Your new post is loading...

|
Scooped by
Juan Lama
February 24, 2:12 PM
|
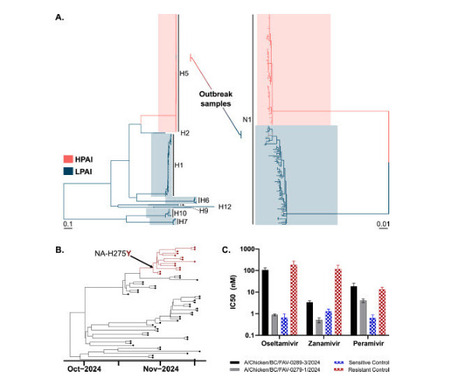
We report the detection of a clade 2.3.4.4b A(H5N1) reassortant virus with a neuraminidase surface protein derived from a North American lineage low-pathogenic avian influenza virus. This virus caused a widespread and ongoing outbreak across 45 poultry farms in British Columbia, Canada. Isolates from 8 farms reveal a mutation in the neuraminidase protein (H275Y) that is exceptionally rare among clade 2.3.4.4b viruses (present in 0.045% of publicly available clade 2.3.4.4b isolates). NA-H275Y is a well-known marker of resistance to the neuraminidase inhibitor oseltamivir. We demonstrate that this substitution maintains its resistance phenotype on the genetic background of H5N1 clade 2.3.4.4b viruses. Published in Emerging Microbes and Infections (Feb.18, 2025): https://doi.org/10.1080/22221751.2025.2469643

|
Scooped by
Juan Lama
February 23, 12:49 PM
|
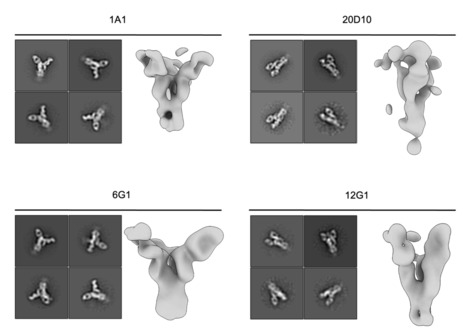
The highly pathogenic avian influenza H5N1 virus clade 2.3.4.4b has been spreading globally since 2022, causing mortality and morbidity in domestic and wild birds and mammals, including infection in humans, raising concerns about its pandemic potential. We aimed to generate a panel of anti-hemagglutinin (HA) human monoclonal antibodies (mAbs) against the H5 protein of clade 2.3.4.4b. H2L2 Harbour Mice, which express human immunoglobulin germline genes, were immunized with H5 and N1 recombinant proteins from A/mallard/New York/22-008760-007-original/2022 H5N1 virus, enabling the generation of human chimeric antibodies. Through hybridoma technology, sixteen full human mAbs were generated, most of which showed cross-reactivity against H5 proteins from different virus variants. The functionality of the sixteen mAbs was assessed in vitro using hemagglutination inhibition and microneutralization assays with viruses containing a clade 2.3.4.4b HA. Fourteen out of the sixteen mAbs neutralized the virus in vitro. The mAbs with the strongest hemagglutination inhibition activity also demonstrated greater neutralizing capacity and showed increased protective effects in vivo when administered prophylactically or therapeutically in a murine H5N1 challenge model. Using cryo-electron microscopy, we identified a cross-clonotype conserved motif that bound a hydrophobic groove on the head domain of H5 HA. Akin to mAbs against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during the coronavirus 2019 (COVID-19) pandemic, these mAbs could serve as important treatments in case of a widespread H5N1 epidemic or pandemic. Preprint in bioRxiv (February 21, 2025): https://doi.org/10.1101/2025.02.21.639446

|
Scooped by
Juan Lama
February 22, 10:13 AM
|
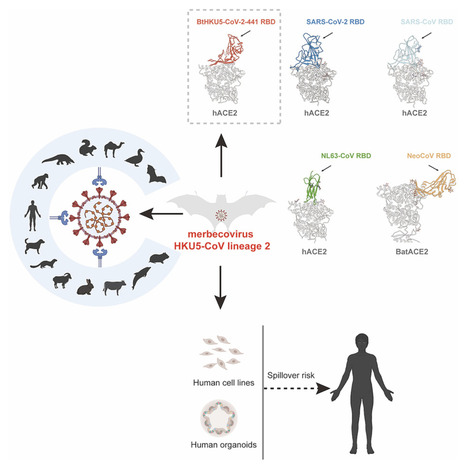
Highlights • A distinct HKU5 coronavirus lineage (HKU5-CoV-2) is discovered in bats • Bat HKU5-CoV-2 uses human ACE2 receptor and ACE2 orthologs from multiple species • Bat HKU5-CoV-2 RBD engages human ACE2 with a distinct binding mode from other CoVs • Bat HKU5-CoV-2 was isolated and infect human-ACE2-expressing cells Summary Merbecoviruses comprise four viral species with remarkable genetic diversity: MERS-related coronavirus, Tylonycterisbat coronavirus HKU4, Pipistrellusbat coronavirus HKU5, and Hedgehog coronavirus 1. However, the potential human spillover risk of animal merbecoviruses remains to be investigated. Here, we reported the discovery of HKU5-CoV lineage 2 (HKU5-CoV-2) in bats that efficiently utilize human angiotensin-converting enzyme 2 (ACE2) as a functional receptor and exhibits a broad host tropism. Cryo-EM analysis of HKU5-CoV-2 receptor-binding domain (RBD) and human ACE2 complex revealed an entirely distinct binding mode compared with other ACE2-utilizing merbecoviruses with RBD footprint largely shared with ACE2-using sarbecoviruses and NL63. Structural and functional analyses indicate that HKU5-CoV-2 has a better adaptation to human ACE2 than lineage 1 HKU5-CoV. Authentic HKU5-CoV-2 infected human ACE2-expressing cell lines and human respiratory and enteric organoids. This study reveals a distinct lineage of HKU5-CoVs in bats that efficiently use human ACE2 and underscores their potential zoonotic risk. Published in Cell (Feb. 18, 2025)

