The 2016 MIT SMR/BCG Sustainability Report finds investors’ concerns are being overlooked by execs.
Even in Healthcare and Pharmaceutical industry sustainability is key. Issue however is the way in which this strategy is communicated which could influence responses from investors who grow more and more to be keen on sustainability as a criterion for their investments!
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

 Your new post is loading... Your new post is loading...
A group of healthcare organizations and medtech companies have formally launched the Medical Device Cybersecurity Task Force.
rob halkes's insight:
Needed so much now a collaboration of medical industry to secure devices from being intervened with! Necessary. Good luck!
Here's the download to the full report covering the survey the Enterprise Mobility Exchange, conducted to provide you with what is driving the global market for enterprise mobility, across the entire spectrum of professionals who operate in the space.
rob halkes's insight:
This recent overview of enterpise mobility also give some data on mobile health services and specifically highlights the motivation to develop customer services in this perspective!
What Are 6 Do's And 5 Don'ts With Social Media For Healthcare? #HCSM #infographic SocialSpotlightMedia I look 4Ward to your feedback. Keep Digging for Worms! DR4WARD enjoys helping connect students and pros to learn about all forms of communication and creativity. He talks about, creates, and curates content on: Digital, Marketing, Advertising, Public Relations, Social Media, Journalism, Higher Ed, Innovation, Creativity, and Design. Curated global resources can be found here: https://www.rebelmouse.com/dr4ward/ Find DR4WARD resources on Pinterest: http://pinterest.com/dr4ward/ Follow DR4WARD on Twitter: @DR4WARD Via Plus91
rob halkes's insight:
INteresting view in social media and health
The Economist Intelligence Unit's latest white paper looks at the latest developments in value-based healthcare. After years of tight healthcare budgets in many OECD countries, healthcare spending is now starting to accelerate again. In the UK, where doctors are about to go on strike, the government is having to promise extra money to bolster emergency or even routine care as demand from an ageing population rises. It is not alone: in the past month Ireland and Canada have both announced plans to increase spending, as has the much poorer India. But with budgets still struggling to keep pace with demand for health, these countries need to be sure any increase in spending is not wasted. In the latest of a series of reports on value-based healthcare, the Economist Intelligence Unit looks at how countries are working to ensure that spending on health is linked directly to the resulting health improvements, rather than to the volume of operations or doctor visits. For many developed countries that means stepping up the development of health technology assessment (HTA), which attempts to work out the cost-effectiveness of medicines, medical equipment, or treatment methods. These efforts are being echoed by smaller projects in developing markets, which are keen to improve their citizens' health without building up the costly healthcare infrastructure of the US or Europe. Key developments highlighted in the report
Despite these efforts, the implementation of value-based healthcare remains a work-in progress. Although the idea of linking health spending to outcomes is a simple one, both the underlying principles and the implementation mechanisms may be difficult to establish. Many countries are experimenting with different mechanisms, using pilot projects or tweaking their methods as problems arise. But the report emphasises that valuable lessons are emerging from these experiments, as the idea of value-based healthcare spreads worldwide. The full report, entitled Value-based healthcare: an update, is available for free from: http://www.eiu.com/public/thankyou_download.aspx?activity=download&campaignid=VBHNov2015
rob halkes's insight:
News about progress in development of Value Based Health Care from the Economist.
From retrospective to predictive to prescriptive analytics, healthcare organizations are embarking on analytics journeys to enhance medical outcomes.
rob halkes's insight:
Benchmark to your data analytics position!
The health systems we enjoy today, and expected medical advances in the future, will be difficult to finance from public resources without major reforms. Public health spending in OECD countries has grown rapidly over most of the last half century. These spending increases have contributed to important progress in population health: for example, life expectancy at birth has increased, rising on average by ten years since 1970. The challenge now is to sustain and enhance these achievements in a context of tight fiscal constraints in many countries combined with upward pressure on health spending from factors such as new technological advances and demographic changes. Finding policies that can make health spending more sustainable without compromising important achievements in access and quality requires effective co-operation between health and finance ministries. Sound governance and co-ordination mechanisms are therefore essential to ensure effective policy choices. Prepared by both public finance and health experts, this report provides a unique detailed overview of institutional frameworks for financing health care in OECD countries. One of the main features of this book is a comprehensive mapping of budgeting practices and governance structure in health across OECD countries.
rob halkes's insight:
OECD newest report on sustainability of health systems.
