nasal polyps, active pregnancy, and high dosage of beta‐blocking drugs (equivalent to ≥100 mg of metoprolol), when they were not able to stop antihistamines or prednisolone, or were not deemed capable of handling possible delayed anaphylactic reactions at home. Preexistent mast cell mediator‐related symptoms such as pruritus or flushing were not considered to be exclusion criteria in order to represent the real‐life situation at an outpatient clinic. Moreover, flushing can be an indication for ASA. The frequency of ASA hypersensitivity among patients with mastocytosis was 2% in a prospective study and 4.1% in a retrospective cohort. NSAIDs can probably be safely administered to most patients with mastocytosis. A history of hypersensitivity reactions to other drugs might increase the risk of NSAID hypersensitivity among patients with mastocytosis. 2.2 Study protocol All patients underwent a double‐blind, placebo‐controlled ASA challenge in a randomized order. The minimum interval between the two test days was 14 days. The study medication was provided in a blinded fashion by the pharmacy of the Erasmus MC. Patients had to stop H1‐antagonists and leukotriene antagonists for 3 days prior to the drug challenge. The challenge took place at the Allergy Outpatient Clinic. Patients received three incremental doses of ASA of 40, 80, and 400 mg (or matched placebo tablets), leading to a cumulative dose of 520 mg. The interval between each dose was 1 hour, and patients were observed for an additional 2 hours after the administration of the third dose. Mast cell mediator‐related symptoms were systematically scored before the start of each drug challenge and after 1, 2, and 4 hours. We used an adapted form of the scoring system for food challenges as proposed by Grabenhenrich et al.16 This form scores symptoms according to organ system and severity and is in our practice routinely used for both food and drug challenges. In addition, numeric rating scale (NRS) score was obtained for mast cell mediator‐related symptoms such as pruritus and headache. An increase of 3 points in this scale during the challenge was considered significant. All challenges were conducted and assessed by MH and/or SdV. In cases of doubt, a second investigator (RGvW or PvD) was consulted to assess the symptoms. Deblinding of the investigators and patients took place 24 hours after all 50 patients completed both challenge days. 2.3 Outcomes and definitions The ASA challenge was considered positive when a patient developed objective mast cell mediator‐related symptoms within 12 hours after the administration of the third dose on the day they received the verum, and had no symptoms on the placebo day. The challenge was considered negative when a patient developed no symptoms on the verum day, regardless of any symptoms on the placebo day. The WHO criteria were used to define the subtype of mastocytosis.1 Patients with maculopapular cutaneous mastocytosis (MPCM) who never underwent bone marrow biopsy, or had negative bone marrow investigation, were categorized as mastocytosis in the skin (MIS). An atopic background was defined as a history of atopic dermatitis, asthma, rhinoconjunctivitis, and/or positive specific IgE for inhalation or food allergens. Next to atopy, other traditional risk factors for NSAID hypersensitivy were defined as the presence of asthma, nasal polyps, and chronic rhinosinusitis. Eosinophilia was defined as an absolute eosinophil count of >500 × 106 in peripheral blood. 2.4 Additional retrospective cohort study Next to the prospective challenge study, we retrospectively searched the electronic patient records of all adult patients who visited the mastocytosis center from January 2009 until January 2017 and who fulfilled the criteria for mastocytosis in the skin (MIS), cutaneous or systemic mastocytosis (SM). Patients who already participated in the challenge study were excluded from the retrospective cohort. Patients with a history of NSAID‐related hypersensitivity reactions, or patients who had proven NSAID tolerance prior to the start of this study, were subsequently contacted to obtain further clinical details. NSAID tolerance was considered as proven when a drug challenge was negative or when (accidental) NSAID ingestion was uneventful after the diagnosis of mastocytosis was made. The characteristics of the patients with and without NSAID tolerance from this retrospective cohort were compared to identify possible differences. 2.5 Ethical considerations This trial was performed according to the latest Helsinki guidelines. The study was approved by the local medical ethics committee. All participants provided written informed consent. The trial was registered in the EudraCT database, Number 2015‐004604‐37. 2.6 Statistical analysis We used IBM SPSS 21 for all analyses. Patient characteristics were noted as median with interquartile range (IQR) for continuous variables and as the number with percentage for dichotomous variables. To calculate potential differences between the groups with and without NSAID hypersensitivity, the Mann‐Whitney U test was used for continuous variables and the chi‐square test for dichotomous variables. 2.7 Power calculation The prevalence of NSAID‐related hypersensitivity reactions in the general population is <1%. We hypothesized that the risk in patients with systemic mastocytosis is only marginally higher than in the general population. With an estimated frequency of allergic reactions of 4% in our study population, inclusion of 50 subjects in total will lead to a 95% confidence interval of 1%‐13%. The estimated frequency was based on self‐reported reactions by patients in the Erasmus MC cohort combined with circumstantial data of other cohort studies on mastocytosis (see Discussion section for references). 