Your new post is loading...
 Your new post is loading...

|
Rescooped by
Gilbert C FAURE
from Osteoporosis New drugs Review
November 25, 2018 2:18 PM
|
Dependable discs
Intervertebral disc degeneration causes back and neck pain, sometimes necessitating disc fusion surgery. Although fusion may alleviate symptoms, it does not address the underlying cause of degeneration. As an alternative to fusion, Gullbrand and colleagues developed tissue-engineered discs for disc replacement by sandwiching hydrogel and polymer materials seeded with cartilage or mesenchymal stem cells between acellular polymer endplates. Engineered discs integrated with native discs, maintaining their structure and showing near-native mechanical properties 5 months after implantation in a rodent disc replacement model. Similar results were seen 2 months after implantation in a goat model, demonstrating the translational feasibility of this tissue engineering approach.
Abstract
Tissue engineering holds great promise for the treatment of advanced intervertebral disc degeneration. However, assessment of in vivo integration and mechanical function of tissue-engineered disc replacements over the long term, in large animal models, will be necessary to advance clinical translation. To that end, we developed tissue-engineered, endplate-modified disc-like angle ply structures (eDAPS) sized for the rat caudal and goat cervical spines that recapitulate the hierarchical structure of the native disc. Here, we demonstrate functional maturation and integration of these eDAPS in a rat caudal disc replacement model, with compressive mechanical properties reaching native values after 20 weeks in vivo and evidence of functional integration under physiological loads. To further this therapy toward clinical translation, we implanted eDAPS sized for the human cervical disc space in a goat cervical disc replacement model. Our results demonstrate maintenance of eDAPS composition and structure up to 8 weeks in vivo in the goat cervical disc space and maturation of compressive mechanical properties to match native levels. These results demonstrate the translational feasibility of disc replacement with a tissue-engineered construct for the treatment of advanced disc degeneration.
Via Krishan Maggon

