 Your new post is loading...
 Your new post is loading...
Neuropathy Presentation II: El Paso, TX. Chiropractor, Dr. Alexander Jimenez continues the overview with neuropathy part II. Continued are the most common neuropathies to be seen in practice. Because the human body is composed of many different kinds of nerves which perform different functions, nerve damage is classified into several types. Neuropathy can also be classified according to the location of the nerves being affected and according to the disease causing it. For instance, neuropathy caused by diabetes is called diabetic neuropathy. Furthermore, depending on which nerves are affected will depend on the symptoms that will manifest. The complications which follow neuropathy depends on the type of nerves that are damaged. According to Dr. Jimenez, different neuropathies can cause numbness and/or tingling sensations, increased pain or the loss of ability to feel pain, muscle weakness along with twitching and cramps, even dizziness and/or loss of bladder control function. Sciatic Nerve Entrapment - Piriformis Syndrome
- Peroneal Nerve Entrapment
- Tarsal Tunnel Syndrome
Sciatic N. Piriformis Syndrome Causes - Anatomic variation
- Piriformis overuse/tension
Exam - Positive Lasègue test possible
- Doctor extends patient’s leg passively, while patient is lying supine positive test if maneuver is limited by pain
- Tenderness and palpable tension in piriformis muscle which elicits symptoms
Sciatic N. Peroneal Nerve Entrapment - Peroneal or Fibular branch of Sciatic nerve entrapped at the fibular head
- Tinel’s sign may be present at fibular head/neck
- Usually affects common peroneal nerve, therefore motor and sensory symptoms can be seen
- Weakness of ankle dorsiflexion and eversion (tibialis anterior m.)
- Sensory disruption on the dorsum of the foot and lateral aspect of the calf
Sciatic N. Tarsal Tunnel Syndrome - Tibial nerve impinged in the tarsal tunnel
- Sensory changes in the sole of the foot
- Tinel’s sign may be present with percussion posterior to the medial malleolus
Radiculopathy - A mononeuropathy – located in one specific area
- Neuropathy involving spinal nerve roots
- Presents as changes in sensory and/or motor function affecting a single or a few nerve root level(s)
- Most commonly seen radiculopathies include:
- Sciatica
- Cervical radiculopathy
Common Causes Of Radiculopathy - Disc herniation
- Osteophytes
- Spinal Stenosis
- Trauma
- Diabetes
- Epidural abscess or metastasis
- Nerve sheath tumors (schwannomas and neurofibromas)
- Guillain-Barré syndrome
- Herpes Zoster (shingles)
- Lyme disease
- Cytomegalovirus
- Myxedema/Thyroid disorder
- Idiopathic neuritis
Narrowing Down Common Causes Of Radiculopathy -
Disc Herniation - Most commonly affected nerve roots are C6, C7, L5 & S1
-
Spinal Stenosis - Lumbar stenosis may produce neurogenic claudication
- Pain & weakness with ambulation
- Cervical stenosis may present with mixed picture of radiculopathy and myelopathy due to long tract involvement
-
Trauma - May cause compression, trauma or avulsion of the nerve roots
-
Diabetes - More likely to cause a polyneuropathy, but mononeuropathy is possible
-
Herpes Zoster (Shingles) - Most often on the trunk, accompanied by vesicular lesions in a single dermatome
- If pain persits past vesicular regression = post-herpetic neuralgia
Patient History Of Radiculopathy - The patient will often complain of burning pain or tingling that radiates or shoots down an affected area in a dermatomal pattern.
- Sometimes patient will complain of motor weakness, however if onset is recent, there is often no motor involvement
Exam Of Radiculopathy - Most often hypoesthesia in the affected dermatome level
- Best to evaluate for pain, as light touch can be difficult for these patient’s to distinguish
- Fasciculations and/or atrophy may be seen if radiculopathy is chronic, due to lower motor neuron being impinged
- Motor weakness may be seen in muscles innervated by the same root level
Orthopedic tests: -
Straight-leg raise test (SLR) - Pain between 10-60 degrees likely indicates nerve root compression
-
Well-leg raise/Crossed straight-leg raise test (WLR) - If positive, 90% specificity for L/S nerve root compression
-
Valsalva Maneuver - Positive if increase in radicular symptoms
-
Spinal Percussion - Pain may indicate metastatic disease, abscess or osteomyelitis
Examinations: Merck Manual Professional Dermatomes Testing Cervical Nerve Roots Testing Lumbosacral Nerve Roots Specific Radiculopathy Patterns -
T1 radiculopathy can cause Horner’s syndrome - This is due to affect on cervical sympathetic ganglia
- Ptosis, miosis, anhidrosis
-
Below L1, radiculopathies can cause Cauda Equina syndrome - Saddle anesthesia (sensory loss in S2-S5 distribution)
- Urinary retention or overflow incontinence
- Constipation, decreased rectal tone or fecal incontinence
- Loss of erectile function
- Must be referred for emergency care immediately to prevent permanent dysfunction
Other Patterns Of Neuropathy -
Cape/Shawl distribution of symptoms - Intramedullary lesion
- Syringomyelia
- Intramedullary tumor
- Central cord damage
-
Stocking and Glove Distribution of Symptoms - Diabetes mellitus
- B12 deficiency
- Alcoholism/hepatitis
- HIV
- Thyroid dysfunction/myxedema
Cape/Shawl Pattern - Intramedullary lesion such as tumor, syringomyelia or hyperextension injury in patient with C/S spondylosis
- Loss of pain and temp sensation in C/T dermatomes because of arrangement of lateral spinothalamic tract
Stocking & Glove Pattern - Symmetrical polyneuropathy
- Feet/legs usually affected first, followed by hands/arms
- Vibration sensation in the smallest toes is usually the first thing lost and neuropathy progresses across foot to great toe and then upward through the ankle and leg, then hands, arms and finally trunk if sever
- Most likely cause of this distribution is diabetes mellitus, but other possible causes include B12 deficiency, alcoholism, HIV, chemotherapy treatment, thyroid dysfunction and multiple other causes
Diabetic Neuropathy - Diabetic neuropathy often presents as a polyneuropathy but can also present as a mononeuropathy, usually with acute onset
- Most common in CN III, femoral and sciatic nerves
Demyelinating Neuropathies - Acute inflammatory demyelinating polyneuropathy (Guillain-Barré syndrome)
- Chronic inflammatory demyelinating polyneuropathy
Guillain-Barré Syndrome (AIDP) - Onset 1-2 weeks post viral infection
- Progressive weakness
- Loss of DTRs/areflexia
- Paresthesia in hands and feet
- More motor involvement than sensory
- Potential autonomic fiber involvement
- Elevated CSF protein
- EMG/NCV studies indicate demyelination
- May require treatment with plasmapheresis or IV Ig therapy
Chronic Inflammatory Demyelinating Polyneuropathy - Appears similar to AIDP but does not follow infection
- Symptoms must be present for at least 8 weeks for this diagnosis to be considered
- Anti-inflammatory treatments may help
By Rachel Klein, ND, DC, DACNB National University of Health Sciences Master of Science (MS) - Advanced Clinical Practice (ACP) MS ACP 551: Clinical Neurology © 2018 Sources Blumenfeld, Hal. Neuroanatomy through Clinical Cases. Sinauer, 2002. Evans, Ronald C. Illustrated Orthopedic Physical Assessment. Mosby/Elsevier, 2009. “Radial Nerve Entrapment: Background, Anatomy, Pathophysiology.” Medscape, 25 Oct. 2017, emedicine.medscape.com/article/1244110- overview#a8.
Neuropathy Presentation: El Paso, TX. Chiropractor, Dr. Alexander Jimenez presents an overview of neuropathy. These are the most common neuropathies to be seen in practice. Neuropathy is a medical term used to characterize damage or injury to the nerves, which refers to the peripheral nerves as opposed to the central nervous system. The complications which follow neuropathy depends largely on the type of nerves that are affected. According to Dr. Alex Jimenez, different neuropathies can cause numbness and tingling sensations, increased pain or the loss of ability to feel pain, muscle weakness along with twitching and cramps, even dizziness and/or loss of control over bladder function. Neuropathy Three primary classifications based on location of symptoms: - Mononeuropathy (focal)
- Mononeuropathy multiplex (multifocal)
- Polyneuropathy (generalized)
- Can involve CNS and/or PNS
- Can affect large and/or small diameter fibers
- Can affect both sensory and motor fibers
- Sometimes one more than the other, but often both
- May be permanent or reversible
*https://neupsykey.com/muscle-weakness-cramps-and-stiffness/ Assessment Of Neuropathy Sensory Exam: -
Determine What Sensory Modalities Are Involved - If sensory disruption is limited to certain modalities, it implies CNS is involved
- If all sensation is affected in the area, implies PNS is involved
-
Determine Pattern Of Symptoms - Mononeuropathy (focal)?
- Mononeuropathy multiplex (multifocal)?
- Polyneuropathy (generalized)?