|
Scooped by
Juan Lama
February 19, 10:55 AM
|
The U.S. Department of Agriculture on Tuesday acknowledged it accidentally fired "several" employees to combat the bird flu and is working to rehire them. The U.S. Department of Agriculture said Tuesday that, over the weekend, it accidentally fired "several" agency employees who are working on the federal government's response to the H5N1 avian flu outbreak. The agency said it is now trying to quickly reverse the firings. "Although several positions supporting [bird flu efforts] were notified of their terminations over the weekend, we are working to swiftly rectify the situation and rescind those letters," a USDA spokesperson said in a statement. "USDA’s Food Safety and Inspection Service frontline positions are considered public safety positions, and we are continuing to hire the workforce necessary to ensure the safety and adequate supply of food to fulfill our statutory mission." The spokesperson noted that several agency positions were already exempted from the sweeping cuts President Donald Trump's administration is making across the federal government, adding that the Agriculture Department "continues to prioritize the response to highly pathogenic avian influenza." The error is the latest in the Trump administration's attempts to rapidly shrink the size of the government by conducting mass firings of federal workers — an effort that is being carried out by tech billionaire Elon Musk and the U.S. Department of Government Efficiency, which is heavily staffed by people who have no experience in government. On Friday, the administration tried to notify some nuclear safety employees who were fired last week that they are now due to be reinstated — but struggled to find them because they didn’t have their new contact information. The latest episode comes as the virus has decimated poultry flocks and has sent egg prices soaring. The Centers for Disease Control and Prevention confirmed 68 cases among humans in the U.S. so far. On her first day in office, Agriculture Secretary Brooke Rollins convened a panel on bird flu and "reviewed options for a comprehensive strategy to combat it," the department said in a release. Several agencies within the Agriculture Department play a role in responding to the outbreak, including the Agricultural Research Service and the Animal and Plant Health Inspection Service. On Sunday, Politico reported that some of the Trump administration's layoffs hit the National Animal Health Laboratory Network, which is involved in avian flu research. The layoffs concerned a number of Republican lawmakers, who privately warned the Trump administration that such cuts could hamper the government’s bird flu response and asked them to reconsider, according to two Republican sources with direct knowledge of the situation. Lawmakers had received little guidance from the administration about the recent program cuts and staff terminations at USDA, which sources said has frustrated Republicans on the House Agriculture Committee. The panel, which oversees the USDA, provided a briefing to its members over the weekend to try to provide some more clarity to lawmakers. “They need to be more cautious,” Rep. Don Bacon, R-Neb., a member of the Agriculture Committee, told NBC News of the DOGE team. “There’s an old saying, ‘Measure twice, cut once.’ Well, they are measuring once and having to cut twice. Some of this stuff they’re going to have to return back. I just wish they’d make a better decision up front.” The layoffs also concerned researchers working on bird flu. Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory, said that the firing of three employees at the USDA’s National Animal Health Laboratory Network program would hurt efforts to combat the spread of the virus. “It’s creating a lot of problems,” he said. Egg prices, which were already high, have continued to soar as the bird flu has spread. Several committee members, who were back in their districts this week, told NBC News they are hearing an earful from constituents over the sky-high price of eggs. Republicans on the House Agriculture Committee have raised their concerns to the chairman, Rep. Glenn "GT" Thompson, R-Pa., and his staff, who have been working to relay those concerns to the USDA and obtain more information about the moves, sources said. In a statement to NBC News, Thompson expressed broad support for the DOGE mission. “With Secretary Rollins now confirmed, we anticipate further clarity on the status of this review across USDA mission areas,” Thompson said in a statement. Some Republicans have also complained about cuts to a program that works with poultry farmers to reduce the number of birds around airports in an effort to enhance aviation safety. And more broadly, there is uncertainty over how widespread funding cuts across the government, as well as new restrictions on funding for National Institutes of Health grants, may affect infectious disease researchers and local health officials working to respond to the bird flu Latest data from USDA shows 151 confirmed flocks have been hit, affecting 23 million birds. In recent days, the Trump administration has fired probationary employees across the government — a move that could affect hundreds of thousands of people, according to data from the Office of Personnel Management. An agency spokesperson said the administration would not be able to provide full details on how many individuals were fired until Tuesday evening. Probationary status typically applies to someone who has been with the federal government for less than two years — before full civil service protections kick in. But it can also apply to longtime civil service workers who move to a different agency or take a promotion. The Trump administration has cited "performance" issues in letters to fired employees explaining why they were let go — though some of those same employees have received strong performance reviews from their superiors.

|
Scooped by
Juan Lama
February 16, 10:30 AM
|
With egg prices in the United States soaring because of the spread of H5N1 influenza virus among poultry, the U.S. Department of Agriculture (USDA) yesterday conditionally approved a vaccine to protect the birds. President Donald Trump’s administration may therefore soon face a fraught decision on whether to join the ranks of other nations—including China, France, Egypt, and Mexico—that vaccinate poultry against H5N1. Although many influenza researchers contend that vaccination can help control spread of the deadly virus, the U.S. government has long resisted allowing its use because of politics and trade concerns that many contend are unscientific. The USDA approval may signal a shift in policy linked to the Trump administration’s worries about egg prices. Even with the conditional approval, USDA must still approve its use before farmers can start to administer the vaccine because special regulations apply to H5N1 and other so-called highly pathogenic avian influenza (HPAI) viruses. The vaccine, made by Zoetis, contains a killed version of an H5N2 variant that the company has designed to work against circulating variants of the H5N1 virus that have decimated poultry flocks and have even jumped to cows and some humans. (The “H” in both variants stands for hemagglutinin, the surface protein of the virus, and antibodies against it are the main mechanism of vaccine-induced protection.) Researchers at the U.S. Centers for Disease Control and Prevention reported yesterday that three cow veterinarians harbored antibodies to the H5N1 virus in dairy cattle. None had symptomatic disease, they noted in the Morbidity and Mortality Weekly Report, suggesting the virus may be more widespread in humans than previously thought. Zoetis CEO Kristin Peck announced the approval yesterday on CNBC. “The decision to vaccinate commercial poultry flocks rests solely with national regulatory authorities in consultation with their local poultry sector,” said Zoetis in a statement, which noted it has approval for similar vaccines in other countries. Zoetis also had an earlier version approved in 2016 that was in the National Veterinary Stockpile until 2021, but it was never used. HPAI strains such as the current H5N1 have for decades been stamped out largely by culling affected flocks and enforcing strict biosecurity measures. But that strategy has failed since the February 2022 emergence in the U.S. of an H5N1 virus that belongs to a lineage known as clade 2.3.4.4b. Many scientists now worry the virus cannot be eradicated from the U.S. poultry flock, which means it has become endemic rather than epidemic. “The future of H5 in the Americas isn’t entirely clear, but endemicity looks likely,” says Richard Webby, a bird flu investigator at St. Jude Children’s Research Hospital. “Updated and quality H5 vaccines for poultry must be a big part of future responses if this is indeed the case.”

|
Scooped by
Juan Lama
February 13, 1:53 PM
|
The vets had no symptoms, and one worked only in states where no dairy infections had been reported. Three dairy veterinarians, including one who worked only in states with no known bird flu outbreaks in cows, had recent, undetected bird flu infections, according to a new study from the Centers for Disease Control and Prevention. The results are based on antibody testing of 150 veterinarians working in 46 U.S. states. The findings were not entirely surprising, experts said, but did suggest that the virus, known as H5N1, could be infecting cows and people in more states than have been officially reported. “We do not know the extent of this outbreak in the U.S.,” said Seema Lakdawala, a virologist at Emory University. “There are clearly infections happening that we’re missing.” Since the bird flu outbreak in dairy cows was first reported last March, the virus has been confirmed in more than 950 herds in 16 states. It has also been detected in 68 people, 41 of whom had contact with sick cows. Most people have had mild symptoms. The new study, which was published in the C.D.C.’s flagship Morbidity and Mortality Weekly Report, was initially slated for publication several weeks ago but was delayed by the Trump administration’s pause on public communications from health and science agencies. “It’s important for public health preparedness that we have this data,” said Dr. Nahid Bhadelia, the director of the Boston University Center on Emerging Infectious Diseases.... REsearch Cited published in tje MMWR Journal of the CDC (Feb. 13, 2025): http://dx.doi.org/10.15585/mmwr.mm7404a2

|
Scooped by
Juan Lama
February 13, 1:23 PM
|
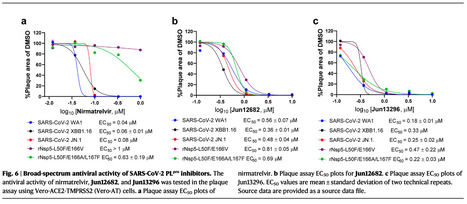
The ever-evolving SARS-CoV-2 variants necessitate the development of additional oral antivirals. This study presents the systematic design of quinoline-containing SARS-CoV-2 papain-like protease (PLpro) inhibitors as potential oral antiviral drug candidates. By leveraging the recently discovered Val70Ub binding site in PLpro, we designed a series of quinoline analogs demonstrating potent PLpro inhibition and antiviral activity. Notably, the X-ray crystal structures of 6 lead compounds reveal that the 2-aryl substitution can occupy either the Val70Ub site as expected or the BL2 groove in a flipped orientation. The in vivo lead Jun13296 exhibits favorable pharmacokinetic properties and potent inhibition against SARS-CoV-2 variants and nirmatrelvir-resistant mutants. In a mouse model of SARS-CoV-2 infection, oral treatment with Jun13296 significantly improves survival, reduces body weight loss and lung viral titers, and prevents lung tissue damage. These results underscore the potential of quinoline PLpro inhibitors as promising oral SARS-CoV-2 antiviral candidates, instilling hope for the future of SARS-CoV-2 treatment. The SARS-CoV-2 papain-like protease inhibitor, Jun13296, displays potent oral antiviral efficacy in a mouse model of SARS-CoV-2 infection and inhibits SARS-CoV-2 variants and nirmatrelvir-resistant mutants, rendering it a promising antiviral candidate. Published in Nature Communications (Feb. 13, 2025): https://doi.org/10.1038/s41467-025-56902-x