|
Scooped by
Gilbert C FAURE
November 17, 2018 5:09 AM
|
Abstract Objective To estimate the prevalence and distribution of asymptomatic monosodium urate monohydrate (MSU) crystal deposition in sons of patients with gout. Methods Patients with gout were mailed an explanatory letter with an enclosed postage‐paid study packet to mail to their son(s) age ≥20 years old. Sons interested in participating returned a reply form and underwent telephone screening. Subsequently, they attended a study visit at which blood and urine samples were obtained and musculoskeletal ultrasonography was performed, with the sonographer blinded with regard to the subject's serum urate level. Images were assessed for double contour sign, intraarticular or intratendinous aggregates/tophi, effusion, and power Doppler signal. Logistic regression was used to examine associations. Adjusted odds ratios (ORadj) and 95% confidence intervals (95% CIs) were calculated. Results One hundred thirty‐one sons (mean age 43.8 years, mean body mass index 27.1 kg/m2) completed assessments. The serum urate level was ≥6 mg/dl in 64.1%, and 29.8% had either a double contour sign or intraarticular aggregates/tophi in ≥1 joint. All participants with MSU deposition had involvement of 1 or both first metatarsophalangeal joints. Intratendinous aggregates were present in 21.4% and were associated with intraarticular MSU crystal deposits (ORadj 2.96 [95% CI 1.17–7.49]). No participant with a serum urate level of ≤5 mg/dl had MSU crystal deposition seen on ultrasonography, and 24.2% of those with serum urate levels between 5 and 6 mg/dl had ultrasonographic MSU deposition. MSU crystal deposition was associated with increasing serum urate levels (ORadj 1.61 [95% CI 1.10–2.36] for each increase of 1 mg/dl). Conclusion Asymptomatic sons of patients with gout frequently have hyperuricemia and MSU crystal deposits. In this study MSU crystal deposits were present in participants with serum urate levels of ≥5 mg/dl. Evaluation of subjects without a family history of gout is needed to determine whether the threshold for MSU crystal deposition is also lower in the general population. Gout is the most common form of inflammatory arthritis and results from persistent hyperuricemia that causes intra‐ and periarticular monosodium urate monohydrate (MSU) crystal deposition. It has multiple risk factors including genetic factors that act by modulating renal uric acid excretion 1. The heritability of serum urate and urinary uric acid excretion is estimated to be ~60% and 60–87%, respectively 2, while the heritability of gout is lower at 17.0% and 35.1% in Taiwanese women and men, respectively 3, and was estimated to range between 0% and 58% in a study from the US 1. As 14.5–25% of people with high serum urate levels have asymptomatic MSU crystal deposition 4-6, studies that use a symptomatic disease phenotype may underestimate the heritability of MSU crystal deposition. The prevalence of asymptomatic MSU crystal deposition in people at high genetic risk of gout, e.g., those with a parent who has gout, is not known. It has implications for screening and primary prevention of symptomatic gout and contrasts with rheumatoid arthritis, in which familial risk and prevalence of autoantibodies in first‐degree relatives are well understood. Thus, we undertook the present study to 1) examine the prevalence and distribution of asymptomatic MSU crystal deposition among sons of people with gout; 2) examine the association between serum urate, age, and asymptomatic MSU crystal deposition; and 3) explore whether parental age at gout onset is associated with asymptomatic MSU crystal deposition in sons. Patients and Methods Study design, subject recruitment, and ethics approval. This community‐based cross‐sectional study was approved by the Nottingham NHS Research Ethics Committee 2 (Rec ref: 15/EM/0316). People with self‐reported physician‐diagnosed gout who had participated in previous surveys at Academic Rheumatology, University of Nottingham and consented to future research contact were mailed a letter informing them of the present study and were asked to mail an enclosed study packet to their sons age ≥20 years. Sons of patients with primary gout who attended the rheumatology clinic at the Nottingham NHS Treatment Centre were approached in a similar manner, and the study was advertised on Facebook and once in a local newspaper. These advertisements were targeted at sons living in and around Nottingham who have a parent with gout. Sons who returned a reply form or contacted us in response to the advertisements underwent a telephone screening questionnaire to exclude those with gout 7. The screening questionnaire included questions that form part of the 8‐point chronic gout diagnosis (CGD) scale 7. The CGD scale includes current or past history of attack of acute arthritis, monoarthritis or oligoarthritis, rapid progression of pain and swelling (<24 hours), podagra, erythema, unilateral tarsitis, tophi, and hyperuricemia 7. As serum urate was not measured at the screening visit in this study, a history of hyperuricemia was substituted. Participants scoring ≤3 on the CGD were invited for the study visit. Study visit. Participants attended a study visit at which data on demographic characteristics, lifestyle factors, comorbidities, and drug prescriptions were collected. Targeted musculoskeletal assessment was performed, height, weight, and blood pressure were measured, and random blood and second‐void early‐morning urine samples were collected. Serum urate and creatinine and urinary uric acid and creatinine were measured at the clinical pathology laboratories of Nottingham University Hospitals NHS Trust. Fractional excretion of uric acid (FEUA) was calculated as ([urinary uric acid × serum creatinine]/[serum urate × urinary creatinine]) × 100% 8. Ultrasonography was performed by a rheumatologist with 5 years of ultrasonography experience (AA), who was blinded with regard to the subject's serum urate level. The ultrasonographic examination involved assessment of both first metatarsophalangeal (MTP) joints, talar domes, femoral condyles, second metacarpophalangeal joints, wrist triangular fibrocartilages, and patellar and triceps tendon insertions 9. These joints and tendons were chosen as they have best sensitivity and specificity for differentiating subjects with gout from those with other arthropathies 9. Ultrasound images were scored for double contour sign, intraarticular or intratendinous tophi/aggregates, and hyperechoic deposits (present or absent, as defined by the Outcome Measures in Rheumatology group 10). Joint effusion and power Doppler signal were graded on a 0–3 scale. All ultrasonographic assessments were performed using a Toshiba Aplio machine (8–14 MHz). Images with inconclusive readings were reviewed by a second ultrasonographer with >15 years of ultrasonography experience (PC), also under blinded conditions with regard to the subject's serum urate level. For the purpose of this study, MSU crystal deposits were defined as present if there was an intraarticular double contour sign or tophi/aggregates. Hyperechoic deposits alone were not sufficient to define MSU crystal deposits. When available, data on sex of the parent with gout and age at onset of gout were extracted from databases at Academic Rheumatology, University of Nottingham. Statistical analysis. The mean ± SD and the number (%) were used to describe continuous and categorical data, respectively. Independent‐sample t‐tests and chi‐square tests were used for univariate analysis; the Kruskal‐Wallis test was used if the data were nonparametric. Logistic regression was used to examine the association between intraarticular MSU crystal deposition at any joint in an individual and 1) serum urate level, 2) FEUA, 3) age, and 4) intratendinous aggregates/tophi at any tendon. The associations were adjusted for age where required, body mass index (kg/m2), current purine‐rich alcohol consumption (yes/no), hypertension (yes/no), hyperlipidemia (yes/no), diabetes (yes/no), estimated glomerular filtration rate (ml/minute), and father with gout (yes/no). Adjusted odds ratios (ORadj) and 95% confidence intervals (95% CIs) were calculated. The individual was the unit of analysis. Statistical calculations were performed using Stata version 15. P values less than 0.05 were considered significant. Results One hundred thirty‐four participants were recruited into the study: 125 via postal survey (1,435 study packets sent, 249 replies received), 6 from among sons of gout patients attending Nottingham University Hospitals NHS Trust, and 3 from advertisements. The 3 individuals recruited from advertisements did not present for ultrasonographic assessment and were excluded from further analysis. The serum urate level was ≥6 mg/dl in 64.1% of the subjects and ≥7 mg/dl in 29.0%. Demographic characteristics and comorbidities of the 131 participants are summarized in Table 1. The mean ± SD FEUA was 5.33 ± 1.87%, and FEUA was low (defined as ≤6.6%) in 78.6% of the subjects with a serum urate level of ≥6 mg/dl. Total Asymptomatic MSU crystal deposition Present (n = 39) Absent (n = 92) Age, mean ± SD years 43.80 ± 11.20 44.20 ± 8.91 43.63 ± 12.08 Age 20–29 years, no. (%) 20 (15.3) 3 17 Age 30–39 years, no. (%) 27 (20.6) 10 17 Age 40–49 years, no. (%) 40 (30.5) 15 25 Age 50–59 years, no. (%) 36 (27.5) 10 26 Age 60–69 years, no. (%) 8 (6.1) 1 7 Body mass index, mean ± SD kg/m2 27.10 ± 4.75 27.65 ± 3.99 26.85 ± 5.04 Current purine‐rich alcohol consumption, no. (%) 97 (74.1) 31 (79.5) 66 (71.7) Weekly purine‐rich alcohol intake, median (IQR) units 10 (5–20) 10 (5–20) 10 (4–20) Hypertension, no. (%) 12 (9.2)b 3 (7.7) 9 (9.8) Hyperlipidemia, no. (%) 10 (7.6)c 3 (7.7) 7 (7.6) Diabetes, no. (%) 2 (1.5)d 0 2 (2.2) eGFR, mean ± SD ml/minute 85.23 ± 7.19 85.21 ± 7.71 85.24 ± 7.00 Serum urate, mean ± SD mg/dl 6.41 ± 1.13 6.79 ± 0.96e 6.25 ± 1.16 Serum urate <5 mg/dl, no. (%) 14 (10.5) 0 14 Serum urate ≥5 and <6 mg/dl, no. (%) 33 (26.9) 8 25 Serum urate ≥6 and <7 mg/dl, no. (%) 46 (34.3) 18 28 Serum urate ≥7 and <8 mg/dl, no. (%) 27 (20.2) 8 19 Serum urate ≥8 and <9 mg/dl, no. (%) 9 (6.7) 4 5 Serum urate ≥9 mg/dl, no. (%) 2 (1.5) 1 1 FEUA, mean ± SD % 5.3 ± 1.9 5.3 ± 1.7 5.3 ± 1.9 Father with gout, no. (%) 111 (84.7) 33 (84.6) 78 (84.8) a All participants with asymptomatic monosodium urate monohydrate (MSU) crystal deposition had first metatarsophalangeal joint involvement. IQR = interquartile range; eGFR = estimated glomerular filtration rate; FEUA = fractional excretion of uric acid. b Eleven participants were prescribed antihypertensive drugs; 1 received bendroflumethiazide. c Six participants were prescribed statins. d Both participants were prescribed oral hypoglycemic drugs. e P = 0.01 versus participants without asymptomatic MSU crystal deposition. MSU crystal deposition was found in 29.8% of the subjects, with involvement of the first MTP joint (Figure 1) observed in all subjects in whom asymptomatic MSU crystal deposition was present. MSU crystal deposition was not found in any participant with a serum urate level of ≤5 mg/dl. Among the 262 first MTP joints examined, intraarticular aggregates were numerically more common than double contour sign (Table 2). Only 1 participant had a double contour sign at the ankle, and MSU crystal deposits were not present at the other joints examined. MSU crystal deposition at the first MTP joint was associated with grade ≥2 effusion at the same joint (ORadj 9.44 [95% CI 3.62–24.63], ORadj 5.44 [95% CI 1.57–18.82] for the right and left sides, respectively). The power Doppler signal was grade ≥2 in only 1 first MTP joint. Asymptomatic MSU deposition in first MTP joints Present (n = 49) Absent (n = 213) First MTP joints Double contour sign 13 (5.0) – – Tophi 27 (10.3) – – Double contour sign and tophi 9 (3.4) – – Grade ≥2 effusion 56 (21.4) 26 30 Patellar tendon Hyperechoic deposits 19 (7.3) 11 8 Unilateral 13 7 6 Bilateral 3 2 1 Triceps tendon Hyperechoic deposits 15 (5.7) 8 7 Unilateral 13 6 7 Bilateral 1 1 0 a One participant had a double contour sign at 1 ankle; triangular fibrocartilage involvement was not observed in any participant. Values are the number (%) of joints/tendons. MSU = monosodium urate monohydrate; MTP = metatarsophalangeal. Hyperechoic aggregates were present in at least 1 tendon in 28 participants (21.4%). Sixteen participants (12.2%) had patellar tendon involvement, and 14 (10.7%) had triceps tendon involvement. Of the 28 participants with hyperechoic aggregates in at least 1 tendon, 14 had asymptomatic MSU crystal deposition at 1 or both first MTP joints. The presence of MSU crystal deposition at either first MTP joint was associated with the presence of hyperechoic aggregates in at least 1 tendon (OR 3.12 [95% CI 1.31–7.42]). This association was statistically significant after adjustment for covariates (ORadj 2.96 [95% CI 1.17–7.49]). Subjects with asymptomatic MSU crystal deposition had higher serum urate levels than those without (mean difference 0.54 mg/dl [95% CI 0.12–0.96]). The prevalence of asymptomatic MSU crystal deposition at either first MTP joint increased from 0% to 24.2%, 39.1%, 29.6%, 44.4%, and 50%, respectively, in participants with serum urate levels of <5, 5–5.99, 6–6.99, 7–7.99, 8–8.99, and ≥9 mg/dl (Table 1). Other disease, demographic, and laboratory parameters were comparable between the 2 groups (Table 1). MSU crystal deposition was associated with increasing serum urate level (OR 1.50 [95% CI 1.06–2.11], ORadj 1.61 [95% CI 1.10–2.36] for each 1‐mg/dl increase in serum urate). However, there was no association between MSU crystal deposition and uric acid underexcretion status (FEUA ≤6.6%) (OR 0.71 [95% CI 0.29–1.71], ORadj 0.78 [95% CI 0.31–1.98]). Among the 117 participants with serum urate levels of ≥5 mg/dl (the cutoff value above which MSU crystal deposits were found in this study), the prevalence of asymptomatic MSU crystal deposition was 33.33%, and this increased numerically from ages in the 20s to the 40s before stabilizing (see Supplementary Table 1, on the Arthritis & Rheumatology web site at http://onlinelibrary.wiley.com/doi/10.1002/art.40572/abstract). However, the increase was not statistically significant, and participants age >40 years were not significantly more likely to have asymptomatic MSU crystal deposition than those ≤40 years of age (OR 1.32 [95% CI 0.59–2.95], ORadj 1.69 [95% CI 0.34–8.47]). There was no association between hyperuricemia and tendon hyperechoic deposits, and, in those with serum urate levels ≥5 mg/dl, there was no association between increasing age and tendon hyperechoic deposits (Supplementary Tables 2 and 3, on the Arthritis & Rheumatology web site at http://onlinelibrary.wiley.com/doi/10.1002/art.40572/abstract). Self‐reported data on age at onset of gout were available for 60 parents. The median age at onset was 53 years. On univariate analysis, there was no association between parental gout onset at or before 53 years of age and asymptomatic MSU crystal deposition (with parental gout onset after the age of 53 years as the referent) (OR 2.64 [95% CI 0.79–8.87]). However, this approached significance after adjustment