3 RESULTS 3.1 Study population At the moment of inclusion in April 2017, 173 patients were considered eligible to participate in the trial (Figure 1), and 58 patients signed the informed consent. After inclusion, 8 patients dropped out before the ASA challenge was performed completely. One of these patients was excluded after the first challenge day because she started to use prednisolone for arthritis which was not related to the trial. Two patients experienced anaphylactoid reactions related to their mastocytosis within days after cessation of the antihistamines. The other patients withdrew consent. The inclusion process was stopped after 50 subjects completed both days of the challenge. The final study population thus consisted of 50 patients. The median age was 55 years, and most participants had indolent SM (Table 1). Age in years, median (IQR) 55 (16) Male, n (%) 16 (32) Subtype according to WHO criteria 1, 2, n (%) MIS 9 (18)a ISM With skin lesions 26 (52) Without skin lesions 9 (18) SSM 3 (6) SM‐AHN 2 (4) ASM 1 (2) Serum tryptase level at diagnosis in μg/L, median (IQR) 25.0 (17.8) Atopic background, n (%) 13 (26) Eosinophilia, n (%) 2 (4) Previous hypersensitivity reaction to any drug, n (%) 5 (10) Previous anaphylaxis due to any trigger, n (%) 23 (46) Wasp 7 (30) Unknown 7 (30) Physical stimuli 4 (17) Other drugsb 5 (22) Miscellaneousc 6 (26) ASM, aggressive systemic mastocytosis; IQR, interquartile range; ISM, indolent systemic mastocytosis; MIS, mastocytosis in the skin; SSM, smoldering systemic mastocytosis; SM‐AHN, systemic mastocytosis with associated hematological neoplasm. a One patient underwent incomplete bone marrow investigation, and 8 patients declined bone marrow punction. b Other drugs: proton pump inhibitor (1×), morphine (2×), penicillin (1×), and codeine (1×). c Miscellaneous triggers: horsefly (n = 2), jellyfish sting (n = 1), fire ant (n = 1), anesthesia (n = 1), codeine (n = 1). 3.2 Results of ASA challenge The challenge was positive in one patient (2%), who developed an urticarial rash 4 hours after ingestion of the third dose of ASA, which correspond s with a cumulative dose of 520 mg. The rash subsided after she took 10 mg of hydroxyzine. This patient had smoldering SM based on a serum tryptase level of ≥200 μg/L and hepatosplenomegaly. She had never used NSAIDs before. She had previously developed a rash after the administration of radiocontrast media and reported an increase in mast cell mediator‐related symptoms after the consumption of alcoholic beverages and histamine‐rich food. Three other patients reported subjective symptoms on the day of the verum but not on the day they received placebo. These symptoms consisted of mild flushing in 1 patient, generalized pruritus in 1 patient, and lightheadedness in 1 patient. The flushing was not considered as a positive challenge because it occurred after the second dose of 80 mg and subsided spontaneously despite the fact that the next increasing dose of ASA was administered according to protocol. Moreover, this patient has spontaneous flushes multiple times a week. Similarly, the patient with pruritus already had pruritus before the start of the challenge and the NRS score increased by 2 points throughout the day of the challenge which was below the prespecified threshold of 3 points (see Methods section). The last patient experienced lightheadedness 15 minutes after the ingestion of the third dose of ASA, but had no other mast cell mediator‐related symptoms and stable vital parameters. The serum tryptase level did not increase as compared to a baseline measurement. Seven patients had a reaction on the placebo day, of whom 1 had objective macular erythema on the arms and trunk and the other 6 patients had subjective symptoms. Four patients who had a reaction to placebo already had mast cell mediator‐related symptoms at the start of the challenge, consisting of pruritus and/or flushing. 3.3 Patients with a history of NSAID‐related reactions In addition to the challenge study, we retrospectively searched the electronic records of all adult patients with mastocytosis that visited the Erasmus MC from 2009 until 2017. Of a total of 191 patients, 8 patients had an annotation of “NSAID allergy” in their medical record. This results in a prevalence of self‐reported NSAID‐related hypersensitivity of 4.1% in our entire cohort. Fifteen patients had proven NSAID tolerance prior to this study. Table 2 summarizes the clinical characteristics of these patients. Age at diagnosis (years) Sex Subtype Skin involvement Serum tryptase at diagnosis (μg/L) Atopy Type of NSAID Timing of reaction Symptoms of reaction MC mediator‐related reaction to other stimuli 1 41 F CMa MPCM 8.6 Yes ASAb 80 mg 2 h Angioedema Penicillin, lidocaine 2 72 M ISM No 20.0 No Ibuprofen Diclofenacc Unknown Generalized pruritus, blurry vision – 3 51 F ISM MPCM 125.0 Yes Ibuprofen Diclofenacc 5 min Angioedema, palpitations, collapsed Heat 4 62 F ISM MPCM 118.0 No Diclofenac Unknown Angioedema Alcohol consumption 5 42 M ISM MPCM 31.4 No Naproxen 10 min Erythema, stridor, hypotensiond Alcohol consumption, wasp sting, temperature changes (cold) 6 40 M ISM No 24.7 Yes Acetaminophen 1000 mg 5 min Diffuse erythema Morphine, strong odors 7 48 F ISM MPCM 43.5 Naproxen 5 min Diffuse erythema – 8 68 F ISM MPCM 17.8 No Diclofenac 20 min Hypotension, collapsed Iodated contrast media ASA, acetylsalicylic acid; CM, cutaneous mastocytosis; MPCM, maculopapular cutaneous mastocytosis; NSAID, nonsteroidal anti‐inflammatory drug. a Complete workup with bone marrow investigation was negative for mastocytosis. b Hymenoptera sensitization could not be confirmed by specific IgE nor intradermal tests. c Two separate reactions at different occurrences. d Treatment at emergency department required. All patients had experienced NSAID‐related reactions before they received the diagnosis of mastocytosis. The most frequent symptoms were angioedema, erythema, and hypotension. Three patients required treatment in an emergency department. Of the patients who could reliably recall their reaction at the time of questioning, everyone experienced a reaction within 2 hours after the ingestion of the NSAID. Patient number 5 developed a reaction after the combination of naproxen and a wasp sting. Hymenoptera sensitization could not be confirmed. Although it is likely that Hymenoptera was the main culprit and naproxen acted as a cofactor, the patient was labeled as “NSAID intolerant” because of the severity of the reaction and the risk of aggravation of future reactions with the use of NSAIDs. Patient number 3 later had a drug challenge with celecoxib which was negative. Patient numbers 6 and 8 both later had a negative drug challenge with naproxen, which excludes a general nonspecific NSAID hypersensitivity. Notably, seven patients (87.5%) reported mast cell mediator‐related reactions to physical stimuli. These reactions ranged from flushing or gastrointestinal symptoms to anaphylaxis. 