|
Scooped by
Juan Lama
February 11, 12:19 PM
|
Bird flu is infecting more people than we think. We need to stop it now before a new pandemic begins. Right after President Donald Trump took office, amid the flurry of executive orders and agency upheavals, the administration told the Centers for Disease Control and Prevention not to release any reports or communications until one of Trump’s people could take a look at them. Among the many reports not released that week was a study on how many veterinarians had gotten bird flu. On the surface, this might seem like a small thing compared to the drama unfolding over tariffs, immigration, the firings of inspectors general and whatever new, egregious thing Elon Musk is doing without congressional approval. But this report matters. The H5N1 bird flu virus has been on the warpath since 2022, infecting chickens, cows, wild birds and now pigs, ducks, cats and several other animals. This virus is versatile. This virus is mutating. And it is surely infecting more people than we think. Sure, the risk of a human epidemic is still considered low. (Sound familiar?) Widespread human-to-human disease hasn’t been proven. But viruses are masters of adaptation—a strain of bird flu that has made people really sick has now been found in cows. We are one fateful mutation away from yet another infectious disease that runs riot among people, and our country has just reelected a president who doesn’t just discount public health, but actively thwarts it. Robert F. Kennedy, Jr., who would run our biggest health care agency, has not publicly walked back his antivaccine sentiments. The doctors who would run the Food and Drug Administration and the National Institutes of Health both decried common sense infection control during COVID. Our agricultural and food safety systems are riddled with loopholes that have allowed this virus to spread. We’ve seen this movie before. Millions of people have died in the COVID pandemic that began under Trump’s watch. The Biden administration missed key opportunities to stop bird flu’s spread. As a nation, we still have not recovered from the physical, mental and social toll of COVID. What will happen if bird flu starts coursing through us? In January U.S. poultry producers killed a staggering 14 million egg-laying hens. In December 2024, that number was 13.2 million. Avian influenza not only spreads quickly; it kills quickly too—usually within a couple of days. When poultry producers find infected birds, whether in tight cages or roaming free-range, they basically get paid to kill the entire flock to try and slow down the disease. This is how we have managed avian flu in the past. History gives us reason for pessimism. The Trump administration and red-state officials had no problem downplaying the number of people who had COVID. If H5N1 becomes more transmissible, will we do the same again? This is why that report on veterinarians is important—the question isn’t if they are getting infected, it’s how many. If we want to understand how this virus spreads and how it may morph into something dangerous to humans, we need open, unvarnished data. Slowing the flow of communication increases the flow of disease. The pause on CDC communications was supposed to lift on Feb. 1. The report still hasn’t been released. Before Biden left office, HHS gave Moderna $590 million to make an mRNA-based vaccine for bird flu, calling it a move to strengthen pandemic preparedness. We have an H5N1 vaccine stockpile—but farmworkers aren’t getting it. Do we have any faith that RFK, Jr., will push to authorize either the stockpile or Moderna’s offering? This is the man who tried to stop the availability of COVID vaccines at the height of the pandemic. As the Trump administration slashes and burns federal government, as his cronies take the helms of agencies designed to uphold the health and welfare of both humans and the animals we use for food, I’m preparing for a repeat of their COVID response. Maybe we will be lucky and fewer people will die. But we didn’t have to get sick in the first place. My partner made a joke the other day about fixing himself a $50 omelet. A couple of days ago, Waffle House announced a price hike. So much for bringing grocery prices down. Eggs feed millions of Americans. We’ve long known that public health is an economic issue. Right now, it is decidedly a political one, too. Let’s see if the administration will at least act on that. This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.

|
Scooped by
Juan Lama
February 8, 10:40 AM
|
New York on Friday ordered a weeklong shutdown of all live bird markets in New York City, Westchester and Long Island after seven cases of avian flu were detected at bird markets in the city. Gov. Kathy Hochul said there is no immediate threat to public health and that the temporary closure of bird markets comes out of an abundance of caution. No cases of avian flu have been detected among humans in New York, officials said. The order came after seven cases of bird flu were found in poultry during routine inspections of live bird markets in the New York City boroughs of the Bronx, Brooklyn and Queens. The U.S. Centers for Disease Control and Prevention has said the virus poses low risk to the general public. The agency said there have been 67 confirmed cases of bird flu in humans in the U.S., with illnesses mild and mostly detected among farmworkers who were exposed to sick poultry or daily cows. The first bird flu death in the U.S. was reported last month in Louisiana, with health officials saying the person was older than 65, had underlying medical problems and had been in contact with sick and dead birds in a backyard flock. In New York, live bird markets where the virus was detected have to dispose of all poultry in a sanitary manner, according to the order. Other bird markets that do not have cases will have to sell off remaining poultry, clean and disinfect and then remain closed for at least five days and be inspected by state officials before reopening. The H5N1 strain of bird flu has been spreading among wild birds, poultry, cows and other animals. Officials have urged people who come into contact with sick or dead birds to wear respiratory and eye protection and gloves when handling poultry.

|
Scooped by
Juan Lama
February 7, 11:12 AM
|
The data, which appeared fleetingly online on Wednesday, confirmed transmission in two households. Scientists called on the agency to release the full report. Cats that became infected with bird flu might have spread the virus to humans in the same household and vice versa, according to data that briefly appeared online in a report from the Centers for Disease Control and Prevention but then abruptly vanished. The data appear to have been mistakenly posted but includes crucial information about the risks of bird flu to people and pets. In one household, an infected cat might have spread the virus to another cat and to a human adolescent, according to a copy of the data table obtained by The New York Times. The cat died four days after symptoms began. In a second household, an infected dairy farmworker appears to have been the first to show symptoms, and a cat then became ill two days later and died on the third day. The table was the lone mention of bird flu in a scientific report published on Wednesday that was otherwise devoted to air quality and the Los Angeles County wildfires. The table was not present in an embargoed copy of the paper shared with news media on Tuesday, and is not included in the versions currently available online. The table appeared briefly at around 1 p.m., when the paper was first posted, but it is unclear how or why the error might have occurred. The virus, called H5N1, is primarily adapted to birds, but it has been circulating in dairy cattle since early last year. H5N1 has also infected at least 67 Americans but does not yet have the ability to spread readily among people. Only one American, in Louisiana, has died of an H5N1 infection so far. The report was part of the C.D.C.’s prestigious Morbidity and Mortality Weekly Report, which, until two weeks ago, had regularly published every week since the first installment decades ago. But a communications ban on the agency had held the reports back, until the wildfire report was published on Wednesday. Experts said that the finding that cats might have passed the virus to people was not entirely unexpected. But they were alarmed that the finding had not yet been released to the public.

