Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
June 12, 2021 3:17 AM
|
Researchers investigating the benefits of 3D printing technology found it can deliver significant improvements to the running of hospitals. The research, which compared the drawbacks and advantages of using 3D printing technology in hospitals, has been published in the International Journal of Operations and Production Management. The study revealed that introducing such technology into hospitals could help alleviate many of the strains the UK healthcare system and healthcare systems worldwide face. Boosting surgery success rates - 3D printing makes it possible for surgical teams to print 3D models based on an individual patient’s surgical needs, providing more detailed and exact information for the surgeon to plan and practice the surgery, minimising the risk of error or unexpected complications. - the use of 3D printed anatomical models was useful when communicating the details of the surgery with the patient, helping to increase their confidence in the procedure. Speeding up patient recovery time - significant reduction in post-surgery complications, patient recovery times and the need for subsequent hospital appointments or treatments. Speeding up procedures - provide surgeons with custom-built tools for each procedure, with the findings revealing that surgeries with durations of four to eight hours were reduced by 1.5 to 2.5 hours when patient-specific instruments were used. - could also make surgeries less invasive (for example, removing less bone or tissue) - result in less associated risks for the patient (for example, by requiring less anaesthesia). Real-life training opportunities - enables trainee surgeons to familiarise themselves with the steps to take in complex surgeries by practicing their skills on examples that accurately replicate real patient problems, and with greater variety. Careful consideration required Despite the research showing strong and clear benefits of using 3D printing, Dr Chaudhuri and his fellow researchers urge careful consideration for the financial costs. 3D printing is a significant financial investment for hospitals to make. In order to determine whether such an investment is worthwhile, the researchers have also developed a framework to aid hospital decision-makers in determining the return on investment for their particular institution. read the study at https://www.researchgate.net/publication/344956611_Accepted_for_publication_in_International_Journal_of_Operations_and_Production_Management_Should_hospitals_invest_in_customised_on-demand_3D_printing_for_surgeries read more at https://www.healtheuropa.eu/3d-printing-technology-boosts-hospital-efficiency-and-eases-pressures/108544/

|
Scooped by
nrip
June 10, 2021 2:19 AM
|
Antibiotic resistance is a significant public health challenge, caused by changes in bacterial cells that allow them to survive drugs that are designed to kill them. Resistance often occurs through new mutations in bacteria that arise during the treatment of an infection. Understanding how this resistance emerges and spreads through bacterial populations is important to preventing treatment failure. Scientists have developed a mathematical model that predicts how the number and effects of bacterial mutations leading to drug resistance will influence the success of antibiotic treatments. Their model, described in the journal eLife, provides new insights on the emergence of drug resistance in clinical settings and hints at how to design novel treatment strategies that help avoid this resistance occurring. "Mathematical models are a crucial tool for exploring the outcome of drug treatment and assessing the risk of the evolution of antibiotic resistance," explains first author Claudia Igler, Postdoctoral Researcher at ETH Zurich, Switzerland. "These models usually consider a single mutation, which leads to full drug resistance, but multiple mutations that increase antibiotic resistance in bacteria can occur. So there are some mutations that lead to a high level of resistance individually, and some that provide a small level of resistance individually but can accumulate to provide high-level resistance." "Our work provides a crucial step in understanding the emergence of antibiotic resistance in clinically relevant treatment settings," says senior author Roland Regoes, Group Leader at ETH Zurich. "Together, our findings highlight the importance of measuring the level of antibiotic resistance granted by single mutations to help inform effective antimicrobial treatment strategies." read the study paper at https://elifesciences.org/articles/64116 read the original unedited article at https://phys.org/news/2021-05-mathematical-effect-bacterial-mutations-antibiotic.html

|
Scooped by
nrip
June 2, 2021 9:13 AM
|
Data encoded on DNA could last 500 years! Check out a new DNA decoder that can read data at 330 gigabits per square centimeter Years ago, the world marveled as it recognized that more human information was created on the internet than had been written in thousands of years of human history. But with the information age growing more complex by the day, we may have to look at new ways of storing information, and it turns out the DNA we're made of might hold the key to the ultimate organic hard drive. A team of scientists has developed a new way of storing data, using pegs and pegboards composed of DNA, which can be retrieved via microscope, in a molecular variant of the traditional Lite-Brite, according to a recent study published in the journal Nature Communications. The prototype can store information in DNA strands with a 10-nanometer space between them. This distance is less than one-thousandth of the diameter of a human hair, and roughly one-hundredth the size of a living bacterium. The team tested a digital nucleic acid memory (dNAM) with the storage of a simple statement: "Data is in our DNA/n." Earlier attempts to retrieve data stored in DNA called for DNA sequencing, which involves reading the genetic code of DNA strands — which is a critical tool in biology and medicine, but not very efficient for DNA memory. Data stored on DNA strands can last for 500 years Using a microscope, the team imaged hundreds of thousands of DNA pegs in one recording, allowing for an error-correction algorithm to retrieve all data. Once all of the bits were organized via algorithms, the prototype DNA decoder could read data at 330 gigabits per square centimeter. While this technology likely won't show up in smartphones or laptops in the near future, DNA storage has incredible potential for archival use. In case you missed it, DNA evolved to store unconscionable amounts of data. If we knew how, our genes could store all of the emails, tweets, songs, photos, films, and books that ever existed in a DNA volume the size of a jewelry box. read the original version of this interesting article at https://interestingengineering.com/dna-could-store-every-tweet-movie-book-and-more-in-a-jewelry-box-sized-device

|
Scooped by
nrip
June 1, 2021 4:32 PM
|
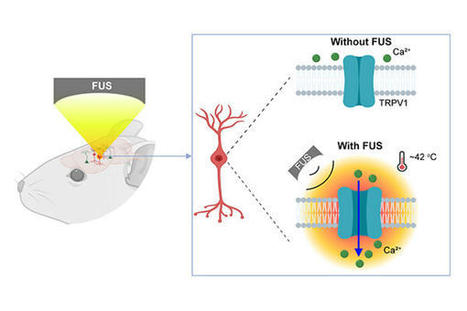
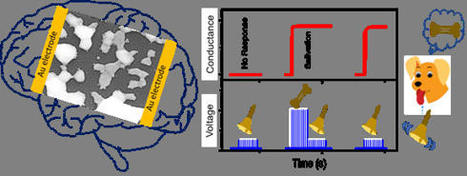
Neurological disorders such as Parkinson's disease and epilepsy have had some treatment success with deep brain stimulation, but those require surgical device implantation. A multidisciplinary team at Washington University in St. Louis has developed a new brain stimulation technique using focused ultrasound that is able to turn specific types of neurons in the brain on and off and precisely control motor activity without surgical device implantation. The team, led by Hong Chen, is the first to provide direct evidence showing noninvasive, cell-type-specific activation of neurons in the brain of mammal by combining ultrasound-induced heating effect and genetics, which they have named sonothermogenetics. It is also the first work to show that the ultrasound- genetics combination can robustly control behavior by stimulating a specific target deep in the brain. Results of the three years of research, which was funded in part by the National Institutes of Health's BRAIN Initiative, were published online in Brain Stimulation May 11, 2021. "Our work provided evidence that sonothermogenetics evokes behavioral responses in freely moving mice while targeting a deep brain site," Chen said. "Sonothermogenetics has the potential to transform our approaches for neuroscience research and uncover new methods to understand and treat human brain disorders." more at https://medicalxpress.com/news/2021-05-tool-deep-brain-neurons-combining.html

