Your new post is loading...
 Your new post is loading...

|
Scooped by
Gilbert C FAURE
December 18, 2022 7:22 AM
|
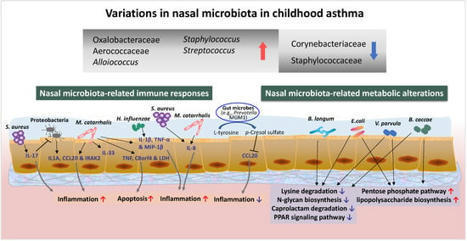
Childhood asthma is a major chronic non-communicable disease in infants and children, often triggered by respiratory tract infections. The nasal cavity is a reservoir for a broad variety of commensal microbes and potential pathogens associated with respiratory illnesses including asthma.

|
Scooped by
Gilbert C FAURE
December 10, 2022 1:53 AM
|
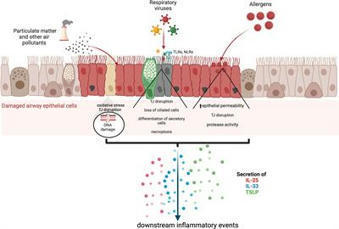
Asthma is a heterogeneous, chronic respiratory disease affecting 300 million people and is thought to be driven by different inflammatory endotypes influenced by a myriad of genetic and environmental factors. The complexity of asthma has rendered it challenging to develop preventative and disease modifying therapies and it remains an unmet clinical need. Whilst many factors have been implicated in asthma pathogenesis and exacerbations, evidence indicates a prominent role for respiratory viruses. However, advances in culture-independent detection methods and extensive microbial profiling of the lung, have also demonstrated a role for respiratory bacteria in asthma. In particular, airway colonization by the Proteobacteria species Nontypeable Haemophilus influenzae (NTHi) and Moraxella catarrhalis (Mcat) is associated with increased risk of developing recurrent wheeze and asthma in early life, poor clinical outcomes in established adult asthma and the development of more severe inflammatory phenotypes. Furthermore, emerging evidence indicates that bacterial-viral interactions may influence exacerbation risk and disease severity, highlighting the need to consider the impact chronic airway colonization by respiratory bacteria has on influencing host responses to viral infection. In this review, we first outline the currently understood role of viral and bacterial infections in precipitating asthma exacerbations and discuss the underappreciated potential impact o

|
Scooped by
Gilbert C FAURE
October 15, 2022 8:57 AM
|
The exposure of the airway epithelium to external stimuli such as allergens, microbes, and air pollution triggers the release of the alarmin cytokines IL-25, IL-33 and thymic stromal lymphopoietin (TSLP). IL-25, IL-33 and TSLP interact with their ligands, IL-17RA, IL1RL1 and TSLPR respectively, expressed by hematopoietic and non-hematopoietic cells including dendritic cells, ILC2 cells, endothelial cells, and fibroblasts. Alarmins play key roles in driving type 2-high, and to a lesser extent type 2-low responses, in asthma. In addition, studies in which each of these three alarmins were targeted in allergen-challenged mice showed decreased chronicity of type-2 driven disease. Consequently, ascertaining the mechanism of activity of these upstream mediators has implications for understanding the outcome of targeted therapies designed to counteract their activity and alleviate downstream type 2-high and low effector responses. Furthermore, identifying the factors which shift the balance between the elicitation of type 2-high, eosinophilic asthma and type-2 low, neutrophilic-positive/negative asthma by alarmins is essential. In support of these efforts, observations from the NAVIGATOR trial imply that targeting TSLP in patients with tezepelumab results in reduced asthma exacerbations, improved lung function and control of the disease. In this review, we will discuss the mechanisms surrounding the secretion of IL-25, IL-33, and TSLP from the airway epithelium and how thi

|
Scooped by
Gilbert C FAURE
October 3, 2022 3:48 AM
|
A Th2 immune response is central to allergic airway inflammation, which afflicts millions worldwide. However, the mechanisms that augment GATA3 expression in an antigen-primed developing Th2 cell are not well understood.