|
Scooped by
Juan Lama
February 5, 11:18 AM
|
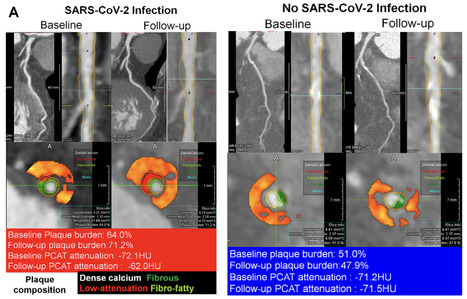
Background Patients with acute SARS-CoV-2 infection are reportedly at increased risk for future cardiovascular events; the mechanism underlying this risk remains unclear. Purpose To evaluate the impact of SARS-CoV-2 infection on coronary inflammation and plaques by using coronary CT angiography (CCTA) and the impact on clinical outcomes. Materials and Methods This retrospective analysis of a prospective study included consecutive patients who underwent serial CCTA between September 2018 and October 2023. The quantitative total and compositional percent atheroma volume (PAV) and annualized PAV change, presence of high-risk plaque, and attenuation of lesion-specific pericoronary adipose tissue (PCAT) at baseline and follow-up were compared between lesions in patients with and without SARS-CoV-2 infection. Relationships between SARS-CoV-2 infection and target lesion failure, which is a composite of cardiac death, target lesion myocardial infarction, and clinically driven target lesion revascularizations, were assessed with Cox models and log-rank tests. Results In 803 patients (mean age, 63.9 years ± 10.1 [SD]; 543 [67.6%] male patients), 2108 coronary artery lesions were evaluated in patients with SARS-CoV-2 infection (n = 690) and 480 coronary artery lesions were evaluated in patients without SARS-CoV-2 infection (n = 113). Compared with lesions in patients without SARS-CoV-2 infection, lesions in patients with SARS-CoV-2 infection demonstrated more rapid progression of overall PAV (0.90% per year ± 0.91 vs 0.62% per year ± 0.68, respectively; P < .001) and noncalcified PAV (0.78% per year ± 0.79 vs 0.42% per year ± 0.45, respectively; P < .001). The incidence of becoming high-risk plaque (21.0% [442 of 2108] vs 15.8% [76 of 480]; P = .03) and PCAT attenuation of −70.1 HU or higher (27.1% [571 of 2108] vs 19.8% [95 of 480]; P < .001) at follow-up was also greater in lesions in patients with SARS-CoV-2 infection (P < .001), despite similar prevalence at baseline. Lesions in patients with COVID-19 had a higher risk of target lesion failure (10.4% vs 3.1%, respectively; adjusted hazard ratio, 2.90; 95% CI: 1.68, 5.02; P < .001). Conclusion SARS-CoV-2 infection was associated with a more rapid progression of lesion-based plaque volume and an increase in incidence of becoming high-risk plaque. Coronary plaques among patients who experienced COVID-19 were more prone to having an elevated risk of target lesion failure. Published in Radiology (Feb.4, 2025): https://doi.org/10.1148/radiol.240876

|
Scooped by
Juan Lama
February 3, 10:59 AM
|
Scientists were slow to recognize that Covid spreads through the air. Some are now trying to get ahead of the bird flu. In early February 2020, China locked down more than 50 million people, hoping to hinder the spread of a new coronavirus. No one knew at the time exactly how it was spreading, but Lidia Morawska, an expert on air quality at Queensland University of Technology in Australia, did not like the clues she managed to find. It looked to her as if the coronavirus was spreading through the air, ferried by wafting droplets exhaled by the infected. If that were true, then standard measures such as disinfecting surfaces and staying a few feet away from people with symptoms would not be enough to avoid infection. Dr. Morawska and her colleague, Junji Cao at the Chinese Academy of Sciences in Beijing, drafted a dire warning. Ignoring the airborne spread of the virus, they wrote, would lead to many more infections. But when the scientists sent their commentary to medical journals, they were rejected over and over again. “No one would listen,” Dr. Morawska said. It took more than two years for the World Health Organization to officially acknowledge that Covid spread through the air. Now, five years after Dr. Morawska started sounding the alarm, scientists are paying more attention to how other diseases may also spread through the air. At the top of their list is the bird flu. Last year, the Centers for Disease Control recorded 66 people in the United States who were infected by a strain of avian influenza called H5N1. Some of them most likely got sick by handling virus-laden birds. In March, the Department of Agriculture discovered cows that were also infected with H5N1, and that the animals could pass the virus to people — possibly through droplets splashed from milking machinery. If the bird flu gains the ability to spread from person to person, it could produce the next pandemic. So some flu experts are anxiously tracking changes that could make the virus airborne, drifting in tiny droplets through hospitals, restaurants and other shared spaces, where its next victims could inhale it....

|
Scooped by
Juan Lama
February 1, 1:27 PM
|
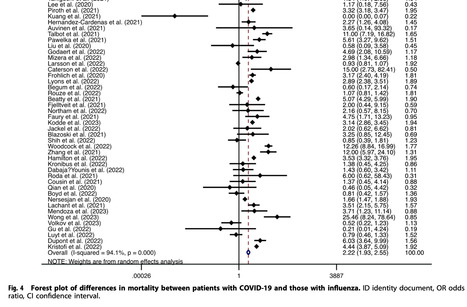
The coronavirus disease 2019 (COVID-19) epidemic has brought major challenges to the global health system, and influenza is also a problem that cannot be ignored. We aimed to explore and compare the clinical characteristics of COVID-19 and influenza to deepen the understanding of these two diseases and provide some guidance for clinicians to make differential diagnoses. We searched PubMed, Embase and Web of Science for articles and performed a meta-analysis using Stata 14.0 with a random-effects model. This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. One hundred articles involving 226,913 COVID-19 patients and 201,617 influenza patients were included, and all the articles included patients with these two diseases as experimental and control groups. Compared to influenza, COVID-19 was more common among men (OR = 1.46, 95% CI: 1.23–1.74) and people with a higher body mass index (MD = 1.43, 95% CI: 1.09–1.77). The proportion of current smokers among COVID-19 patients was lower than that among influenza patients (OR = 0.25, 95% CI: 0.18–0.33). Patients with COVID-19 had longer stays in the hospital (MD = 3.20, 95% CI: 2.58–3.82) and ICU (MD = 3.10, 95% CI: 1.44–4.76), required mechanical ventilation more frequently (OR = 2.30, 95% CI: 1.77–3.00), and had higher mortality (OR = 2.22, 95% CI: 1.93–2.55). We also found significant differences in some blood parameters between the two groups of patients. Upper respiratory symptoms were more obvious in influenza patients, and the proportion of comorbidities was higher than that among COVID-19 patients. There are some differences in the major characteristics, symptoms, laboratory findings and comorbidities between COVID-19 patients and influenza patients. COVID-19 patients often require more medical resources and have worse clinical outcomes. Published in Prim. Care Respir. Med. (Jan. 28, 2025): https://doi.org/10.1038/s41533-025-00414-0
|

|
Scooped by
Juan Lama
February 24, 1:41 PM
|
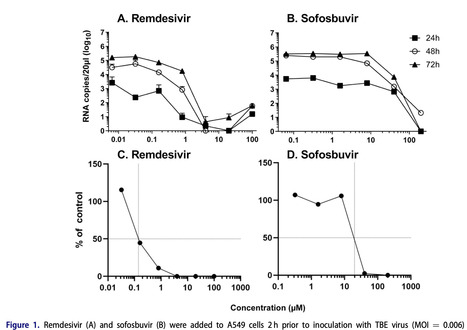
Background Tick-borne encephalitis (TBE) is a neurological disease caused by the tick-borne encephalitis virus (TBEV). Despite available vaccines, breakthrough infections occur, some fatal. Objectives As no antiviral therapy for TBE is currently approved, this study evaluated the in vitro activity of already licenced remdesivir (RDV) and sofosbuvir (SOF) for possible drug repurposing against TBEV. Methods TBEV was cultured in A549 cells, and the inhibitory effects of RDV (GS-5734), its parent nucleotide GS-441524, and SOF (GS-7977) were assessed. Results After 78 h, RDV demonstrated significantly lower EC50 values than SOF (0.14 vs. 11 µM) based on TBEV RNA levels measured by RT-qPCR. RDV also had a lower mean EC50 (0.55 µM) compared to GS-441524 and SOF (>8.9 and 13.1 µM, respectively) using crystal violet staining after 5 days. After 11 passages of TBEV in the presence of RDV, emergence of virus with a higher EC50 (1.32 vs. 0.55 µM) was detected with two mutations (L3122F and Y3278F) in NS5, the viral RNA-dependent RNA polymerase (RdRp), and one substitution in envelope (E) protein (E402G). Similarly, SOF resistance appeared after 20 passages, increasing EC50 values (35.5 vs. 10 µM). Conclusion RDV exhibits potent in vitro antiviral activity against TBEV via specific targeting of the viral RdRp as confirmed by the emergence of resistance-associated double NS5 substitutions in vitro in the presence of RDV. While the potential in vivo implications of the observed RDV resistance remain to be determined, these in vitro data support further assessment of RDV for the treatment of TBEV infection. Published (Feb.20, 2025) in Infectious Diseases: https://doi.org/10.1080/23744235.2025.2468510