|
Scooped by
nrip
May 31, 2021 3:55 PM
|
What is photonics? In short, photonics is the scientific study and technological harnessing of light. However, it is important to note that the term "photonics" is something of a nebulous one. That being said, it is often used today to refer to a set of emerging technologies that deal with various aspects of light. These include technologies used to store, transfer, or manipulate information, but can also be used to include methods of harvesting energy from light and/or converting it to electricity. To put it another way, photonics, in the technological sense, refers to devices that use photons to send, receive, and process information similar to modern-day electronics. Today, one of the major applications of photonics, specifically integrated photonics, is in high-performance computing. Specific examples would be in the servers in large data server farms used by large tech companies like Google or Amazon. Beyond computing, photonics has applications in many other fields from medical sciences to energy production. In medical sciences, for example, photonics is used in a variety of ways including in surgery (such as eye surgery), tattoo removal, and surgical endoscopy. In the future, optical integrated circuits may well lead to the development of smaller, more compact, biosensors and other implantable medical devices freed from the limitation of electronics. more at https://interestingengineering.com/photonics-a-story-of-our-quest-to-harness-the-power-of-light

|
Scooped by
nrip
May 30, 2021 1:41 AM
|
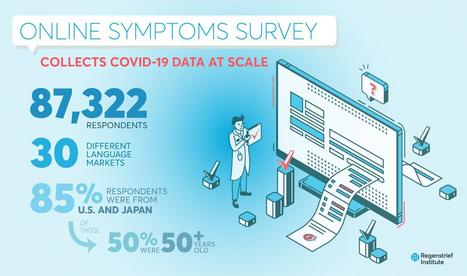
Identifying new COVID-19 cases is challenging. Not every suspected case undergoes testing, because testing kits and other equipment are limited in many parts of the world. Yet populations increasingly use the internet to manage both home and work life during the pandemic, giving researchers mediated connections to millions of people sheltering in place.
Objective: The goal of this study was to assess the feasibility of using an online news platform to recruit volunteers willing to report COVID-19–like symptoms and behaviors.
Methods: An online epidemiologic survey captured COVID-19–related symptoms and behaviors from individuals recruited through banner ads offered through Microsoft News. Respondents indicated whether they were experiencing symptoms, whether they received COVID-19 testing, and whether they traveled outside of their local area.
Results: A total of 87,322 respondents completed the survey across a 3-week span at the end of April 2020, with 54.3% of the responses from the United States and 32.0% from Japan. Of the total respondents, 19,631 (22.3%) reported at least one symptom associated with COVID-19. Nearly two-fifths of these respondents (39.1%) reported more than one COVID-19–like symptom. Individuals who reported being tested for COVID-19 were significantly more likely to report symptoms (47.7% vs 21.5%; P<.001). Symptom reporting rates positively correlated with per capita COVID-19 testing rates (R2=0.26; P<.001). Respondents were geographically diverse, with all states and most ZIP Codes represented. More than half of the respondents from both countries were older than 50 years of age.
Conclusions: News platforms can be used to quickly recruit study participants, enabling collection of infectious disease symptoms at scale and with populations that are older than those found through social media platforms. Such platforms could enable epidemiologists and researchers to quickly assess trends in emerging infections potentially before at-risk populations present to clinics and hospitals for testing and/or treatment.
source: Credit to Regenstrief Institute read the entire study here : https://www.jmir.org/2021/5/e24742

|
Scooped by
nrip
May 29, 2021 3:52 AM
|
The pandemic drove many patients to their primary care docs via video. And it worked. A telehealth expert (Dr. Peter Antall) explains how this shift could become a permanent hybrid with in-person care in an Interview with healthcareITNews Here is a summary from the interview. What is Virtual Primary Care Virtual primary care is allowing patients to see their primary care physician in person or virtually, depending on their needs. It combines the convenience of telehealth with the ability to strengthen recurring relationships with primary care physicians. It also can help provide a medical home for patients who have no primary care physician, either due to lack of access or lack of engagement. The emergence of virtual primary care stems from the recognition that the traditional primary care model doesn't work well for many patients. Access to care remains a major issue for many patients, due to geographical constraints and a growing shortage of primary care physicians, which has only been exacerbated by the pandemic. Do Patients Want it? Patients are receptive. A recent Amwell survey shows consumers want a virtual approach to primary care – - Most consumers (77%) would prefer to see their existing primary care provider via video.
- 25% of consumers are willing to switch providers to get it.
- 80% saying they would prefer to see the same primary care physician regularly via virtual care.
Can virtual primary care provide a simple, seamless care experience? How are patients supported throughout the care process? The best virtual primary care programs are well coordinated and enable a seamless care experience with the ability to transition patients between in-person and virtual care settings, and to various specialties or allied care providers as needed. In this way the care is holistic and the patient journey is clear and simple. Data sharing is an important part of creating a highly coordinated and seamless care experience. Records from all visits should be available to all providers on the telehealth platform across specialties and should be shared with the primary care physician in brick and mortar if one exists. This interoperability improves care and improves the referral and transition process. To ensure patients are supported, virtual primary care programs should include care coordination capabilities. For example, secure messaging between patients, healthcare professionals and administrative staff can help patients receive quick answers to their questions and ensure that all of their needs are met in a timely fashion, even after a visit has finished. Can virtual primary care help with population health? The flexibility of remote access makes it possible for providers to see patients' living conditions, evaluate social determinants of health, and respond in ways that make a deep impact on patients' lives. Providers also can leverage virtual primary care to evaluate medication adherence among patients with diabetes, hypertension and high cholesterol. When breakdowns in medication adherence are discovered, providers and support staff can work to engage patients in following their treatment plan more closely. This avoids complications that can occur when patients deviate from recommended treatment. Improvements in compliance and ongoing care can be accomplished through use of frequent brief touchpoints, care coordination, nudges and team-based care. Prompts and reminders can be used to reinforce the care plan. With capabilities such as these, virtual primary care positions providers and health plans not only to improve population health, but also to perform well under value-based models of care. More and more, it's clear that the future of care depends on hybrid models of care delivery such as this and I believe we've only just begun to scratch the surface of what's possible with virtual primary care and how it contributes to the continued transformation of healthcare. read the unedited article on the interview at https://www.healthcareitnews.com/news/will-virtual-primary-care-become-new-model-healthcare-delivery