|
Scooped by
Gilbert C FAURE
April 23, 2022 11:05 AM
|
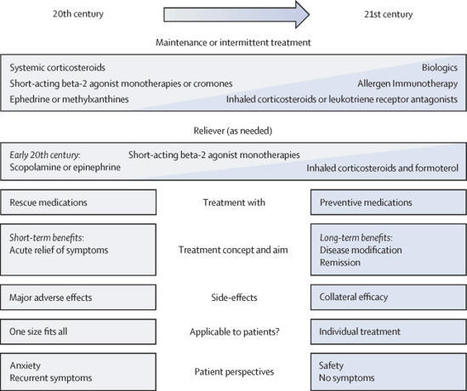
Drugs available for asthma treatment in the first decades of the 20th century (sympathomimetic agents such as oral ephedrine, intravenous adrenaline, or inhaled epinephrine; anticholinergics such as inhaled scopolamine; methylxanthines such as oral caffeine or theophylline1) aimed at relieving...

|
Scooped by
Gilbert C FAURE
December 27, 2021 10:48 AM
|
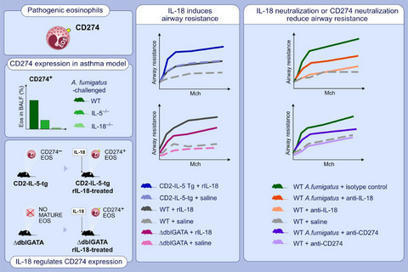
Abstract Background IL-5-dependent residential and IL-18-transformed pathogenic eosinophils have been reported; however, the role of IL-18-transformed CD274-expressing pathogenic eosinophils compar...

|
Scooped by
Gilbert C FAURE
October 24, 2021 2:18 PM
|
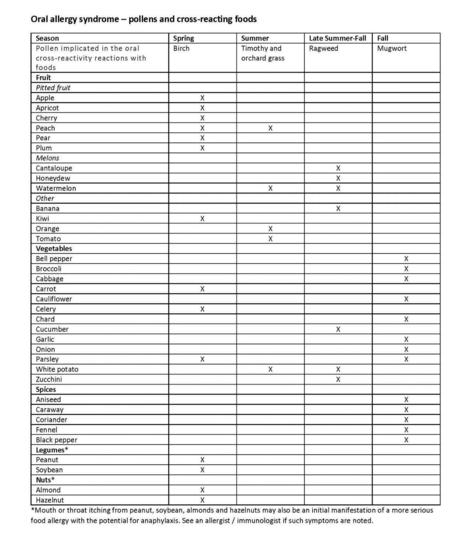
Understanding the relationship between outdoor and food allergies written and reviewed by the leading experts in allergy, asthma and immunology.

|
Scooped by
Gilbert C FAURE
July 29, 2021 5:09 AM
|

|
Scooped by
Gilbert C FAURE
April 18, 2021 4:57 AM
|
Abstract Secondary adrenal insufficiency (AI) occurs as the result of any process that disrupts normal hypothalamic and/or anterior pituitary function and causes a decrease in the secretion of ster...

