Your new post is loading...
 Your new post is loading...
The AI, trained on around 13,000 fundus images from over 600 Alzheimer's patients, has demonstrated up to 92% accuracy.
Via Emmanuel Capitaine
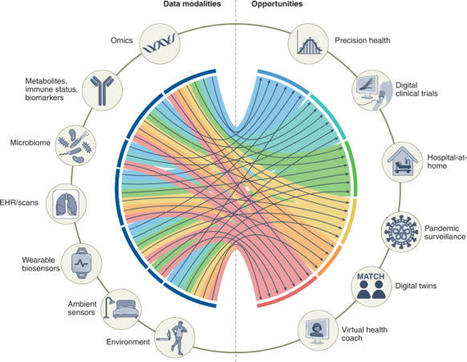
Clinical decision-making in oncology is challenging and requires the analysis of various data types – from medical imaging and genetic information to patient records and treatment guidelines.
Via Emmanuel Capitaine
Behavioral health doesn’t need tech that replaces people. It needs technology that respects them, amplifying what clinicians do best and helping more people get the care they deserve.
Via Emmanuel Capitaine
There have been extensive evaluations of artificial intelligence (AI) systems for
narrow medical tasks, but more work is needed to systematically evaluate and deploy
AI systems that can perform a broad range of medical tasks. The medical training process
itself might offer a template for addressing this challenge. Clinicians undergo rigorous
education and training, progressing through stages of increasing responsibility and
autonomy. Similarly, generalist medical AI systems could be subjected to a phased
certification model before they are granted greater autonomy in patient care.
Electronic health records (EHRs) have become nearly universal in the United States, enhancing care coordination and patient access to health data. However, these advancements have introduce
The offering measures AI's real-world performance and safety around handling realistic medical conversations, using physician-created rubrics and GPT-4.1 scoring.
Découvrez huit startups accompagnées par le Startup Program d’OVHcloud qui réinventent dès aujourd’hui les solutions de santé de demain
This perspective provides a critical framework for evaluating the use of Generative AI (GenAI) in healthcare, informed by two roundtable events and a series of semi-structured expert interviews. By outlining key principles and risks—including mapping applications to GenAI strengths, ensuring rigorous evaluation frameworks, and fostering transparency and collaboration—it will support healthcare professionals and policymakers in navigating the ethical and impactful integration of GenAI into healthcare.
Voice recordings, examined by artificial intelligence, might provide new biomarkers for conditions such as heart disease and Alzheimer’s.
AI-powered start-ups such as ReportAId, which has raised $2.2 million of new funding, are focusing on the power of technology to reduce manual processes in healthcare...
Via Emmanuel Capitaine
|
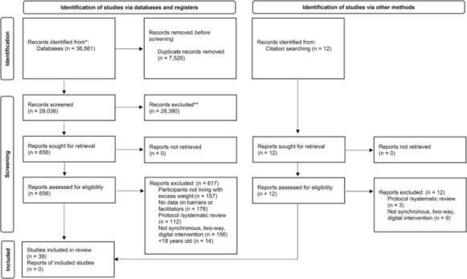
Obesity rates are continually rising and remote weight management interventions appear to demonstrate feasible prospects. Previous reviews have investigated influential factors to engagement of such interventions in community settings; however, limited research has examined adults’ engagement in...
Via Emmanuel Capitaine
Neurological conditions, including dementia, pose a major public health challenge, contributing to a significant and growing clinical, economic, and societal burden. Traditionally, research and clinical practice have focused on diseases like dementia in isolation.
Via Emmanuel Capitaine
In a landmark comparative study published in the Journal of Health Organization and Management, researchers from the University of Maine have embarked on a rigorous investigation to evaluate the diagnostic capabilities of artificial intelligence (AI) models against those of seasoned human clinicians...
Via Emmanuel Capitaine
Alors que 80 % des dépenses de santé sont dédiées au curatif, 3 % profitent à la prévention. Comment inverser la tendance ? « Pour accompagner le passage du curatif vers le préventif, nous savions que l’innovation allait jouer un très grand rôle. C’est pourquoi nous avons monté un “accélérateur prévention” », explique Chahra Louafi, directrice du fonds Patient autonomie de Bpifrance, partie prenante de ce programme d’accompagnement de start-up lancé en septembre 2024. Mi-mai, un bilan de la première promotion a été présenté au sein de PariSanté campus.