3.4 Characteristics associated with NSAID hypersensitivity As only one patient had a positive ASA challenge, the data from the prospective study could not be used to reliably identify any potential clinical characteristics that are associated with NSAID hypersensitivity. Therefore, the data from the retrospective cohort were analyzed for this purpose (Table 3). No NSAID hypersensitivity (n = 15) NSAID hypersensitivity (n = 8) P‐value Age, median (IQR) 51 (20) 49 (25) >.10 Male sex, n (%) 6 (40) 3 (33.3) >.10 Subtype, n (%) MIS 5a (33.3) 1b (12.5) >.10 ISM 10 (66.7) 7 (87.5) SSM 0 0 SM‐AHN 0 0 ASM 0 0 Presence of skin mastocytosis, n (%) 11 (73.3) 5 (62.5) >.10 Serum tryptase at diagnosis, median (IQR) 28.2 (10.9)c Range: 2.2‐72.0 28 (53)c Range: 8.6‐125.0 >.10 History of anaphylaxis, n (%) 5 (33.3) 4 (50) >.10 Pruritus, n (%)d 7 (46.7) 0 .021 Flushing, n (%)d 5 (33.3) 1 (12.5) >.10 Dyspepsia, n (%)d 3 (10.3) 1 (12.5) >.10 Diarrhea, n (%)d 3 (20) 0 >.10 Fatigue, n (%)d 6 (42.9) 1 (12.5) >.10 Subjective cognitive problems, n (%) 4 (40) 0 .074 Osteoporosis, n (%) 1 (7.1) 2 (28.6) >.10 Eosinophilia, n (%) 2 (13.3) 3 (37.5) >.10 Atopy, n (%) 4 (26.7) 3 (37.5) >.10 History of hypersensitivity reaction to other drugs, n (%)e 1 (6.7) 3 (37.5) .063 Alcohol intolerance, n (%)f 4/5 (44.4) 4/5 (80) >.10 MC mediator‐related reaction to physical triggers, n (%)c 5/8 (62.5) 4/5 (80) >.10 a Bone marrow investigation was incomplete in 1 patient and not performed in the other patients. b Bone marrow investigation negative, classifying this patient as cutaneous mastocytosis. c Physical triggers: heat, cold, stress, exercise. d Symptom present ≥3 d per week. e The culprit drug was amoxicillin in the NSAID‐tolerant patient. See Table 2 for the culprit drugs in the NSAID hypersensitivity group. f Not known for all patients because some patients never consume alcohol. Overall, patients with NSAID tolerance appear to have more daily mast cell mediator‐related symptoms such as flushing, cognitive problems, fatigue, and pruritus. Only the latter was statistically significant (P = .021, chi‐square test), probably due to the small numbers of patients. Patients with NSAID hypersensitivity reported more reactions to other drugs, although this difference did not reach statistical significance (P = .063). The same accounted for peripheral blood eosinophilia (P = .181), osteoporosis (P = .186), and alcohol intolerance (P = .308). Strikingly, traditional risk factors for NSAID hypersensitivity in the general population such as atopy, asthma, or rhinitis were not more frequent in the NSAID hypersensitivity group of our cohort. Neither were there any relevant differences in age, sex, serum tryptase levels, or skin involvement of mastocytosis. 4 DISCUSSION This is the first double‐blind, placebo‐controlled challenge study to investigate the prevalence and severity of ASA hypersensitivity among patients with mastocytosis. Only 1 of 50 participants (2%) had a positive ASA challenge, consisting of an urticarial rash. Three other patients had subjective symptoms to ASA. The characteristics of the study population were overall representative of a patient cohort in a tertiary center for mastocytosis, except for a relatively low number of male participants.17, 18, 13 However, the exclusion of patients with known risk factors for NSAID hypersensitivity might have led to a selection bias. Therefore, we performed an additional retrospective analysis of our entire cohort of 191 patients. This resulted in a prevalence of self‐reported NSAID‐related hypersensitivity of 4.1%. Importantly, all patients with NSAID hypersensitivity experienced one or more reactions before the diagnosis of mastocytosis was established. Although interpretation of any differences between the patients with and without NSAID hypersensitivity is difficult due to the small patient numbers, it appears from the retrospective cohort that patients with NSAID hypersensitivity more often experienced hypersensitivity reactions to other drugs and/or alcohol. It must be noted that three patients reported a hypersensitivity reaction to amoxicillin, which is the third most reported culprit for drug‐related reactions in the Netherlands. We cannot exclude that the relationship between amoxicillin and the reported reactions was based on coincidence. Another notable difference is the higher prevalence of mast cell mediator‐related symptoms among NSAID‐tolerant patients. Possibly, this difference represents the clinical practice, because patients with symptoms such as flushing are more often in need for ASA and therefore were more likely to undergo an NSAID challenge out of medical necessity. A causal explanation seems unlikely. Interestingly, 2 of 8 patients with a history of NSAID‐related hypersensitivity reactions later had negative unblinded challenges with another NSAID. This can be explained in multiple ways: They might have a specific, IgE‐mediated allergy to the culprit NSAID. Another, more likely, explanation is the fact that NSAIDs can be a cofactor to augment anaphylaxis.19, 20 The current trial does not provide prospective data on the role of NSAIDs as a cofactor in patients with mastocytosis. Also, although the use of ASA as a model for general NSAID hypersensitivity is widely accepted, a specific allergy for one type of NSAID is potentially missed with this approach. Moreover, the currently presented data cannot be extrapolated to patients with traditional risk factors for NSAID hypersensitivity, such as asthma, nasal polyposis, or atopic constitution. However, most patients with mastocytosis do not have such risk factors21; thus, most patients would fulfill the currently used inclusion criteria. Lastly, a possible caveat of drug challenges in patients with mastocytosis is the fact that many of them already have mast cell mediator‐related symptoms on a daily basis, especially as anti‐mediator medications need to be interrupted prior to a challenge. Using NRS scores, we tried to score these symptoms as objectively as possible; however, some degree of bias in the assessment of challenge studies