|
Scooped by
Gilbert C FAURE
January 20, 2021 4:38 AM
|
Home: Reviews & News: Medical Journal Reviews: 2021: January 2021 Medical Journal Review January 2021 WAO Reviews – Editors' Choice Articles are selected for their importance to clinicians who care for patients with asthma and allergic/immunologic diseases by Juan Carlos Ivancevich, MD, and John J. Oppenheimer, MD - FACAAI - FAAAAI, WAO Reviews Editor. Asthma and COVID-19: Do we finally have answers? Eger K, Bel EH European Respiratory Journal 2020; in press https:/doi.org/10.1183/13993003.04451-2020 In this paper, Eger and Bel explore the impact of asthma on COVID 19. While it is well known that older age, obesity, cardiovascular disease, and diabetes are risk factors of poor COVID-19 outcome, much controversy surrounds asthma’s impact. The focus of this manuscript was 2 papers published in the same edition of the ERJ (Choi et al and Izquierdo et al). In summary, these large-scale studies confirmed previous findings regarding risk for asthma patients to develop (severe) COVID-19 – specifically that asthmatics appear to be slightly more susceptible to contracting COVID-19, but severe disease progression does not seem to be related to medication use, including asthma biologics, but rather linked to older age and co-morbidities. The authors stress the fact that often when examining studies of COVID-19 and asthma, potential bias factors have not been considered, leaving many questions unanswered. Furthermore, large-scale, multinational real-life studies with detailed information on asthma phenotype and medication usage in patients with a confirmed diagnosis of COVID-19 would be ideal to aid us in resolving these questions. The Metabolomics of Childhood Atopic Diseases: A Comprehensive Pathway-Specific Review Schjødt MS, Gürdeniz G, Chawes B Metabolites 2020;10(12):511 https://doi.org/10.3390/metabo10120511 Asthma, allergic rhinitis, food allergy, and atopic dermatitis are common childhood diseases with several different underlying mechanisms, i.e., endotypes of disease. In this review, the authors stress that metabolomics has the potential to identify disease endotypes, which could beneficially promote personalized prevention and treatment. They do a wonderful job of reviewing the metabolomics literature in children with atopic diseases, focusing on tyrosine and tryptophan metabolism, lipids (particularly, sphingolipids), polyunsaturated fatty acids, microbially derived metabolites (particularly, short-chain fatty acids), and bile acids. Specifically, tyrosine, 3-hydroxyphenylacetic acid, N-acetyltyrosine, tryptophan, indolelactic acid, 5-hydroxyindoleacetic acid, p-Cresol sulfate, taurocholic acid, taurochenodeoxycholic acid, glycohyocholic acid, glycocholic acid, and docosapentaenoate n-6 were identified in at least two studies as being impactful. They stress that altered metabolic pathways highlight some of the underlying biochemical mechanisms leading to these common childhood disorders, which in the future could provide utility in clinical practice. Much further work on this topic is still needed. Helicobacter pylori and skin disorders: a comprehensive review of the available literature Guarneri C, Ceccarelli M, Rinaldi L, Cacopardo B, Nunnari G, Guarneri F European Review for Medical and Pharmacological Sciences 2020;24(23):12267-12287 https://www.doi.org/10.26355/eurrev_202012_24019 Helicobacter pylori is a Gram-negative bacterium identified for the first time about 30 years ago and commonly considered as the main pathogenic factor of gastritis and peptic ulcer. Since then, it was found to be associated with several gastrointestinal and extra-gastrointestinal diseases, including skin disorders such as chronic urticaria, rosacea, lichen planus, atopic dermatitis, psoriasis, pemphigus vulgaris, vitiligo, primary cutaneous MALT-type lymphoma, sublamina densa-type linear IgA bullous dermatosis, primary cutaneous marginal zone B-cell lymphomas, and cutaneous T-cell pseudolymphoma. The aim of this review is to summarize the available studies regarding the topic and draw possible conclusions. The authors found that, overall, further clinical and laboratory studies are needed to assess the real plausibility and relevance of these associations, as well as the possible role of Helicobacter pylori with the underlying pathogenic mechanisms. Allergy prevention: An overview of current evidence Royal C, Gray C Yale Journal of Biology and Medicine 2020;93(5):689-698 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7757062/ There has been a rapid rise in allergic disorders worldwide, which has resulted in increased research into the determinants of allergy development in attempt to identify factors that may be manipulated to mitigate risk. Present literature demonstrates that an opportune window in immunological development appears to exist in early life, whereby certain exposures may promote or prevent the development of an allergic disposition. Furthermore, factors that affect the composition and diversity of the microbiome in early life may also be impactful. In this review, the authors explore the current literature and recommendations relating to exposures that may prevent allergy development or promote tolerance. They note several risk factors, including delivery by caesarean section, omission of breastfeeding, vitamin D insufficiency, and environmental exposures, such as cigarette smoke exposure, all increase the risk of an allergic predisposition. Likewise, they note several protective factors, including dietary diversity during pregnancy, lactation, and in infancy is protective. They also note that recommendations for food-allergen exposure have shifted from delayed introduction to early introduction as a tolerance-inducing strategy. Supplements such as probiotics and vitamins during pregnancy and infancy have yet to produce conclusive results for allergy prevention. Finally, they note that emollient use in infancy has not been shown to be protective against eczema or food allergy. The airways microbiome of individuals with asthma treated with high and low doses of inhaled corticosteroids Martin MJ, Zain NMM, Hearson G, Rivett DW, Koller G et al PLoS One 2020;15(12):e0244681 https://www.doi.org/10.1371/journal.pone.0244681 Inhaled corticosteroids (ICS) are the mainstay of asthma treatment, but evidence suggests a link between ICS usage and increased rates of respiratory infections. In this study, Martin and colleagues assessed the composition of the asthmatic airways microbiome in patients taking low and high dose ICS and the stability of the microbiome over a 2-week period. Sputum from each subject underwent DNA extraction, amplification and 16S rRNA gene sequencing of the bacterial component of the microbiome. Nineteen subjects returned for further sputum induction after 24 h and 2 weeks. A total of 5,615,037 sequencing reads revealed 167 bacterial taxa in the asthmatic airway samples, with the most abundant being Streptococcus spp. No significant differences in sputum bacterial load or overall community composition were seen between the low- and high-dose ICS groups; however, Streptococcus spp. showed significantly higher relative abundance in subjects taking low-dose ICS (p = 0.002). Furthermore, Haemophilus parainfluenzae was significantly more abundant in subjects on high-dose fluticasone propionate compared to those on high-dose budesonide (p = 0.047). There were no statistically significant changes in microbiota composition over a 2-week period. The authors note that the clinical implications for patients are not known, but suggest that this does provide a possible explanation for the increased risk of pulmonary infection seen in asthma and COPD, particularly with FP. More research is needed.