A lot of people ask me about the future of medicine and healthcare. What’s coming next, what about the future of radiology, genomics or health sensors. They ask me to make really sharp predictions. But instead of this, let’s do something else now. Let’s look back from 2050, and see what today’s healthcare included, what barbaric elements played an important role in today’s healthcare in the 2010s....
rob halkes's insight:
Chane perspectives on heakthcare as it is now. Put your status quo in a different view and ask yourself: what are we doing?
PLAINSBORO, N.J. (PRWEB) July 16, 2015 -- The link between getting patients to take medication correctly and keeping down healthcare costs is strong enough that adherence is being tied to reimbursement for healthcare providers. A study published recently in The American Journal of Managed Care examines connections at the health plan level between good plan-level adherence, lower rates of disease complications, and lower medical spending.
rob halkes's insight:
Interesting finding AJMC: there's a relation between quality of care (plans) with adherence to medication. It's one of the mysterious ways how taking on'e medicines is influenced by the providers way of engagement and conduct. So more need for attention by those providers and in depth research. It has to start with understanding patients' concerns, as there are: concerns about their conditions, concerns about their providers and about the medication itself: a battle field to win trust! See the article here
The leading hospital magazine for hospital business news and analysis for hospital and health system executives. Massachusetts General Hospital in Boston reclaimed the top spot on the Honor Roll for 2015-16, and there is a tie for No. 3. U.S. News & World Report has released its 2015-16 Best Hospital rankings, the 26th edition of its annual rankings. The following are six things to know about this year's rankings, including which organizations made the Honor Roll and landed in top spots for three major specialties. 1. Massachusetts General Hospital in Boston reclaimed the top spot on the Honor Roll this year, which is comprised of hospitals raking at or near the top in six or more specialties. Mass General was No. 2 on last year's Honor Roll. 2. Just 15 hospitals qualified for the Honor Roll this year by ranking at or near the top in six or more specialties. That's down from 17 in 2014-15's rankings. They are as follows, in rank order: 1. Massachusetts General Hospital (Boston)
Cancer care Cardiology & heart surgery Orthopedics 4. This year, 137 hospitals performed well enough in complex care to be nationally ranked in one of 16 specialties. Rankings for 12 of the specialties (cancer; cardiology & heart surgery; diabetes & endocrinology; ear, nose & throat; gastroenterology & GI surgery; geriatrics; gynecology; nephrology; neurology & neurology; orthopedics; pulmonology; and urology) are based on reputation, patient survival, patient safety and care-related factors. The remaining four specialties (ophthalmology, psychiatry, rehabilitation and rheumatology) are based on reputation alone, pulled from the three latest annual physician surveys.... Read on at the site!
rob halkes's insight:
Good news, knowing best hospitals. But we can see that quality rates of specific departments are better guides to select health services than overall hospital rate. Hosptals are challenged to do good in departments first ;-)
rob halkes's insight:
Great inspiring news to the health devices industry: PatientView's outcomes of the corporate reputation study amongst patient groups! Best 5? Coloplast, Roche Diagnostics, Medtronic, St.Jude Medical and ConvaTec. Last, at 28th: GE Healthcare..Read to know why and how!