cannot be excluded in this patient category. The prevalence of NSAID hypersensitivity in our cohort of patients with mastocytosis is only slightly higher compared to the prevalence of 1%‐2% of self‐reported NSAID‐related hypersensitivity in a general population.22 There are few comprehensive data on NSAID hypersensitivity among patients with mastocytosis published to date. One retrospective study described 20 patients who received ASA in varying dosages and schedules. Two patients (10%) reported a mild reaction: either delayed urticaria or immediate flushing.10 Other descriptive population studies reported a prevalence ranging between 2.3% and 6%, of mostly mild immediate‐type reactions.20, 23, 24 We could not find published proof of fatal anaphylaxis due to NSAIDs in patients with mastocytosis. Conversely, in a population of 137 persons with drug‐ or food‐related anaphylaxis, mastocytosis was found in only 2 patients.25 Moreover, there was no association between NSAID hypersensitivity and serum tryptase levels in a general cohort.26 An EAACI position paper advises that patients with mastocytosis and known NSAID tolerance can safely keep taking NSAIDs, but all others should undergo workup.27 However, that workup is not further specified in this study. Based on our current results, we suggest that everyone with mastocytosis who has never experienced a hypersensitivity reaction to NSAIDs, or other drugs, can safely start taking NSAIDs at home. Given the fact that patients who have experienced a hypersensitivity reaction to another drug appear to be at a higher risk of NSAID hypersensitivity reactions, it seems appropriate to administer the first dose in a clinical setting, preferably with an incremental challenge protocol. As mentioned before, the interpretation of such challenges is very delicate and requires experience in this area. Despite the placebo‐controlled approach, some patients will have only subjective symptoms to an NSAID, and although this is likely to be a “placebo reaction,” it cannot be excluded that these minor symptoms reflect some reaction to the NSAID. The risk of developing more serious reactions in the future is unclear for these patients, and careful counseling is of paramount importance. Possibly, patients with a history of NSAID‐related hypersensitivity reactions can also be challenged with another NSAID. Depending on the type and severity of the previous reaction(s), it can be safer to challenge with a selective COX‐2 inhibitor in these cases. Unfortunately, our study cannot corroborate this suggestion. Prospective placebo‐controlled studies on these topics would be highly interesting, although are hindered by potential safety issues. On a final note, although the possible benefits of ASA and NSAIDs in general for patients with mastocytosis are clear, the indication must be weighed against possible adverse effects. For instance, patients with mastocytosis already are at risk of peptic ulcer disease,28 which might be increased by the use of NSAIDs. Moreover, it is well‐known that NSAIDs can act as a cofactor in anaphylaxis. Ultimately, a careful consideration of risks and benefits needs to be made for each individual, and patients should be consulted on the possible risks. 5 CONCLUSIONS In summary, the frequency of NSAID hypersensitivity among patients with mastocytosis was 2%, as determined by a prospective double‐blind ASA challenge. The frequency of self‐reported NSAID hypersensitivity in a retrospective cohort was 4.1%. Based on the mild reactions we saw in our study, combined with the real‐life experience that all patients with severe NSAID hypersensitivity experienced these reactions prior to their diagnosis of mastocytosis, we conclude that it is safe to administer NSAIDs to most patients with mastocytosis if they do not have a history of prior NSAID hypersensitivity reactions. Extra caution might be taken in patients with previous hypersensitivity reactions to other drugs, or with traditional risk factors for NSAID hypersensitivity. ACKNOWLEDGMENTS We would like to thank N.W. de Jong, PhD (Dept. of Allergy, Erasmus MC), for her assistance with the practical organization of the challenge study, and M.S. van Maaren, MD (Dept. of Allergy, Erasmus MC), for providing and advising on the scoring system for the ASA challenges. CONFLICTS OF INTEREST The authors declare that they have no conflicts of interest. AUTHORS’ CONTRIBUTIONS MH and PvD are responsible for the concept and design of the study. MH and SdV performed the inclusion and drug challenges and collected and analyzed the data. PvH and RGvW gave advice about the design of the trial and interpretation of the data. All authors revised the manuscript on multiple occasions. REFERENCES Notes : Trial registration: This trial was registered in the EudraCT database, Number 2015‐004604‐37. ASM, aggressive systemic mastocytosis; IQR, interquartile range; ISM, indolent systemic mastocytosis; MIS, mastocytosis in the skin; SSM, smoldering systemic mastocytosis; SM‐AHN, systemic mastocytosis with associated hematological neoplasm. 3 One patient underwent incomplete bone marrow investigation, and 8 patients declined bone marrow punction. 4 Other drugs: proton pump inhibitor (1×), morphine (2×), penicillin (1×), and codeine (1×). 5 Miscellaneous triggers: horsefly (n = 2), jellyfish sting (n = 1), fire ant (n = 1), anesthesia (n = 1), codeine (n = 1). ASA, acetylsalicylic acid; CM, cutaneous mastocytosis; MPCM, maculopapular cutaneous mastocytosis; NSAID, nonsteroidal anti‐inflammatory drug. 7 Complete workup with bone marrow investigation was negative for mastocytosis. 8 Hymenoptera sensitization could not be confirmed by specific IgE nor intradermal tests. 9 Two separate reactions at different occurrences. 10 Treatment at emergency department required. 11 Bone marrow investigation was incomplete in 1 patient and not performed in the other patients. 12 Bone marrow investigation negative, classifying this patient as cutaneous mastocytosis. 13 Physical triggers: heat, cold, stress, exercise. 14 Symptom present ≥3 d per week. 15 The culprit drug was amoxicillin in the NSAID‐tolerant patient. See Table 2 for the culprit drugs in the NSAID hypersensitivity group. 16 Not known for all patients because some patients never consume alcohol.