|
Scooped by
Gilbert C FAURE
November 13, 2020 1:31 PM
|
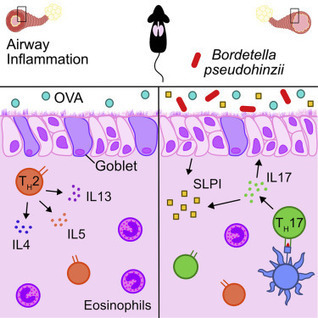
Asthma is known to be modified by airway microbes. Jaeger et al. use a murine-adapted
bacterium to show that airway colonization evokes a Th17 response associated with
increased SLPI, an antimicrobial peptide, and protection from lung inflammation.

|
Scooped by
Gilbert C FAURE
September 12, 2020 4:20 AM
|
Morning Session Morning Chair: Dr Tom Marrs 09:00 Welcome and Introduction Dr Tom Marrs Consultant in Paediatric Allergy St Thomas' Hospital, London 09:10 Remote managment of eczema and urticaria in primary care Dr Alya Abdul-Wahab Consultant Dermatologist St George's Hospital, London 09:50 How to fix common gastro-intestinal symptoms in children Dr Rakesh Vora Paediatric Gastroenterology Consultant St Thomas' Hospital, London 10:35 << BREAK >> 11:00 How to manage IgE and non-IgE food allergies Dr Tom Marrs Consultant in Paediatric Allergy St Thomas' Hospital, London 11:40 How to recomment avoidance of egg and nuts Rebecca Brocklehurst Paediatric Allergy Dietitian St Thomas' Hospital, London 12:20 << LUNCH >> Afternoon Session Afternoon Chair: Dr Rosy Wells 13:00 Preventing food allergy: what to tell parents Dr Michael Perkin Consultant Allergist and Reader in Clinical Epidemiology St George's Hospital, London 13:30 Priorities to Tell Families Living With Food Allergy Professor Adam Fox Professor in Paediatric Allergy St Thomas' Hospital, London 14:00 QUICK FIRE: Adrenaline auto-injector guide IN PRACTICE: Spare pens in schools Alia Boardman Clinical Nurse Specialst in Paediatric Allergy St George's Hospital, London 14:30 << BREAK >> 15:00 Managing Long-Term Asthma in a Virtual World Dr Richard Iles Paediatric Respirology Consultant St Thomas' Hospital, London 15:40 How to recognise and treat allergic rhinitis Dr Anne Chsitopher Consultant Paediatrician and Allergist St George's Hospital, London 16:10 New inhalers and nasal sprays Katherine Knight Clinical Nurse Specialist in Paediatric Allergy St Thomas' Hospital, London 16:40 Webinar feedback and Close of meeting