for covariates (ORadj 4.14 [95% CI 0.88–19.46], P = 0.07). Discussion This study demonstrates that the sons of patients with gout have a higher prevalence of hyperuricemia 11, uric acid underexcretion 8, and asymptomatic MSU crystal deposition than observed in previous studies in which participants were preselected according to their serum urate level 4-6. The results also raise the possibility that MSU crystal deposition occurs initially in the first MTP joints and in tendons before appearing in other joints such as the ankle and the knee. However, this observation is limited by the cross‐sectional study design. It was surprising that 1 in 5 subjects with serum urate levels between 5 and 6 mg/dl had ultrasonographic features of MSU crystal deposition at the first MTP joints. This observation must be interpreted with caution as it is based on a single serum urate measurement, and it is possible that serum urate levels in these participants were higher at a previous time. However, it raises the possibility that the threshold for MSU crystal deposition in vivo may be lower than that estimated from laboratory studies. This may be due to the fact that the saturation point of urate reduces from 6.75 mg/dl at 37°C to between 4.5 and 6 mg/dl at 30–35°C, the mean temperature of the human big toe in temperate climates 12, 13. While MSU crystals were present in subjects with serum urate levels of 5–6 mg/dl, we did not find ultrasonographic evidence of MSU crystal deposition in those with levels below 5 mg/dl. This raises the possibility that the target serum urate level for treat‐to‐target urate‐lowering therapy should be <5 mg/dl, at least in individuals who continue to have gout flares despite serum urate levels between 5 and 6 mg/dl. However, further prospective studies are needed before such a strategy can be recommended. A lower‐than‐expected serum urate level in sons of patients with gout might also be explained in part by inherited tissue factors (either an increase in promoters or decrease in inhibitors) that enhance MSU crystal deposition at relatively low serum urate levels. The present findings suggest that MSU crystal deposition begins early (in the third decade of life) and becomes more prevalent with increasing age. The reduction in prevalence of MSU crystal deposition in subjects older than 60 years could be due to the sampling for this study, as people older than 60 years with MSU crystal deposits are likely to have developed gout flares, which would have excluded them from the study population. We observed intratendinous hyperechoic deposits in 35.9% of participants with MSU crystal deposits elsewhere. This is consistent with previous reports of tendon involvement in gout 14, 15. As shown in Table 2, a substantial proportion of tendon hyperechoic deposits occurred in subjects without ultrasonographic features of MSU crystal deposition in the first MTP joints. Further research, e.g., using dual‐energy computed tomography, is therefore needed to confirm the composition of these tendinous deposits before their presence can be used to imply MSU crystal deposition in the absence of a double contour sign or intraarticular tophi in other joints. Our results indicate that ultrasonographic evaluation of both first MTP joints is sufficient to identify all individuals with MSU crystal deposition. Thus, men at a high risk of gout (e.g., those with a positive family history) could undergo serum urate measurement and ultrasonography of both first MTP joints to screen for MSU crystal deposition. While ultrasonographic examination of multiple peripheral joints is time consuming, assessment of both first MTP joints takes 10–15 minutes and may make it possible for asymptomatic MSU crystal deposits to be diagnosed, in turn allowing consideration of lifestyle changes to prevent development of symptomatic gout and associated consequences. Initiation of prophylactic pharmacologic urate‐lowering treatment at this early stage would be considered controversial given the absence of symptoms and the possibility that in many people with asymptomatic MSU crystal deposition, gout flares would not develop. Such a screening strategy would require ultrasonography of 3 individuals with a serum urate level of ≥5 mg/dl to detect 1 person with asymptomatic MSU crystal deposition. However, in the absence of prospective studies evaluating the relationship between asymptomatic MSU crystal deposition and symptomatic gout, the benefit from such a strategy remains unproven. Our data also suggest that parents with younger‐onset gout are more likely to pass on the trait to their sons, although this association was not statistically significant and requires further investigation in a study with a larger sample size. There are several caveats to this study. First, the response rate was low, and it is possible that patients with severe, troublesome gout were more likely to pass on the study packets to their sons, or that sons with lifestyle risk factors were more likely to agree to participate. This raises the possibility of selection and response bias. However, the mean ± SD age at gout onset in parents of sons who participated and for whom data on the age at gout onset were available (n = 60) was 52 ± 13.65 years, and they reported a mean ± SD of 1.33 ± 2.10 gout flares in the 12‐month period preceding their original research visit. These parents also had a low comorbidity burden, with a median of 1 cardiovascular or renal comorbidity (interquartile range 1–2). Second, we did not perform joint aspiration to confirm the validity of our findings. However, in subjects with hyperuricemia, ultrasonographic changes have 100% sensitivity and 88% specificity for MSU crystal deposition, compared to joint aspiration 5. Finally, we measured serum urate only on a single occasion. In conclusion, the results of this study demonstrate that asymptomatic sons of patients with gout frequently have hyperuricemia and uric acid underexcretion, and have a high prevalence of MSU crystal deposition. This suggests that screening of such individuals and discussion of early management, involving addressing modifiable risk factors (overweight, obesity, high fructose intake, etc.) in order to reduce their risk of developing symptomatic gout, should be considered. Acknowledgments The authors would like to acknowledge the study participants and their parents. Author Contributions All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Abhishek had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design Abhishek, Courtney, Jones, Zhang, Doherty. Acquisition of data Abhishek, Courtney, Jenkins. Analysis and interpretation of data Abhishek, Sandoval‐Plata. Supporting Information References Notes : Drs. Abhishek and Doherty's work was supported by an investigator‐initiated departmental research grant from AstraZeneca and Ironwood Pharmaceuticals. Ms Sandoval‐Plata's work was supported by a PhD scholarship from Consejo Nacional de Ciencia y Tecnología, Mexico. Dr. Abhishek has received speaking fees from Menarini (less than $10,000) and research grants from AstraZeneca and Oxford Immunotec. Dr. Zhang has received speaking fees and/or honoraria from AstraZeneca, Grünenthal, Bioiberica, and Hisun (less than $10,000 each). Dr. Doherty has received consulting fees and/or honoraria from AstraZeneca, Grünenthal, Mallinkrodt, and Roche (less than $10,000 each) and research grants from AstraZeneca and Oxford Immunotec. 3 All participants with asymptomatic monosodium urate monohydrate (MSU) crystal deposition had first metatarsophalangeal joint involvement. IQR = interquartile range; eGFR = estimated glomerular filtration rate; FEUA = fractional excretion of uric acid. 4 Eleven participants were prescribed antihypertensive drugs; 1 received bendroflumethiazide. 5 Six participants were prescribed statins. 6 Both participants were prescribed oral hypoglycemic drugs. 7 P = 0.01 versus participants without asymptomatic MSU crystal deposition. 8 One participant had a double contour sign at 1 ankle; triangular fibrocartilage involvement was not observed in any participant. Values are the number (%) of joints/tendons. MSU = monosodium urate monohydrate; MTP = metatarsophalangeal. Citing Literature Number of times cited: 1 Xiao Chen, Zhongqiu Wang, Na Duan, Wenjing Cui, Xiaoqiang Ding and Taiyi Jin, The benchmark dose estimation of reference levels of serum urate for gout, Clinical Rheumatology, 10.1007/s10067-018-4273-1, (2018). Crossref
NORTH CHICAGO, Ill., Oct. 23, 2018 /PRNewswire/ -- AbbVie (NYSE: ABBV), a research-based global biopharmaceutical company, today announced new patient-reported outcomes data from the ongoing Phase 3 SELECT-MONOTHERAPY trial evaluating upadacitinib (15 mg and 30 mg, once-daily), an investigational JAK1-selective inhibitor, as a monotherapy treatment in patients with moderate to severe rheumatoid arthritis who did not adequately respond to treatment with methotrexate.1 Improvements in physical function, health-related quality of life, pain and morning joint stiffness were reported after 14 weeks of treatment with upadacitinib monotherapy compared to patients continuing methotrexate.1 These results will be presented at the 2018 American College of Rheumatology (ACR)/Association for Rheumatology Health Professionals (ARHP) Annual Meeting in Chicago. AbbVie has previously announced positive top-line results from SELECT-MONOTHERAPY. "Upadacitinib as a monotherapy showed significant improvements in rheumatoid arthritis patients' ability to perform daily activities and overall health-related quality of life," said Marek Honczarenko, M.D., Ph.D., vice president, global immunology development, AbbVie. "These results show that the improvements in clinical symptoms are accompanied by improvement in outcomes important to patients. These results reinforce upadacitinib's therapeutic potential across diverse rheumatoid arthritis patient populations and its use as a monotherapy treatment option." Patient-reported outcome results from SELECT-MONOTHERAPY are as follows: Physical Function1 Improvements in physical function, as measured by the Health Assessment Questionnaire-Disability Index (HAQ-DI), were observed as early as two weeks after initial treatment with upadacitinib across both doses compared to eight weeks for patients receiving methotrexate. At week 14, 65/69 percent of patients receiving 15/30 mg of upadacitinib reported improvements in physical function (HAQ-DI) compared with 45 percent of patients receiving methotrexate (p<0.001). Health-related Quality of Life1 At week 14, 65/73 percent of patients receiving 15/30 mg of upadacitinib reported improvements in health-related quality of life (physical component score of Short Form 36 Health Survey) compared with 48 percent of patients receiving methotrexate (p<0.001). Joint Pain1 Patients reported reductions in pain, as measured by the Patient's Assessment of Pain (based on Visual Analog Scale [VAS]), as early as two weeks after initial treatment with both doses of upadacitinib compared to four weeks for patients receiving methotrexate. At week 14, 64/75 percent of patients receiving 15/30 mg of upadacitinib reported a reduction in pain compared with 46 percent of patients receiving methotrexate (p<0.001). Morning Stiffness1 Patients receiving upadacitinib reported reductions in the severity of morning stiffness as early as two weeks after initial treatment with both doses of upadacitinib compared to four weeks for patients receiving methotrexate. At week 14, 74/83 percent of patients receiving 15/30 mg of upadacitinib reported reductions in the severity of morning joint stiffness compared to 57 percent of patients receiving methotrexate (p<0.001). Additionally, patients treated with both 15/30 mg of upadacitinib had a mean reduction of 95/102 minutes in the duration of morning stiffness compared to 53 minutes with methotrexate (p<0.05) at week 14. "Upadacitinib significantly improved physical function, joint pain and morning stiffness in addition to health-related quality of life as an oral, monotherapy treatment in this trial," said Vibeke Strand, M.D., adjunct clinical professor in the Division of Immunology/Rheumatology at Stanford University and lead investigator in the studies. "These results are especially important because many patients cannot tolerate or do not respond to treatment with methotrexate and additional effective monotherapy options are needed for these patients." Results from a separate, exploratory analysis evaluating the association between patient-reported outcomes and clinical outcomes will be presented at ACR and show that achieving substantial improvements in pain, physical function and fatigue were associated both with individual physician-derived measures and with composite disease outcomes such as ACR20/50/70, clinical remission and low disease activity.10 The analysis demonstrated how the use of patient-reported outcomes in clinical trials provides critical insight into the impact of rheumatoid arthritis on patients.10 The analysis included a diverse patient population with difficult-to-treat disease, refractory to biologics and conventional synthetic DMARDs, such as methotrexate, who were enrolled in the Phase 3 SELECT-NEXT, SELECT-BEYOND (both studies with background csDMARDs) and SELECT-MONOTHERAPY clinical trials.10 Rheumatoid arthritis, which affects an estimated 23.7 million people worldwide, is a chronic and debilitating disease.11 Many patients do not respond to or cannot tolerate methotrexate, a commonly used first-line therapy.12-14 Increasingly, patient-reported outcomes are being included in randomized clinical trials in order to understand how rheumatoid arthritis patients perceive the physical, psychological and social impact of their disease.15 Using patient-reported outcomes data to assess the impact of disease provides valuable insights to healthcare providers.15 Safety results from SELECT-MONOTHERAPY have been previously reported here. About SELECT-MONOTHERAPY4 SELECT-MONOTHERAPY is a Phase 3, multicenter, randomized, double-blind, parallel-group study designed to evaluate the safety and efficacy of upadacitinib monotherapy in adult patients with moderate to severe rheumatoid arthritis and an inadequate response to a stable dose of methotrexate. Patients were randomized to switch from methotrexate to upadacitinib monotherapy (15 mg or 30 mg once-daily) or continue on their prior stable dose of methotrexate in a blinded manner. The primary endpoints of the first phase included the percentage of subjects achieving an ACR20 response and low disease activity (LDA) after 14 weeks of treatment. Secondary endpoints included proportion of patients achieving ACR50, ACR70 and clinical remission at week 14, HAQ-DI, duration of morning (AM) stiffness and health-related quality of life (QoL) by SF-36. The trial is ongoing and the second phase is a blinded long-term extension period to evaluate the long-term safety, tolerability, and efficacy of the two once-daily doses (15 mg and 30 mg) of upadacitinib monotherapy in patients who have completed the first phase. More information on this trial can be found at www.clinicaltrials.gov (NCT02706951).
Via Krishan Maggon