|
Scooped by
Gilbert C FAURE
November 6, 2018 6:42 AM
|

|
Rescooped by
Gilbert C FAURE
from Immunology and Biotherapies
October 23, 2018 2:56 AM
|
Ingesting small doses of peanut products guards against allergic reactions—but an undercurrent of anxiety persists.
![Figure][1]
Jacob Kingsley, 12, visits a bakery that was off-limits before he began oral immunotherapy for a peanut allergy.
PHOTO: MADDIE MCGARVEY
Jacob Kingsley was 9 years old when he was handed the poison he'd shunned since before he could walk and told to swallow it as medicine. Obediently, he gulped down a few micrograms of peanut flour—less than 1/1000 of a peanut—diluted in grape Kool-Aid. His mother and a nurse hovered, ready to inject him with epinephrine if an itchy throat and wheezing struck.
Jacob's mother, Jennifer Kingsley, had driven him 2 hours from their home in Columbus to this doctor's office in Cincinnati, Ohio, for the first of dozens of sessions of peanut immunotherapy. Giving Jacob gradually increasing doses of peanuts, she hoped, would desensitize his immune system.
It's a strategy Kingsley hadn't pursued until she reached her breaking point. A year earlier, Jacob had swallowed a handful of popcorn that, unbeknownst to him, was laced with peanut product. He suffered a particularly frightening reaction: two bouts of intense symptoms about 6 hours apart. The incident marked his second peanut-related trip to the emergency room, and Kingsley was terrified that the next encounter could be fatal. “I decided, ‘I can't live like this,’” she says. “I was desperate.”
As Jacob sat through the hourslong appointment in Cincinnati, playing video games and swigging increasing doses of peanut-spiked Kool-Aid, he joined legions of children writing food allergy's next chapter. Today, more than 3000 people worldwide, most of them children, have undergone peanut immunotherapy, with the goal of protecting them if they accidentally encounter the food. Other children are trying immunotherapy for allergies to milk, eggs, and tree nuts. Some, like Jacob, get treatment in allergists' offices, where doctors share protocols informally and in published papers. Other children have enrolled in clinical trials, including those run by two companies racing to introduce a peanut-based capsule or skin patch. Both plan to apply for approval from the Food and Drug Administration (FDA) this year. The agency's blessing would dramatically boost immunotherapy's credibility and reach.
In a field that for decades has had nothing to offer patients beyond avoidance, immunotherapy marks a seismic shift. As it edges closer to mainstream, “There's mixed feelings, with a whole range of enthusiasm,” says Corinne Keet, a pediatric allergist-immunologist at Johns Hopkins Medicine in Baltimore, Maryland. Fear that it might cause harm is mingling with euphoria that children living constrained lives could be set free. Doctors who offer immunotherapy describe families eating in Chinese restaurants for the first time and home-schooled children rejoining their peers.
Like many medical firsts, the therapy is not perfect. “This is version 1.0,” says Brian Vickery, a pediatric allergist-immunologist at Emory University in Atlanta. He has conducted peanut immunotherapy trials and worked for 2 years at Aimmune Therapeutics, headquartered in Brisbane, California, one of the companies whose products are nearing approval. Physicians fret about oral immunotherapy's rigors—treatment must continue indefinitely—and its risks, which include the same allergic reactions it aims to prevent. Last year in Japan, a child suffered brain damage during a trial of immunotherapy for milk allergies.
Meanwhile, physicians on the front lines are navigating hazy science. No one knows exactly how immunotherapy works or who's most likely to be helped or hurt by it. “For me,” Keet says, “it's really not clear for an average child with peanut allergy whether it will make sense to do oral immunotherapy or not.”
LIKE MANY WHO STUDY food allergies, Keet was enticed by their mystery. Animal models are poor. The intensity of allergic reactions varies unpredictably, even in the same person over time. Why one child outgrows an allergy and another doesn't is unknown.
“This was something we didn't cover much in medical school” in the 1990s, says Matthew Greenhawt, a pediatric allergist-immunologist at Children's Hospital Colorado in Denver. Greenhawt's career trajectory tracks with a surge in food allergies, and these days, he can barely keep up with the stream of affected children who visit his hospital. Today, between 1% and 2% of people in the United States, the United Kingdom, and several other countries are allergic to peanuts—a rate that has roughly tripled since the mid-1990s. Other food allergies, such as those to tree nuts, are also on the rise. What's causing the increase is not well understood.
Despite rising caseloads, deaths from food allergies remain rare. Precise numbers are hard to come by, and estimates range from fewer than 10 to more than 150 a year in the United States. But even though an affected child is more likely to be struck by lightning than to die of a food allergy, the risk can feel ever-present. Parents never know when their children will happen upon culprit foods and how they'll be affected if they do. “We live in a complex world—people move food all over the place,” says David Bunning, a businessman whose two sons, now adults, have multiple food allergies. “The impact on children in terms of their confidence to explore their environment can be extreme.” Bunning's family almost never traveled or ate out. At their grandparents' house, the boys were usually confined to one room where food wasn't allowed.