|
Scooped by
nrip
May 27, 2021 4:56 AM
|
Anticipating the risk of gastrointestinal bleeding (GIB) when initiating antithrombotic treatment (oral antiplatelets or anticoagulants) is limited by existing risk prediction models. Machine learning algorithms may result in superior predictive models to aid in clinical decision-making. Objective: To compare the performance of 3 machine learning approaches with the commonly used HAS-BLED (hypertension, abnormal kidney and liver function, stroke, bleeding, labile international normalized ratio, older age, and drug or alcohol use) risk score in predicting antithrombotic-related GIB. Design, setting, and participants: This retrospective cross-sectional study used data from the OptumLabs Data Warehouse, which contains medical and pharmacy claims on privately insured patients and Medicare Advantage enrollees in the US. The study cohort included patients 18 years or older with a history of atrial fibrillation, ischemic heart disease, or venous thromboembolism who were prescribed oral anticoagulant and/or thienopyridine antiplatelet agents between January 1, 2016, and December 31, 2019. In this cross-sectional study, the machine learning models examined showed similar performance in identifying patients at high risk for GIB after being prescribed antithrombotic agents. Two models (RegCox and XGBoost) performed modestly better than the HAS-BLED score. A prospective evaluation of the RegCox model compared with HAS-BLED may provide a better understanding of the clinical impact of improved performance. link to the original investigation paper https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2780274 read the pubmed article at https://pubmed.ncbi.nlm.nih.gov/34019087/

|
Scooped by
nrip
May 26, 2021 4:33 AM
|
A team of researchers has developed the first human "mini-hearts" in the lab to have clearly beating chambers. The miniature organs, or organoids, are no bigger than sesame seeds and were generated by self-assembly using pluripotent stem cells, according to Science Magazine. The organoids mimic the functioning heart of a 25-day-old human embryo, and they may help humans solve the heart's many mysteries. Our capability to model the complexity of the human heart in vitro is still limited, consequently limiting our knowledge of how heart diseases develop. Congenital heart defects, for example, are the most common birth condition in humans, affecting around 1 percent of all live births. This alone demonstrates the need to create more precise organ-like platforms, which is where the researchers come in, with their newly devised method which was described in a study published in the journal Cell. The researchers engineered human pluripotent stem cells, which can divide into any kind of tissue, into multiple forms of cardiac cells to create heart organoids whose cells self-organize like those in an embryo. The aim was to create three tissue layers that make up a heart chamber's walls, which are one of the first parts of the heart to form. The organoids, which are around 2 mm in diameter and have survived more than 3 months in the lab so far, become structurally equal to the heart of a 25-year-old embryo in a week. They only have one chamber and the main types of cells at this point of development. Moreover, the heart's clearly defined chamber beats 60 to 100 times a minute, much like the heart of an embryo at the same age. read the entire story at https://interestingengineering.com/lab-grown-mini-heart-beats-like-a-25-day-old-human-embryos-heart

|
Scooped by
nrip
May 20, 2021 5:07 PM
|
The linked interview gives us all in Healthcare Technology a lot of food for thought. This below is a set of points extracted and massaged with my viewpoints The biggest barrier to physicians having the most complete medical history for their patients at every point of patient care is the lack of interoperability among information systems. State of Interoperability today: The industry has made progress in developing open standards and application programming interfaces to facilitate data fluidity and sharing among multiple electronic health record systems and data repositories. As a result, commercial and open source interoperability services are coming online. While there is room for optimism, the industry is still grappling with data structure and management challenges . First, incomplete, disparate and disconnected data. Most health and patient data is stored as unstructured medical format, and identifying information in the data is a manual and time-consuming process. There are significant variations in the way data is shared, read and understood across health systems, which can result in information being siloed and overlooked or misinterpreted . Further, most EHR systems do not follow patients on their care journey beyond the hospital or clinic walls. As a result, only a portion of healthcare data is available at any point of care, resulting in a fragmented view of a patient's health history. Second, slow adoption and scaling of open interoperability standards. Standards can streamline the structured data exchange needed to improve preventive and value-based care for people, predictions, diagnostics, post-marketing surveillance of medical products (for example drug, device), care quality, cost reduction and clinical research. Industry guidelines and resources like the Fast Healthcare Interoperability Resources (FHIR) from Health Level Seven International (HL7) have helped to set a standard, though there is still more work to be done to support organizations to remove barriers toward adoption and make the electronic exchange of data more seamless, with the goal of providing a better provider and patient experience. Third, risks due to siloed data: When it comes to storing health information including clinical, genomic, device, financial, supply chain and claims, data security is the top priority. Storing patient data across different systems and platforms makes it difficult to deliver personalized care, draw data insights and streamline service. This is a pivotal moment in time when healthcare can take what it's learned over the past year and fix the underlying problems. Perhaps the most important learning is that achieving true healthcare interoperability requires understanding, evaluating and solving issues in the underlying syntactic and semantic characteristics of the data. Syntactic interoperability requires a common structure so that data can be exchanged and interpreted between health IT systems, while semantic interoperability requires a common language so that the meaning of data is transferred along with the data itself. This combination supports data fluidity. The industry has made meaningful progress on this front. Unlocking Benefits of Interoperability As technology creates more data across healthcare organizations, applying technologies like artificial intelligence and machine learning will be essential to help take that data and create the shared structure and meaning necessary to achieve interoperability. Shared structure and meaning will enable interoperability solutions that transform data input from various media types and forms: voice, image, scan, PDF, etc., into a common text format which can be shared with and leveraged by every entity in the value chain. Instead of moving static, electronic documents or faxes like care summaries between healthcare providers, clinical AI-service APIs can enable EHR vendors and health systems to communicate in a standardized way with apps and other EHRs. With access to all available information, advanced analytics and machine learning can then enhance medical and scientific insights tied to patient outcomes in an accurate, scalable, secure and timely manner. read more at https://www.healthcareitnews.com/news/amazon-web-services-exec-talks-interoperability-lessons-past-year