Growth And Dispersion Of Accountable Care Organizations In 2015 | The Policy Journal of the Health Sphere March 31, 2015 In January, an additional 89 provider organizations joined the Medicare Shared Savings Program (MSSP) as accountable care organizations (ACOs). While this year’s new entrants are a smaller cohort than those that joined in 2013 and 2014, they represent a continuation of the expansion of the accountable care movement. The recent Department of Health and Human Services (HHS) announcement of its goal to move 50 percent of Medicare payments to alternative payment models (including ACO-based arrangements) indicates the government’s strong backing of the model and, coupled with continuing endorsement of the approach from state Medicaid programs and commercial insurers, there is strong support for this care delivery approach to continue. In an ACO, health care providers accept responsibility for the cost and quality of care for a defined population. Each ACO’s laudable goal is to achieve what Don Berwick has called the “triple aim” — to improve quality, increase patient satisfaction, and lower costs. The key to reaching those goals is to change how providers are paid, based on reaching certain cost and quality benchmarks. In effect, the objective is to change incentives so that it is in providers’ best interest to maximize health, rather than focus on increasing the volume of services rendered. ACO GrowthLeavitt Partners has been actively tracking ACOs since 2010, maintaining a database that is updated regularly from publicly available information and personal and industry interviews. Over the past year, approximately 120 organizations have become ACOs in public and private programs, bringing the total to 744 since 2011 (Figure 1). The historical ACO growth data shown in Figure 1 are slightly different from our past estimates, as they are now based on the start date of the ACO’s contract, not on when the ACO was announced. For example, the 89 ACOs announced in December 2014 are listed as beginning in January 2015, which is the start of their contract. Regardless of how many contracts an ACO is engaged in, both public and private, an ACO is counted only once. Note that some of the new Medicare Shared Savings Program participants already had commercial contracts, and are thus tracked beginning at the start of their first contract. Figure 1. Total Public and Private Accountable Care Organizations, 2011 to January 2015 (See top) Source: Leavitt Partners Center for Accountable Care Intelligence In addition to growth in the total number of ACOs, there has been continued growth in the number of people covered by ACO arrangements Read on the original blog here
rob halkes's insight:
Great overview of a trend in US to shared savings in healthcare by Accountable Care Organisations! I'm convinced these organisations will quickly turn to implementation of ehealth applications because fo the immanent strength to save costs and create more active self management by patients, two important sources for shared savings agreements!
White paper IMS: "Four Drivers of Successful Business Download
rob halkes's insight:
Not too often you find a good overview of the current implications of health data and big data for your institution of healthcare provision. I think IMS gives here a fair one!
This third edition of Health at a Glance: Europe presents a set of key indicators related to health status, determinants of health, health care resources and a
rob halkes's insight:
Very, insightful - I used these as background to the study of pharma's developments around "value added services" .. Will pharma have the competence to repositions itself as partner in health care rather than 'just' a supplier of drugs.
Healthcare is Headed Down a New Road with New Rules The healthcare industry is entangled in a transitory phase in which therapeutics, products and services are sold into traditional care settings that are saturated and exhausted. At the same time, opportunities for new services and care, such as ambulatory, mobile, and home care, lack the appropriate level of maturity to provide robust revenue streams. The webinar examines the degree to which we can expect the impact to take hold and transpire over the upcoming year. Preditctied trends for 2015 in healthcare:
Top trends: Pharma: Product as a service - Platform as a service - Data as a Service -
Top trends Medical technology - Is your healthcare in your smartphone -
rob halkes's insight:
Great insights of ongoing trends to health care! I guess it will be a year of intesifying trends and mutually influencing trends. The Overarching trends as I predicted it last year ( http://bit.ly/1icTOvZ ) "integration should be the trend of 2014", is obviously recognized!
Approximately $6.5 billion in new funding flowed into the digital health space in 2014, more than double the previous year's haul of $2.9 billion, according to data from digital healthcare accelerator StartUp Health. But investors placed their bets on fewer companies. Only 459 companies received funding this year, a drop from the 590 who received investments in 2013. The decrease in companies financed is one of the “signs of a maturing market,” StartUp Health says. Another sign may be the stage at which venture capitalists and firms are making investments in startups. According to StartUp Health's data, just over 25% of deals were in the seed capital stage, a very early stage in a company's development. That's the lowest percentage since 2010, and indicates that there are relatively fewer funded startup entrants in this year's cohort.
rob halkes's insight:
Indeed, the health care market is structurally changing, also due to the volume compnay's entering the health care place from new perspectives: computers (e.g. Apple), Smartphones (e.g. Samsung) and IT - software (e.g. McKesson).
rob halkes's insight:
To me about WatsonAnalytics by IBM, now open to everyine to use for their businesses, only tells me that in the coming future, nearby, we'll have Watson medical descision making, open for everyone.. What would that do to the business of health?