-
Motor Exam - Determine if there is change to muscle strength
- Determine if there is a change in muscle tone
- Determine which muscles are affected
- Determine if there has been a change in reflexes
- This information can help determine the level(s) of involvement
-
Check For Autonomic Signs - Auscultate heart
- Palpate palms
- Auscultate abdomen
- Assess autonomic history
- For example, is patient complaining about sweating more on one side than another? Complaining of stress levels?
- Suggest ANS involvement
Exams: Merck Manual Professional Version Classification Of Nerve Injuries Resulting In Neuropathy - Neurapraxia - This is a transient episode of motor paralysis with little or no sensory or autonomic dysfunction; no disruption of the nerve or its sheath occurs; with removal of the compressing force, recovery should be complete
- Axonotmesis - This is a more severe nerve injury, in which the axon is disrupted but the Schwann sheath is maintained; motor, sensory, and autonomic paralysis results; recovery can occur if the compressing force is removed in a timely fashion and if the axon regenerates
- Neurotmesis - This is the most serious injury, in which both the nerve and its sheath are disrupted; although recovery may occur, it is always incomplete, secondary to loss of nerve continuity
Brachial Plexopathies - Erb’s Palsy
- Klumke’s Palsy
Erb’s Palsy - AKA Erb–Duchenne palsy or Waiter's tip palsy
- Most common mechanism of injury in adults is a patient who fall forward while holding onto something behind them
- Can also happen to an infant during childbirth Results from damage to C5-6 nerve roots in the brachial plexus
- Dermatomal distribution of sensory disruption
- Weakness or paralysis in deltoid, biceps, and brachialis muscles resulting in “waiter’s tip” position
Klumke’s Palsy - AKA Dejerine–Klumpke palsy
- Happens to infants during childbirth if arm is pulled overhead
- Can also happen to adults with overhead traction injuries
- Results from damage to C8-T1 nerve roots in the brachial plexus
- Dermatomal distribution of sensory disruption
- Weakness or paralysis in wrist flexors and pronators as well as muscles of the hand
- May produce Horner’s syndrome due to T1 involvement
- Results in a “claw hand” appearance
- Forearm supinated with wrist hyperextended, with finger flexion
Entrapment Neuropathies - Thoracic Outlet Syndromes
- Median Nerve Entrapment
- Pronator Teres syndrome
- Carpal Tunnel syndrome
- Ulnar Nerve Entrapment
- Cubital Tunnel syndrome
- Tunnel of Guyon syndrome
- Radial Nerve Entrapment
- Spiral Groove Entrapment
- Supinator Syndrome
- Posterior Interosseous Syndrome (Radial Tunnel Syndrome)
- Sciatic Nerve Entrapment
- Piriformis syndrome
- Fibular head entrapment
- Tarsal tunnel syndrome
Thoracic Outlet Syndromes -
Neurogenic thoracic outlet syndrome - Compression of the brachial plexus
-
Vascular thoracic outlet syndrome - Veins (venous thoracic outlet syndrome) or arteries (arterial thoracic outlet syndrome) are compressed
-
Nonspecific-type thoracic outlet syndrome - Worsens with activity
- Idiopathic
Causes - Cervical rib
- Subclavius muscle tension
- Postural - excessive thoracic kyphosis
- Trauma
- Repetitive activity
- Obesity
- Pregnancy
Tests - Adsons test
- Allen maneuver
- Costoclavicular maneuver
- Halstead maneuver
- Reverse bakody maneuver
- Roos test
- Shoulder compression test
- Wright test
Median Nerve Entrapment - Sensory disruption in the lateral portion (3.5 fingers) of the palmar aspect of the hand, and dorsal finger tips of the same fingers
- Motor fibers affected in forearm if applicable, muscles of the thenar eminence
- Abductor pollicis brevis
- Opponens pollicis
- Flexor pollicis brevis
Median N. Pronator Teres Syndrome Etiology - Compression of the median nerve at the elbow
Causes - Repetitive movement
- Pronator teres muscle inflammation
- Thickened bicipital aponeurosis
Findings - Tenderness with palpation of the pronator teres muscle
- Pain with resisted pronation of the arm
- Flexor pollicus longus and flexor digitorum profundus involvement
- Otherwise may appear similar to carpal tunnel syndrome in symptoms, but without positive wrist orthopedics
Median N. Carpal Tunnel Syndrome Etiology - Compression of the median nerve at the wrist
Causes - Repetitive motions
- Hypothyroidism
- Obesity
- Rheumatoid Arthritis
- Diabetes
- Pregnancy
Orthopedic Tests Tinel’s Sign - Positive if tapping over the median nerve reproduces/exacerbates symptoms
Phalen’s Maneuver/Prayer Sign - Hands together with wrists flexed
- Repeat in reverse with wrists extended
- Hold each for at least 60 seconds
- Positive if tests reproduce/exacerbate symptoms
Wringing Test - Wringing a towel produces paresthesia
Ulnar Nerve Entrapment - Sensory disruption in the medial two digits of the palmar & dorsal aspects of the hand
- Motor fibers affected in hand, all fingers besides the thumb weakened general hand weakness
Ulnar N. Cubital Tunnel Syndrome Etiology - Compression of the ulnar nerve at the elbow
Causes - Repetitive motions
- Hypothyroidism
- Obesity
- Diabetes
- Trauma to the cubital tunnel
- Prolonged sitting with pressure on bent elbow
Ulnar N. Tunnel Of Guyon Syndrome Etiology - Compression of the ulnar nerve at the wrist
Causes Repetitive motions - Long term crutch use
- Break of the hamate
- Ganglion cyst
- Hypothyroidism
- Obesity
- RheumatoidArthritis
- Diabetes
Orthopedic Tests Tinel’s Sign - Present if test over the ulnar nerve at the wrist elicits symptoms
Wartenberg Sign - 5th digit abducts when patient performs hard grip strength test or attempts to squeeze fingers together
- Reduced two-point discrimination in the hand
Radial Nerve Entrapment - Sensory disruption in the lateral 3.5 digits of the dorsal aspect of the hand
- Motor fibers affected in posterior arm and extensor compartment of the forearm
- Wrist drop may be seen
Spiral Groove Entrapment - All radial nerve innervated muscles below entrapment are affected
- “Saturday night palsy” (from sleeping on own arm)
- Brachioradialis & triceps reflexes both diminished
Supinator Syndrome - Compression at the arcade of Frohse
- No change in reflexes
Posterior Interosseous Syndrome (Radial Tunnel Syndrome) By Rachel Klein, ND, DC, DACNB National University of Health Sciences Master of Science (MS) - Advanced Clinical Practice (ACP) MS ACP 551: Clinical Neurology © 2018 Sources Blumenfeld, Hal. Neuroanatomy through Clinical Cases. Sinauer, 2002. Evans, Ronald C. Illustrated Orthopedic Physical Assessment. Mosby/Elsevier, 2009. “Radial Nerve Entrapment: Background, Anatomy, Pathophysiology.” Medscape, 25 Oct. 2017, emedicine.medscape.com/article/1244110- overview#a8.
Neuropathy affects about 8 percent of individuals over the age of 55. Your nervous system is composed of 2 parts: the central nervous system and the peripheral nervous system. The nerves of your peripheral nervous system transmit messages between your central nervous system, that is your brain and spinal cord, along with the rest of the body. These nerves regulate a massive range of functions throughout the body, such as voluntary muscle movement, involving the motor nerves, involuntary organ action, through the autonomic nerves, and also the perception of stimuli, involving the sensory nerves. Peripheral neuropathy, which is often simply referred to as “neuropathy,” is a state that happens when your nerves become damaged or injured, often times simply disrupted. It’s estimated that neuropathy affects roughly 2.4 percent of the general populace and approximately 8 percent of people older than age 55. However, this quote doesn’t include people affected by neuropathy caused by physical trauma to the nerves.
Back pain is one of the most common complaints reported by a majority of the population. Affecting many people temporarily or for an extended period of time at least once throughout their lifetime, back pain is generally the result of trauma from an accident, injury or due to an aggravated medical condition. But, can an improper diet based on refined sugar and processed fat cause back pain?
Researchers from Rensselaer Polytechnic Institute and the Icahn School of Medicine believe that consuming an excess amount of these foods can cause inflammation in the body which may gradually degenerate the intervertebral discs, cartilaginous joints found between each vertebrae that act as shock absorbers and ligaments for all the movements of the spine. The degeneration of these structures may lead to back pain and other spinal complications.
Furthermore, an improper nutrition is also associated with the development of type 2 diabetes, another factor which may cause changes to the spine that could also lead to back pain and other painful symptoms.
Pesticides are some of the most harmful substances found in our environment today. The primary function of these chemicals is to eradicate unwanted insects, plants, molds and rodents. They are also utilized in a variety of settings, including homes and schools. Chemicals referred to as insecticides, herbicides, fungicides and bactericides are all different forms of pesticides. This includes: bug bombs, ant spray, mosquito spray, mosquito fogging, termicides, flea and tick spray, lice treatments, bee and wasp spray, weed prevention, weed abatement, crop spraying and rodent control. Individuals with allergies, asthma or nerve damage may have already be affected by the pesticides in the environment.