Bunning now chairs the board of directors at Food Allergy Research & Education (FARE), an advocacy group in McLean, Virginia. Families like his, and the doctors who cared for their children, began to agitate for new treatments about a decade ago. Immunotherapy was the obvious candidate: Injections that desensitize the immune system to pollen, grass, pet dander, and bee venom have been around for decades.
Whether for an allergy to cats or pistachios, immunotherapy aims to disrupt the cells that swing out of control when faced with an allergen. When a child who is allergic to a food eats it, food proteins cross from the digestive tract into the bloodstream. An antibody called immunoglobulin E (IgE), which is bound to white blood cells called mast cells in tissues, recognizes the culprits. IgE activates the mast cells, which release histamine and other chemicals. In the skin, that response can lead to hives; in the respiratory tract, wheezing; and in the gut, vomiting. The most serious symptoms, such as a swollen throat or a reaction throughout the body, mark anaphylaxis, which is what families fear the most. Allergy shots blunt production of IgE, in part, researchers believe, by boosting levels of certain T cells that prompt a cascade of immune changes.
![Figure][1]
Fighting fire with fire
Eating gradually increasing doses of a food allergen seems to desensitize the immune system over time. Thousands of children have tried oral immunotherapy, and a capsule to treat peanut allergies might be approved by regulators next year. But there's anxiety about the strategy's risks and unknowns.
GRAPHIC: C. BICKEL/ SCIENCE
Brief testing decades ago indicated that shots for food allergies weren't safe. So around the mid-2000s, scientists began to feed children the allergen instead. One watershed moment came in 2005, when the National Institutes of Health formed a consortium for food allergy clinical trials. A second was in 2011, when advocates sponsored a symposium at Harvard Medical School in Boston to standardize goals and strategy for the pioneering immunotherapy efforts. About 60 people attended. “The patients were very clear,” says Carla McGuire Davis, a pediatric allergist-immunologist at Texas Children's Hospital in Houston. They didn't care about eating a peanut butter sandwich; they wanted protection if they accidentally encountered one. Trialists set their end dose at a couple of peanuts and pressed ahead.
The results of early clinical trials were promising, says Hugh Sampson, a pediatric allergist-immunologist at the Icahn School of Medicine at Mount Sinai in New York City, who has studied immunotherapy in food allergies for many years. After 6 to 12 months of treatment, he says, about 70% to 80% of patients could handle higher doses of the food than before. Lab data were encouraging, too: Ingesting allergens over time seems to make mast cells less reactive, inhibiting their release of harmful chemicals. The therapy also produces other immunoglobulins: IgG4, which further inhibits mast cell activity, and IgA, which helps keep food allergens from escaping the gut (see graphic, p. 280).
The 2011 conference inspired the founding of the company now called Aimmune, fueled by more than $3.5 million from FARE. A second company, DBV Technologies, based in Montrouge, France, and New York City, expanded a few years later. Aimmune began to develop an oral product, essentially a capsule of powder derived from peanut flour with proteins held to consistent levels. In February, the company announced in a press release the results of a phase III trial involving 496 children and teenagers, with a regimen stepping up every 2 weeks through 11 dose levels. Among the 372 people in the treatment group, about 20% dropped out for various reasons, including side effects. After about a year, 96% of people who completed treatment could consume one peanut with no more than mild symptoms, 84% could tolerate two, and 63% could tolerate at least three.
DBV's skin patch represents a more conservative strategy: It delivers tiny amounts of peanut protein, the equivalent of one peanut over 3 years. Last year, DBV announced that in its phase III trial of almost 400 patients, after a year, those using the patch could, on average, eat three peanuts over the course of several hours before experiencing clinical symptoms such as vomiting or hives; before the trial, the average was just under one peanut. Outcomes varied substantially from person to person.
If one or both products are approved by FDA in the coming months, expectations are high that they'll be welcomed: Aimmune is now worth about $1.5 billion on the U.S. stock exchange. In 2016, FARE sold its share in Aimmune for $47 million.
MEANWHILE, SOME DOCTORS embrace another route: offering peanut immunotherapy in their practices. “I can treat 20 patients with $5.95 of peanut flour,” says Richard L. Wasserman, a pediatric allergist-immunologist in Dallas, Texas.
Wasserman ventured into food allergy immunotherapy 11 years ago. He developed a protocol based partly on published case reports and protocols for allergy shots, and he put IVs into his first five peanut allergy patients in case he had only seconds to rescue them from severe anaphylaxis. “When they all sailed through the first day, we stopped doing IVs,” he says. “But that's a measure of how concerned I was.”
Wasserman has since treated more than 300 children with peanut allergies and more than 400 with other food allergies. Other practitioners are joining in, among them the Cincinnati allergist whom the Kingsley family sought out: Justin Greiwe at Bernstein Allergy Group. Greiwe joined the practice in 2014, straight out of medical training. “It was a little nerve-wracking at the beginning,” he says, because no officially sanctioned oral immunotherapy protocol existed. He took precautionary measures, such as lung testing before every treatment, to help ensure patient safety.
Some clinicians—and executives at the companies developing products—aren't happy about the doctor's office treatments. “That gives a lot of us pause,” says Sampson, who in addition to his academic post is chief scientific officer of DBV. “We're very afraid that if this goes on enough, somebody is going to have an accident or a fatal reaction, and that's really going to change the FDA's viewpoint” about the products in development, he says.
Wasserman agrees about the need for caution. “Not every practicing allergist should be doing oral immunotherapy,” he says. Greiwe suggests the treatment requires a dedicated staff, and he gives every immunotherapy family his cellphone number.