|
Scooped by
Juan Lama
February 22, 10:21 AM
|
New research finds that Paxlovid, a COVID-19 antiviral, had minimal benefit in vaccinated older adults. Most of us are pretty adept by now at managing COVID-19, with an armor of past infections, vaccinations, self-tests, and antiviral medications like Paxlovid. In the latest study, however, researchers report that taking Paxlovid may not provide as much benefit as doctors originally thought—particularly for older people who are vaccinated. In a research letter published in JAMA on Feb. 20, Dr. John Mafi, associate professor of medicine at the David Geffen School of Medicine at UCLA, and his colleagues used Canadian data to explore what happened when people took Paxlovid. A Canadian health policy in 2022 allowed prescriptions for Paxlovid only for symptomatic people around age 70 in order to reserve the medication for those who needed it most. Older people are at higher risk of developing complications from COVID-19. The policy allowed the scientists to compare people in this age group who took Paxlovid to those who didn’t. Among the nearly 1.5 million people they studied, those who received prescriptions for the drug did not have significantly different rates of being hospitalized or dying from COVID-19 than those who didn’t get the drug. Most of the people studied were vaccinated. “Our main finding was that among vaccinated older adults, Paxlovid showed no statistically significant reduction in COVID-19 hospitalizations or on mortality,” says Mafi, the study’s lead author. That’s very different from the results that Paxlovid’s maker, Pfizer, first reported in 2022. In that study, Pfizer found that the drug reduced hospitalizations and deaths from COVID-19 by 89% compared to people receiving placebo. But the group they studied was mostly middle-aged and unvaccinated, which is a much different population than exists today. “Yet that 2022 Pfizer study was and continues to be used to support the assumption that the benefits of Paxlovid in unvaccinated adults also apply to vaccinated adults,” says Mafi. “That’s what is being used to justify its perceived effectiveness—and its list price at $1,650 per treatment course.” In a statement, Pfizer said it could not comment on a study in which it did not participate, but that the company "remain[s] confident in Paxlovid's clinical effectiveness at preventing severe outcomes, including hospitalization and death, from COVID-19 in patients at high risk of severe illness." Paxlovid is meant to help those at high risk of developing complications from COVID-19, including the elderly, people with compromised immune systems, and those with multiple underlying health conditions. That remains a primary criterion for prescribing the medication, which is now available for anyone age 12 or older and who is at high risk of severe disease. Still, Mafi says there aren't strong data on how Paxlovid affects the disease course in people who are vaccinated. His findings suggest that the benefits are about four times smaller than those reported by Pfizer. “We are not saying that Paxlovid is useless,” says Mafi. “What this research is saying is that its effectiveness in older groups who are most vulnerable to COVID-19, but who are vaccinated, is far lower than what the earlier evidence from unvaccinated groups showed.” More research is needed, but doctors can consider this new information when deciding whether to recommend a patient take Paxlovid. Other important factors include a person's medical history, the medication's risk of relatively mild side effects, and Paxlovid rebound, in which people taking Paxlovid may test positive again after testing negative. Dr. Katherine Kahn, distinguished professor of medicine at UCLA and the study’s senior author, says that she will discuss the latest results with her patients, and “for generally health people, I’m not encouraging or discouraging [Paxlovid] if they meet the criteria for taking it,” she says. “But for people with higher risk of morbidity or mortality, we’re more likely to say we might consider [Paxlovid] at this time, even though we don’t know 100% if you will benefit.” The new study raises questions for future research. It doesn’t take into account, for instance, how past infections might cause the body to respond to Paxlovid. Mafi and Kahn say that they were also not able to delve more deeply into participants’ vaccination history—how many and which doses they received—or confirm whether they took Paxlovid within five days of their first symptoms, when the drug is most effective. But they are planning to access the individual-level data and do a more in-depth analysis of other factors that may impact how effective the drug is at reducing hospitalizations and deaths. “One of the conclusions of this study is the recommendation for more studies, of both older individuals and those who are vaccinated, of the effectiveness of Paxlovid,” says Kahn. Research Cited Published in JAMA (Feb. 20, 2025): https://doi.org/10.1001/jama.2024.28099

|
Scooped by
Juan Lama
February 19, 11:25 AM
|
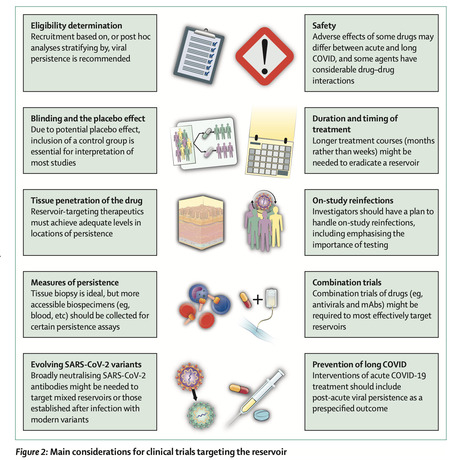
There are no approved treatments for post-COVID-19 condition (also known as long COVID), a debilitating disease state following SARS-CoV-2 infection that is estimated to affect tens of millions of people. A growing body of evidence shows that SARS-CoV-2 can persist for months or years following COVID-19 in a subset of individuals, with this reservoir potentially driving long-COVID symptoms or sequelae. There is, therefore, an urgent need for clinical trials targeting persistent SARS-CoV-2, and several trials of antivirals or monoclonal antibodies for long COVID are underway. However, because mechanisms of SARS-CoV-2 persistence are not yet fully understood, such studies require important considerations related to the mechanism of action of candidate therapeutics, participant selection, duration of treatment, standardisation of reservoir-associated biomarkers and measurables, optimal outcome assessments, and potential combination approaches. In addition, patient subgroups might respond to some interventions or combinations of interventions, making post-hoc analyses crucial. Here, we outline these and other key considerations, with the goal of informing the design, implementation, and interpretation of trials in this rapidly growing field. Our recommendations are informed by knowledge gained from trials targeting the HIV reservoir, hepatitis C, and other RNA viruses, as well as precision oncology, which share many of the same hurdles facing long-COVID trials. Published in The Lancet Infectious Diseases (Feb. 10, 2025): https://doi.org/10.1016/S1473-3099(24)00769-2

|
Scooped by
Juan Lama
February 17, 10:16 AM
|
Laboratories in a national network of 58 facilities responding to the spread of bird flu were notified Friday that 25 percent of the staff in a central program office coordinating their work were fired in the Trump administration’s mass layoffs of federal employees. USDA’s National Animal Health Laboratory Network program office has a staff of only 14 people, but it plays a major role in responding to animal disease outbreaks. It’s responsible for data management, ensuring that labs across the country are conducting the same tests and following similar protocols to accurately and effectively track animal diseases. The labs that make up the American Association of Veterinary Laboratory Diagnosticians were informed that testing and other responses to the H5N1 outbreak would be slower after the layoff, said Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory. “They’re the front line of surveillance for the entire outbreak,” Poulsen said. “They’re already underwater and they are constantly short-staffed, so if you take all the probationary staff out, you’ll take out the capacity to do the work.” USDA did not immediately respond to a request for comment. The department’s work responding to diseases like African swine fever and foot and mouth disease could also be affected. Avian influenza has killed more than 100 million birds since the start of the current outbreak in 2022, including 22 million in the last 30 days, according to USDA’s latest data. The virus has spread in the past year to dairy cattle, infecting the majority of California’s herds and setting off outbreaks in more than a dozen states. USDA’s Animal and Plant Health Inspection Service announced a third spillover event — the term for when a new strain of the virus infects another species — in dairy cattle in Arizona, another indicator that the nation has not yet contained the H5N1 virus. The outbreak has sent the price of eggs skyrocketing to a record high of $4.95 per dozen and led to shortages in some grocery stores. Brooke Rollins, who was confirmed and sworn in as secretary of Agriculture this week, said that she convened a meeting about bird flu on her first day on the job. It’s unclear whether the layoffs were discussed. Thousands of USDA employees across multiple agencies, most of whom are new hires, have been notified they would lose their jobs as the Trump administration moves to aggressively shrink the federal government.