Prolonged exposure to pesticides has been previously associated with poor mental development, autism and ADHD. One research study even determined that pesticides may be capable of inducing some of the core characteristics of pervasive development disorders or autism. Further experimental and observational research data suggested a connection between parental pesticide exposure and physical birth defects, low birth weight and fetal death.
A research study published in the Journal of the American Medical Association in September 2015 demonstrated that nearly 50 percent of adults in the United States may have pre-diabetes or diabetes.
Approximately 9 out of 10 people may have undiagnosed pre-diabetes while 1 out of every 4 people may have undiagnosed diabetes. Statistics from the Center for Disease Control also revealed that about 30 percent of all individuals with pre-diabetes will develop type 2 diabetes within 5 years.
While these statistics have become dangerously alarming in the United States, the increasing issue of pre-diabetes and diabetes cases in adults has been growing throughout the world. Over the last decade, for instance, Great Britain has seen a drastic rise in both pre-diabetes and diabetes cases as well. According to a BBC News report, approximately more than one-third of British adults have been diagnosed with pre-diabetes, as compared to a 2003 report, where only 11.6 percent of British adults had been diagnosed with pre-diabetes. By 2011, the amount of individuals diagnosed with the conditions had almost tripled to about 35.3 percent.
Pre-diabetes is medically characterized as having a fasting blood sugar of 100-125 mg/dl or a hemoglobin A1C of 5.7-6.4 percent. Researchers medically defined diabetes as having a fasting blood sugar greater than 126 mg/dl or a hemoglobin A1C > 6.5 percent, a measure of long term glucose control.
Throughout the United States, U.K., and Australia, more and more cases of liver disease are arising in the absence of alcohol abuse. Decades ago, we only saw conditions like Fatty Liver Disease and cirrhosis occur as a direct result of excessive alcohol indulgence, however, this trend has changed in the current day. Today, more and more adults and children are being diagnosed with NON-ALCOHOLIC FATTY LIVER DISEASE (NAFLD).
NAFLD is a medical condition that is characterized by an excessive accumulation of fats, within liver cells. This means normal, healthy liver tissue becomes partly replaced with fatty tissue. The fat starts to invade the liver, gradually infiltrating the healthy liver areas, decreasing the amount of healthy active liver tissue. While it’s normal for your liver to contain some fat, accumulations of more than 5 percent to 10 percent of your liver’s weight are problematic. 70 million Americans have fatty liver disease and don’t even know it.
Did you ever let your foot fall asleep and suffer first from numbness and then from a tingling, pins-and-needles sensation while it “awakened”? People with peripheral neuropathy suffer from those types of sensations all the time. And there’s growing evidence that peripheral neuropathy is linked with celiac disease and gluten sensitivity.
Peripheral neuropathy is a condition that occurs from damaged nerves in the arms, legs, hands, and feet. Commonly, symptoms experienced as a result of this are numbness, tingling, burning, and pain. The condition has a number of different causes, such as, diabetes, chemotherapy, statin medications, disc herniation and traumas, toxic metal exposure, chronic alcohol consumption and vitamin deficiencies. Now, however, scientists have linked peripheral nerve damage to gluten sensitivity and celiac disease.
Gluten is a protein found in wheat, rye, spelt, kamut and barley. Celiac disease is an autoimmune disorder that wreaks havoc on the digestive tract. When a person afflicted with celiac’s eats even the tiniest bit of gluten it causes damage to the small intestine and interferes with nutrient absorption. In many cases, the inability to absorb nutrients can stunt growth, weaken bones and damage peripheral nerves resulting in neuropathy.
According to the Center for Disease Control and Prevention, approximately 29 million type 2 diabetes cases have currently been diagnosed in the United States, where another 8.1 million cases are undiagnosed. Diabetes can have various serious complications, including the development of diabetic peripheral neuropathy. The U.S. Department of Health and Human Services stated that between 60 and 70 percent of individuals diagnosed with diabetes have some form of neuropathy. Patients with diabetes often report experiencing symptoms of pain and discomfort, while other may report minor or no symptoms at all. Nerve damage can even manifest up to 10 years after being diagnosed with diabetes. blog picture of a green button with a phone receiver icon and 24h underneath Diabetic neuropathy can occur due to an extended period of elevated blood sugar levels. High, unregulated blood glucose can cause injury to the vessels that supply the body's nerves with the proper nutrition and oxygen they require to function accordingly. Over time, the nerves can become damaged, impairing the nervous system's ability to communicate effectively. The symptoms of peripheral neuropathy can vary greatly depending on the severity and extent of the nerve damage.
Neurotoxins are substances which can interfere with nerve cells by overstimulating them to death or interrupting the electrical activities of nerves and their communication process, altering the normal function of the nervous system. Common symptoms associated with the consumption of neurotoxins can manifest immediately after ingestion or they may be delayed. Symptoms include: weakness in the extremities; tingling sensations or numbness; memory loss; loss of vision and/or intellect; uncontrollable obsessive and/or compulsive behaviors; delusions; headaches; cognitive and behavioral issues; and sexual dysfunction. Also, people with certain types of disorders can be more vulnerable to these substances. Research studies have demonstrated that neurotoxins can shorten the life span of nerve cells. In addition, these substances have been associated with the development of brain disorders, peripheral neuropathy as well as neurodegenerative diseases, such as Alzheimer’s, Huntington’s Chorea and Parkinson’s disease. To make matters worse, the availability of neurotoxins has increased dramatically within the last few decades. A majority of the neurotoxins our bodies absorb are found in the food we eat and the water we drink. Even worse, these can also be found in baby food.
Over 3 million people in the United States have been diagnosed with type I diabetes. This disorder is considered an auto-immune condition where the immune system destroys the insulin producing Beta cells of the pancreas. A new case study showed how chiropractic adjustments dramatically improved a 4 year old child’s ability to manage this disorder.
A large UK study has revealed that type 1 diabetes has increased 5-fold in children less than 5 years of age between the years of 1985 and 2004. During those same years there was a doubling in children under 15 years of age being diagnosed with type I diabetes. Studies in other European countries and the US have shown similar results.
Environmental Risk Factors
The most common risk factors include exposure to environmental toxins and other stressors. The list of toxins includes pesticides, herbicides, and household cleaning agents. Additionally, food allergens such as pasteurized cow’s milk, gluten and processed soy, peanuts, & eggs are thought to be possible triggers. Low maternal and infant vitamin D3 levels and less than 6 months of breast feeding appear to be very serious risk factors as well. Birth trauma affecting the upper cervical spine has been hypothesized as a risk factor by some experts.
A recent case study published in the November 2011 edition of the Journal of Pediatric, Maternal, & Family Health documents a case of a 4 year old child, who had terrific results stabilizing her blood sugar through chiropractic care.
The child’s mother described her as being a very healthy baby, who was not vaccinated at all and was breastfed for a full 12 months. She was officially diagnosed with type I diabetes at 2 years of age. The family ate a healthy, whole food based diet and avoided processed foods and other environmental toxins.
Understanding the role of Neuroendoimmunology
The nervous, endocrine and immune system are hardwired and work together to create optimal responses for the body to adapt and heal appropriately. The new study of neuroendoimmunology looks closely at this intimate relationship between bodily systems.
Neural dysfunctions due to spinal subluxations are stressful to the body and cause abnormal changes that lead to a poorly coordinated immune response. Chiropractic adjustments have been shown to reduce subluxations and boost the coordinated responses of the nervous, endocrine, and immune systems.
The patient was diagnosed with spinal subluxations in the upper cervical region. She began chiropractic care and was seen a total of 24 times over a 2 month period. During this 2 month period, she experienced a decrease in hemoglobin A1C from 7.2% to 6.5%. She also decreased the amount of insulin used from 15 units to 11 units per day.
These results are quite remarkable because the literature states that intensive medical treatment of type I diabetes often does not succeed in lowering A1C levels under 7.0%. Chiropractic care works by optimizing the neural connections throughout the body.
This enhanced brain-body connection works to better coordinate immunity and hormone function throughout the body. This improvement in type I diabetes management is most likely a result of better cellular communication.
Peripheral neuropathy is a condition that affects the nerves outside of the brain or spinal cord. It can cause changes to sensation, movement and involuntary functions. Pressure on the nerves can cause peripheral neuropathy, as can certain conditions such as Charcot-Marie-Tooth disease, an inherited disorder. MedlinePlus, a website of the National Institutes of Health, points out that some types of peripheral neuropathy do not have a cure. The nerve damage from this condition can have lasting effects. Peripheral neuropathy affects three types of nerves: sensory, motor and autonomic. The sensory nerves relay information to the brain such as a change in temperature. When peripheral neuropathy damages the sensory nerves, patients can experience nerve pain, burning sensations or tingling. Some patients may have numbness that starts in the feet and moves up in the body. MayoClinic.com explains that with the numbness, patients can have reduced feeling in their limbs, which can affect their ability to sense changes. Problems can arise, such as in the case of a peripheral neuropathy patient who cannot feel pain in his feet and therefore does not notice a foot injury. If the injury goes untreated, an infection can develop.