|
Suggested by
Société Francaise d'Immunologie
September 22, 2018 2:19 PM
|
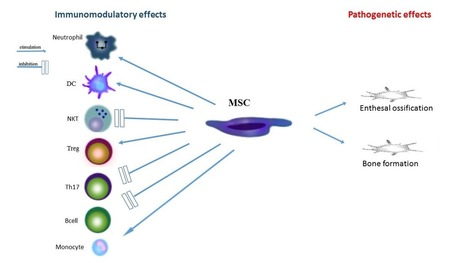
Abstract It is now well accepted that an imbalance between the Th17 and regulatory T‐cell responses is closely associated with the development of rheumatoid arthritis (RA). However, the precise regulatory mechanism for the differentiation of Th17 and Treg in RA is not well characterized. The present study showed that metallothionein‐1 (MT‐1), which is a low molecular weight protein that is involved in the detoxification of heavy metals and scavenging of free radicals, was upregulated in RA. Furthermore, the synovial inflammation and pathologic symptoms in collagen‐induced arthritis and collagen antibody‐induced arthritis mice were significantly suppressed when MT‐1 was expressed intraarticularly. Further investigation revealed that MT‐1 inhibited the differentiation of Th17 cells but enhanced that of Treg cells. Furthermore, it markedly decreased both STAT3 and RAR‐related orphan receptor gamma t (RORγt) expression in vitro and in vivo. Collectively, our studies demonstrated that MT‐1 might manifest as a protein involved in immunosuppression of RA pathogenesis by shifting Th17/Treg balance and may prove to be a potential therapeutic target for RA autoimmune diseases. Introduction Rheumatoid arthritis (RA) is a systemic inflammatory autoimmune disease of unknown etiology that is characterized by a wide clinical spectrum including chronic synovial inflammation and joint destruction as well as physical disability 1, 2. Evidence has suggested that IL‐17 is a major proinflammatory cytokine that is responsible for cartilage and bone destruction 3-6, which suggests that IL‐17‐ producing Th17 cells exert predominate effects on the RA pathogenic progress 7, 8. Although the detailed molecular mechanism for the Th17 differentiation is not fully understood, it is clear that cytokines including TGF‐β and IL‐6 are required to induce the differentiation of naïve CD4+ Th cells toward the phenotype of Th17 lineage in mice 9. It has become increasingly clear in the previous studies that transcription factors including STAT3 and RAR‐related orphan receptor gamma t (RORγt) also play fundamental roles in Th17 cell development 10-14. More importantly, cytokines such as IFN‐γ, IL‐4, IL‐21, and IL‐27 are associated with Th17 cell differentiation by their regulation of STAT3, RORγt, and RORα 3, 15-18. In contrast, activation of naive CD4+ Th cells in the presence of TGF‐β leads to the development of Treg cells that express the transcriptional regulator Foxp3 and exhibit a suppressive phenotype in RA development 9, 19-21. Of note, Th17 and Treg cells can be interconverted by reciprocal regulation: specifically, Foxp3 can antagonize the DNA‐binding ability of RORγt, whereas RORγt can repress Foxp3 expression 22-24. Therefore, challenges and opportunities coexist in the exploration of the mechanisms that contribute to Th17/Treg balance in homeostasis and RA therapy. Metallothioneins (MTs) are low molecular weight (<10KD) cysteine‐rich proteins that play key roles in the regulation of metal homeostasis and protection against heavy metal toxicity as well as oxidative stress under physiological conditions 25. It has been documented that MTs are released into the extracellular environment under some stress conditions. The mechanisms for this release are unknown because MT‐1 does not possess the hydrophobic signal sequences that are necessary for normal excretion of proteins 26-28. The accumulated evidence suggests that extracellular MTs participate in the regulation of immune responses including suppressing humoral immunity 29, interacting with the plasma membranes of lymphocytes and macrophages 30, 31 and impairing the functions of cytotoxic T lymphocytes 32. Additionally, MTs can function as a chemoattractants that induce movement of leukocytes 33 and as immune regulators that induce the expansion of regulatory T cells 34, 35. It has been reported that collagen‐induced arthritis (CIA) mice exhibit reduced clinical manifestations when MT‐1/2 proteins were repeatedly administered 36. Furthermore, Huh et al. reported that MT may play an important role in the regulation of Th1‐dependent autoimmune arthritis with research in MT‐1/2‐deficient and transgenic mice 34, but the effects of MT‐1 alone on RA development, especially with respect to the RA pathogenic and immune regulatory mechanisms, have not yet been elucidated. Results MT‐1 is upregulated in RA To investigate the potential role of MT‐1 in RA pathogenesis, we first compared the levels of MT‐1 in PBMCs and plasma from 53 RA patients with those of 40 healthy controls (HCs). As shown in Fig. 1A and B, the MT‐1 mRNA and protein levels were markedly higher in the samples from patients with RA than in those from the HCs. Furthermore, we confirmed these results in CIA mouse models. As expected, the MT‐1 mRNA levels in the spleens, LNs, and synovia of CIA mice were significantly higher than those from control mice (Fig. 1C–E). Compared to the control mice, the CIA mice had higher MT‐1 concentrations in the synovial fluid (Fig. 1F). To further investigate the cellular sources of MT‐1 among the PBMCs of RA patients, the expression levels of MT‐1 in T and B cells from RA patients and HCs were analyzed. Our data suggested that the expression of MT‐1 mRNA was significantly higher in the CD3+ and CD4+ T cells from the RA patients compared with the HCs (Fig. 1G and H), whereas no differences between the RA patients and HCs were observed in the CD8+ T cells or CD19+ B cells (Fig. 1I and J). Collectively, these data indicated that MT‐1 is upregulated in the RA and CIA samples and is closely associated with RA disease. Locally increased MT‐1 suppresses arthritis development CIA shares many similarities with human RA and is the gold standard in vivo model for RA studies with respect to two of its characteristics: breach of tolerance and generation of autoantibodies toward self and collagen. To explore the potential functions of MT‐1 during CIA, we induced a local elevation of MT‐1 expression by injecting adenovirus that expresses MT‐1 (Ad‐MT‐1) or empty adenovirus (Ad‐Vec) intraarticularly in CII‐immunized mice (Fig. 2A). First, we determined the level of MT‐1 expression after adenovirus injection at steady state and during CIA. As shown in Supporting Information Fig. 1, the CIA mice expressed higher levels of MT‐1 in the synovia, spleens, and LNs. However, we found that Ad–MT‐1 strongly expressed MT‐1 only in synovium of the mice (Supporting Information Fig. 1A). Compared with the Ad–Vec‐injected mice, the Ad–MT‐1‐injected mice demonstrated lower levels of MT‐1 expression in the spleen and LNs during CIA (Supporting Information Fig. 1B and C). Notably, the onset of CIA was delayed and the incidence of CIA was lower in the Ad‐MT‐1‐injected mice compared to the Ad‐Vec‐injected mice (Fig. 2B). In addition, Ad‐MT‐1 administration clearly alleviated the symptoms of arthritis as assessed by the clinical score and footpad thickness in mice with CIA (Fig. 2C and D), and these effects were accompanied by smaller popliteal LNs and spleens (Fig. 2E and F). Consistent with these results, histopathologic examination of the knee joints revealed that the increased expression of MT‐1 induced by intraarticular injection of Ad‐MT‐1 significantly reduced the synovial hyperplasia, cartilage damage and bone erosion (Fig. 2G and H). To evaluate whether the humoral immune response against CII was modulated by the Ad–MT‐1 treatment, the sera and synovial fluid from Ad–MT‐1–treated and Ad‐Vec–treated mice were analyzed for the presence of CII‐specific IgG1 and IgG2a Abs. Interestingly, no obvious differences in the levels of serum and synovial fluid CII‐specific IgG1 Abs were observed between these two groups (Fig. 2I). In contrast, the synovial fluid levels of CII‐specific IgG2a Abs were dramatically lower in the Ad‐MT‐1‐injected mice compared with the Ad‐Vec‐injected mice, whereas the serum CII specific IgG2a Ab levels were not affected (Fig. 2J). Taken together, these results clearly indicate that locally increased MT‐1 directly contributes to the suppression of CIA development and alleviation of articular pathology. Next, we assessed the role of Ad‐MT‐1 in the collagen antibody‐induced arthritis (CAIA) model, which is induced by administration of the monoclonal anti‐type II collagen antibody cocktail (Fig. 4A). Consistently, Ad‐MT‐1 administration resulted in significantly reduction of incidence and alleviation of clinical score and footpad thickness (Fig. 4B–D). MT‐1 inhibits expression of RA‐relevant cytokines To gain insight into whether MT‐1 directly affects the inflammatory cytokine production during RA pathogenesis, PBMCs from RA patients and HCs were purified and cultured in the presence or absence of 20 μM recombinant MT‐1 protein. The expression of proinflammatory cytokines including IL‐1β, IL‐6, and TNF‐α, which are prominent mediators in the pathogenesis of RA, was significantly suppressed in the PBMCs from the RA patients after treatment with recombinant MT‐1, whereas this phenomenon was not observed in the PBMCs from the HCs (Supporting Information Fig. 2A–C). In an attempt to further confirm the antiarthritic inflammatory response of MT‐1 in vivo, cytokines were analyzed in the synovium and synovial fluid from the CIA mice. The results of the RT‐qPCR and ELISA evaluations of the CIA mice were consistent with the data for the PBMCs from the RA patients (Fig. 3A–H). More importantly, our experiments indicated that expression of MT‐1 in the knee joints also dramatically reduced the levels of the IL‐17A and IFN‐γ proteins (Fig. 3G and H), which are pivotal mediators for the development and progression of the inflammation that is associated with CIA. Consistently, these phenomena were also observed in CAIA mice (Fig. 4E–L). In summary, all of the results together demonstrated that MT‐1 suppresses RA pathogenesis at least in part by inhibiting the proinflammatory cytokine expression to attenuate immunoresponse during RA. MT‐1 modulates Th17 and Treg cell differentiation in vitro Considering that Th17 cells are major players in inflammation and the development of the pathogenesis of RA and that Treg cells are crucial to maintaining the immune homeostasis in the body, flow cytometry was used to analyze the effect of MT‐1 on the differentiation of Th17 and Treg cells. The gating strategy was shown in Supporting Information Fig. 4. Of interest, compared to controls, a significantly lower percentage of IL‐17A‐producing cells were observed in the CD4+ T cells that had been treated with recombinant MT‐1 protein under Th17‐skewing cell culture conditions (Fig. 5A and B). Moreover, the mRNA levels of Th17‐related genes such as IL‐17A and IL‐17F were also markedly decreased in the MT‐1‐treated cells (Fig. 5E and F). In striking contrast to our findings with respect to Th17, the proportion of Foxp3+ cells was dramatically increased in the MT‐1‐treated naïve CD4+ T cells under Th17‐skewing conditions (Fig. 5C and D). In addition to the expression of FOXP3 protein, the mRNA levels of Treg‐related genes including Foxp3 and IL‐10 were also higher in the MT‐1‐treated cells than that in the non‐MT‐1‐treated cells (Fig. 5G and H). To further elucidate whether MT‐1 could regulate Th17 cytokine expression in PBMCs, PBMCs from HCs and RA were collected and cultured in the presence or absence of MT‐1. As shown in Supporting Information Fig. 3, MT‐1 treatment markedly inhibited the expression of Il‐17A, IL‐17F, IL‐22, IL‐21, and IL‐23 in the PBMCs from the RA subjects but failed to regulate the expression of these genes in the PBMCs from the HCs. Notably, we could not find any significant differences in the T‐cell proliferation or apoptosis in the CD4+ T cells cultured in the presence or absence of 20 μM recombinant MT‐1 protein under Th17‐skewing conditions (Fig. 5I and J). Collectively, these findings demonstrate that MT‐1 directly modulated the differentiation program of Th17 and Treg cells in vitro without influencing T‐cell proliferation or apoptosis. MT‐1 regulates Th17 and Treg balance during arthritis To more precisely understand how MT‐1 inhibits arthritis pathogenesis in vivo, we sought to examine the effects of MT‐1 on the generation of the Th17 and Treg subsets in mice. Compared with the Ad‐Vec‐treated CIA mice, intracellular cytokine staining showed a significantly reduced frequency of IL‐17A‐producing Th17 cells in the spleens of the Ad‐MT‐1‐treated mice (Fig. 6A and B). Consistently, we also observed decreased levels of the Th17 signature cytokines in the synovia of the Ad‐MT‐1‐treated mice (Fig. 6E and F). However, the frequency of Foxp3‐producing Treg cells in the spleens and Treg signature cytokine levels in synovia were markedly greater in the Ad‐MT‐1‐treated mice than in the Ad‐Vec‐treated mice (Fig. 6C, D, G, and H). Furthermore, these observations could also be recapitulated in CAIA mice. Local increase of MT‐1 expression by injecting Ad‐MT‐1 resulted in reduction of Th17 cells but elevation of Treg cells in the spleens (Fig. 7A–D), as well as the production of their signature cytokines (Fig. 7E–H). These results were consistent with those obtained from the in vitro differentiation experiment, which indicated that MT‐1 inhibits RA pathogenesis by shifting the differentiation of CD4+ T cells toward Treg cells. MT‐1 inhibits STAT3 signaling pathway Th17 cell differentiation is known to be determined by transcription factor RORγt, which is induced by STAT3 activation. As shown in Fig. 8A and B, MT‐1 treatment downregulated the STAT3 phosphorylation level in CD4+ T cells under Th17‐skewing conditions. Consistently, RORγt was markedly reduced in the MT‐1‐treated cells compared with the control cells (Fig. 8E). Additionally, we also detected a reduction in the levels of STAT3 phosphorylation and RORγt expression in the synovial tissues of the Ad‐MT‐1‐treated mice compared to those of the Ad‐Vec‐treated mice (Fig. 8C, D, and F). Collectively, these results indicated that MT‐1 modulates the differentiations of Th17 and Treg cells toward Treg during RA, most likely by suppressing the activation of the STAT3 signaling pathway. Discussion Rheumatoid arthritis is a crippling disease. It is a leading cause of disability throughout the world, but the inflammatory response mechanisms that underlie the RA disease process are still poorly understood. As a consequence, current therapeutic options are nonspecific, and most of the drugs are highly toxic. In this study, we identified a small protein, MT‐1, that function as an immune suppressor in the development of RA, and further demonstrated that its immunoregulatory mechanism in the pathogenesis of RA involves modulation of the Th17/Treg balance. Specifically, MT‐1 suppressed Th17 but promoted Treg differentiation by downregulating STAT3 activation and RORγt expression. This indicates a negative feedforward mechanism for MT‐1 in RA immunoregulation. In this mechanism, RA inflammation upregulates MT‐1 expression; MT‐1 in turn shifts the balance of Th17/Treg, thereby inhibiting the RA immune inflammation. In general, the MTs are considered to be a family of metalloregulatory and antioxidant proteins 25. There are four MT isoforms in mice: MT‐1, MT‐2, MT‐3, and MT‐4 37. It has been demonstrated that MT‐1 and MT‐2 are inducible under stressful conditions 38-40. In addition, studies using MT‐1/2 knockout mice have indicated that the MTs affect the immune system under pathophysiological conditions such as acute lung injury, immunoglobulin production, NF‐ΚB activity, and asthma 41-44. It was found in our study that the MT‐1 mRNA and protein levels were significantly elevated in RA patients and in arthritis mice. More interestingly, recombinant MT‐1 protein could effectively inhibit the production of RA‐related proinflammatory cytokines such as TNFα, IL‐1β, and IL‐6 in the PBMCs from the RA patients but not in those from the HCs. These data indicated that MT‐1 plays an important role as a ligand that suppresses the inflammatory response in RA. In the in vivo study, adenoviral‐mediated expression of MT‐1 in mouse knees reduced the incidence of CIA or CAIA, the clinical scores and the bone erosion, as well as the arthritis‐related proinflammatory cytokines, which further demonstrated that MT‐1 had an immunoregulatory function on the inflammatory reaction in RA. Hence, our results suggested that proinflammatory cytokines not only enhance the pathogenic process of RA but also induce expression of the suppressive factor MT‐1, which in turn downregulates the excessive inflammatory response during RA. Recent data from several murine models have suggested that an appropriate balance between Th17 and Treg cells is critical to minimizing the development of RA autoimmune disease 21. In general, Th17 cells are the predominant initiators of the RA‐associated inflammation. These cells release the proinflammatory cytokine IL‐17, which is a key effector in the progressive destruction of bone and cartilage in the joints 45, 46. In contrast, Treg cells demonstrate the opposite effects on autoimmunity and inflammation and play a role in maintaining peripheral immune tolerance and immune homeostasis 47, 48. The identification of IL‐17‐producing FOXP3+ Treg cells suggests a relationship between the ontogeny of the Th17 and Treg lineages. Therefore, to understand the immune regulatory mechanisms of RA, studies to identify new factors that are involved in the balance of Th17/Treg regulation are of great importance, and the subject is worthy of further intensive research. Considering their ability to reduce the T‐cell responses and induce regulatory T cells or T‐cell anergy, tolerogenic DCs are considered to be an immunotherapeutic target in autoimmune diseases such as rheumatoid arthritis 49. It is clear that DCs that have been treated with carvacrol plus thermal stress produce high levels of MT‐1 mRNA and have the phenotype of tolerogenic cells that suppress arthritis 50. Furthermore, the membrane‐bound MT‐1 of tolerogenic DCs induced a FoxP3+ phenotype in antigen‐specific CD4+ T cells and promoted the expansion of these regulatory T cells 35. Thus, these data suggested that MT‐1 could induce the production of regulatory T cells from CD4+ T cells. In the present study, we examined whether the immune regulatory mechanism by which MT‐1 affects RA involved the control of the differentiation of Th17 and Treg cells. A detailed analysis of the Th17 and Treg cells at various levels including the cell frequencies and production of the related cytokines was conducted. Our in vivo data showed that in the arthritis mice that were treated with Ad‐MT‐1, the frequency of the Th17 cells decreased but the Treg cells frequency increased compared with mice treated with Ad‐Vec. Consistent with these observations, the in vitro data showed that recombinant MT‐1 suppressed the Th17 cells but enhanced the Treg cells differentiation under Th17‐skewing conditions. We therefore hypothesized that one possible mechanism by which MT‐1 alleviates inflammatory response in RA might be through restoring the Th17/Treg balance. Another important aspect of the present study was the investigation of the underlying regulatory molecular mechanism by which MT‐1 affected the Th17 differentiation. It is well established that TGF‐β and IL‐6 are critical factors for the generation of Th17 cells. They act in a STAT3‐dependent manner to induce the expression of the transcription factor RORγt, which subsequently induces the production of a set of effector molecules including IL‐17A, IL‐17F, and IL‐23 12, 51, 52. The results described herein showed that MT‐1 inhibited the phosphorylation of STAT3 not only in synovium of the CIA mice but also in CD4+ T cells under Th17‐skewing conditions. The mechanism by which MT‐1 suppresses STAT3 activation and whether it is also involved in other regulatory mechanisms that contribute the balance of Th17/Treg in the RA immunoresponse remain to be defined. Based on our findings, it is conceivable that MT‐1 may inhibit RA inflammatory process in additional ways beyond shifting the balance of the differentiation of Th17 and Treg cells. Indeed, our data demonstrated that MT‐1 decreased the production of key proinflammatory cytokines related to the RA inflammatory response including IL‐1β, IL‐6, and TNFα. These results are consistent with previous studies in which repeated administration of MT‐1/2 suppressed CIA via the induction of TGF‐β and the downregulation of the proinflammatory mediators TNF‐α and Cox‐2 36. These data imply that MT‐1 may have a more complex mechanism in the regulation of autoimmune inflammation during RA process. Further research needs to be conducted to study the immunoregulatory mechanism of MT‐1 in RA. In summary, our present study demonstrated suppressive effects of MT‐1 in the progression of RA, characterized a negative feedforward mechanism in which MT‐1 modulated the Th17/Treg balance, and showed that the underlying molecular mechanism for the regulation of the Th17/Treg balance in RA involved the inhibition of the activation of the STAT3 signaling pathway. Taken together, our findings showed that MT‐1 may have a certain ability to restore immune homeostasis during the RA inflammatory process and suggested that this low molecular weight protein may be a potential therapeutic candidate for the treatment of RA and other autoimmune diseases. Materials and methods Subjects We recruited 53 patients with RA from the Peking University Shenzhen Hospital for the present study. The clinical characteristics of the RA subjects are summarized in Supporting Information Table 1. The classification of RA fulfilled the 1987 American College of Rheumatology criteria. At the time of sample acquisition, 40 of the 53 patients were being treated with 10–15 mg day−1 prednisone, and no patients were naïve for DMARDs. An additional set of 40 age‐ and sex‐matched healthy individuals served as the HCs. The protocols for the study were approved by the Review Board for Peking University Shenzhen Hospital. Informed written consent was obtained from the recruited subjects. Arthritis induction and Ad‐MT‐1 treatment DBA/1J and Balb/c mice were purchased from The Jackson Laboratory and maintained in a laminar airflow cabinet under specific pathogen‐free conditions according to the NIH standards established in the Guide for the Care and Use of Laboratory Animals. All of the protocols were approved by Shenzhen University. CIA induction was performed as previously described 53. Briefly, male DBA/1J mice were immunized with 100 μg of CII emulsified with an equal volume of complete Freund's adjuvant (Difco). A booster injection of CII emulsified with incomplete Freund's adjuvant (Difco) was administered 21 days later. 108 pfu Ad‐Vec or Ad‐ MT‐1 was injected intraarticularly into the knee joints on days 15, 20, and 25 after the first immunization. The mice were sacrificed on day 32 or later for the experimental analyses. To induce CAIA, the monoclonal antibody cocktail (1.5mg/mouse, Chondrex, Inc.) was injected intraperitoneally. Three days later, 50 μg LPS was injected intraperitoneally. The experiment was ended 9 days after antibody administration. Ad‐Vec or Ad‐MT‐1 was injected intraarticularly into the knee joints on day –3 before the first immunization and on day 2 after the first immunization. The signs of arthritis were monitored daily as previously described 54, and the disease severity was scored in each paw on a scale of 0–3 for a maximum score of 12 per mouse. Histological examination The mice were killed on day 32, and the knee joints were fixed, decalcified, and paraffin‐embedded. Tissue sections (5 μm) were prepared and stained with hematoxylin and eosin. The clinical evaluation of joint damage was graded from 0 to 3 as previously described 54. T‐cell differentiation Spleen CD4+ T cells were isolated by negative selection using the CD4+ T Cell Isolation Kit (Miltenyi Biotec) according to the manufacturer's instructions. The purified cells were cultured in 24‐well plates that were precoated with anti‐CD3 (1 μg mL−1) and anti‐CD28 (1 μg mL−1). The culture medium contained 5 ng mL−1 TGF‐β, 20 ng/mL IL‐6, and 20 ng mL−1 IL‐23 in the presence or absence of 20 μM recombinant MT‐1 protein. The cells were collected for further analysis after 72 h of culture. Flow cytometric analysis Single‐cell splenocyte suspensions were prepared, and the purified CD4+ T cells were cultured under Th17‐skewing conditions for 3 days, then stimulated with PMA (100 ng mL−1; Sigma‐Aldrich) and ionomycin (500 ng mL−1; Sigma‐Aldrich) in the presence of monensin (BD Biosciences) for the last 5 h before the flow cytometric analysis. After surface staining for CD4, intracellular staining for IL‐17 and Foxp3 was performed using the Cytofix/CytopermTM Plus (BD Biosciences) and Foxp3 Staining Kit (eBioscience), respectively. The flow cytometric analysis was performed using a flow cytometer (BD Biosciences) and analyzed using FlowJo software. For the proliferation assay, the CD4+ T cells were labeled with 2 μM CFSE, then cultured under Th17‐skewing conditions for 3 days before the flow cytometric analysis. For the apoptosis assay, CD4+ T cells were cultured under Th17‐skewing conditions for 3 days. The cells were stained using the FITC Annexin V Apoptosis Detection kit (BD Biosciences). Enzyme‐linked immunosorbent assay Blood samples were collected from the study subjects by venipuncture, and the plasma was then obtained by centrifugation. Synovial fluid was collected according to a previously described protocol. Briefly, the synovial cavity was washed carefully by repetitive injections and aspirations of 300 μL PBS. The plasma and synovial fluid samples were stored at –80°C prior to assay. The MT‐1 concentrations in the plasma and synovial fluid were determined using ELISA Kits (Uscn Life Science, Wuhan). The concentrations of IL‐1β, TNF‐α, IL‐6, IL‐17A, and IFN‐γ were measured according to the assay kit manufacturer's instructions (eBioscience). Reverse transcriptase‐quantitative polymerase chain reaction PBMCs were isolated using lymphocyte separation medium (TBD Science, China) and cultured with RPMI‐1640 supplemented with 10% FBS. Synovial tissues were obtained from the arthritis mice and ground into a powder under liquid nitrogen. CD4+ T cells were cultured under Th17‐skewing conditions and collected 3 days later. The RNA was extracted using Trizol (Invitrogen), and cDNA was prepared using ReverAid First Strand cDNA Synthesis Kit (Thermo). RT‐qPCR was performed using TransStart Tip Green qPCR SuperMix (Transgene Biotech) on a real‐time PCR system (7900 Fast, Applied Biosystems). The primers used for RT‐qPCR are summarized in Supporting Information Table 2. Western blotting CD4+ T cells that had been cultured for 3 days under Th17‐skewing conditions were lysed. Synovial tissue was obtained from the CIA mice and homogenized with RIPA lysis buffer (Solarbio). Equal amounts of proteins were separated on SDS/PAGE gels. Antibodies against STAT3, phospho‐STAT3 (p‐STAT3), and β‐actin were purchased from Cell Signaling Technology. The immunoreactive protein bands were visualized using an enhanced chemiluminescence detection system. Statistics The results are expressed as the mean ± SEM and were analyzed using Graphpad Prism software. Statistical comparisons of two groups were performed using a two‐tailed Student's t‐test. A two‐way ANOVA analysis was used for multiple comparisons. Differences with *p < 0.05, **p < 0.01, and ***p < 0.001 were considered to be significant. Acknowledgments This work was supported by grants from the Technology Development Project of Shenzhen Science and Technology Innovation Committee (grant CXZZ20150930105220591) and the Basic Research Project of Shenzhen Science and Technology Innovation Committee (grant JCY20150403091443312). The authors would like to thank the patients for donation of samples to the study. In addition, the authors thank the staff of Peking University Shenzhen Hospital for assistance with the collection of the clinical samples and members of the laboratory for help with the sample processing and clinical data. Jinxia Sun, Li Li, and Lingyun Li designed and performed the experiments and helped with the preparation of manuscript; Xiaokai Liu performed the experiment and helped with the writing of the manuscript; Liping Ding performed the RT‐qPCR and ELISA experiments; Xianxiong Chen performed the in vitro experiment; Jinshun Zhang and Xin Qi performed the in vivo experiment; Zhong Huang and Jing Du conceived and supervised the study and prepared the manuscript. Conflict of Interest The authors declare no commercial or financial conflicts of interest. Supporting Information References Abbreviations ACR American College of Rheumatology Ad‐MT‐1 adenovirus that expresses MT‐1 Ad‐Vec empty adenovirus CAIA collagen antibody‐induced arthritis HCs healthy controls RA rheumatoid arthritis RORγt RAR‐related orphan receptor gamma t