|
Scooped by
Juan Lama
February 15, 1:16 PM
|
It appears that there may have been another spillover of H5N1 bird flu virus from wild birds into dairy cattle. The Arizona Department of Agriculture announced Friday that it had found the virus in milk from a herd of cows in Maricopa County, which contains the state capital, Phoenix. This is the first detection of H5N1 in dairy cows in Arizona, making it the 17th state in which affected cows have been found. Nearly 970 herds have tested positive since the outbreak was first identified in late March 2024. The Arizona detection occurred as part of the U.S. Department of Agriculture’s National Milk Testing Strategy, which samples bulk milk looking for presence of H5N1 viruses. Last week, USDA and Nevada’s Department of Agriculture announced a detection there of H5N1 in dairy herds. Since it was first discovered that bird flu viruses were infecting cows and spreading among herds, it was thought that all of the detections were connected — that there had been a single jump of the H5N1 virus into cows, in either late 2023 or early 2024, likely in Texas. That assessment was based on ongoing analysis of the genetic sequences of the viruses, which belong to a family of H5N1 known as clade 2.3.4.4b, genotype B3.13... APHIS Press Release (Feb. 13, 2025): https://www.aphis.usda.gov/news/program-update/aphis-identifies-third-hpai-spillover-dairy-cattle

|
Scooped by
Juan Lama
February 13, 1:44 PM
|
RFK Jr. was confirmed Thursday as HHS secretary, but it remains to be seen how he will turn his MAHA vision into specific policies to improve America's health. Robert F. Kennedy Jr., the activist-turned-politician with a long history of embracing anti-scientific views, will become the next secretary of the Department of Health and Human Services. Senators voted 52-48 on Thursday to confirm Kennedy to the role. Republican Sen. Mitch McConnell (R-Ky.) voted against RFK Jr., as did all Democrats. “Mr. Kennedy is committed to reorienting our approach to health care and restoring faith in our institutions,” Mike Crapo (R-Idaho), the chair of the Senate Finance Committee, said ahead of the vote. “His passion for addressing America’s chronic disease epidemic will save lives, reduce costs, and establish a foundation for a healthier, stronger country.” RFK Jr. will now be tasked with overseeing the department’s 13 agencies and tens of thousands of federal employees, and safeguarding the nation’s health. Kennedy brings to the job his slogan, “Make America Healthy Again,” which rallied support from unconventional figures, including President Trump. RFK Jr. steps into the role as one of the most visible and scrutinized health secretaries in recent memory. His confirmation process included tense questioning from both sides of the aisle, spanning his views on everything from abortion to Wi-Fi and, of course, vaccines. With the Senate’s assent, Kennedy becomes the first health secretary to take the role after having made a name for himself by encouraging anti-vaccine sentiment and promoting numerous other dubious, pseudoscientific ideas. Many senators remain concerned by RFK Jr.’s views on vaccines (he notably declined to say that vaccines don’t cause autism during his confirmation hearings), though that wasn’t enough to halt his confirmation. Plenty more in the medical and scientific establishment have expressed similar panic over the idea that Kennedy will have control over the nation’s foremost research and public health bodies. “He demonstrated a shocking lack of knowledge about the federal health programs he’ll be charged with running, and a willful desire to mislead senators about his views on science matters like vaccine safety,” Sen. Ron Wyden (D-Ore.) said on Wednesday. Kennedy enters the role in the midst of massive upheaval. In the first month of Trump’s presidency, American health and science institutions have endured communications freezes, threats of funding cuts and mass layoffs, pressure to dismantle diversity programs, and more. Federal health websites have been deleted or scrubbed of key information, including public health data. Foreign health aid has been imperiled, as Trump and ally Elon Musk targeted the U.S. Agency for International Development. Kennedy transformed from an environmental advocate to a vaccine-challenging nonprofit leader before making this pivot into Trump’s orbit in the latter half of 2024, as the presidential race was coming to a close. As an independent candidate, Kennedy didn’t make it very far. However, by the strength of his wide-ranging MAHA movement, and with a Trump endorsement, RFK Jr. got pulled into the Trump campaign as a surrogate. He gave the president a populist health care message in an election where many voters listed it among their top concerns. Trump, in turn, introduced his giant base to MAHA. It remains to be seen just how RFK Jr. will turn his broad vision into specific policies. He has offered few details so far, beyond calling the status quo unacceptable and saying Trump enlisted him to end the chronic disease epidemic. Kennedy has also vowed — against his own record — to support vaccines and not interfere with their availability, and to keep his personal views out of the work of independent federal scientists. Kennedy is a leader in the anti-vaccine movement, and has for years spread the unfounded idea that vaccines are not as safe as the government says they are. Even in his confirmation hearings, RFK Jr. refused to walk back his claims that vaccines cause autism, and declined to accept scientific evidence to the contrary. He has in the past expressed a desire to reform national vaccine safety testing and key oversight panels within HHS. His opponents fear that, regardless of the vows Kennedy made to senators in recent weeks, RFK Jr. will work behind the scenes to undermine science and public health. As HHS secretary, RFK Jr. will be able to pursue his interests, shape health agendas, and influence the nation’s health in countless ways. He will also have the benefit of working with agency heads, including nominees Dave Weldon at the Centers for Disease Control and Prevention, and Mehmet Oz at the Centers for Medicare and Medicaid Services.

|
Scooped by
Juan Lama
February 12, 12:35 PM
|
In 2023, an unprecedented outbreak of highly pathogenic avian influenza (HPAI) H5N1 resulted in the death of thousands of pinnipeds along the Argentinean coast, raising concerns about its ecological and epidemiological impact. Here, we present clinical, pathological, and molecular findings associated with HPAI H5N1 infection in pinnipeds from Chubut, Argentina. Necropsies were conducted on three South American Sea Lions (SASLs) (Otaria flavescens) and one Southern Elephant Seal (SES) (Mirounga leonina), followed by histopathological, immunohistochemical and RT-sqPCR analyses. Neurological clinical signs were observed in two SASLs, with one also exhibiting respiratory distress. Neuropathological findings included lymphoneutrophilic meningoencephalomyelitis and choroiditis, neuronal necrosis, gliosis, hemorrhages, and perivascular cuffing. Viral antigen was localized in neurons, glial cells, choroid plexus epithelial cells, ependymal cells, and the neuropil. Systemic manifestations included HPAI-related necrotizing myocarditis in the elephant seal and placental necrosis in a sea lion, with fetal tissues testing positive for HPAIV. Pulmonary lesions were minimal, limited to bronchial glands in one individual. RT-sqPCR confirmed HPAI H5 in all tested animals. Our findings highlight the neurotropism of HPAI H5N1 in pinnipeds, and expand the known systemic effects of the virus, revealing new tissue tropism and vertical transmission. Preprint in bioRxiv (Feb. 8, 2025): https://doi.org/10.1101/2025.02.07.636856