|
Scooped by
nrip
May 18, 2021 11:48 PM
|
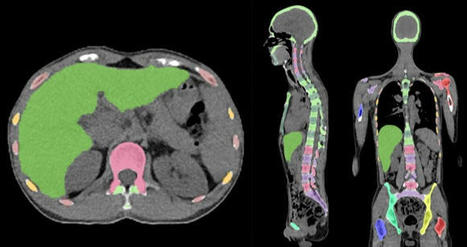
Skeleton/bone marrow involvement in patients with newly diagnosed Hodgkin’s lymphoma (HL) is an important predictor of adverse outcomes1. Studies show that FDG-PET/CT upstages patients with uni- or multifocal skeleton/bone marrow uptake (BMU) when iliac crest bone marrow biopsy fails to find evidence of histology-proven involvement. The general recommendation is, therefore, that bone marrow biopsy can be avoided when FDG-PET/CT is performed at staging. Our aim was to develop an AI-based method for the detection of focal skeleton/BMU and quantification of diffuse BMU in patients with HL undergoing staging with FDG-PET/CT. The output of the AI-based method in a separate test set was compared to the image interpretation of ten physicians from different hospitals. Finally, the AI-based quantification of diffuse BMU was compared to manual quantification. Artificial intelligence-based classification A convolutional neural network (CNN) was used to segment the skeletal anatomy11. Based on this CNN, the bone marrow was defined by excluding the edges from each individual bone; more precisely, 7 mm was excluded from the humeri and femora, 5 mm was excluded from the vertebrae and hip bones, and 3 mm was excluded from the remaining bones. Focal skeleton/bone marrow uptake The basic idea behind our approach is that the distribution of non-focal BMU has a light tail and most pixels will have an uptake reasonably close to the average. There will still be variations between different bones. Most importantly, we found that certain bones were much more likely to have diffuse BMU than others. Hence, we cannot use the same threshold for focal uptake in all bones. At the other end, treating each bone individually is too susceptible to noise. As a compromise, we chose to divide the bones into two groups: -
“spine”—defined as the vertebrae, sacrum, and coccyx as well as regions in the hip bones within 50 mm from these locations, i.e., including the sacroiliac joints. -
“other bones”—defined as the humeri, scapulae, clavicles, ribs, sternum, femora, and the remaining parts of the hip bones. For each group, the focal standardized uptake values (SUVs) were quantified using the following steps: - Threshold computation. A threshold (THR) was computed using the mean and standard deviation (SD) of the SUV inside the bone marrow. The threshold was set to
- 2. Abnormal bone region. The abnormal bone region was defined in the following way:
Only the pixels segmented as bone and where SUV > THR were considered. To reduce the issues of PET/CT misalignment and spill over, a watershed transform was used to assign each of these pixels to a local maximum in the PET image. If this maximum was outside the bone mask, the uptake was assumed to be leaking into the bone from other tissues and was removed. Finally, uptake regions smaller than 0.1 mL were removed. - 3.Abnormal bone SUV quantification. The mean squared abnormal uptake (MSAU) was first calculated as
MSAU=meanof(SUV−THR)2overtheabnormalboneregion. To quantify the abnormal uptake, we used the total squared abnormal uptake (TSAU), rather than the more common total lesion glycolysis (TLG). We believe TLG tends to overestimate the severity of larger regions with moderate uptake. TSAU will assign a much smaller value to such lesions, reflecting the uncertainty that is often associated with their classification. Instead, TSAU will give a larger weight to small lesions with very high uptake. This reflects both the higher certainty with respect to their classification and the severity typically associated to very high uptake. TSAU=MSAU×(volumeoftheabnormalboneregion). This calculation leads to two TSAU values; one for the “spine” and one for the “other bones”. As the TSAU value can be nonzero even for patients without focal uptake, cut-off values were tuned using the training cohort. The AI method was adjusted in the training group to have a positive predictive value of 65% and a negative predictive value of 98%. For the “spine”, a cut-off of 0.5 was used, and for the “other bones”, a cut-off of 3.0 was used. If one of the TSAU values was higher than the corresponding cut-off, the patient was considered to have focal uptake. Results Focal uptake Fourteen of the 48 cases were classified as having focal skeleton/BMU by the AI-based method. The majority of physicians classified 7/48 cases as positive and 41/48 cases as negative for having focal skeleton/BMU. The majority of the physicians agreed with the AI method in 39 of the 48 cases. Six of the seven positive cases (86%) identified by the majority of physicians were identified as positive by the AI method, while the seventh was classified as negative by the AI method and by three of the ten physicians. Thirty-three of the 41 negative cases (80%) identified by the majority of physicians were also classified as negative by the AI method. In seven of the remaining eight patients, 1–3 physicians (out of the ten total) classified the cases as having focal uptake, while in one of the eight cases none of the physicians classified it as having focal uptake. These findings indicate that the AI method has been developed towards high sensitivity, which is necessary to highlight suspicious uptake. Conclusions The present study demonstrates that an AI-based method can be developed to highlight suspicious focal skeleton/BMU in HL patients staged with FDG-PET/CT. This AI-based method can also objectively provide results regarding high versus low BMU by calculating the SUVmedian value in the whole spine marrow and the liver. Additionally, the study also demonstrated that inter-observer agreement regarding both focal and diffuse BMU is moderate among nuclear medicine physicians with varying levels of experience working at different hospitals. Finally, our results show that the automated method regarding diffuse BMU is comparable to the manual ROI method. read the original paper at https://www.nature.com/articles/s41598-021-89656-9

|
Scooped by
nrip
May 18, 2021 12:56 PM
|
The aim of the Connected Healthcare Study was to understand the impact COVID-19 has had on health care and communication with providers and gain insights into experiences and preferences as it relates to telehealth and online health care tools. More than two-thirds of U.S. patients (69%) had seen a health care provider via telehealth since the COVID-19 pandemic began, with more than two in five (46%) meeting with a PCP and about one in five (19%) meeting with a mental health care provider. Other providers whom respondents have seen via telehealth since the pandemic began included specialties like ophthalmology and women’s health and orthopedic care, which were not considered typical telehealth users before the pandemic. Telehealth is clearly emerging from the COVID-19 pandemic as the new normal – an overwhelming majority (84%) of respondents who received telehealth services since March 2020 reported that they plan to continue using telehealth appointments in the future, with the top reasons being that it’s more convenient (43%) or to avoid being around people who are ill (39%). One of the most striking results of the survey was that nearly half of U.S. patients (48%) reported that they have sought (4%) or would be likely to seek care (44%) from a different health care provider if their current provider did not offer telehealth appointments. This is clearly a resounding message of support for telehealth from patients to their physicians. As we look back on the broader impact of the COVID-19 pandemic, it will have catapulted patient awareness and acceptance of telehealth and virtual care to the extent that would have been inconceivable before the pandemic. It has also brought to the forefront many other aspects of patient electronic and virtual engagement with providers across all specialties. read the entire post at https://www.kevinmd.com/blog/2021/05/how-do-patients-really-feel-about-virtual-care-and-electronic-patient-engagement.html