|
Rescooped by
Gilbert C FAURE
from Mucosal Immunity
August 9, 2020 9:28 AM
|
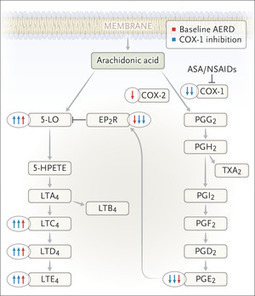
Aspirin-Exacerbated Respiratory Disease About 7% of patients with asthma have mucosal swelling, nasal polyps, and worsening of asthma in response to aspirin and other COX-1 inhibitors. Symptoms may...
|

|
Scooped by
Gilbert C FAURE
December 10, 2022 10:23 AM
|
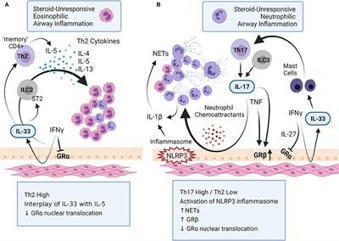
Asthma is a heterogeneous respiratory disease characterized by airflow obstruction, bronchial hyperresponsiveness and airway inflammation. Approximately 10% of asthma patients suffer from uncontrolled severe asthma (SA). A major difference between patients with SA from those with mild-to-moderate asthma is the resistance to common glucocorticoid treatments. Thus, steroid-unresponsive uncontrolled asthma is a hallmark of SA. An impediment in the development of new therapies for SA is a limited understanding of the range of immune responses and molecular networks that can contribute to the disease process. Typically SA is thought to be characterized by a Th2-low and Th17-high immunophenotype, accompanied by neutrophilic airway inflammation. However, Th2-mediated eosinophilic inflammation, as well as mixed Th1/Th17-mediated inflammation, is also described in SA. Thus, existing studies indicate that the immunophenotype of SA is diverse. This review attempts to summarize the interplay of different immune mediators and related mechanisms that are associated with airway inflammation and the immunobiology of SA.

|
Scooped by
Gilbert C FAURE
November 14, 2022 4:54 AM
|
Allergist Kathleen May, MD, of Augusta, GA was installed as president of the American College of Allergy, Asthma and Immunology at the ACAAI Annual Scientific M...

|
Scooped by
Gilbert C FAURE
October 10, 2022 3:22 AM
|
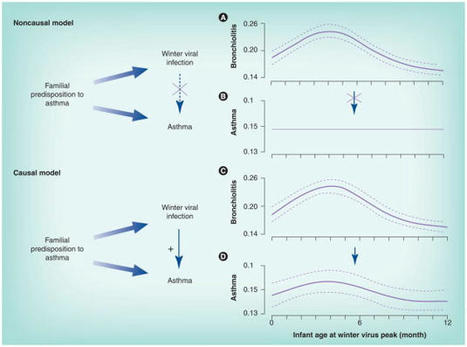
Respiratory syncytial virus (RSV) infects all children early in life, is the most common cause of infant lower respiratory tract infections, and causes disease exacerbations in children with asthma. Episodes of lower respiratory tract infection in early ...