|
Scooped by
Gilbert C FAURE
September 10, 2018 1:23 PM
|
View printer-friendly version << Back Histogenics Announces Top-Line Results From Phase 3 Clinical Trial of NeoCart® in Patients With Knee Cartilage Damage ‒ Phase 3 Clinical Trial of NeoCart Did Not Meet Primary Endpoint of a Statistically Significant Improvement in Pain and Function in a Dual Threshold Responder Analysis One Year After Treatment as Compared to Microfracture ‒ ‒ NeoCart Demonstrated Statistically Significant and Clinically Meaningful Improvements on Dual Threshold Responder Analysis Six Months After Treatment and Nearly All Pain and Function Measures Compared to Microfracture One and Two Years After Treatment ‒ ‒ Data Compared Favorably to Other Products on the Market or in Development Per Guidance from the U. S. Food and Drug Administration ‒ ‒ Company to Discuss Plans for Submission of Biologics License Application with U.S. Food and Drug Administration ‒ ‒ Company to Host Conference Call and Webcast Today at 8:30 a.m. ET ‒ WALTHAM, Mass., Sept. 05, 2018 (GLOBE NEWSWIRE) -- Histogenics Corporation (Histogenics) (Nasdaq: HSGX), a leader in the development of restorative cell therapies that may offer rapid-onset pain relief and restored function, today announced that its Phase 3 clinical trial of NeoCart did not meet the primary endpoint of a statistically significant improvement in pain and function in a dual threshold responder analysis one year after treatment as compared to microfracture. In the modified Intent to Treat (mITT) population (which excludes those patients who were randomized but not treated with NeoCart), 74.2% of the NeoCart patients exhibited clinically meaningful improvements in pain and function compared to 62.0% of microfracture patients at one year (p=0.071). However, in this mITT population, patients treated with NeoCart achieved a statistically significant improvement in pain and function (p=0.018) six months after treatment as compared to patients treated with microfracture. Both NeoCart and microfracture were well tolerated and exhibited strong safety profiles. “Based on the totality of the data generated in the Phase 3 clinical trial, we continue to believe in NeoCart’s potential as a treatment for knee cartilage damage. When we designed our Phase 3 clinical trial in 2009, we set a very high clinical bar for NeoCart and narrowly missed hitting the trial’s primary endpoint with statistical significance by only two microfracture responders out of the 249 patients that participated in the trial. While the NeoCart treatment group exhibited a response as early as three months after treatment that continued through two years, the microfracture response rate was better than expected, which impacted the statistics. We are encouraged by the results and believe we have a meaningfully differentiated product that, if approved, can compete effectively and provide physicians and patients with a beneficial treatment option that may grow the market,” said Adam Gridley, President and Chief Executive Officer of Histogenics. “We continue to analyze the data and are in the process of scheduling a meeting with the FDA to discuss the results and prepare for a potential submission of a biologics license application for NeoCart. We wish to acknowledge and thank the patients and investigators who participated in the trial and shared their positive experiences with NeoCart,” stated Mr. Gridley. The NeoCart Phase 3 clinical trial is believed to be the largest and first prospectively designed, randomized clinical trial in North America evaluating the safety and efficacy of a restorative cell therapy to treat knee cartilage damage. It is also believed to be the only trial with a dual threshold responder analysis endpoint. As part of the prospective data analysis, Histogenics collected a variety of patient reported outcome endpoints, including all measures of the Knee Injury and Osteoarthritis Outcomes Score (KOOS) and the International Knee Documentation Committee (IKDC) score, which are validated, patient-centered assessments of pain and function that are commonly used in current clinical trials of cartilage therapies. On all but one of these measures, two of which are being utilized as primary endpoints in ongoing clinical trials by third parties in the U.S. for other therapies, NeoCart demonstrated statistically significant superiority versus microfracture at one and two years. The Phase 3 clinical trial is the first study prospectively enrolled consistent with current U.S. Food and Drug Administration (FDA) guidance, which provides for the use of microfracture as a comparator treatment in trials to repair knee cartilage damage. The published FDA guidance also specifically calls for a study population that, given the clinical limitations and variable results of microfracture, we believe provides more favorable results than what is typically seen in microfracture in both the literature and a real-world setting. “We are pleased with the overall performance of NeoCart in this Phase 3 clinical trial and the data confirm the feedback we have received from several of the investigators who participated in the trial. Most importantly, patients treated with NeoCart displayed an early and sustained recovery from pain and return to function that was clinically meaningful. The data from this trial are also consistent with results seen in prior clinical trials of NeoCart as well as the biomechanical data generated as part of our collaboration with Cornell University,” said Lynne Kelley, M.D., Chief Medical Officer of Histogenics. “While we are continuing to analyze the data, we have already seen a number of important results, including a statistically significant improvement of NeoCart compared to microfracture in lesion sizes of greater than 2 cm and patients with higher body mass index. We think that results such as these will be an important part of our planned discussions with the FDA, as well as with clinicians if NeoCart is approved,” continued Dr. Kelley. There are approximately 1.2 million arthroscopic procedures conducted each year to treat knee cartilage defects in the U.S., with less than half of eligible patients currently electing to receive treatment. Based on the data generated to date, NeoCart may offer many of these patients a safe and effective alternative, subject to FDA approval. “As a physician who treats patients with knee cartilage damage, I am keenly aware of the limitations of current treatment approaches for this common and underserved condition,” said David C. Flanigan, MD Associate Professor, Department of Orthopedics, Director, Cartilage Restoration Program at The Ohio State University Wexner Medical Center, and a high-enrolling investigator in the Phase 3 clinical trial. “The pain and loss of function associated with uncorrected knee cartilage lesions can significantly limit these patients’ ability to maintain their daily routines and often leads to other more serious comorbidities over time. The rapid recovery for patients who received this cartilage tissue implant compared to those who underwent microfracture indicates that implants, such as NeoCart, may be an attractive alternative for patients seeking a better quality of life and faster return to function,” continued Dr. Flanigan. The primary endpoint for the Phase 3 clinical trial was a dual-threshold responder analysis measuring the improvement in KOOS pain and IKDC function scores for each patient treated with NeoCart compared to those treated with microfracture one year after the time of treatment. Dual-threshold responders were defined as patients who, relative to their baseline measurements, had at least a 12-point improvement in the KOOS pain sub-score assessment and a 20-point improvement in the IKDC subjective assessment. The trial also evaluated additional pain, quality of life, and function outcomes using all five measures of KOOS subscales, including Sports and Recreation. The change from baseline and the relative change between the NeoCart and microfracture arms was also measured at one year which contrasts with clinical trials of other products, either on the market or in development, that measured these changes at two years. Efficacy and safety will continue to be followed out to three years, and Histogenics expects to further track patients for future planned analyses, including patients from prior clinical trials who received a NeoCart treatment. Demographics for both study arms were similar and represent a patient population that was intended to ensure that microfracture would respond favorably, including patients with an average age of approximately 39 years old and a Body Mass Index (BMI) of approximately 27. Furthermore, the mean lesion size was 2.1 cm in the NeoCart arm and 1.8 cm in the microfracture arm. There were no other significant differences between the treatment arms. The results with respect to the primary endpoint (dual threshold responder analysis one year after treatment) are summarized below: NeoCart Microfracture Positive Responders Responder Rate Positive Responders Responder Rate Difference ITT 121/170 71.2% 49/79 62.0% 9.2 p=0.1877 mITT 121/163 74.2% 49/79 62.0% 12.2 P=0.0714 As Treated 120/162 74.1% 50/80 62.5% 11.6 p=0.0735 Per Protocol 118/155 76.1% 43/65 66.2% 10.0 p=0.1362 Key additional findings from the clinical trial include: NeoCart demonstrated statistically significant improvements in pain and function at both one and two years after treatment as measured by changes in the KOOS and IKDC scores. KOOS pain score (mITT Population) Change from Baseline (NeoCart Baseline = 54.0; Microfracture Baseline = 52.4) NeoCart Microfracture Visit N Mean N Mean P-Value 3-months 160 24.1 75 22.4 0.0487* 6-months 157 28.6 75 27.0 0.0819 1-year 158 31.4 72 28.7 0.0239* 2-years 87 32.2 34 28.9 0.0080* 3-years 39 34.3 16 30.7 0.1071 * Statistically significant IKDC subjective knee exam score (mITT Population) Change from Baseline (NeoCart Baseline = 40.3; Microfracture Baseline = 40.0) NeoCart Microfracture Visit N Mean N Mean P-Value 3-months 159 13.7 76 14.5 0.9686 6-months 156 24.4 74 22.4 0.1572 1-year 158 33.1 71 28.3 0.0126* 2-years 87 35.3 34 30.2 0.0366* 3-years 38 39.9 16 32.6 0.2691 * Statistically significant NeoCart, the most advanced therapy from Histogenics restorative cell therapy platform, is functional cartilage that combines breakthroughs in bio-engineering, biomaterials and cell processing to enhance the autologous cartilage repair process. NeoCart, which is one of the most rigorously studied restorative cell therapies for orthopedic use, merges a patient’s own cells with a fortified three-dimensional scaffold designed to accelerate healing and reduce pain. NeoCart’s ability to function like cartilage at the time of treatment may enable patients to return to work and daily activities more rapidly than currently available treatment options such as microfracture. Histogenics is in the process of requesting a meeting with the FDA to discuss the data and a potential BLA submission. In addition, Histogenics intends to present the complete study results at upcoming medical conferences and will seek to have the data published in one or more peer reviewed journals. Conference Call and Webcast Information Histogenics management will host a conference call on Wednesday, September 5, 2018 at 8:30am EDT. A question-and-answer session will follow Histogenics’ remarks. To participate on the live call, please dial (877) 930-8064 (domestic) or (253) 336-8040 (international) and provide the conference ID 8764946 five to ten minutes before the start of the call. To access a live audio webcast of the presentation on the “Investor Relations” page of the Histogenics website, please click here. A replay of the webcast will be archived on Histogenics’ website for approximately 60 days following the presentation. About Histogenics Corporation Histogenics (Nasdaq: HSGX) is a leader in the development of restorative cell therapies that may offer rapid-onset pain relief and restored function. Histogenics’ lead investigational product, NeoCart, is designed to rebuild a patient’s own knee cartilage to treat pain at the source and potentially prevent a patient’s progression to osteoarthritis. NeoCart is one of the most rigorously studied restorative cell therapies for orthopedic use. NeoCart is designed to perform like articular hyaline cartilage at the time of treatment, and as a result, may provide patients with more rapid pain relief and accelerated recovery as compared to the current standard of care. Histogenics’ technology platform has the potential to be used for a broad range of additional restorative cell therapy indications. For more information on Histogenics and NeoCart, please visit www.histogenics.com. Forward-Looking Statements Various statements in this release are “forward-looking statements” under the securities laws. Words such as, but not limited to, “anticipate,” “believe,” “can,” “could,” “expect,” “estimate,” “design,” “goal,” “intend,” “may,” “might,” “objective,” “plan,” “predict,” “project,” “target,” “likely,” “should,” “will,” and “would,” or the negative of these terms and similar expressions or words, identify forward-looking statements. Forward-looking statements are based upon current expectations that involve risks, changes in circumstances, assumptions and uncertainties. Important factors that could cause actual results to differ materially from those reflected in Histogenics’ forward-looking statements include, among others: NeoCart’s potential as a treatment for knee cartilage damage; expectations regarding the timing and success of discussions with the FDA regarding the submission of a biologics license application for NeoCart; the timing, associated expenses and ability to obtain and maintain regulatory approval of NeoCart or any product candidates, and the labeling for any approved products; the market size and potential patient population in markets where Histogenics’ and its partners expect to compete; updated or refined data based on Histogenics’ continuing review and quality control analysis of clinical data; the scope, progress, timing, expansion, and costs of developing and commercializing Histogenics’ product candidates; the ability to obtain and maintain regulatory approval regarding the comparability of critical NeoCart raw materials following its technology transfer and manufacturing location transition; Histogenics’ expectations regarding its expenses and revenue; Histogenics’ ability to obtain additional debt or equity capital and other factors that are described in the “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” sections of Histogenics’ Annual Report on Form 10-K for the year ended December 31, 2017 and Quarterly Report on Form 10-Q for the quarter ended June 30, 2018, which are on file with the SEC and available on the SEC’s website at www.sec.gov. In addition to the risks described above and in Histogenics’ Annual Report on Form 10-K and Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and other filings with the SEC, other unknown or unpredictable factors also could affect Histogenics’ results. There can be no assurance that the actual results or developments anticipated by Histogenics will be realized or, even if substantially realized, that they will have the expected consequences to, or effects on, Histogenics. Therefore, no assurance can be given that the outcomes stated in such forward-looking statements and estimates will be achieved. All written and verbal forward-looking statements attributable to Histogenics or any person acting on its behalf are expressly qualified in their entirety by the cautionary statements contained or referred to herein. Histogenics cautions investors not to rely too heavily on the forward-looking statements Histogenics makes or that are made on its behalf. The information in this release is provided only as of the date of this release, and Histogenics undertakes no obligation, and specifically declines any obligation, to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise. Contacts: Investor Relations: Tel: +1 (781) 547-7909 InvestorRelations@histogenics.com Media Relations: Glenn Silver, Lazar Partners Ltd. Tel: + 1 (646) 871-8485 gsilver@lazarpartners.com Histogenics Corporation
SCs have proven their potential and safety for OA treatment. Nevertheless, there are still many questions to be resolved before their widespread used in clinical practice, such as the treatment mechanism, the best cell source, the most appropriate processing method, the most effective dose and delivery procedure, and their efficacy. In this sense, long-term follow-up and larger randomized controlled trials utilizing standardized and established outcome scores are mandatory to make objective conclusions.
Keywords: osteoarthritis, cell therapy, mesenchymal stem cells, cartilage regeneration, scaffolds/hydrogels, growth factors
Via Krishan Maggon