|
Scooped by
nrip
May 18, 2021 1:22 AM
|
Low anterior resection syndrome (LARS) is a common functional disorder that develops after patients with rectal cancer undergo anal preservation surgery. Common approaches to assess the symptoms of patients with LARS are often complex and time-consuming. Instant messaging/social media has great application potential in LARS follow-up, but has been underdeveloped. Objective: The aim of this study was to compare data between a novel instant messaging/social media follow-up system and a telephone interview in patients with LARS and to analyze the consistency of the instant messaging/social media platform. Methods: Patients with R0 resectable rectal cancer who accepted several defecation function visits via the instant messaging/social media platform and agreed to a telephone interview after the operation using the same questionnaire including subjective questions and LARS scores were included. Differences between the 2 methods were analyzed in pairs and the diagnostic consistency of instant messaging/social media was calculated based on telephone interview results. Conclusions The instant messaging/social media system provides a promising solution to accommodate the primary follow-up needs of patients with LARS by integrating complex functional follow-up tools into smartphone apps. Although it is currently not a substitute for manual follow-up, it has the potential of becoming a major LARS screening method. However, further research on response rate, information accuracy, and user acceptance is needed before an advanced system can be implemented
|

|
Scooped by
nrip
June 11, 2021 3:57 AM
|
Antibiotic resistance is one of the greatest global health challenges of our time. Wastewater treatment plants are a true breeding ground for antibiotic-resistant germs, as this is where pathogens and antibiotic residues come together. The resistant bacterial strains then re-enter the environment via the treated water and can spread further. Scientists at the University of Naples Federico II have now developed a nanomaterial to combat this problem. Supported by instrument scientist Dr. Judith Houston from Forschungszentrum Jülich (and meanwhile at the European Spallation Neutron Source ESS in Sweden), they have analyzed it at the Heinz Maier-Leibnitz Zentrum. The material is a hybrid of humic acid and titanium dioxide (TiO2). Humic acids (HAs), which occur naturally in humus soils, have useful properties that can counteract water pollution: on the one hand, they have an antibacterial effect, and on the other hand, they can bind small molecules such as antibiotics. Highlights • In situ hydrothermal route is a versatile approach to realize multifunctional hybrid nanomaterials for biowaste valorization.
• The combination at molecular scale of HAs and TiO2 improves the.•OH generation even under visible light;
• Hybrid HA-NDL/TiO2 nanomaterials exert a ROS-mediated antibacterial activity.
• Surface and colloidal properties make the hybrid nanomaterials as valid sequestering agents against antibiotics.
• A high and selective activity is shown in sequestering amoxicillin and tetracycline contaminants. image © Wenzel Schuermann / TU Muenchen read the study at https://www.sciencedirect.com/science/article/abs/pii/S0013935120314596 read the entire article/press release at the MLZ website at https://mlz-garching.de/englisch/news-und-press/news-articles/nanomaterial-sagt-resistenten-bakterien-den-kampf-an.html

|
Scooped by
nrip
June 2, 2021 9:54 AM
|
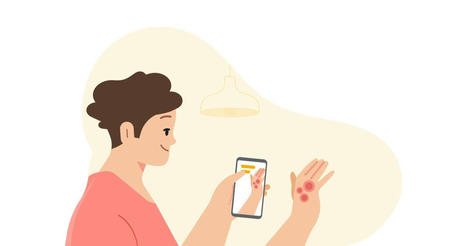
Google's AI-powered tool that will be available later this year helps anyone identify skin conditions using their phone’s camera. Artificial intelligence (AI) has the potential to help clinicians care for patients and treat disease — from improving the screening process for breast cancer to helping detect tuberculosis more efficiently. When we combine these advances in AI with other technologies, like smartphone cameras, we can unlock new ways for people to stay better informed about their health, too. Google's AI-powered dermatology assist tool is a web-based application that they hope to launch as a pilot later this year, to make it easier to figure out what might be going on with their skin. Once the user launchs the tool, simply use their phone’s camera to take three images of the skin, hair or nail concern from different angles. They are then asked questions about their skin type, how long they’ve had the issue and other symptoms that help the tool narrow down the possibilities. The AI model analyzes this information and draws from its knowledge of 288 conditions to give the user a list of possible matching conditions that they can then research further. For each matching condition, the tool will show dermatologist-reviewed information and answers to commonly asked questions, along with similar matching images from the web. The tool is not intended to provide a diagnosis nor be a substitute for medical advice as many conditions require clinician review, in-person examination, or additional testing like a biopsy. Rather Google hopes it gives users access to authoritative information so they can make a more informed decision about their next step. Developing an AI model that assesses issues for all skin types Google's tool is the culmination of over three years of machine learning research and product development. To date, Google has published several peer-reviewed papers that validate their AI model and they claim more are in the works. Recently, the AI model that powers the tool successfully passed clinical validation, and the tool has been CE marked as a Class I medical device in the EU. more at https://blog.google/technology/health/ai-dermatology-preview-io-2021/