|
Scooped by
Gilbert C FAURE
July 25, 2022 8:38 AM
|
Traditional farming lifestyle has been shown to be protective against asthma and allergic diseases. The individual factors that appear to be associated with this "farm-life effect" include consumption of unpasteurized farm milk and exposure to farm animals and stables.

|
Scooped by
Gilbert C FAURE
February 17, 2022 11:02 AM
|
There have been no worldwide standardised surveys of prevalence and severity of asthma, rhinoconjunctivitis and eczema in school children for 15 years.The present study aims to provide this information.Following the exact International Study of Asthma and Allergies in Childhood (ISAAC) methodology...

|
Scooped by
Gilbert C FAURE
November 3, 2021 3:55 AM
|
Abstract Background Interleukin-23 has been implicated in airway inflammation that is mediated by type 2 and type 17 cytokines. Whether targeting interleukin-23 in the treatment of asthma improve

|
Scooped by
Gilbert C FAURE
October 24, 2021 2:14 PM
|
We are a European alliance of 39 allergy, asthma and chronic obstructive pulmonary disease (COPD) patients’ associations representing 30% of European citizens currently living with these diseases. Our mission is to convey their voice and to be actively involved in the decisions impacting their...

|
Scooped by
Gilbert C FAURE
May 29, 2021 10:22 AM
|
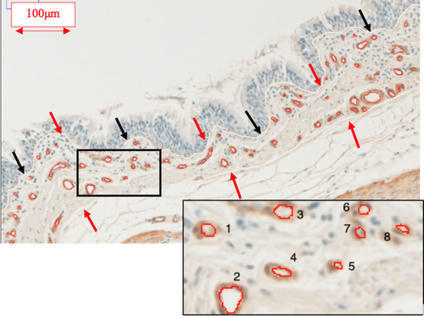
Abstract Background Severe asthma in horses is characterized by structural changes that thicken the lower airway wall, a change that is only partially reversible by current treatments. Increased va...

|
Scooped by
Gilbert C FAURE
April 3, 2021 7:00 AM
|
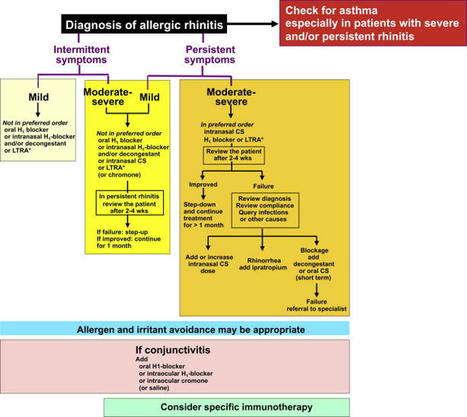
Allergic rhinitis (AR) and asthma represent global health problems for all age groups.
Asthma and rhinitis frequently coexist in the same subjects. Allergic Rhinitis and
its Impact on Asthma (ARIA) was initiated during a World Health Organization workshop
in 1999 (published in 2001).

|
Scooped by
Gilbert C FAURE
December 4, 2020 1:49 AM
|
SLIT is effective, tolerable, and convenient for many allergic patients. Still, real-world evidence is scarce and the aim of this study is to assess the patient-reported outcome of treatment with SLIT against grass pollen allergy in a consecutive patient population. The total sample size consisted of 329 patients who were confirmed to be allergic to timothy grass and had been prescribed SLIT were consecutively enrolled in the study and completed a questionnaire online or in hard copy. 207 patients provided their responses to the administered questionnaire. 113 patients reported they had completed the full 3-year treatment period, 49 were still on treatment, and 45 had discontinued treatment prematurely. The betterment of asthma was twice as common among patients who completed compared to discontinued treatment. Younger age and a higher prevalence of reported oral and/or gastrointestinal side effects characterized the group that terminated SLIT. Forgetfulness was the most commonly reported specific reason. The study concluded through its findings that the treatment perseverance resulted in the improved patient-reported outcome. Forgetfulness was the most frequently reported reason for discontinuing SLIT treatment against grass pollen allergy. Reference: https://clinicalmolecularallergy.biomedcentral.com/articles/10.1186/s12948-018-0093-8