Jacob was one of Greiwe's first immunotherapy patients. His mother remembers Jacob's ears burning—a minor reaction that subsided on its own. “Or he said he hated peanuts and wanted to quit,” she says. Worst was about 6 months in, when Kingsley discovered that for 2 weeks, Jacob had hidden his dose to avoid eating it. That was “the only time we ever felt danger,” she says. Stopping treatment can quickly alter the immune system, says Cecilia Berin, an immunologist at Mount Sinai, because immunotherapy requires constant exposure. When Jacob squirreled away his daily dose, the changes induced in his immune system almost certainly started to fade out, putting him at risk. Greiwe restarted him on a lower dose and, his mother says, “We got through it.”
EVEN CHILDREN WHO faithfully follow instructions face risks. The immune system can react to even subtle pressures, and the list of what can provoke a reaction to treatment is long. Exercising within a couple of hours of the dose can do it; so can a cold, a stomach virus, menstruation, or a hot shower. An asthma attack can trigger a reaction—many children with allergies have asthma as well—and so can stress. “We had a patient who had just played the violin on a stage, came down, and about 15 minutes later … took the dose and had a reaction,” Davis says.
Berin posits that external pressures such as physical activity or illness make the gut more permeable, pushing more of the immunotherapy dose into the bloodstream. But that remains hypothesis. Regardless, it's becoming clear that “there are people who react years down the road to a maintenance dose,” Keet says. For Jacob, such a moment came 9 months in. One evening while watching a movie, he downed his peanut M&M's and later ran outside with his cousins to dance in a rainstorm. He broke out in hives head to toe. Kingsley dialed Greiwe's number, and Jacob got a double dose of an allergy medication.
![Figure][1]
Food allergies are becoming more common, and a handful of foods accounts for the vast majority of allergies. But small doses of the foods can blunt allergic reactions.
PHOTO: SCIENCE PHOTO LIBRARY/SCIENCE SOURCE
The most tragic data point to date is the case in Japan. A child had enrolled in a trial of immunotherapy for milk allergies at the Kanagawa Children's Medical Center in Yokohama. He'd raised what he could ingest from less than 8 milliliters to 135 milliliters—about half a glass of milk. After 3 months on that maintenance dose, he swallowed it and soon complained of pain. Within minutes, he had stopped breathing. His heartbeat was later restored in the emergency room, but he'd gone too long without it and sustained severe brain damage, according to a statement from the hospital's president, Sumimasa Yamashita, in November 2017. Kanagawa Children's Medical Center declined to comment, saying only that the incident remains under investigation.
In its statement, the hospital noted the boy had suffered an asthma attack the day before the catastrophic dose. He also was on a protocol that aimed to rapidly escalate the volume of milk he could drink over less than 3 weeks. But why the child reacted so disastrously to that glass of milk is unknown.
“What people don't understand is this level of protection fluctuates,” says Mimi Tang, a pediatric allergist-immunologist at Murdoch Children's Research Institute in Melbourne, Australia. “It is not guaranteed, nor is it constant.”
One of the few long-term analyses was published in 2013 in The Journal of Allergy and Clinical Immunology . Keet, pediatric allergist-immunologist Robert Wood at Johns Hopkins Medicine, and their colleagues sought out 32 children who'd been in a milk immunotherapy trial. Three to 5 years later, “The results were surprising in a sobering kind of way,” Wood says. Only about a quarter “were doing great … tolerating unlimited quantities of milk without side effects.” Another quarter had abandoned the protocol and returned to strict avoidance. The rest were eating dairy products inconsistently, with intermittent or even frequent allergic reactions. “It's hard to know which comes first, whether they got complacent” about ingesting it “or backed off because [they were] having too many symptoms,” Wood says.
MORE AND MORE families are willing to live with those uncertainties because the alternative is greater anxiety. “We were scared senseless,” says Divya Balachandar, whose daughter Leena Wong, now 7 years old, had her first episode of anaphylaxis at age 4 after being touched by a cashew. Testing revealed Leena also was allergic to sesame, eggs, milk, other tree nuts, and peanuts. Balachandar, a pediatric pulmonologist in New York City, and her husband enrolled Leena in a federally funded oral immunotherapy trial for peanut allergy in 2015. “It made me nervous, really nervous, to put something in my daughter's mouth that she was allergic to,” Balachandar says. She gravitated toward a trial over treatment with a local allergist because, she says, “there were no rules” about how to treat in private practice. By this spring, Leena could eat two spoonfuls of peanut butter—about 25 peanuts—without a problem. She started second grade sitting with her classmates at lunchtime, liberated from a separate nut-free table.
Both companies developing peanut-based treatments say they had more volunteers for their trials than they could accommodate. Private practitioners usually have a waiting list; Greiwe's runs more than 4 months. At Stanford University in Palo Alto, California, which has a large food allergy research program, more than 2000 patients are waitlisted to enroll in the university's clinical trials, says Sharon Chinthrajah, an allergist-immunologist there.
More treatments are on the horizon. In Australia, Tang is working with a company that's testing an approach she pioneered, a combination of a probiotic and oral peanut immunotherapy. The probiotic should tilt the body toward producing the subset of T cells that tolerate the allergen and away from making cells that attack it, she says. Chinthrajah and others are enthusiastic about combining oral immunotherapy with a monoclonal antibody called omalizumab, which is FDA approved to treat allergic asthma. Clinical trials are also gearing up to test other monoclonal antibodies that target molecules involved in allergic inflammation.
Jacob's and Leena's families are eager to see what comes next. Jacob is also allergic to pistachios and cashews, but because he finds those foods easier to avoid than peanuts, the family has rejected immunotherapy that targets them. Leena's family is the opposite. With her older sister and her parents, Leena attends Indian functions regularly, where tree nuts are a common ingredient in sauces. In August, another episode of anaphylaxis landed her in the emergency room: She began to vomit and suffered chest tightness and eye swelling after eating Indian food her parents suspect contained cashews—despite having triple-checked with the restaurant that it did not. “I would love to do tree nuts,” Balachandar says, once immunotherapy “becomes more available and better understood.”