|
Scooped by
nrip
June 2, 2021 7:24 AM
|
Scientists have fabricated a device that can mimic human brain cognitive actions and is more efficient than conventional techniques in emulating artificial intelligence, thus enhancing the computational speed and power consumption efficiency. Artificial intelligence is now a part of our daily lives, starting from email filters and smart replies in communication to helping battle the Covid-19 pandemic. But AI can do much more such as facilitate self-driving autonomous vehicles, augmented reality for healthcare, drug discovery, big data handling, real-time pattern/image recognition, solving real-world problems, and so on. These can be realised with the help of a neuromorphic device which can mimic the human brain synapse to bring about brain-inspired efficient computing ability. The human brain comprises of nearly a hundred billion neurons consisting of axons and dendrites. These neurons massively interconnect with each other via axons and dendrites, forming colossal junctions called synapse. This complex bio-neural network is believed to give rise to superior cognitive abilities. Software-based artificial neural networks (ANN) can be seen defeating humans in games or helping handle the Covid-19 situation. However, the power-hungry (in megawatts) von Neumann computer architecture slows down ANNs performance due to the available serial processing while the brain does the job via parallel processing consuming just 20 W. It is estimated that the brain consumes 20% of the total body energy. From the calory conversion, it amounts to 20 watts. While the conventional computing platforms consume megawatts, i.e., 1 million watts of energy, to mimic basic human cognition. To overcome this bottleneck, a hardware-based solution involves an artificial synaptic device that, unlike transistors, could emulate the functions of human brain synapse. Scientists had long been trying to develop a synaptic device that can mimic complex psychological behaviors without the aid of external supporting (CMOS) circuits. To address this challenge, Scientists from Jawaharlal Nehru Centre for Advanced Scientific Research, Bengaluru, an autonomous institute of the Department of Science & Technology, Government of India, devised a novel approach of fabricating an artificial synaptic network (ASN) resembling the biological neural network via a simple self-forming method (the device structure is formed by itself while heating). This work has been recently published in the journal ‘Materials Horizons’. “Nature has had an incredible amount of time and diversity to engineer ever new forms and functions through evolution. Learning and emulating new processes, technologies, materials and devices from the nature and biology are the important pathways to the significant advances of the future which will increasingly integrate the worlds of the living with the man-made technologies,” said Prof Ashutosh Sharma, Secretary, DST. read the original unedited post at https://www.indianext.co.in/2021/06/scientists-develop-efficient-artificial-synaptic-network-that-mimics-human-brain/

|
Scooped by
nrip
June 1, 2021 3:18 AM
|
If there’s one dialogue that’s been growing louder across the healthcare landscape, it’s the consumerization of healthcare. Market trends are undeniably steering the healthcare experience into a new paradigm where patients are seizing control. Yet this new direction is not always beneficial for patients or providers. Just as consumer-driven industries like Uber and Netflix offer quick and seamless digital transactions, many patients want greater convenience and speed from care delivery. Many are also seeking more cost-effective options, thanks to climbing medical debt and high-deductible insurance plans. They’re less willing to tolerate care delays and inefficiencies; many will leave a poor online review after a frustrating appointment. These are all understandable goals and reactions. But as patients climb into the driver’s seat of healthcare, they’re not always given a roadmap to their intended destination. As they navigate their options, some are running up against four dynamics: 1. Dr. Google In our fast-paced world, many patients don’t want to wait weeks for an appointment or take time off from work to bring their child to the pediatrician. Instead they take out their smartphone and look up symptoms to get a quick and theoretical diagnosis. Patients can view photographs of lesions, read checklists of cancer symptoms and lurk on forums where people describe surgery experiences – and encourage each other to self-diagnose.
2. Retail Clinics
Retail clinics like CVS and Walgreens have exploded in popularity – and the market is expected to surpass $8 billion USD by 2028. Patients who feel they’re too busy or too peripatetic to maintain a consistent PCP relationship often prefer the extended hours and easy access of these clinics.
3. Cost Avoidance
Patients are paying higher and higher coinsurances, deductibles and copays – and they’re sick of it. They’re annoyed by a hospital’s inability to give them an accurate procedure cost in advance; many are stuck with “surprise” invoices after checking into a network hospital and receiving care from an out-of-network doctor.
4. Application Chaos
As applications and portals take over the Internet, many healthcare systems have turned a great idea into patient confusion. Even patients with moderate care needs may find themselves managing an overwhelming collection of healthcare apps for their OB/GYN practice, dentist, dermatologist, PCP, various hospital online payment portals, lab result repositories and data from their wearables.

|
Scooped by
nrip
May 30, 2021 3:41 AM
|
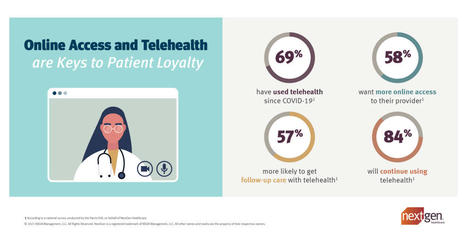
A Recent Harris Poll Survey on behalf of NextGen Healthcare Confirms Patients Seek the Convenience of Self Service and Option to See Providers Virtually The survey was conducted online and the results are based on the inputs gathered from 2,000 U.S. adults, including 1,733 who typically see a healthcare provider annually (“patients”). The survey results generated insights into patient experiences and preferences related to online healthcare tools. Telehealth is here to stay. - 84 % of U.S. patients who received telehealth services since March 2020 plan to continue using telehealth appointments in the future citing reasons such as
- convenience (43 %)
- or to avoid being around people who are ill (39 %).
- More than half of U.S. patients (57 %) say they would be more likely to get follow-up medical care if telehealth appointments were an option.
- 48 % patients indicate they would switch to a different healthcare provider if their current provider did not offer telehealth appointments.WOW!
- 69 % patients have seen a healthcare provider via telehealth since the COVID-19 pandemic began,
- 46 % - primary care physician (PCP)
- 19 % - mental healthcare provider.
- 15% - women’s health provider
- 9% ophthalmologist
- 7% orthopedist
Online access is a must. 58 percent patients would like to have more online access to their healthcare provider. Age plays a role in this: Patients from 18-54 are significantly more likely than patients 55 and older to say they would like to have more online access to their healthcare provider (68 percent vs. 43 percent). Topping the list of most important online services patients would look for if seeking a new provider are: - online appointment scheduling (49 percent)
- ability to check-in or complete health forms/appointment paperwork online before an appointment (49 percent)
- online prescription management (48 percent)
- online medical records access (47 percent)
John Beck, chief solutions officer for NextGen Healthcare says in the release - “These survey results confirmed that patients’ overall expectations for healthcare have shifted permanently. Integrated healthcare technology is good for the patient and good for the practice.” read the original release at https://www.businesswire.com/news/home/20210520005327/en/National-Survey-Shows-Online-Access-and-Telehealth-are-Keys-to-Patient-Loyalty

|
Scooped by
nrip
May 29, 2021 1:41 PM
|
The COVID-19 pandemic has had an unprecedented impact on the education and wellbeing of medical trainees. In supporting learning during these times, residency programs have adopted flexible scheduling, focused on frequent and transparent communication, incorporated different strategies to build community and promote psychological wellbeing, and advanced virtual teaching modalities. We are hopeful that these interventions will be long lasting. This pandemic will undoubtedly be a defining moment in our careers and our lives. We not only learned to be better physicians; the experience has made us better human beings. We shared the same fears and worries of our patients and their families and became more compassionate; we grew more patient, flexible and understanding. We were taught important lessons in courage and teamwork. From this experience, we have learned not to fear the unknown, but to grow from the process and rebuild stronger. The aim of this article is to share strategies that have helped us to move forward in the aftermath of the first phases of the pandemic, whilst we prepare for the uncertainty of the future. We hope that the lessons we have learned can help inform other programs as they react and adapt to the global after-effects of this crisis. The - Prioritize Residents' Wellbeing
- Incorporate Leadership Training into the Curriculum
- Establish Frequent and Active Communication
- Continue to Build Community – Even Virtually
- Embrace Technology
- Every Day, Small Gestures Can Have a Large Impact
read the entire paper at https://www.dovepress.com/rebuilding-graduate-medical-education-after-a-crisis-perspectives-of-m-peer-reviewed-fulltext-article-AMEP