The governance of generative artificial intelligence (AI) technologies in medicine
has become a major topic of discussion due to concerns about their rapid development
and use, which have outpaced existing regulatory measures.1 Findings from a recent
large-scale survey underscore the urgency of renewed oversight, revealing that one
(20%) in five of the UK-based general practitioners surveyed use large language model
(LLM) chatbots for clinical tasks.2 Although much attention has been focused on popular
and widely available LLM-based chatbots, such as ChatGPT (OpenAI and Microsoft), addressing
unresolved challenges related to privacy, bias, accuracy, and accountability requires
a standardised frameworks that goes beyond the regulation of chatbot as conversational
tools and considers the wider AI capabilities for data generation.
Il s'agit à la fois d'une discrimination de conception et d’usage.
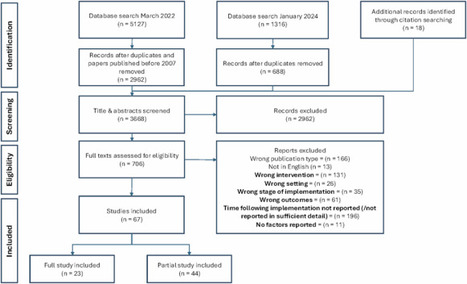
Existing reviews have identified factors influencing Clinical Decision Support (CDS) adoption by clinicians in practice but overlook the dynamic and evolving nature of technology and users’ needs over time. This review aimed to identify factors that influence early, mid-term, and sustained acceptance and use of CDS in hospital settings. Five databases were searched from 2007 to January 2024 and 67 papers were included. Factors were extracted and synthesised according to the time that data were collected following CDS implementation. Factors relating to the CDS intervention (e.g. utility) and inner setting (e.g. fit with workflows) were reported across all time periods. Perceived outcomes were more often identified in the first year of use, and individual factors after the first 6 months of use. Strategies to work around CDS limitations were reported 5 years after implementation. Our review provides guidance for developing, implementing, and supporting ongoing use of CDS systems.
This marks one of the most ambitious attempts yet to embed AI deep within a regulatory agency.
Alors que l’on célèbre cette année les 80 ans de la Sécurité sociale, les inquiétudes sur la soutenabilité de notre système de soins se multiplient. Le déficit de la branche maladie atteint un niveau record hors crise sanitaire, alors qu’un mur démographique et épidémiologique se profile à l’horizon. Les solutions purement comptables et les facilités de court terme ne permettront ni de résoudre l’équation financière ni de relever les défis qui se présentent. Un autre modèle est à inventer. Selon Nicolas Revel, il doit se construire autour d’une nouvelle organisation du suivi des pathologies chroniques et faire le pari de la qualité des soins comme vecteur essentiel d’attractivité pour les soignants et de maîtrise des dépenses de santé. Alors que l’on célèbre cette année les 80 ans de la Sécurité sociale, les inquiétudes sur la soutenabilité de notre système de soins se multiplient. Le déficit de la branche maladie atteint un niveau record hors crise sanitaire, alors qu’un mur démographique et épidémiologique se profile à l’horizon. Les solutions purement comptables et les facilités de court terme ne permettront ni de résoudre l’équation financière ni de relever les défis qui se présentent. Un autre modèle est à inventer. Selon Nicolas Revel, il doit se construire autour de la problématique des pathologies chroniques et faire le pari de la qualité des soins comme vecteur essentiel d’attractivité pour les soignants et de maîtrise des dépenses de santé.
Les investisseurs affluent, les fonds se multiplient, les deals s'enchaînent. Pourtant, beaucoup d'entrepreneurs français passent encore à côté.
HealthBench doit aider dans l'évaluation de la sécurité et des performances des grands modèles de langage dans le domaine de la santé. En...-IA générative
This follows the clearance for heart rate measurement on the FaceHeart mobile app in 2023.
Via Emmanuel Capitaine
|





 Your new post is loading...
Your new post is loading...