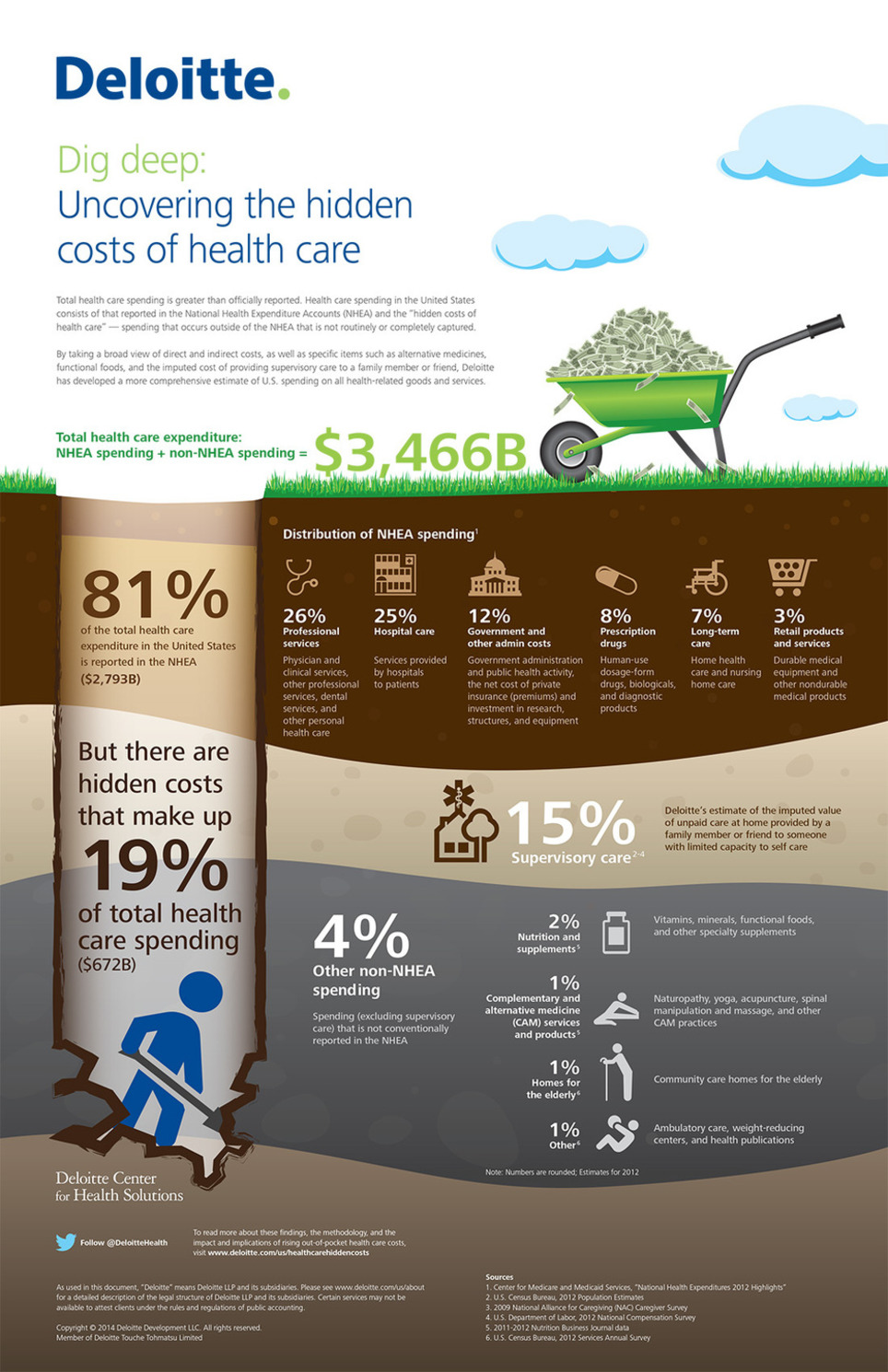
Dig deep: Increases in consumer health care OOP spending also impact hospitals, life sciences companies and health plans. How should stakeholders respond? Even though more consumers are gaining health insurance coverage, they are by no means insulated from the burden of health care costs. Consumers are paying more of their health plan premiums and experiencing higher out-of-pocket (OOP) cost-sharing for all types of health care services. Moreover, government estimates of health care spending do not take into account discretionary consumer spending on a number of products and services; Deloitte’s Hidden Costs Analysis shows these purchases add considerably to the total. OOP spending increases extend beyond consumers to impact hospitals, life sciences companies and health plans. What are the implications for these stakeholders? This report:
rob halkes's insight:
Hidden costs of health care: When governments all over the world tend to cut on costs of care because of the raising trends, consumers will run the risks of paying more for their care too. To all stakeholders insights into the drivers of costs of care is relevant. Politicians are challenged to look into it and make their choices of divide between stakeholders. Next step for them: how to regulate sustainable and affordable care by measures to development and improvement by means of:
Earlier this month, Kaiser Health News reported that "more hospitals are receiving penalties than bonuses in the second year of Medicare’s quality incentive program, and the average penalty is steeper than it was last year" (here). Kaiser wasn't the only troubling news that appeared recently for Americans who are 65 and older and rely on Medicare for their healthcare coverage.
Like The Commonwealth Fund report earlier this year (U.S. Healthcare Ranked Dead Last Compared To 10 Other Countries), this new survey used 11 countries for their comparative analysis. The survey was conducted from March through May of this year and the number of respondents for each country is indicated in parentheses...