|
Scooped by
nrip
May 28, 2021 6:03 PM
|
Improving the management of unstructured content is crucial when it comes to creating successful healthcare platforms. Clinicians can build better pictures of their patients when they use healthcare platforms which harness unstructured content, as well as structured content, to create a single source of clinical information. Analysts estimate that as much as 80 per cent of patient information is currently unstructured and is not contained in Electronic Health Records (EHRs). This means that vital clinical information, such as paper records or medical imaging, which does not tick specific boxes, can be overlooked. to read more, visit https://www.healthcareitnews.com/news/apac/improving-healthcare-better-managing-unstructured-content

|
Scooped by
nrip
May 26, 2021 1:48 PM
|
Researchers at Duke University are developing an artificial intelligence tool for toilets that would help providers improve care management for patients with gastrointestinal issues through remote patient monitoring. The tool, which can be installed in the pipes of a toilet and analyzes stool samples, has the potential to improve treatment of chronic gastrointestinal issues like inflammatory bowel disease or irritable bowel syndrome, according to a press release. When a patient flushes the toilet, the mHealth platform photographs the stool as it moves through the pipes. That data is sent to a gastroenterologist, who can analyze the data for evidence of chronic issues. A study conducted by Duke University researchers found that the platform had an 85.1 percent accuracy rate on stool form classification and a 76.3 percent accuracy rate on detection of gross blood. read the entire article at https://mhealthintelligence.com/news/ai-toilet-tool-offers-remote-patient-monitoring-for-gastrointestinal-health

|
Scooped by
nrip
May 22, 2021 5:15 PM
|
In the United States, on April 5, a federal rule went into effect that requires health care providers to give patients electronic access to their health information without delay upon request, at no cost. Many patients may now find their doctors’ clinical notes, test results and other medical data posted to their electronic portal as soon as they are available. Advocates herald the rule as a long-awaited opportunity for patients to control their data and health. But the rollout of the rule has hit bumps, as doctors learn that patients might see information before they do. Patients have long had a legal right to their medical records but often have had to pay fees, wait weeks or sift through reams of paper to see them. The rule aims not only to remove these barriers, but also to enable patients to access their health records through smartphone apps, and prevent health care providers from withholding information from other providers and health IT companies when a patient wants it to be shared. “This levels the playing field, A decade ago, the medical record belonged to the physician.” as per Jan Walker, co-founder of OpenNotes“ Privacy rules under the Health Insurance Portability and Accountability Act, which limit sharing of personal health information outside a clinic, remain in place, although privacy advocates have warned that patients who choose to share their data with consumer apps will put their data at risk. Studies have shown numerous benefits of note sharing. Patients who read their notes understand more about their health, better remember their treatment plan and are more likely to stick to their medication regimen. Non-white, older or less educated patients report even greater benefits than others. read the original unedited story at https://www.kevinmd.com/blog/2021/05/doctors-now-must-provide-patients-their-health-data-online-and-on-demand.html

|
Scooped by
nrip
May 19, 2021 3:46 AM
|
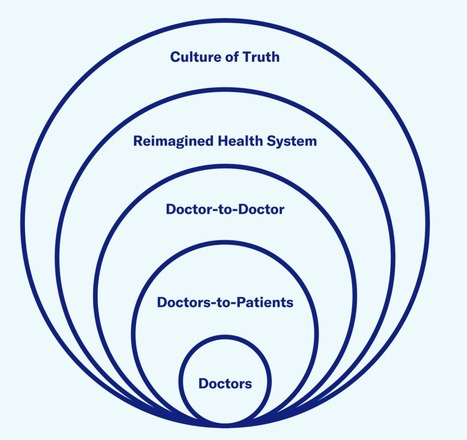
The Future of Health care needs Doctors and Technologists to work well together
In a new report - The Truth About Doctors - Covid 19 Edition, McCann Health identifies four key ways how health care technology has changed since 2016. It highlights the the role of the health care industry in leveraging these changes to carve a new way forward In the past, technology has been gradually revolutionizing health care. While patients have adopted it whole heartedly, It has received push back from various quarters of care providers. Many think it may be having less-positive effects for physicians, some of whom eye it as a threat to doctoring. However, come Covid-19, and the world simultaneously looked up to technology and the medical community in more or less an equal measure. They wanted Tech to help us navigate the pandemic and the medical community to get us out of it, and the need for both to work together and amplify became clearer with each day since the pandemic started As the world moves towards a period of renewal, it will be increasingly important that technology plays a complementary role in care, not just supporting doctoring but super-powering it. Lets look at the 4 main focus areas mentioned in the report. Technology is redefining the where of care Home defines most individuals’ physical, mental, and social health. Until recently, home has also been a place where doctors are absent. That changed with Covid-19 and the rapid growth of telemedicine If marketers and others within the health care industry can help doctors acclimatize to the new where of care — supporting them to embrace the home as an extension of their domain rather than something outside of it — health can be elevated in a more holistic level. Technology can help cultivate inter-professional collaboration During the pandemic, by using social media and messaging platforms like Twitter and WhatsApp, doctors with diverse backgrounds were able to pool knowledge and emotionally support each other in the collective effort to fight Covid-19. They collaborated in new ways with allied health care professionals, government, and industry, sparking a reimagining of the health ecosystem. The challenge moving forward is giving this organic way of working across care teams and borders a structure to make it scalable. How can the health care system evolve so an expert in peripheral neuropathy in Australia can collaborate with a startup in Belgium? On a more local level, how can health care systems ensure that the different health professionals involved in a patient’s care work together? Secure, shared platforms can nurture a sense of belonging and create a new kind of community for doctors — a “care tribe” that has the power to connect perspectives and passions to advance the experience of care. Technology can foster continuity and ‘contiguity’ There is a new willingness to take control over personal well-being in light of the pandemic. However this can only go so far in a health care system where time is limited and resources are fragmented. With the proliferation of sensors there may be no better time to apply the quantifiable self to achieve more personalized care. However, new self-monitoring technologies must be integrated with the full health care ecosystem to make personal health care easier and more seamless, rather than adding to the confusion. Even if technology provides access to more health information, it does not necessarily follow that patients or health care providers will understand it. Health care providers must be taught the skills to not only help patients decipher their health information but to advance their care by proactively identifying and addressing their health risks. With this comes a need to ensure that work is being done in a way that overcomes health inequities rather than heightens them. Technology can care for the carers Covid-19 has shown that, instead of posing an existential threat to doctors, technology may be a lifeline for them. By assessing patients before a consult, tech platforms can allow doctors to channel their energy to the problems that need it most. In complicated therapy areas such as oncology, it can ease their load through supporting diagnosis, treatment, and prognosis. In the day-to-day practice of caregiving, technology can enrich relationships by enabling doctors to focus on the human art of medicine. Combined with the flexibility of video consultations and the panoramic perspective of integrated systems, technology can give doctors their time back to practice care on their own terms. It’s easy to think that health care is behind the curve when it comes to embracing technology. Covid-19 has shown that this just isn’t the case. When it comes to the relationship between doctors and technology, the pandemic has been an epiphany. Instead of displacing doctors, technology has the power to help them provide better care, supercharging the humanity and empathy that lies at the heart of medicine. Technology has a role in medicine, especially in the service of care. along with my own insights and thoughts