|
Scooped by
Gilbert C FAURE
June 6, 2018 5:37 AM
|
Osteoarthritis (OA) is the most common degenerative disease of the joint. Despite many reports and numerous clinical trials, OA is not entirely unders…

|
Scooped by
Gilbert C FAURE
April 11, 2018 11:07 AM
|
Defining environmental factors responsible for development of autoimmunity in rheumatoid arthritis (RA) is critical for understanding mechanisms of disease initiation and propagation. Notably, a history of cigarette smoking has been implicated in the genesis of RA and is associated with worse disease outcomes. Antibodies to peptidylarginine deiminase 4 (PAD4) are also associated with more severe RA. A subset of patients who have PAD4 autoantibodies that cross-react with PAD3 (anti-PAD3/4) are at the highest risk for interstitial lung disease, and this risk is augmented by a history of cigarette smoking. It is unclear, however, if smoking is etiologically linked to the development of anti-PAD4 antibodies. Patients were included in this study if they had physician-diagnosed RA as well as DNA, serum, and a date-matched clinical assessment (n = 274). Anti-PAD4 and anti-CCP antibodies were measured by immunoprecipitation and ELISA, respectively; shared epitope (SE) status was determined by HLA-DRβ1 genotyping. Logistic regression analysis was used to evaluate associations of smoking with PAD4 antibodies, with adjustment for relevant demographic and clinical features. Stratified analyses by disease duration and shared epitope status were also performed. Anti-PAD4 antibodies were present in 25% of RA patients, with 50% of these individuals having anti-PAD3/4 cross-reactive antibodies. Anti-PAD4 antibodies were significantly associated with a longer disease duration, SE alleles, and anti-CCP antibodies. Importantly, there were no significant differences in smoking history between anti-PAD4 positive and negative groups in univariate analyses, stratified analyses, or multivariable models. However, an inverse relationship between smoking and anti-PAD4 antibodies was suggested by a lower prevalence of current smokers among patients with anti-PAD3/4 antibodies compared to antibody negative individuals (p = 0.04). Further, the lowest levels of anti-PAD4 antibodies were observed in current smokers (p = 0.14), and a significant association of SE and anti-PAD4 antibodies was only present among never smokers (p = 0.01). Smoking history was not associated with anti-PAD4 antibodies in patients with RA. The finding that anti-PAD4 antibodies were not associated with smoking suggests that other environmental factors may contribute to the development of autoimmunity to PAD4 in these patients.