Physicians with deep roots in food allergy immunotherapy hope those new to it tread carefully. Doctors who offer such treatments “have to know the data cold,” including published results and side effects that may crop up, Greenhawt says. Still, he's thrilled that peanut immunotherapy treatments may soon be approved. The other day, talking with a peanut-allergic 4-year-old and his mother, Greenhawt shared what the next year might bring. “I said, ‘I'm going to see you a year from now; hopefully, we will have two products that are approved, and we can talk about which one might be best for you.’” The mother looked startled and delighted, Greenhawt says. “I've never seen somebody smile as brightly as that.”
[1]: pending:yes
Via Krishan Maggon

|
Rescooped by
Gilbert C FAURE
from Immunology and Biotherapies
October 11, 2018 3:28 PM
|
1 Background There are limited data on the feasibility, efficacy and safety of high‐dose oral immunotherapy (OIT) in children highly allergic to peanuts. 2 Objective In children highly allergic to peanut, we primarily aimed to determine the feasibility of reaching the maximum maintenance dose (MMD) of 5000 mg peanut protein or, alternatively, a lower individual maintenance dose (IMD), by OIT up‐dosing. Secondarily, we aimed to identify adverse events (AEs) and determine factors associated with reaching a maintenance dose. 3 Methods The TAKE‐AWAY peanut OIT trial enrolled 77 children 5‐15 years old, with a positive oral peanut challenge. Fifty‐seven were randomized to OIT with biweekly dose step‐up until reaching MMD or IMD and 20 to observation only. Demographic and biological characteristics, AEs, medication and protocol deviations were explored for associations with reaching maintenance dose. 4 Results All children had anaphylaxis defined by objective symptoms in minimum two organ systems during baseline challenge. The MMD was reached by 21.1%, while 54.4% reached an IMD of median (minimum, maximum) 2700 (250, 4000) mg peanut protein, whereas 24.5% discontinued OIT. During up‐dosing, 19.4% experienced anaphylaxis. Not reaching the MMD was caused by distaste for peanuts (66.7%), unacceptable AEs (26.7%) and social reasons (6.7%). Increased peanut s‐IgG4/s‐IgE ratio (OR [95% CI]: 1.02 [1.00, 1.04]) was associated with reaching MMD. 5 Conclusion Although 75.5% of children with peanut anaphylaxis reached a maintenance dose of 0.25‐5 g, only 21.1% reached the MMD. Distaste for peanuts and AEs, including high risk of anaphylaxis, limited the feasibility of reaching MMD.
Via Krishan Maggon

|
Scooped by
Gilbert C FAURE
September 18, 2018 12:03 PM
|
People with autosomal dominant hyper-immunoglobulin E syndrome (HIES) have recurrent bacterial infections of the skin and lungs. Patients with HIES typically also have eczema, distinct facial features, and a tendency to experience bone fractures. The disease has several other names, including Job’s syndrome, STAT3 deficiency, and Buckley syndrome. HIES is a primary immune deficiency disease (PIDD). For more information on PIDD research and patient care at NIAID, visit the NIAID PIDD site. For further information about HIES, visit the National Library of Medicine, Genetics Home Reference autosomal dominant hyper-IgE syndrome site. What's New Latest News Releases NIAID and Children’s National Partner to Advance Pediatric Clinical Research, September 17, 2018 NIAID Scientists Identify Cause, Possible Treatment for Life-Threatening Gut Condition, June 28, 2017 NIAID Scientists Discover Rare Genetic Susceptibility to Common Cold, June 12, 2017 NIAID Now Blog Video: Understanding Immune Cell Defects in Chediak-Higashi Syndrome, December 15, 2017 56 Years Later, NIAID Scientists Find Gene Behind NIH Distinguished Investigator’s Eponymous Syndrome, October 11, 2017 Causes Most cases of autosomal dominant HIES result from mutations in the gene that encodes a signaling protein called STAT3. This protein is involved in many different activities of the body, explaining why HIES affects facial appearance, bones, lungs, skin, and arteries. NIAID investigators identified the role of STAT3 in autosomal dominant HIES in 2007. Symptoms & Diagnosis People with HIES may have recurrent infections of the skin and lungs. These infections are often caused by the bacterium Staphylococcus aureus but also may be caused by other bacteria and fungi. Furthermore, people with HIES tend to have recurrent bone fractures, unusually flexible joints, and inflamed skin. Baby teeth in people with HIES often do not fall out on their own. A doctor will suspect HIES in a person with eczema, recurrent boils, and pneumonias. Treatment The most effective treatments for HIES are continuous antibiotics and antifungals as needed. Some patients receive antibody replacement therapy. Antiseptic approaches, such as dilute bleach baths, are often helpful to prevent skin infections and improve eczema. Watch an NIAID video on wet-wrap therapy for eczema. Clinical Trials NIAID-supported clinical research seeks to determine the effect of HIES on the immune system, including which immune cells and responses are affected and how these abnormalities translate into patient's symptoms. Read more about selected clinical trials that are seeking volunteers

|
Scooped by
Gilbert C FAURE
September 2, 2018 5:08 AM
|
There are two types of IgE-mediated reactions to stinging insects: large local reactions and systemic reactions. Acute management of large local reactions is symptomatic and a patient history of a large local reaction does not indicate need for an epinephrine auto-injector or venom immunotherapy.

|
Scooped by
Gilbert C FAURE
August 16, 2018 3:58 PM
|
<b><i>Background:</i></b> The diagnosis of drug hypersensitivity reactions (DHRs) is based both on clinical history and in vivo tests, such as specific IgE and cutaneous tests, when available.<b><i>O...
|



 Your new post is loading...
Your new post is loading...