|
Scooped by
nrip
May 18, 2021 7:12 PM
|
The pandemic has accelerated some trends here, notably telemedicine. That’s given a healthy push to an emerging field – remote diagnostics. Your phone is gradually – with some extensions – turning into a remote diagnostic tool to replace doctor visits and expensive tests. That’s fairly well known, even if it is extraordinary: blood oxygen levels are captured by a device costing less than $20, while an always-on cardiac monitor tracks heart activity, for example. But that’s just the very tip of the iceberg. Remote diagnosis can transform the entire scientific basis of modern medicine. Currently, the gold standard for testing the safety and efficacy of treatments is the randomized control trial (RCT), in which some part of the trial group is treated while another part is not. Both are tracked to see whether the treatment worked, and to look for adverse events like additional illness or even deaths. Outcomes are assessed using standard statistical tools to compare the two groups. This is the gold standard. But it is based on a single core assumption: that humans by and large react similarly to treatments, and hence that the best way to address disease is to identify treatments that work effectively for large numbers of patients. Ideally, treatments work for everyone, although sometimes RCTs and subsequent tracking find groups for which a treatment doesn’t work, or another for which it works especially well – maybe the old (or young), men (or women), or people with specific pre-existing conditions. Still, this is definitely mass-oriented medicine: it’s based on the impact of treatments on what might be called the median patient. Amazon is about to enter healthcare in a big way. It is already planning to offer Amazon Care (its primary care system organized around telehealth) not just to its 1.2 million employees, but to other employers as a service, much like it offered Amazon Web Services 15 years ago (and AWS is now the leading provider of internet infrastructure in the world). It also purchased Pillpack and set up Amazon Pharmacy to deliver medications and other health products online for delivery. But the real revolution is coming inside the home. The Amazon Halo is a new health monitoring device (with some admittedly creepy privacy-related features). It is designed to apply the capabilities of AI to the needs of individual patients. And then there is Alexa, which is clearly going to be Amazon’s device of choice for wellness in the home. It’s already partnered with Sharecare to provide automated advice on 80,000 wellness and health questions, as a first line response to health concerns. Alexa will likely expand, gaining the capacity to integrate remote diagnostics and escalation into Amazon’s wider telehealth network. Still, this mostly sounds like more of the same: using telehealth and the telemedicine capabilities, but mainly just extending what we do now, making it all a bit more convenient – possibly, a lot more convenient. But all these new tools, and especially diagnostics tools, make truly personal medicine possible – like Amazon, all this will be individual-specific: a market segment of you. read the entire unedited article at https://www.healthitanswers.net/into-the-future-amazon-and-the-coming-rise-of-personal-healthcare/

|
Scooped by
nrip
May 18, 2021 4:49 AM
|
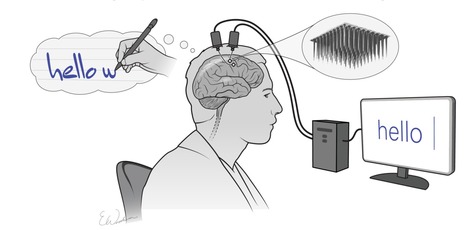
The combination of mental effort and state-of-the-art technology have allowed a man with spinal injury and immobilized limbs, to communicate by text at speeds rivaling those achieved by his able-bodied peers texting on a smartphone. Call it mindwriting. Scientists at Stanford University, Howard Hughes Medical Institute, and Brown University, developed an implanted brain-computer interface (BCI) technology that uses artificial intelligence to convert brain signals generated when someone visualizes the process of handwriting, into text on a computer, in real time. The team now reports on a trial in which a paralyzed clinical trial participant with a BCI implant was able to “type” words on a computer by merely thinking about the hand motions involved in creating written letters. The software effectively decoded the information from the BCI to quickly convert the man’s thoughts about handwriting into text on a computer screen. In the reported study, the 65-year-old male participant achieved a typing rate of 90 characters per minute, more than double the previous record for typing with a brain-computer interface. The goal is to restore the ability to communicate by text. As per Frank Willett, PhD, the first author of the paper, The system is so fast because each letter elicits a highly distinctive activity pattern, making it relatively easy for the algorithm to distinguish one from another, The new study is part of the BrainGate clinical trial, directed by Leigh Hochberg, MD, a neurologist and neuroscientist at Massachusetts General Hospital, Brown University, and the Providence VA Medical Center. The BrainGate collaboration has been working for several years on systems that enable people to generate text through direct brain control. While a major focus of BCI research has been on restoring gross motor skills, as the team further noted, “rapid sequences of highly dexterous behaviors, such as handwriting or touch typing, might enable faster rates of communication.” What wasn’t known, they pointed out, was whether “… the neural representation for a rapid and highly dexterous motor skill, such as handwriting, also remains intact.” Next, the team intends to work with a participant who cannot speak, such as someone with amyotrophic lateral sclerosis, a degenerative neurological disorder that results in the loss of movement and speech. In addition, they are looking to increase the number of characters available to the participants, such as capital letters and numbers. read the paper "High performance Brain-to-Text communication via handwriting" read the article in its entirety at https://www.genengnews.com/news/brain-computer-interface-converts-mental-handwriting-into-written-text/
|



 Your new post is loading...
Your new post is loading...