What Is Metabolic Syndrome?Metabolic Syndrome is the name applied to a group of risk factors that drastically raise your risk of cardiovascular disease, stroke and diabetes. These risk factors include elevated waist circumferance (men >40 in., women > 35 in.), Elevated triglycerides, reduced HDL (good) cholesterol(men <40, women < 50), elevated blood pressure >130/85 , and elevated fasting glucose (>100mg/dL). In order to be diagnosed with metabolic syndrome, you must have 3 of any of these factors, as outlined by the American Heart Association's guidelines and the NIDH) Research Reveals: 1 Junk Food Snack, Alone, Enough To Trigger Metabolic SyndromeA recent study has found that just one high-calorie milkshake was enough to make metabolic syndrome worse for some people. And overindulgence in just a single meal or snack (especially junk food) is enough to trigger the beginnings of metabolic syndrome, which is associated with the risk of developing cardiovascular disease and diabetes.
That finding by researchers at the Microbiology and Systems Biology Group of the Netherlands Organisation for Applied Scientific Research (TNO) was reported in the online edition of the Nov. 2015 issue of The FASEB Journal.
For some people, “acute effects of diet are mostly small, but may have large consequences in the long run,” said TNO researcher Suzan Wopereis, Ph.D., senior author of the report.
The researchers gave male volunteers in two groups a high-fat milkshake consisting of 1.6 g protein, 16 g fat, and 3.2 g carbohydrates.
The first group included 10 healthy male volunteers. They were also given a snack diet consisting of an additional 1300 kcal per day, in the form of sweets and savory products such as candy bars, tarts, peanuts, and crisps for four weeks.
The second group included nine volunteers with metabolic syndrome and who had a combination of two or more risk factors for heart disease, such as unhealthy cholesterol levels, high blood pressure, high blood sugar, high blood lipids, and abdominal fat. Shocking Test Results Both groups had blood samples taken, before and after the snacks. In these blood samples, the researchers measured 61 biomarkers, such as cholesterol and blood sugar.
For the subjects with metabolic syndrome, the blood tests showed that biochemical processes related to sugar metabolism, fat metabolism, and inflammation were abnormal. This came as no surprise considering these test subjects already had metabolic syndrome.
What was shocking were the findings for the group of healthy men. For the 10 healthy male volunteers, the blood tests showed that signaling molecules controlling sugar and fat metabolism were changed and levels of inflammation were significantly elevated. These findings resemble the start of negative health effects similar to those found at the start of metabolic disease.
“Eating junk food is one of those situations where our brains say ‘yes’ and our bodies say ‘no,’” said Gerald Weissmann, M.D., Editor-in-Chief of The FASEB Journal. “Unfortunately for us, this report shows that we need to use our brains and listen to our bodies. Even one unhealthy snack has negative consequences that extend far beyond any pleasure it brings.”nervedoctor.info
Via Wildcat2030, Dr. John Coppola
|
Neuropathy is a medical term used to describe a collection of general diseases or malfunctions which affect the nerves. The causes of neuropathy, or nerve damage, can vary greatly among each individual and these may be caused by a number of different diseases, injuries, infections and even vitamin deficiency states. However, neuropathy can most commonly affect the nerves that control the motor and sensory nerves. Because the human body is composed of many different kinds of nerves which perform different functions, nerve damage is classified into several types. Neuropathy can also be classified according to the location of the nerves being affected and according to the disease causing it. For instance, neuropathy caused by diabetes is called diabetic neuropathy. Furthermore, depending on which nerves are affected will depend on the symptoms that will manifest as a result. Below we will discuss several specific types of neuropathies clinically treated by chiropractors, physical therapists and physical medicine doctors alike, as well as briefly describing their causes and their symptoms.
The vast array of symptoms caused by neuropathy, also known as peripheral neuropathy, reflect the fact that it may be caused by an equally broad range of ailments involving disease and damage to peripheral nerves. Signs and Symptoms of Neuropathy Depending on the reason and unique to each patient, signs and symptoms of neuropathy can include: pain; tingling, burning or prickling sensations; increased sensitivity to touch; muscle weakness or wasting; temporary or permanent numbness; paralysis; dysfunction in glands or organs; or impairment in urination and sexual functioning. Such signs and symptoms are dependent on whether autonomic, sensory, or motor nerves, as well as a combination of them, are ultimately affected. Autonomic nerve damage can influence physiological functions like blood pressure or create gastrointestinal problems and issues. Damage or dysfunction in the sensory nerves may impact sensations and sense of equilibrium or balance, while harm to motor nerves may affect movement and reflexes. When both sensory and motor nerves are involved, the condition is known as sensorimotor polyneuropathy.
Muscle Fasciculations: Key indexing terms: - Fasciculation
- muscular
- Gluten
- Celiac disease
- Chiropractic
- Food hypersensitivity
Abstract
Objective: The purpose of this case report is to describe a patient with chronic, multisite muscle fasciculations who presented to a chiropractic teaching clinic and was treated with dietary modifications. Clinical features: A 28-year-old man had muscle fasciculations of 2 years. The fasciculations began in his eye and progressed to the lips and lower extremities. In addition, he had gastrointestinal distress and fatigue. The patient was previously diagnosed as having wheat allergy at the age of 24 but was not compliant with a gluten-free diet at that time. Food sensitivity testing revealed immunoglobulin G–based sensitivity to multiple foods, including many different grains and dairy products. The working diagnosis was gluten neuropathy. Intervention and outcome: Within 6 months of complying with dietary restrictions based on the sensitivity testing, the patient’s muscle fasciculations completely resolved. The other complaints of brain fog, fatigue, and gastrointestinal distress also improved. Conclusions: This report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary changes. There is strong suspicion that this case represents one of gluten neuropathy, although testing for celiac disease specifically was not performed. Introduction: Muscle FasciculationsThere are 3 known types of negative reactions to wheat proteins, collectively known as wheat protein reactivity: wheat allergy (WA), gluten sensitivity (GS), and celiac disease (CD). Of the 3, only CD is known to involve autoimmune reactivity, generation of antibodies, and intestinal mucosal damage. Wheat allergy involves the release of histamine by way of immunoglobulin (Ig) E cross-linking with gluten peptides and presents within hours after ingestion of wheat proteins. Gluten sensitivity is considered to be a diagnosis of exclusion; sufferers improve symptomatically with a gluten-free diet (GFD) but do not express antibodies or IgE reactivity.1 The reported prevalence of WA is variable. Prevalence ranges from 0.4% to 9% of the population.2,3 The prevalence of GS is somewhat difficult to determine, as it does not have a standard definition and is a diagnosis of exclusion. Gluten sensitivity prevalence of 0.55% is based on National Health and Nutrition Examination Survey data from 2009 to 2010.4 In a 2011 study, a GS prevalence of 10% was reported in the US population.5 In contrast to the above 2 examples, CD is well defined. A 2012 study examining serum samples from 7798 patients in the National Health and Nutrition Examination Survey database from 2009 to 2010 found an overall prevalence of 0.71% in the United States.6 Neurologic manifestations associated with negative reactions to wheat proteins have been well documented. As early as 1908, “peripheral neuritis” was thought to be associated with CD.7 A review of all published studies on this topic from 1964 to 2000 indicated that the most common neurologic manifestations associated with GS were ataxia (35%), peripheral neuropathy (35%), and myopathy (16%). 8 Headaches, paresthesia, hyporeflexia, weakness, and vibratory sense reduction were reported to be more prevalent in CD patients vs controls.9 These same symptoms were more prevalent in CD patients who did not strictly follow a GFD vs those who were compliant with GFD. At present, there are no case reports describing the chiropractic management of patient with gluten neuropathy. Therefore, the purpose of this case study is to describe a patient presentation of suspected gluten neuropathy and a treatment protocol using dietary modifications. Case ReportA 28-year-old man presented to a chiropractic teaching clinic with complaints of constant muscle fasciculations of 2 years’ duration. The muscle fasciculations originally started in the left eye and remained there for about 6 months. The patient then noticed that the fasciculations began to move to other areas of his body. They first moved into the right eye, followed by the lips, and then to the calves, quadriceps, and gluteus muscles. The twitching would sometimes occur in a single muscle or may involve all of the above muscles simultaneously. Along with the twitches, he reports a constant “buzzing” or “crawling” feeling in his legs. There was no point during the day or night when the twitches ceased. The patient originally attributed the muscle twitching to caffeine intake (20 oz of coffee a day) and stress from school. The patient denies the use of illicit drugs, tobacco, or any prescription medication but does drink alcohol (mainly beer) in moderation. The patient ate a diet high in meats, fruits, vegetables, and pasta. Eight months after the initial fasciculations began, the patient