|
Scooped by
Gilbert C FAURE
November 8, 2020 6:08 AM
|
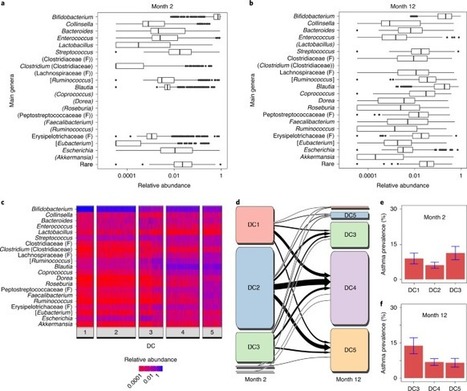
Growing up on a farm is associated with an asthma-protective effect, but the mechanisms underlying this effect are largely unknown. In the Protection against Allergy: Study in Rural Environments (PASTURE) birth cohort, we modeled maturation using 16S rRNA sequence data of the human gut microbiome in infants from 2 to 12 months of age. The estimated microbiome age (EMA) in 12-month-old infants was associated with previous farm exposure (β = 0.27 (0.12–0.43), P = 0.001, n = 618) and reduced risk of asthma at school age (odds ratio (OR) = 0.72 (0.56–0.93), P = 0.011). EMA mediated the protective farm effect by 19%. In a nested case–control sample (n = 138), we found inverse associations of asthma with the measured level of fecal butyrate (OR = 0.28 (0.09–0.91), P = 0.034), bacterial taxa that predict butyrate production (OR = 0.38 (0.17–0.84), P = 0.017) and the relative abundance of the gene encoding butyryl–coenzyme A (CoA):acetate–CoA-transferase, a major enzyme in butyrate metabolism (OR = 0.43 (0.19–0.97), P = 0.042). The gut microbiome may contribute to asthma protection through metabolites, supporting the concept of a gut–lung axis in humans. Growing up in the rich microbial environment of a farm strongly influences the maturation of the gut microbiome in the first year of life, which helps protect against the development of asthma in children.

|
Suggested by
LIGHTING
September 11, 2020 3:20 PM
|
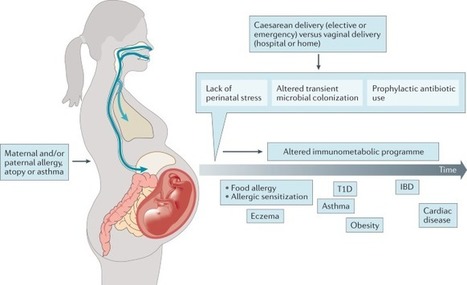
Allergies, including asthma, food allergy and atopic dermatitis, are increasing in prevalence, particularly in westernized countries. Although a detailed mechanistic explanation for this increase is lacking, recent evidence indicates that, in addition to genetic predisposition, lifestyle changes owing to modernization have an important role. Such changes include increased rates of birth by caesarean delivery, increased early use of antibiotics, a westernized diet and the associated development of obesity, and changes in indoor and outdoor lifestyle and activity patterns. Most of these factors directly and indirectly impact the formation of a diverse microbiota, which includes bacterial, viral and fungal components; the microbiota has a leading role in shaping (early) immune responses. This default programme is markedly disturbed under the influence of environmental and lifestyle risk factors. Here, we review the most important allergy risk factors associated with changes in our exposure to the microbial world and the application of this knowledge to allergy prevention strategies. Here, the authors explore how the modern way of life increases the risk of allergy and asthma, in particular by affecting the formation and diversity of the microbiota in early life. Understanding these changes highlights strategies for allergy prevention.
|

 Your new post is loading...
Your new post is loading...
 Your new post is loading...
Your new post is loading...