(see orgiginal post).. Perhaps the biggest surprise was the fact that older Americans (age 65+) said that cost was the primary reason for skipping medical care or treatment. This was significant because Medicare is often presumed to be free and universal health coverage for every American over the age of 65 [..]. The other big takeaway was the fact that older Americans had the highest prevalence of chronic conditions. The survey found that 87% of older Americans had at least one chronic health condition and 68% reported 2 or more chronic conditions. The next highest was Canada which reported 83% with at least one chronic condition and 56% with 2 or more. Whether this is the result of delayed healthcare or other socioeconomic factors is unknown and was also outside the scope of the survey.... For further reading see original post..!
rob halkes's insight:
Great insights. Desiging and improving nations' systems of Health Care is not an easy task: we don't know to much of the specific interests of the several and different stakeholders, like patients payers, industry and health care providers! Leave alone that we don't know too much about their interests and inclination to work together! It can't be left to governments by themselves, leave alone to politicians! ;-)
The applications at the start of the three-month enrollment period showed that in contrast to initial problems last year, HealthCare.gov was working.
rob halkes's insight:
Good! ;)
This fact sheet describes the results of research into the factors influencing physician professional satisfaction and their implications for health care. The American Medical Association (AMA) asked RAND Health to identify the factors that influence physicians' professional satisfaction and describe their implications for the U.S. health care system. To do this, the researchers interviewed and surveyed physicians, allied health professionals, and other staff in 30 practices across six states, including a variety of practice sizes, specialties, and ownership models. Among the factors identified, two stood out as the most novel and important:
rob halkes's insight:
Physicians do want to go on and innovate to better care. In my opinion the dominant issues are:
In my experience that's conditional; it has suprised me how a lot of them are prepared to go all the way to innovate and improve quality of care to patients!