|
Scooped by
Gilbert C FAURE
March 1, 2018 3:12 PM
|
The autoantibody profile of seropositive rheumatoid arthritis (RA) is very diverse and consists of various isotypes and antibodies to multiple post-translational modifications. It is yet unknown whether this varying breadth of the autoantibody profile is associated with treatment outcomes. Therefore, we investigated whether the composition of the autoantibody profile in RA, as a marker of the underlying immunopathology, influences initial and long-term treatment outcomes. In serum from 399 seropositive patients with RA in the IMPROVED study, drawn at baseline and at the moment of drug tapering, we measured IgG, IgM, and IgA isotypes for anti-cyclic citrullinated peptide-2 and anti‐carbamylated protein antibodies, IgM and IgA rheumatoid factor, and reactivity against four citrullinated and two acetylated peptides (anti-modified protein antibodies (AMPAs)). We investigated the effect of the breadth of the autoantibody profile on (1) change in disease activity score (DAS)44 between 0 and 4 months, (2) initial drug-free remission (DFR, drug-free DAS44 < 1.6) achieved between 1 and 2 years of follow up, and (3) long-term sustained DFR until last follow up. Patients with a broad autoantibody profile at baseline had a significantly better early treatment response: ΔDAS 0–4 months of 1–2, 3–4, and 5–6 vs 7–8 isotypes, -1.5 (p < 0.001), -1.7 (p = 0.03), and -1.8 (p = 0.04) vs -2.2. Similar results were observed for AMPA number. However, patients with a broad baseline autoantibody profile achieved less initial DFR. For long-term sustained DFR there was no longer an association with the breadth of the autoantibody response. When assessing autoantibodies at the moment of tapering, similar trends were observed. A broad baseline autoantibody profile is associated with a better early treatment response. The breadth of the baseline autoantibody profile, reflecting a break in tolerance against several different autoantigens and extensive isotype switching, may indicate a more active humoral autoimmunity, which could make the underlying disease processes initially more suppressible by medication. The lack of association with long-term sustained DFR suggests that the relevance of the baseline autoantibody profile diminishes over time.
ISRCTN11916566
. Registered on 7 November 2006. EudraCT, 2006- 06186-16. Registered on 16 July 2007.

|
Scooped by
Gilbert C FAURE
February 14, 2018 4:51 AM
|
High-throughput sequencing assays have become an increasingly common part of biological research across multiple fields. Even as the resulting sequences pile up in public databases, it is not always obvious how to make use of these data sets. Functional genomics offers approaches to integrate these "big" data into our understanding of rheumatic diseases. This review aims to provide a primer on thinking about big data from functional genomics in the context of rheumatology, using examples from the field’s literature as well as the author’s own work to illustrate the execution of functional genomics research. Study design is crucial to ensure the right samples are used to address the question of interest. In addition, sequencing assays produce a variety of data types, from gene expression to 3D chromatin structure and single-cell technologies, that can be integrated into a model of the underlying gene regulatory networks. The best approach for this analysis uses the scientific process: bioinformatic methods should be used in an iterative, hypothesis-driven manner to uncover the disease mechanism. Finally, the future of functional genomics will see big data fully integrated into rheumatology, leading to computationally trained researchers and interactive databases. The goal of this review is not to provide a manual, but to enhance the familiarity of readers with functional genomic approaches and provide a better sense of the challenges and possibilities.

|
Scooped by
Gilbert C FAURE
January 12, 2018 1:06 PM
|
The European Medicines Agency updated guidance on clinical investigations of rheumatoid arthritis drugs to add new endpoints and distinguish between patient subgroups in trials. Drug therapy for rheumatoid arthritis has made major advances since 2003 when the EMA issued a Points to Consider document, including more intensive early-disease intervention, with many combining biologic and non-biologic disease-modifying anti-rheumatic drugs (DMARDs). As a result of the advances, endpoints for treatment targets of remission have also changed to reflect earlier interventions than the previous six-month primary endpoint, the . . .