|
Scooped by
Juan Lama
February 11, 12:02 PM
|
A dairy worker in Nevada may have tested positive for a strain of H5N1 bird flu known to have killed one person and severely sickened another. CNN reported Saturday night that a worker tested positive for the D1.1 version of the H5N1 bird flu virus. Confirmation testing by the Centers for Disease Control and Prevention is underway. The report has not been confirmed by the CDC or Nevada’s Department of Health and Human Services. According to CNN, the person’s symptoms include conjunctivitis, or pink eye — a common symptom that has been seen in people who have been exposed to the virus in North America since March 2024, when the virus was first reported in Texas dairy herds. Since that time, 67 people have been infected with H5N1 bird flu. In 63 of those cases, workers picked up the virus while working with infected animals; 40 got it working with dairy cattle, 23 with infected poultry. In three cases, the source of exposure was not determined. And in one case, a person got it from handling sick and or dead birds in a backyard flock. That person died. Last week, federal health officials announced that at least four dairy herds in Nevada had been infected by a strain of the H5N1 bird flu that is circulating in wild birds and that led to the death of one person in Louisiana and several sickened a teenager in Canada. That strain is called D1.1, and it is slightly different than the one that had been circulating widely in the nation’s dairy herds, which is called B3.13. The news comes on the heels of a U.S. Department of Agriculture report that examined the D1.1 strain found in the Nevada dairy cows and found changes in the genetic code thought to help the virus copy itself more easily in mammals, including humans. Researchers have not been able to determine how the wild bird version of the virus spilled into Nevada herds, although there were reports of massive bird die-offs in the area during that period. Jennifer Nuzzo, director of the Pandemic Center at the Brown University School of Public Health, said if confirmed, it’s a relief this latest dairy worker is reported to have only shown mild symptoms, but she underscored how little we actually know about who gets sick and why when it comes to H5N1 bird flu. She said there are several hypotheses floating around about why most dairy workers have, thus far, only shown mild symptoms after infection when compared to the severe cases reported in two people who had been exposed to D1.1. (Several poultry workers in Washington were also exposed to D1.1 while depopulating an infected poultry operation. While many had respiratory symptoms, they were considered mild cases by public health officials.) One of those theories is that the H5N1 B3.13 version is less dangerous than D1.1, she said. “I’ve not been convinced of that,” she said. Now seeing someone having milder infection with D 1.1, “I think, just raises more questions about why some people have severe illness and why some people don’t,” she said. “I would argue that at this point, we have no idea ... and we shouldn’t assume that just because someone was exposed to one variant or another means they’re going to have mild or severe illness. ... We shouldn’t assume that H5N1 is in any way destined to be a mild virus. And for that reason, we need to treat each infection with caution and work to prevent future infections.” Asked if she was surprised that roughly one year into the outbreak of H5N1 bird flu in dairy cattle people are still getting sick and infected, she said “no.” Little has been done to increase the protection of dairy workers against this virus, she said, and health officials have not “done much to try to stay ahead of how this virus is transmitting and where.” John Korslund, a former USDA scientist, agreed, and said in an email that his biggest concern about the news of a worker possibly being infected “is that the story had to be leaked - i.e. reporting to CNN was unauthorized. Why??” He said recent comments from the Nevada State Agriculture Commissioner about “workers” with conjunctivitis suggested multiple cases, but there was no information about how many workers have been tested, he said. Nor have there been any official reports about clinical illness in the infected dairy herds, he said — although media reports have described the symptoms as respiratory. The USDA highlighted in its report the National Milk Testing Strategy — a new program operating in 40 states, including Nevada, that requires testing of all raw milk destined for pasteurization — as a major contributor to the virus’s discovery in Nevada dairy herds. According to the agency’s report on the herds in Nevada, samples collected on Jan. 6 and Jan. 7 tested positive, triggering an investigation by Nevada state officials to trace the source. On Jan. 17, regulatory officials collected samples from suspected dairies and submitted them to the Washington Animal Disease Diagnostic Laboratory, a USDA-approved lab. On Jan. 31, whole genome sequencing of the virus from affected farms indicated the strain was D1.1. “Clinical signs were not observed in the cattle prior to the detection, but have been reported since,” wrote agency officials in the report. “This virus is getting a shot at infecting a lot more people with much improved genomic adaptations! Risks have grown greatly,” said Korslund in an email. “Our best options are to isolate, sequence, and analyze as rapidly as possible as we develop a new ‘Warp Speed’ human and animal vaccination and therapeutics effort. OMB [the U.S. Office of Management and Budget] needs to take its foot off the throats of our saviors.”

|
Scooped by
Juan Lama
February 8, 10:37 AM
|
In a Friday night move that quickly drew howls of protest from the U.S. biomedical research community, President Donald Trump’s administration today announced it is immediately reducing by at least half the so-called indirect cost payments that the National Institutes of Health (NIH) makes to universities, hospitals, and research institutes to help cover facilities and administrative costs. A 15% indirect cost rate will now apply to all new and existing grants, NIH said in a memo from its Director’s office. Typically, about 30% of an average NIH grant to an institution is earmarked for indirect costs, according to NIH, but some universities get much higher rates. In 2023, NIH, the world’s largest funder of biomedical research, spent nearly $9 billion on indirect costs; the change would likely leave research institutions needing to find billions of dollars from other sources to support laboratories, students, and staff. “It is… vital to ensure that as many funds as possible go towards direct scientific research costs rather than administrative overhead,” NIH wrote in the memo. The new rate brings NIH into line with the maximum indirect costs rates allowed by private foundations, NIH stated, and is higher than the minimum 10% indirect cost payment NIH says it is required to provide. “This rate will allow grant recipients a reasonable and realistic recovery of indirect costs,” the memo stated. The reaction from university groups and researchers has been swift and overwhelmingly negative, and some are already arguing the NIH action is illegal. “This is a surefire way to cripple lifesaving research and innovation,” said a statement from the Council on Governmental Relations (COGR), which tracks federal policy for major universities and medical research centers. “America’s competitors will relish this self-inflicted wound. We urge NIH to rescind this dangerous policy before its harms are felt by Americans.”
Alondra Nelson of the Institute for Advanced Study, former head of the White House Office of Science and Technology Policy, lamented on BlueSky what she said would amount to a "generational restructuring of the US research and development ecosystem." She added that "This funding shift will not only reduce US research leadership, it will put working people out of work and reduce healthcare access." “This would have the most dramatic alteration on research in the United States that one has seen in decades,” says virologist Larry Corey of the Hutchinson Cancer Center, a former leader of the institution who has managed its $2 billion budget. “No one's saying that that research costs are perfect,” he adds, but indirect costs are critical to paying for research infrastructure. Private foundations that pay lower indirect costs can do so only because universities are making up for any shortfall, says Corey. The abrupt change represents “a nuclear bomb on university budgets,” says Morgan Polikoff, an education researcher at the University of Southern California. “I mean, listen, it doesn't take a rocket scientist to figure this out. They're just trying to hurt universities.” This is not the first time Trump has taken aim at reducing indirect costs, which the federal government has been adding to research grants since 1947. In 2017, his first administration proposed reducing NIH’s indirect cost rate to 10% in a budget request to Congress, but lawmakers blocked the change. Slashing NIH’s indirect costs rate was also proposed in Project 2025, a blueprint for an incoming Republican administration that Trump once disavowed but has since embraced. Traditionally, each university negotiated its own overhead rate—including one rate for facilities and one for administration—with the government every few years. Rates vary widely because of geography—costs are higher in urban areas—and because research expenses differ. Biomedical science, for example, often requires animal facilities, ethics review boards, and pricey equipment that aren't needed for social science. But universities have long complained that even the negotiated rates don't cover true research costs. Both Republican and Democratic policymakers, in contrast, have tried to rein in overhead payments. Most notably, in 1994 the U.S. government capped the administration rate for universities at 26% after several instances in which universities were found to have applied the money for purposes outside the scope of the grant. President Barack Obama's administration also floated setting an unspecified flat rate, which economists said would increase efficiency and reduce paperwork. Many who advocate for cutting NIH’s indirect cost rate have long argued that universities are willing to accept lower rates from philanthropic foundations. Today’s NIH notice, for example, notes the Gates Foundation limits indirect costs to 10%, while the Packard Foundation sets the ceiling at 15%. But such reasoning is based on “perverse logic,” Corey says, because foundations use their funds to increase the productivity of research infrastructure already paid for by the federal government. And universities say they are often willing to accept foundation grants that carry low overhead rates because those grants amount to a relatively small fraction of their funding. Some aspects of the new policy aren’t clear. One question, Polikoff says, is whether researchers who can no longer claim certain costs as indirect could roll them into the direct costs of their research. The NIH memo notes that, in 2023, it spent roughly $26 billion on direct research costs, in addition to the $9 billion in indirect costs. It is not clear whether institutions could persuade a court to block the new rate. The NIH memo cites federal rules, adopted nearly a decade ago, that appear to empower the agency to impose a new rate. But COGR says the move “contradicts current law and policy.” It also remains to be seen whether the research community could persuade Congress, currently controlled by Republicans, to block NIH’s change. This is a developing story.
With reporting by Jon Cohen, Jessica Slater, Meredith Wadman, and Jeff Mervis