began to experience gastrointestinal (GI) distress. Symptoms included constipation and bloating after meals. He also began to experience what he describes as “brain fog,” a lack of concentration, and a general feeling of fatigue. The patient noticed that when the muscle fasciculations were at their worst, his GI symptoms correspondingly worsened. At this point, the patient put himself on a strict GFD; and within 2 months, the symptoms began to alleviate but never completely ceased. The GI symptoms improved, but he still experienced bloating. The patient’s diet consisted mostly of meats, fruit, vegetables, gluten-free grains, eggs, and dairy. At the age of 24, the patient was diagnosed with WA after seeing his physician for allergies. Serum testing revealed elevated IgE antibodies against wheat, and the patient was advised to adhere to a strict GFD. The patient admits to not following a GFD until his fasciculations peaked in December 2011. In July of 2012, blood work was evaluated for levels of creatine kinase, creatine kinase–MB, and lactate dehydrogenase to investigate possible muscle breakdown. All values were within normal limits. In September of 2012, the patient under- went food allergy testing once again (US Biotek, Seattle, WA). Severely elevated IgG antibody levels were found against cow’s milk, whey, chicken egg white, duck egg white, chicken egg yolk, duck egg yolk, barley, wheat gliadin, wheat gluten, rye, spelt, and whole wheat (Table 1). Given the results of the food allergy panel, the patient was recommended to remove this list of foods from his diet. Within 6 months of complying with the dietary changes, the patient’s muscle fasciculations completely resolved. The patient also experienced much less GI distress, fatigue, and lack of concentration. DiscussionThe authors could not find any published case studies related to a presentation such as the one described here. We believe this is a unique presentation of wheat protein reactivity and thereby represents a contribution to the body of knowledge in this field. This case illustrates an unusual presentation of a widespread sensorimotor neuropathy that seemed to respond to dietary changes. Although this presentation is consistent with gluten neuropathy, a diagnosis of CD was not investigated. Given the patient had both GI and neurologic symptoms, the likelihood of gluten neuropathy is very high. There are 3 forms of wheat protein reactivity. Because there was confirmation of WA and GS, it was decided that testing for CD was unnecessary. The treatment for all 3 forms is identical: GFD. The pathophysiology of gluten neuropathy is a topic that needs further investigation. Most authors agree it involves an immunologic mechanism, possibly a direct or indirect neurotoxic effect of antigliadin anti- bodies. 9,10 Briani et al 11 found antibodies against ganglionic and/or muscle acetylcholine receptors in 6 of 70 CD patients. Alaedini et al12 found anti-ganglioside antibody positivity in 6 of 27 CD patients and proposed that the presence of these antibodies may be linked to gluten neuropathy. It should also be noted that both dairy and eggs showed high responses on the food sensitivity panel. After reviewing the literature, no studies could be located linking either food with neuromuscular symp- toms consistent with the ones presented here. There- fore, it is unlikely that a food other than gluten was responsible for the muscle fasciculations described in this case. The other symptoms described (fatigue, brain fog, GI distress) certainly may be associated with any number of food allergies/sensitivities. LimitationsOne limitation in this case is the failure to confirm CD. All symptoms and responses to dietary change point to this as a likely possibility, but we cannot confirm this diagnosis. It is also possible that the symptomatic response was not due directly to dietary change but some other unknown variable. Sensitivity to foods other than gluten was documented, including reactions to dairy and eggs. These food sensitivities may have contributed to some of the symptoms present in this case. As is the nature of case reports, these results cannot necessarily be generalized to other patients with similar symptoms. Conclusion: Muscle FasciculationsThis report describes improvement in chronic, widespread muscle fasciculations and various other systemic symptoms with dietary change. There is strong suspicion that this case represents one of gluten neuropathy, although testing for CD specifically was not performed. Brian Anderson DC, CCN, MPHa,⁎, Adam Pitsinger DC Attending Clinician, National University of Health Sciences, Lombard, IL Chiropractor, Private Practice, Polaris, OH AcknowledgmentThis case report is submitted as partial fulfillment of the requirements for the degree of Master of Science in Advanced Clinical Practice in the Lincoln College of Post-professional, Graduate, and Continuing Education at the National University of Health Sciences. Funding Sources and Conflicts of InterestNo funding sources or conflicts of interest were reported for this study. References:
1. Sapone A, Bai J, Ciacci C, et al. Spectrum of gluten-related
disorders: consensus on new nomenclature and classification.
BMC Med 2012;10:13.
2. Matricardi PM, Bockelbrink A, Beyer K, et al. Primary versus
secondary immunoglobulin E sensitization to soy and wheat in
the Multi-Centre Allergy Study cohort. Clin Exp Allergy
2008;38:493–500.
3. Vierk KA, Koehler KM, Fein SB, Street DA. Prevalence of
self-reported food allergy in American adults and use of food
labels. J Allergy Clin Immunol 2007;119:1504–10.
4. DiGiacomo DV. Prevalence and characteristics of non-celiac
gluten sensitivity in the United States: results from the
continuous National Health and Nutrition Examination Survey
2009-2010. Presented at: the 2012 American College of
Gastroenterology Annual Scientific Meeting; Oct. 19-24, Las
Vegas.; 2012.
5. Sapone A, Lammers KM, Casolaro V. Divergence of gut
permeability and mucosal immune gene expression in two
gluten-associated conditions: celiac disease and gluten sensitivity.
BMC Med 2011;9:23.
6. Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA,
Everhart JE. The prevalence of celiac disease in the United
States. Am J Gastroenterol 2012 Oct;107(10):1538–44.
7. Hadjivassiliou M, Grunewald RA, Davies-Jones GAB. Gluten
sensitivity as a neurological illness. J Neurol Neurosurg
Psychiatr 2002;72:560–3.
8. Hadjivassiliou M, Chattopadhyay A, Grunewald R, et al.
Myopathy associated with gluten sensitivity. Muscle Nerve
2007;35:443–50.
9. Cicarelli G, Della Rocca G, Amboni C, et al. Clinical and
neurological abnormalities in adult celiac disease. Neurol Sci
2003;24:311–7.
10. Hadjivassiliou M, Grunewald RA, Kandler RH. Neuropathy
associated with gluten sensitivity. J Neurol Neurosurg
Psychiatry 2006;77:1262–6.
11. Briani C, Doria A, Ruggero S, et al. Antibodies to muscle and
ganglionic acetylcholine receptors in celiac disease. Autoimmunity
2008;41(1):100–4.
12. Alaedini A, Green PH, Sander HW, et al. Ganglioside reactive
antibodies in the neuropathy associated with celiac disease.
J Neuroimmunol 2002;127(1–2):145–8.
Here’s yet another reason to get off the couch: Inactivity is associated with greater risk of prediabetes, even for healthy-weight adults, a new study finds. University of Florida researchers said the finding may help explain why up to one-third of slim American adults have prediabetes — elevated blood sugar but not full-blown diabetes.
“We have found that a lot of people who we would consider to be at healthy weight — they’re not overweight or obese — are not metabolically healthy,” said lead investigator Arch Mainous III. He’s chair of health services research, management and policy in the university’s College of Public Health and Health Professions.
Mainous and his colleagues analyzed data from more than 1,000 people, aged 20 and older, in England. All had a healthy weight and no diagnosis of diabetes. Those with an inactive lifestyle were more likely than active people to have a blood sugar level of 5.7 or above, which the American Diabetes Association considers prediabetes. About one-quarter of all inactive people and more than 40 percent of inactive people 45 and older met the criteria for prediabetes or diabetes, according to the study.
Interesting Facts About Peripheral Neuropathy That You Need To Know
Almost everyone is well aware of what peripheral neuropathy means as well as its symptoms. However, many people will be surprised to know that tingling sensation, numbness and pain aren’t the only symptoms experienced by people with peripheral neuropathy. The symptoms of this condition are subjective to the type of nerve that is being affected. The three main types of nerves include motor, sensory and autonomic nerve; each having its own symptoms.
People diagnosed with diabetes must be very careful when it comes to taking all the necessary precautions of peripheral neuropathy. According to top researches, estimates of 70 percent of diabetic patients tend to develop one or more symptoms of neuropathy. While some of the medications may help improve the condition of neuropathy, many medications have the tendency to worsen the situation. Moreover, medications to treat other diseases like cancer are likely to cause nerve damage that leads to peripheral neuropathy.
It is essential for people with this condition to not take the simple symptoms like numbness lightly as it can cause some serious problems with time. For example, if you are feeling a sensation of numbness on your feet then you will not realize it if you even step on a broken glass. For this reason, you must never ignore even the simplest of the symptoms as it can lead to severe results. You must visit http://www.neuropathycure.org for more details.
Unfortunately, there is no treatment of peripheral neuropathy that can completely diminish the matter. The treatments of medication and therapy can only contain the symptoms as well as improve the condition so that the individual suffering can be relived from intense pain and agitation. For this reason, you must not get your hopes up with the prescribed medical treatment.
THE FOUR BIG MYTHS ABOUT NEUROPATHY
Can you recall the first time you were told you might suffer from neuropathy?