World Health Organization Regional Office for Europe Health spending continues to outstrip the economic growth of most member countries of the Organisation for Economic Co-operation and Development (OECD). Pay for performance (P4P) has been identified as an innovative tool to improve the efficiency of health systems but evidence that it increases value for money, boosts quality or improves health outcomes is limited. Using a set of case studies from 12 OECD countries (including Estonia, France, Germany, Turkey and the United Kingdom), this book explores whether the potential power of P4P has been over-sold, or whether the disappointing results to date are more likely to be rooted in problems of design and implementation or inadequate monitoring and evaluation. Each case study analyses the design and implementation of decisions, including the role of stakeholders; critically assesses objectives versus results; and examines the “net” impacts, including positive spillover effects and unintended consequences. See the publication by McGrawHill here
rob halkes's insight:
Pay for Performance is a popular thought to found the system of reimbursement to health care. It is good to see reserach evaluating the thought. I myself have seen cases in which under the flag of this P4P concept and the idea that within smaller regions things would be easier to control, things did not work out. Performance in health care is not a simple idea to operationalize, without relating to the rich-poor issue, the quality of providers, the local inclination for different epidemeologies, etc. I for one would rather focus on health outcomes to begin with.
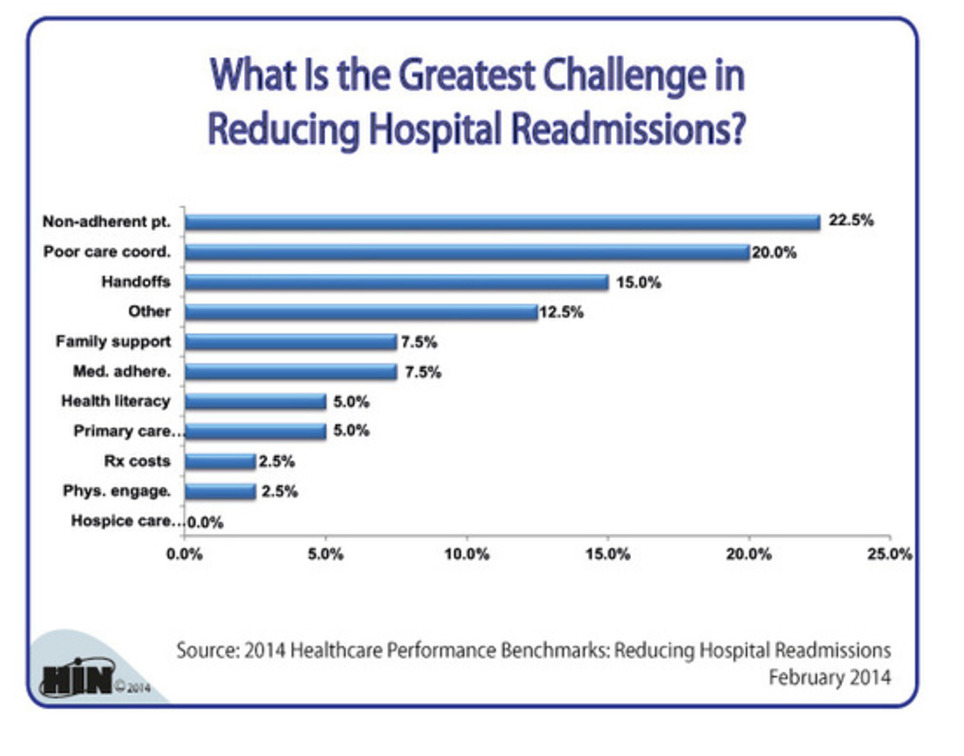
While great strides have been made in the reduction of 30-day all-cause hospital readmissions, CMS still penalized more than 2,200 hospitals in 2013 for exceeding 30-day readmission rates for heart failure, pneumonia and myocardial infarction. In 2015, CMS penalties will extend to acute COPD and elective hip and knee replacements. 2014 Healthcare Benchmarks: Reducing Hospital Readmissions documents the latest key initiatives and partnerships to reduce readmissions by patients with these costly conditions and others by more than 100 healthcare organizations. Development of post-acute partnerships with home health, skilled nursing facilities (SNFs) and hospice is emerging as a key strategy to stem hospital readmissions, according to new market data from the fourth annual Healthcare Intelligence Network (HIN) Reducing Hospital Readmissions Survey. More than half of survey respondents participate in post-acute partnerships, with home health collaborations the most common (79 percent). These partnerships serve to streamline processes and care transitions, educate and align staff, and implement changes of value to patients, respondents say. Looking at more conventional approaches, medication reconciliation and telephonic monitoring of patients post-discharge emerged as frontrunner strategies to curb readmissions. Moreover, the 2013 survey revealed significant upticks in the use of each tactic over 2012 levels: medication reconciliation is now conducted by 73 percent of respondents, versus 54 percent in 2012, while the use of telephonic monitoring jumped from 48 to 71 percent over the same 12-month period. In other new data, almost half of respondents — 47 percent — aim programs at individuals already assessed at high risk for readmission as well as the traditional Medicare (53 percent), Medicaid (28 percent) and high utilizer (23 percent) populations.