|
Scooped by
Gilbert C FAURE
December 29, 2017 2:54 AM
|
Considerable progress has been made recently in understanding the complex pathogenesis and treatment of spondyloarthropathies (SpA). Currently, along with traditional disease modifying anti-rheumatic drugs (DMARDs), TNF-α, IL-12/23 and IL-17 are available for treatment of such diseases as ankylosing spondylitis (AS) and psoriatic arthritis (PsA). Although they adequately control inflammatory symptoms, they do not affect the abnormal bone formation processes associated with SpA. However, the traditional therapeutic approach does not cover the regenerative treatment of damaged tissues. In this regards, stem cells may offer a promising, safe and effective therapeutic option. The aim of this paper is to present the role of mesenchymal stromal cells (MSC) in pathogenesis of SpA and to highlight the opportunities for using stem cells in regenerative processes and in the treatment of inflammatory changes in articular structures.

|
Scooped by
Gilbert C FAURE
July 13, 2017 2:46 PM
|
The main goal of antigen-specific immunotherapy (ASI) in autoimmune and rheumatic diseases is to reprogramme or remove autoreactive cells and/or induce immune tolerance to self-antigens. Current therapies in these diseases either treat symptoms or slow down disease progression but are not yet curative or preventative — disease-specific treatments are urgently needed. In contrast to the nonspecific treatments in current use that induce generalized immune suppression, which is associated with several adverse effects including increased risk of infections, ASIs target a restricted subset of B cells or T cells, and thus do not compromise systemic immunity and host defence. This Review provides a summary of novel approaches for identifying autoepitopes and detecting and targeting autoreactive cells that might help in the development of ASIs. Promising approaches include the use of tolerizing peptides coupled to MHC constructs and/or nanocompounds, tolerizing dendritic cells and antigen-specific vaccines. Following studies in animal models of rheumatoid arthritis and systemic lupus erythematosus, several of these strategies have now entered clinical trials. However, to use these approaches in humans, several important limitations must first be addressed, such as; selecting the proper immunodominant autoantigen; identifying the optimal timing, dosing and route of administration; finding biomarkers for monitoring the therapy; and optimizing methodology.
|

|
Scooped by
Gilbert C FAURE
November 24, 2018 3:54 AM
|
Subclinical joint inflammation in patients with arthralgia is predictive for progression to rheumatoid arthritis (RA). However, the time course of progression for bone marrow edema (osteitis), synovitis, and/or tenosynovitis is unsettled.

|
Scooped by
Gilbert C FAURE
November 10, 2018 7:00 AM
|
Varicella zoster virus (VZV)-specific cellular immunity is essential for viral control, and the incidence of VZV reactivation is increased in patients with rheumatic diseases. Because knowledge of the influence of antirheumatic drugs on specific cellular immunity is limited, we analyzed...

|
Suggested by
Société Francaise d'Immunologie
October 13, 2018 5:37 AM
|
Tumor necrosis factor (TNF) is a pleiotropic cytokine involved in many aspects of immune regulation. Anti-TNF biological therapy has been considered a breakthrough in the treatment of chronic autoimmune diseases, such as rheumatoid arthritis (RA).

|
Scooped by
Gilbert C FAURE
September 20, 2018 2:06 AM
|
Author M.H. Cardiel P.P. Tak W. Bensen F.X. Burch S. Forejtova J.E. Badurski T. Kakkar T. Bevirt L. Ni E. McCroskery A. Jahreis D.J. Zack Year 2010 Title A phase 2 randomized, double-blind study of AMG 108, a fully human monoclonal antibody to IL-1R, in patients with rheumatoid arthritis Journal Arthritis Research & Therapy Volume | Issue number 12 | 5 Pages (from-to) R192 Document type Article Faculty Faculty of Medicine (AMC-UvA)Abstract Introduction: Preclinical work has suggested that IL-1 plays a critical role in the pathogenesis of rheumatoid arthritis (RA). The objective of the present study was to determine the effect of a long-acting IL-1 receptor inhibitor, AMG 108, in a double-blind, placebo-controlled, parallel-dosing study in patients with active RA who were receiving stable methotrexate (15 to 25 mg/week). Methods: Patients were randomized equally to receive placebo or 50, 125, or 250 mg AMG 108 subcutaneously every 4 weeks for 6 months. The primary efficacy endpoint was a 20% improvement in the American College of Rheumatology response (ACR20) at week 24; other efficacy endpoints included the ACR50, the ACR70, and the RA disease activity score (28-joint count Disease Activity Score) responses, patient-reported outcomes, and pharmacokinetic parameters. Safety endpoints included treatment-emergent adverse events (AEs), infectious AEs, serious AEs, serious infections, injection site reactions, laboratory abnormalities, and antibodies to AMG 108. Results: Of 813 patients enrolled in the study, 204 patients were randomized to the 50 mg group, 203 to the 125 mg group, 203 to the 250 mg group, and 203 to placebo. At week 24, 40.4% of the 250 mg group, 36% of the 125 mg group, 30.9% of the 50 mg group, and 29.1% of the placebo group achieved an ACR20 (P = 0.022, 250 mg vs. placebo). Of the individual ACR components, numerical dose-dependent improvements were only seen in tender joint counts, pain (visual analog scale), and the acute phase reactants, erythrocyte sedimentation rate and C-reactive protein. No dose-related increase was observed in the incidence of treatment-emergent AEs. No deaths were reported, and the incidence of AEs and infections, serious AEs and infections, and withdrawals from study for safety were similar in the AMG 108 and placebo groups. Conclusions: This large double-blind randomized trial with a long-acting IL-1 receptor blocker, AMG 108, is consistent with the experience of other IL-1 blockers, represents a definitive experiment showing that IL-1 inhibition provides only moderate symptomatic amelioration of arthritis activity in the majority of RA patients, and provides an answer to a question that has been discussed for many years in the rheumatologic community URL go to publisher's site Language Undefined/Unknown Permalink http://hdl.handle.net/11245/1.339571 Downloads Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library, or send a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible.
Immunotherapy has revolutionized the treatment of cancer, but a rapid rise in the use of the family of therapeutic agents known as checkpoint inhibitors (CPIs) is associated with a new group of immune-related adverse events (irAEs) in almost any organ system. Among these irAEs, rheumatic complications are common and seem to have features that are distinct from irAEs in other organ systems, including a highly variable time of clinical onset and the capacity to persist, possibly indefinitely, even after cessation of CPI therapy. In this Review, mechanisms of action of CPIs and how they might cause rheumatic irAEs are described. Also covered are epidemiology and clinical descriptions of rheumatic irAEs, plus guiding principles for managing irAEs. Finally, we outline future directions that must be taken in response to a series of unanswered questions and unmet needs that now confront rheumatologists who are, or will be, engaged in this new area of rheumatology.
Via Krishan Maggon
Some patients with psoriatic arthritis are refractive to one biologic therapy but not to others, and a strategy for selecting the right therapy for each patient is needed. The findings of a new study highlight the potential benefit of stratifying patients by their immunophenotype to select the...
Via Krishan Maggon

|
Scooped by
Gilbert C FAURE
May 14, 2018 1:39 PM
|

|
Scooped by
Gilbert C FAURE
March 12, 2018 5:14 AM
|
Changes in articular cartilage during the aging process are a stage of natural changes in the human body. Old age is the major risk factor for osteoarthritis but the disease does not have to be an inevitable consequence of aging. Chondrocytes are particularly prone to developing age-related changes. Changes in articular cartilage that take place in the course of aging include the acquisition of the senescence-associated secretory phenotype by chondrocytes, a decrease in the sensitivity of chondrocytes to growth factors, a destructive effect of chronic production of reactive oxygen species and the accumulation of the glycation end products. All of these factors affect the mechanical properties of articular cartilage. A better understanding of the underlying mechanisms in the process of articular cartilage aging may help to create new therapies aimed at slowing or inhibiting age-related modifications of articular cartilage. This paper presents the causes and consequences of cellular aging of chondrocytes and the biological therapeutic outlook for the regeneration of age-related changes of articular cartilage.

|
Scooped by
Gilbert C FAURE
March 1, 2018 10:53 AM
|
Systemic autoimmunity can be present years before clinical onset of rheumatoid arthritis (RA). Adaptive immunity is initiated in lymphoid tissue where lymph node stromal cells (LNSCs) regulate immune responses through their intimate connection with leucocytes. We postulate that malfunctioning of LNSCs creates a microenvironment in which normal immune responses are not properly controlled, possibly leading to autoimmune disease. In this study we established an experimental model for studying the functional capacities of human LNSCs during RA development. Twenty-four patients with RA, 23 individuals positive for autoantibodies but without clinical disease (RA risk group) and 14 seronegative healthy control subjects underwent ultrasound-guided inguinal lymph node (LN) biopsy. Human LNSCs were isolated and expanded in vitro for functional analyses. In analogous co-cultures consisting of LNSCs and peripheral blood mononuclear cells, αCD3/αCD28-induced T-cell proliferation was measured using carboxyfluorescein diacetate succinimidyl ester dilution. Fibroblast-like cells expanded from the LN biopsy comprised of fibroblastic reticular cells (gp38+CD31−) and double-negative (gp38−CD31−) cells. Cultured LNSCs stably expressed characteristic adhesion molecules and cytokines. Basal expression of C-X-C motif chemokine ligand 12 (CXCL12) was lower in LNSCs from RA risk individuals than in those from healthy control subjects. Key LN chemokines C-C motif chemokine ligand (CCL19), CCL21 and CXCL13 were induced in LNSCs upon stimulation with tumour necrosis factor-α and lymphotoxin α1β2, but to a lesser extent in LNSCs from patients with RA. The effect of human LNSCs on T-cell proliferation was ratio-dependent and altered in RA LNSCs. Overall, we developed an experimental model to facilitate research on the role of LNSCs during the earliest phases of RA. Using this innovative model, we show, for the first time to our knowledge, that the LN stromal environment is changed during the earliest phases of RA, probably contributing to deregulated immune responses early in disease pathogenesis.

|
Rescooped by
Gilbert C FAURE
from CME-CPD
February 2, 2018 3:36 AM
|
Giant cell arteritis: Overcoming the Limitations of Conventional Agents with Biologic Therapy Author(s)/Faculty: Leonard H. Calabrese, DO ; Eamonn Molloy, MD, MS, FRCPI; John H. Stone, MD, MPH

|
Scooped by
Gilbert C FAURE
December 29, 2017 2:57 AM
|
Trials. 2017 Dec 19;18(1):605. doi: 10.1186/s13063-017-2363-z.

|
Suggested by
LIGHTING
September 22, 2017 9:53 AM
|
For patients with osteoarthritis, the current palliative approach of analgesic prescription followed by joint replacement is often inappropriate. Instead, care should be tailored to the needs of individuals and targeted towards the central complaints of pain and functional limitation. So why are we still getting it wrong?
|



 Your new post is loading...
Your new post is loading...