Chances are unless you already knew someone who suffered from neuropathy – you didn’t know much about the condition. You’ve likely learned quite a bit about the condition since then – but you no doubt came across false or misleading information along the way.
The truth is, there are still a lot of misleading rumors and false information about neuropathy out there. In fact – you may be surprised to learn that some of the information you’ve picked up over the years may not be completely true.
I’ve encountered a number of half-truths and misleading facts over the years. While some are harmless, others can send you down the wrong path or prevent you from getting the best treatment for your nerve damage. To help dispel these myths, I’ve put together a list of four half-truths, misleading rumors, and other misconceptions about neuropathy that a lot of people still believe.
MYTH #1 – NERVE DAMAGE IS IRREVERSIBLE:
You may have been told at some point that your nerve damage is irreversible. The truth is, it largely depends on the cause and severity of your nerve damage. No one case is the same – but for many people, their nerve damage can in fact be slowed and even reversed. This is especially true for those suffering from diabetic neuropathy or nerve damage resulting from a vitamin B12 deficiency.
For those with diabetic neuropathy, managing blood sugar is the single most effective step one can take to both slow and reverse nerve damage. For those whose neuropathy was a result of a vitamin B12 deficiency, replenishing the body’s B12 reserves can both repair and regenerate damaged nerves.
Of course, those with diabetic neuropathy or a B12 deficiency aren’t the only ones who can hold on to the hope of reversing their nerve damage. With the right treatment, I’ve seen individuals with various different causes of their neuropathy experience nerve regeneration and a reduction (and even elimination) of their symptoms.
MYTH #2 – ONLY PEOPLE WITH DIABETES DEVELOP NEUROPATHY
While it’s true that around 70% of people with diabetes will also develop neuropathy, it isn’t the only cause of nerve damage. There are a number of other causes, affecting people from all walks of life. A list of known causes of neuropathy include:
- Vitamin B12 deficiency
- Chemotherapy
- Medications (see list of 65 medications that can cause neuropathy)
- Surgery
- Alcohol Consumption
- Exposure to Toxins
- Infections
- Autoimmune Diseases
- Trauma
- Repeated Pressure on Nerves
- Kidney Disorders
- Inherited Disorders
MORE: The Ultimate Cheat Sheet to Neuropathy Causes & Treatments
MYTH #3 – PRESCRIPTION MEDICATIONS CURE NEUROPATHY
There is no prescription medication on the market that “cures” neuropathy. In fact, many of the neuropathy drugs on the market today were originally intended for other medical conditions, such as epilepsy.
Rather than cure neuropathy, the prescription drugs on the market today are designed to mask the pain. They act as a volume knob, temporarily turning down the pain levels – but eventually wearing off. As such, the user never gets permanent, lasting relief.
Not only that, but some independent studies have shown most of the common neuropathy prescriptions on the market today to be “largely ineffective”. In one study published by the Cochrane Library in 2015, researchers found that only 1 in 10 patients taking anti-seizure medications for nerve pain experienced a reduction in pain. And of the 10% that did have a reduction in pain, the reduction was minimal.
More: Researchers: “Popular drugs for nerve pain are ineffective”
MYTH #4 – TINGLING, NUMBNESS AND SHOOTING PAINS ARE THE ONLY SYMPTOMS OF NEUROPATHY
While these are the most common symptoms associated with neuropathy, there are many other problems that can manifest themselves if you’re suffering from nerve damage. Depending on the type of nerves that have been damaged, your symptoms could range from tingling sensations in the hands or feet to heartburn or indigestion.
Your peripheral nervous system has three types of nerves: sensory, motor, and autonomic. Each has a different function and the symptoms of your nerve damage will vary depending on which of these nerve types was damaged. In some cases only one type of nerve may be damaged, while in others multiple nerve types may have been compromised.
Common Symptoms of Nerve Damage (based on nerve type):
Sensory:
- Pins and needle-like pain (sharp, painful sensations)
- Tingling or numbness
- Extreme sensitivity to touch
Motor:
- Loss of balance
- Muscle weakness
- Loss of muscle control (i.e. difficulty gripping things, difficulty walking)
- Cramps or twitching
Autonomic:
- Dizziness when standing
- Abnormal heart rate
- Shortness of breath
- Excessive sweating
- Lack of sweat
- Digestive problems
- Bladder problems
- Vision Problems
While there are many other myths and misleading facts floating around out there – these are four of the ones I’ve encountered most often in my years helping people suffering from neuropathy. Some of them can be more harmful than others – depriving the person that has fallen for them of the real information that could make a difference in their life.
What myths or misleading information have you been told over the years – only to discover the truth later on?
Inning accordance with Mayo clinic discomfort research has resulted in discoveries that alpha lipoic acid may operate in relieving uncomfortable symptoms. Much can be done to ease the symptoms of diabetic neuropathy and avoid further damage.
EXACTLY WHAT IS ALPHA LIPOIC ACID?
It’s a naturally occurring fatty acid in our bodies. It’s likewise known as lipoic acid, thioctic acid or abbreviated as ALA however shouldn’t be puzzled with alpha linolenic acid.
Alpha lipoic acid is found in a lot of foods especially in animal internal organs such as the liver, heart and kidney. Due to the fact that it is covalently bound, the naturally happening type is not readily available so that extracting it from natural sources yields poor outcomes.
The chemical structure of alpha lipoic acid shows 2 thiol or sulfur groups. When lowered the result is called dihydrolipoic acid and when in an oxidized type alpha lipoic acid.
FUNCTIONS OF ALPHA LIPOIC ACID IN THE BODY
It is a fat and as such it is used by the body to produce energy for the body’s functions. It transforms glucose into energy.
It is one potent antioxidant. This particular is significant in neuropathy. It’s both water and fat soluble if compared to the majority of antioxidants. Being so, it quickly permeates nerve cells and secures the integrity of nerve cells from oxidative damage. It scavengers for radicals and secures the integrity of the afferent neuron. Another one of its considerable function is its capability to renew vitamin C and glutathione when these antioxidants remain in low supply. Glutathione is another vital anti-oxidant that eliminates hazardous toxins. They cooperate together to safeguard the harmful impacts of complimentary radicals and protect the integrity of cells from oxidative damage.
RESEARCH ON ALPHA LIPOIC ACID AND NEUROPATHY
Initial studies suggest that it might assist in diabetic neuropathy. In one of the biggest research studies, 181 people took 600 mg, 1200 mg or 1800 mg of alpha lipoic acid or a placebo. After 5 weeks, those who took in the supplement have actually shown enhanced signs. A 600 mg daily dose was best endured which likewise provided the finest advantages.
Research carried out by the Linus Pauling Institute has actually shown the following evidence relating to the function of alpha lipoic acid in diabetes and in diabetic neuropathy:
· improves glucose usage in type 2 Diabetes mellitus by boosting insulin sensitivity. The result of 3 various research studies as reported by the institute suggested that the optimum reliable dose is 600 mg/ day. The R-isomer of ALA may be more reliable in enhancing insulin sensitivity than the L-isomer.
· by some mechanism it increases glucose uptake in fat and muscle cells
· enhances the function and conduction of neurons in diabetes
· A neuropathic complication defined by lowered heart rate variability was “considerably enhanced” by treatment of 800 mg daily of the racemic kind.
· Beneficial effects are related primarily to its antioxidant homes. As an antioxidant, alpha lipoic acid scavenges reactive oxygen and nitrogen species that can cause damage to DNA, proteins and lipids in cell membranes. Alpha lipoic acid and dihydrolipoic acid likewise hinder copper and iron moderated oxidative damage.
· may help in diabetic end-stage renal illness on hemodialysis.
· Research study show a considerable enhancement in electrophysiological tests of nerve conduction after 2 years of treatment with 1200/mg or 600/mg than those on placebo.
· Apart from its helpful role in diabetes, it helps in metabolic syndrome, halts Alzheimer’s development and age-related cognitive dysfunction and lots of others.
RECOMMENDED ALPHA LIPOIC ACID DOSE
As you age the capacity of your body to produce alpha lipoic acid reduces and you can gain from its numerous benefits.
The Linus Pauling institute suggests the R-isomer of 200-400 mg daily for healthy individuals.
For diabetic neuropathy, the optimum recommended dose is 600 – 1,800 mg/ day of the R-isomer.
For cardiovascular autonomic neuropathy a suggested oral dosage of 800/day of the R-isomer likewise is suggested.
BOTTOM LINE
If you decide to supplement your anti-diabetic medication with alpha lipoic acid in the hope of treating your diabetic neuropathy ask your physicians’ suggestion specifically if you are taking other medications to lower blood sugar levels.
This antioxidant can assist in your diabetes management. However, it’s essential to remember that management of diabetes is a lifelong dedication. Keep in mind of your diet, workout day-to-day and monitor your blood sugar levels regularly. Take your anti-diabetic medications or insulin as directed by your doctor.
Once they have actually begun, diligently observing these things can prevent complications and stop them in their tracks.