rob halkes's insight:
Preventing readmissions - The pictured graph speaks for itself . It also turns out that any attention to discharged patients will have effect on prevention of readmissions, IF the hospital organizes the attention. SImple telephinci monitoring already contributes, leave alone what structural ehealth applications will mean! See also here!
Governance for health describes the attempts of governments and other actors to steer communities, whole countries or even groups of countries in the pursuit of health as integral to well-being. This study tracks recent innovations to address the priority determinants of health and categorizes them into five strategic approaches to smart governance for health. It relates the emergence of joint action by the health and non-health sectors, public and private actors and citizens, all of which have increasing roles to play in achieving seminal changes in 21st-century societies. "Built upon an understanding of health and the contexts that drive new governance, it is proposed that smart governance for health is composed of five interrelated aspects:
Each of these aspects interacts and manifests differently, depending on the contexts in which they are set." (see page 143 of publication) See more information and a free download here
rob halkes's insight:
Great reading about governance to health - specifically in the current times of digital disruption, higher demands, reshuffle of powers, technological development and ever rising costs. WHO Europe has published an inspiring read!
August 29, 2014- Detroit Medical Center Awarded National Health Care Innovation Award The Detroit Medical Center (DMC) has been selected to receive an award of $9,966,608 as part of the Centers for Medicare and Medicaid Services’ (CMS) Health Care Innovation Awards program. The Principal Investigator and DMC Chief Medical Officer Dr. Suzanne White is one of only 39 recipients of about 3,000 applicants across the United States. The award will enable the DMC to test an innovative primary care and preventative health model that reaches patients who use some of Detroit’s busiest emergency departments. The project, entitled Gateway to Health: An Innovative Model for Primary Care Expansion in Detroit, will make patient-centered medical care immediately accessible to individuals without existing primary care physicians, arriving to four DMC emergency departments at DMC Harper University Hospital, DMC Detroit Receiving Hospital, DMC Sinai-Grace Hospital and DMC Children’s Hospital of Michigan. By embedding primary care services in those areas of highest emergency department use, the DMC project intends to meet patients where they are already seeking care to develop meaningful doctor-patient relationships, improve care coordination and implement strategies to promote wellness. The ultimate goals are to deliver improved health care access, quality and efficiency for the surrounding community. “As a Detroit emergency physician, I understand the challenges and barriers our patients face as they try to access high quality primary care services. I see each day how the system could be improved. Patients lack access to after hours care, unscheduled visits, transportation, and most importantly, a welcoming environment where they feel comfortable and safe,” said Dr. White. “This award is an incredible opportunity for DMC to create a culture of patient partnership, where we start by listening to each patient's story, try to understand their unique challenges and goals, and then match them with the best health caremore team.”
|





























Sustainability gets higher relevance in investors' policy. This research from MIT/BCG points out the significance of this development for the health care industry.