The chemical structure of alpha lipoic acid shows 2 thiol or sulfur groups. When decreased the outcome is called dihydrolipoic acid and when in an oxidized type alpha lipoic acid. In one of the biggest research studies, 181 individuals took 600 mg, 1200 mg or 1800 mg of alpha lipoic acid or a placebo. As an antioxidant, alpha lipoic acid scavenges reactive oxygen and nitrogen species that can cause damage to DNA, proteins and lipids in cell membranes. Alpha lipoic acid and dihydrolipoic acid also inhibit copper and iron mediated oxidative damage.
You have actually been feeling that tingling at your toes for more than a couple of weeks now. At night, a sharp jabbing discomfort at your feet wakes you up. You have trouble in strolling due to discomfort.
Peripheral Neuritis (pronounced/ new.righ’t is/).
Peripheral neuritis is the most common type of neuropathy (pronounced/ new.rop’ uth-ee/) occurring among diabetics. It affects your toes, feet and later your arms and hands. As you lose your capacity to feel any pain in your extremities serious problems set in.
The manifestations of other types of neuropathy depend upon what types of nerves are impacted. Apart from peripheral neuritis other types of diabetic neuropathy are autonomic (pronounced/ aw” tuh.nom’ ick/) neuropathy, radiculoplexus (pronounced/ ra.dick” yoo.lo.pleck’ sus/) neuropathy and mononeuropathy (noticable/ mon” o-new. rop’ uth-ee/).
AUTONOMIC NEUROPATHY
Autonomic neuropathy affects the nerves controlling the functions of your body organs. Your free nerve system is responsible in the functioning of your heart, lungs, stomach, intestines, sex organs, bladder and eyes. When the nerves of your bladder are impacted you’ll experience urinary incontinence. On the other hand, when your stomach nerves are included you’ll feel sluggish stomach clearing described as gastroparesis with queasiness, loss of cravings and throwing up. Irregularity or unchecked diarrhea can also be symptoms.
When the nerves of sex organs are included, males suffer impotence while women sexual troubles.
The nerves of your heart can be impacted too and your body will have trouble in getting used to high blood pressure and heart rate. You’ll feel a quick heart rate at rest. You’ll go through an unexpected drop in blood pressure from a sitting to a standing position that can cause faintness or lightheadedness.
If your eye nerves are impacted, you’ll have difficulty adjusting from light to dark. Dangerously, your body may not identify low blood sugar levels.
RADICULOPLEXUS NEUROPATHY
Radiculoplexus neuropathy is likewise called as diabetic amyotrophy (pronounced/ am” eye.ot’ ruh.fee/), femoral neuropathy or proximal neuropathy. It affects the nerves in your thighs, butts, hips or legs. The signs appear all of a sudden and seriously. The muscles affected become weak then atrophy and you’ll have to struggle increasing from a sitting position. , if your abdomen is impacted swelling happens.. Gradually, weight reduction ensues.
MONONEUROPATHY
Other signs consist of pain in your foot, shin and front of thigh; trouble focusing your eyes, double vision and discomfort behind your eye; chest or abdominal pain. Compression neuropathy can take place such as in carpal tunnel syndrome.
WHY NEUROPATHY OCCURS
Diabetic neuropathy gradually occurs from years of uncontrolled blood sugar level levels that damage the nerves. Sometimes, cigarette smoking and alcohol abuse add to the advancement of neuropathy. Medical professionals say a hereditary personality is to blame and in some cases the cause is totally unidentified.
MANAGEMENT OF NEUROPATHY
Inning accordance with the Mayo clinic the goals in the management of neuropathy is to slow the development of the condition, to ease pain, manage other issues that might occur and to restore the function of the body location impacted.
The best way to slow development is to tighten control of your blood sugar levels. Display your blood sugar level levels daily. Your blood glucose levels should be in between 70- 130 mg/dl prior to meals and no less that 180 mg/dl two hours after meals. Undergo Hemoglobin A1C screening every three months and your values should not be more than 7 percent.
Take your anti-diabetic medications as prescribed by your health care supplier. Couple this with the best diet, workout and healthy way of life habits.
To relieve discomfort, your physician will recommend medications such as anti-seizure medication, anti-depressants, topical anesthetics or opioids which have actually been revealed to work well.
Antispasmodics can ease incontinence. Taking in smaller sized but regular meals can ease gastrointestinal problems. The occurrence of low blood pressure on standing can be avoided by standing gradually and drinking additional fluids.
Medications can bring back functions of organs such as in erectile dysfunction. When they aren’t reliable guys can resort to vacuuming. In females, lubrications can assist.
Alternative Treatment.
Alternative treatments work well too such as transcutaneous electrical nerve acupuncture, stimulation and biofeedback. Scientific research studies had shown that they can assist in reducing signs and slowing the progress of neuropathy.
The best method to prevent diabetic neuropathy is to keep typical blood glucose levels daily. Continue your diabetic medications or insulin as advised by your physician, pay attention to your diet plan, weave in exercise in your day-to-day regimen and maintain healthy way of life practices.
The symptoms of other types of neuropathy depend upon exactly what types of nerves are affected. Apart from peripheral neuritis other types of diabetic neuropathy are free (pronounced/ aw” tuh.nom’ ick/) neuropathy, radiculoplexus (noticable/ ra.dick” yoo.lo.pleck’ sus/) neuropathy and mononeuropathy (noticable/ mon” o-new. Autonomic neuropathy impacts the nerves controlling the functions of your body organs. Radiculoplexus neuropathy is likewise called as diabetic amyotrophy (pronounced/ am” eye.ot’ ruh.fee/), femoral neuropathy or proximal neuropathy. Diabetic neuropathy gradually ensues from years of unchecked blood sugar levels that ruin the nerves.
Exactly what you might not understand is that there are nutritional supplements and vitamins you can take to assist control your blood sugar. And numerous of these supplements go to the website can also assist with the impacts of diabetic neuropathy – one of the chief factors to amputations in diabetic clients.
The number of medical studies that reveal adding crucial nutrients to the health care routines of diabetic neuropathy patients is growing continuously.
Given, these dietary supplements will not fill in correct diet, controlling your blood glucose and a sound exercise strategy, but they can certainly improve the efficiency of all of these pieces of the diabetic neuropathy puzzle.
WHAT YOU MUST LOOK FOR IN NUTRITIONAL SUPPLEMENTS
As a client with diabetic neuropathy, your requirements in nutritional supplements are various than those of other people. While lots of companies utilize the convenience of their once-a-day multivitamin as a selling point, a tablet you take only when a day is only going to be truly effective for the 2 hours after take it. You need more than that for the signs of your diabetic neuropathy.
To get the complete impact for treating your diabetic neuropathy, you have to preserve a stable healing level of these vitamins and nutrients throughout the day to assist keep your blood sugar under control.
Pick supplements that you take at last three times a day to keep the levels consistent in your blood stream.
And look for dietary supplements that come from an FDA authorized producer to make sure that what you’re taking is pharmaceutical grade.
WHICH VITAMIN SUPPLEMENTS YOU SHOULD TAKE
There is a lot information on the marketplace now about nutritional supplements and vitamins. Do not go out there and purchase vitamins without being prepared. Do your research study and talk to a professional like your favorite clinician to make sure you’re taking the ideal vitamins for your specific diabetic neuropathy signs. We have a very particular protocol in our centers.
Here’s a fast cheat sheet of the Top 12 vitamins and nutrients for diabetic neuropathy treatment to assist you determine a few of the important supplements that can assist your diabetic neuropathy and exactly what they do:
Thiamin (Vitamin B1) – assists preserve healthy oxygen levels in the blood stream which suggests that you less possibility of nerve damage due to bad oxygen levels reaching the nerves. The Recommended Daily Allowance (RDA) of thiamine for the average individual is 1.0 to 2.4 mg per day however diabetic neuropathy patients need to take in the series of 60 mg daily in equally divided dosages.
Riboflavin (Vitamin B2) – works in mix with Vitamin B6 to help your body use glucose effectively. The RDA is 1.2 to 1.6 mg each day however restorative levels need to be around 60 mg each day.
Vitamin B6 – in addition to folic acid and B12, it helps avoid nerve damage and heart attacks. It can likewise help avoid diabetic blindness and/or vision loss. Restorative levels should be at least 60 mg each day but be extremely mindful with your dosage. Some toxicity has actually been reported with incredibly high levels of B6.
Vitamin B12 – works with folic acid to assist prevent stroke and loss of limbs due to diabetic neuropathy. It likewise helps ease neuropathy pain.
Biotin – when taken in mix with chromium, biotin (a B vitamin) assists insulin work better, keeps the pancreas working well, and decreases blood sugar levels.
Chromium – when taken with biotin, assists insulin work better, keeps the pancreas working well and reduces blood sugar level levels.
Copper – helps secure the cells in the pancreas that make insulin healthy, helps avoid diabetes related damage to capillary and nerves and lowers blood glucose levels.
Folic Acid – deal with B12 to help avoid strokes and loss of limbs due to diabetic neuropathy.
Magnesium – helps alleviate diabetic neuropathy discomfort and helps insulin work more successfully.
Manganese – helps avoid damage to capillary and nerves.
Selenium – in some cases called an insulin copy cat, selenium helps take blood sugar level into the cells. Selenium protects versus capillary and nerve damage from elevated blood sugar level levels, two of the contributing consider diabetic neuropathy.
Zinc – assists blood glucose enter the cells and insulin work more efficiently.
These supplements, when utilized effectively and under the care and supervision of your very own clinician, can help enhance your diabetic neuropathy signs and reduce the opportunities of permanent nerve damage and eventual amputation.
TAKE NOTE – THESE SUPPLEMENTS WILL NOT TAKE THE PLACE OF CONSUMING PROPERLY & EXERCISING
They operate in mix with a healthier lifestyle, not in location of it.
And never ever self prescribe vitamins supplements and nutrients. Deal with your clinician to get here at the levels you need for your particular diabetic neuropathy and blood glucose control concerns. As with numerous other things, too much of an excellent thing can do more damage than good if not appropriately managed and monitored by a specialist.
And never ever self recommend vitamins supplements and nutrients. Work with you NeuropathyDR ® clinician to reach the levels you require for your specific diabetic neuropathy and blood sugar control problems. Just like lots of other things, too much of a good thing can do more harm than great if not effectively regulated and monitored by an expert.
Exactly what you might not realize is that there are dietary supplements and vitamins you can take to assist manage your blood sugar. And many of these supplements can also assist with the results of diabetic neuropathy – one of the chief contributors to amputations in diabetic patients.
Vitamin B6 – along with folic acid and B12, it assists avoid nerve damage and heart attacks. It can likewise help prevent diabetic loss of sight and/or vision loss. Work with your clinician to get here at the levels you need for your particular diabetic neuropathy and blood sugar control problems.
Peripheral neuropathy may be more common in patients with pre-diabetes than previously thought, and early interventions may be warranted in this patient population, according to researchers from the University of Utah. Currently, 86 million adults — more than one in three U.S. adults — have prediabetes, according to CDC estimates. Without weight loss and moderate physical activity, 15% to 30% of these people will develop full-blown type 2 diabetes within 5 years.1 “We know now a lot more than we did 3 or 5 years ago about neuropathic pain in patients with prediabetes. Neuropathy affects patients with prediabetes in a continuum,” said J. Rob Singleton, MD, who is a professor of neurology at the University of Utah in Salt Lake City. “We think it is more obesity and dysfunction of lipids (fats) that is causing the problem.”
For many families, type 2 diabetes can develop in several members of the household. For some people, diabetes has been diagnosed throughout previous generations of family members. However, does this mean, you are bound to inherit the condition? Over a period of 25 years, according to statistics, the number of people in the world who are diagnosed with type 2 diabetes has increased from 35 million to 240 million. Moreover, these statistics don't take into account the number of individuals with undiagnosed diabetes. Many families have the relevant concern regarding whether they or future generations could genetically develop type 2 diabetes. While the magnitude of cases is quite significant, the reality is that the widespread issue of diabetes couldn't have simply occurred through genetic or inherited means in such a short time span. If genetic alteration is not the reason behind the dramatic increase in type 2 diabetes cases, then why has the condition been on the rise over the past few decades? As a matter of fact, diabetes is a condition that is almost entirely caused by environmental and lifestyle factors. Our genetic code itself may not be altered through these circumstances but our environment as well as stress and improper nutrition and fitness habits can influence the way those genes are expressed. Predisposed genes can certainly contribute to the development of diabetes, however, if you are not exposed to these environmental and lifestyle triggers, the diabetes gene may never fully develop.
Peripheral neuropathy is a condition which occurs due to nerve damage in the arms, legs, hands and feet. Common symptoms include pain, tingling and burning sensations and numbness. This type of neuropathy can be caused by a variety of factors, such as diabetes, chemotherapy, statin medications, disc herniation and trauma from an injury, toxic metal exposure, chronic alcohol consumption and vitamin deficiencies. Recent research studies, however, have associated peripheral nerve damage to gluten sensitivity and celiac disease. Celiac disease is an autoimmune disorder that generally affects the individual's digestive tract. When a person with celiac disease consumes gluten, it can cause damage to the small intestine, interfering with the body's natural nutrient absorption function. In a majority of cases, this inability to properly absorb nutrients can alter growth, weaken bones and even damage peripheral nerves, leading to neuropathy.
Peripheral neuropathy most commonly develops in patients who've been previously diagnosed with pre-diabetes. According to researchers from the University of Utah, early interventions can allow people to maintain their overall health and wellness. Further research studies have revealed that peripheral nerve damage begins with pre-diabetes and obesity. Approximately more than one in three adults in the United States, about 86 million people, have pre-diabetes. Without the proper body weight and moderate physical activity, 15 to 30 percent of these individuals could develop type 2 diabetes within 5 years. "We now know a lot more than we did 3 to 5 years ago about neuropathic pain in patients with pre-diabetes. Neuropathy affects patients with pre-diabetes in a continuum," stated Dr. Rob Singleton, MD, and professor of neurology at the University of Utah in Salt Lake City. "We think obesity and the dysfunction of lips or fats are what's actually causing the issues."
Neuropathy means damage to the nerves, which transmit messages from the spinal cord to the brain. Neuropathy often causes numbness and tingling in the hands and feet, called peripheral neuropathy. Physical injury or trauma to nerves most often causes neuropathy; between 60 to 70 percent of diabetics also have neuropathy, ranging from mild to severe, according to the National Institute of Neurological Disorders and Stroke. A number of diseases, acute infections and toxins can also cause neuropathy. Many people turn to herbs for relief -- but do not take herbs for neuropathy without your doctor’s approval. Cayenne pepper contains capsaicin, a topical pain reliever that can help reduce discomfort from neuropathy. Capsaicin works by depleting substance P, a pain-causing chemical, from nerve receptors. Applying cayenne pepper in a topical solution initially stimulates the release of substance P but then depletes it, which decreases pain. Several over-the-counter topical pain relievers containing cayenne pepper approved for use by United States Food and Drug Administration are available. They appear to help at least some people with neuropathies from shingles; trigeminal neuralgia, which causes facial neuropathy; and diabetic retinopathy, the Diabetes Self-Management website reports. In some cases, topical application of this herb can worsen pain. Wright State University pharmacy suggests starting with the weakest concentration of the herb and increasing over time. It can take one to two months to work up to the strongest dose. A systematic review of studies conducted by the University of Oxford reported on study findings in the April 24, 2004 issue of the “British Medical Journal.” L. Mason and colleagues, of the Pain Research and Nuffield Department of Anaesthetics, reported that capsaicin had poor to moderate effectiveness overall in six separate studies.
Numbness in feet and hands is considered as one of the most discomforting & common health problems in the aged. When you suffer from numbness, you will face some symptoms like burning or tingling sensations, weakness of the troubled parts, body and feet ache, etc. Some common causes of numbness include excessive drinking, fatigue, smoking, constant pressure on the feet and hands, lack of magnesium or vitamin B12, etc. To deal with this problem, there are some quick natural remedies. To know the ways on how to cure numbness in hands and feet, read this post at VKool.com.
|



 Your new post is loading...
Your new post is loading...

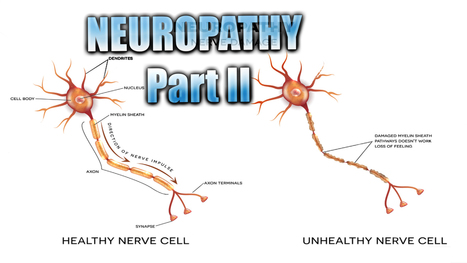






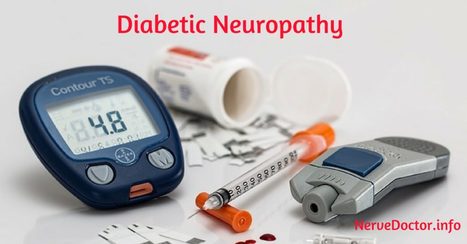








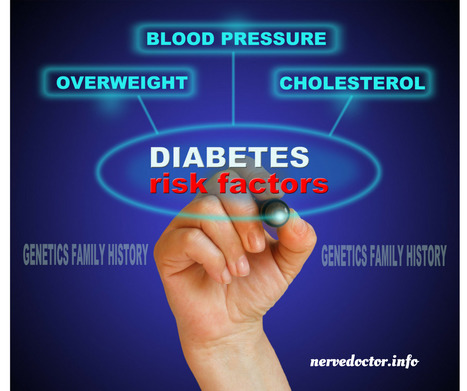








El Paso, TX. Neuropathy Presentation II: El Paso, TX. Chiropractor, Dr. Alexander Jimenez continues with neuropathy part II. Because the human body is composed of many different kinds of nerves which perform different functions, nerve damage is classified into several types. For Answers to any questions you may have please call Dr. Jimenez at 915-850-0900