|
Scooped by
Juan Lama
February 6, 11:10 AM
|
The USDA said four Nevada dairy herds were infected with an H5N1 bird flu strain that has circulated in wild birds, making prospects for containment in cows appear dim. The version in the Nevada herds is one that has been circulating in wild birds. It is also the version behind the severe infection of a teenager in British Columbia, Canada, last year, and a fatal infection in Louisiana last month. To date none of the human infections involving the version of the virus responsible for the main outbreak in cows have resulted in serious illness. Scott Hensley, a professor of microbiology at the University of Pennsylvania’s Perelman School of Medicine, called the finding “a huge development.” For starters, he said, there is reason to think the wild-bird version of the virus might have an easier time acquiring the mutations needed to adapt to spread in people than the version that has been spreading in cows. Research done by scientists in Canada and at the Centers for Disease Control and Prevention has shown that in the two known severe human cases, the viruses were starting to acquire changes during the infections that would have allowed them to more easily infect human respiratory tract cells. And the fact that H5N1, which before last year was not known to infect cows, has spilled over into them at least twice suggests the risk of future spillovers may be higher than previously believed — which would substantially complicate the effort to get the virus out of cows, Hensley said. “It is much easier to control the spread of virus between 1,500 pound cows rather than from birds with wings that are flying around!” he wrote in an email. “And we haven’t been great at controlling the virus spreading between cows.” Both the cow version of the virus and the one circulating in wild birds belong to a large family — a clade, in flu parlance — known as 2.3.4.4b. The subset of viruses responsible for the outbreak in dairy cows is genotype B3.13. The version of the virus found in the Nevada cows was genotype D1.1. Early in the cow outbreak, which was first confirmed in late March, scientists from outside the USDA analyzed the genetic sequences of the viruses available up to that point and determined that the infected herds were all part of a single outbreak, which was moving from herd to herd. That group has been monitoring the sequence data from the outbreak posted by USDA to see if that remained the case, Michael Worobey, an evolutionary biologist at the University of Arizona who convened that group of outside experts, told STAT. The new Nevada herds are the first confirmed new spillover of virus into cows. Because testing has not been rigorous in many states — many farmers have refused to let their animals be tested — it is not possible to rule out the possibility that there have been other such events that went undetected. But the fact that two different versions of the virus could make the leap suggests more such events could happen, Worobey said. “It was an open question whether the first jump had exactly the right pre-adaptations in birds that made it the rare one that could successfully establish itself in cattle,” he said. “If you’re seeing successful jumps from fairly distant branches on the evolutionary tree, there may be lots and lots of viruses out there that, given the chance to interact with cattle, might also become established." That raises concerns about how effective vaccines produced to protect cows might be, Worobey said. Antibodies generated by a vaccine targeting one version of the virus — or indeed by infection — “might not protect, or protect as well,” he warned. There are currently no licensed H5N1 vaccines for cows, but some are in development. Since Worobey and his colleagues reported that the early herd infections were linked, the USDA has maintained that all the infections — in over 950 herds in 16 states to date — trace back to a single introduction of the virus into cows in late 2023 or early 2024, possibly in Texas. The agency suggested control measures like the requirement that cows moving interstate must be tested before transport would lead to a situation where the virus would run out of new animals to infect. This new finding, which was made as a result of a national milk testing strategy the USDA instituted in late 2024, makes prospects for containment appear dim, said Michael Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy. “I’m not surprised that we’re seeing additional introductions, particularly given the very widespread nature right now of H5N1 in migratory waterfowl throughout North America,” Osterholm told STAT. “From a containment standpoint, it just points out that this is not going to burn itself out.” Virologist Angela Rasmussen agreed. “I think it pretty much shows that that idea was completely wrong,” said Rasmussen, who studies emerging infectious diseases at the University of Saskatchewan’s Vaccine and Infectious Disease Organization in Saskatoon, Canada. The fact that the new infections were detected through milk testing shows that relying on finding where the virus is spreading in cows by having farmers report symptomatic animals did not work, she said. “They need to do more testing.” The USDA said in a statement posted to its website that the finding has not made the department rethink its approach. “The detection does not change USDA’s [H5N1] eradication strategy and is a testament to the strength of our National Milk Testing Strategy,” it said.

|
Scooped by
Juan Lama
February 4, 11:31 AM
|
The country desperately needs a White House that will marshal resources toward solving the bird flu problem that's been killing off egg-laying hens by the millions. The price of eggs has reached — if not surpassed — $8 a dozen, depending on where one shops. That’s enough to adversely affect a host of industries, including poultry farming, restaurants, bakeries — not to mention everyday folks who are trying to keep food on their tables. In the wake of all this, the country desperately needs what it hasn’t had since Jan. 20: a fully-functioning White House that can marshal the government’s resources toward solving the bird flu crisis that’s been killing off the nation’s egg-laying poultry stock by the millions. That includes the 3,000 hens who died last month in an outbreak on a family-run farm in Matteson in the south suburbs. The latest evidence that the spread of avian flu is getting worse: Several hundred ducks found dead, most likely from the bird flu, in the past few days along the shores of Lake Michigan in Chicago and the northern suburbs, as the Sun-Times’ Kade Heather reported. But instead of putting more focus on this issue, President Donald Trump and his administration waste time focused on a potentially ruinous tariff war and allow billionaire Elon Musk and the young, highly inexperienced employees at the legally questionable Department of Government Efficiency (created by executive order, not Congress, which has the authority to create federal departments) to run roughshod over federal government agencies and gather sensitive information. Admittedly, skyrocketing egg prices are a global problem driven by the outbreak of bird flu. The European Commission, which is the executive branch of the European Union, reports egg prices have risen 22% in EU countries since 2024. Here in the U.S., average prices rose 50% in the past year. Since the disease is highly contagious and has no cure, a farmer’s only solution when the flu is found is to destroy the stock. The U.S. has lost 25 million laying hens since the outbreak began — about 8% of the nation’s stock. Matteson’s Kakadoodle Farm, which had produced 2,000 eggs a week, was placed under a 150-day quarantine after last month’s outbreak, while the remaining birds are culled. It’s imperative that the government take action, particularly since scientists are reporting the disease can also affect cows — and in rare cases, humans. According to Nature magazine, at least 68 people in North America have become sickened by the virus. And one person has died from it. Now’s the time for the Trump administration, and responsible members in Congress, to give the U.S. Department of Agriculture whatever it needs to solve this problem — and work with the governments of other nations toward a solution.

|
Scooped by
Juan Lama
February 2, 12:49 PM
|
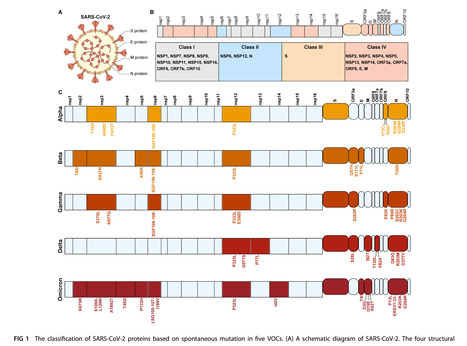
The evolution of SARS-CoV-2 pathogenicity has been a major focus of attention. However, the determinants of pathogenicity are still unclear. Various hypotheses have attempted to elucidate the mechanisms underlying the evolution of viral pathogenicity, but a definitive conclusion has yet to be reached. Here, we review the potential impact of all proteins in SARS-CoV-2 on the viral pathogenic process and analyze the effects of their mutations on pathogenicity evolution. We aim to summarize which virus-encoded proteins are crucial in influencing viral pathogenicity, defined as disease severity following infection. Mutations in these key proteins, which are the virulence factors in SARS-CoV-2, may be the driving forces behind the evolution of viral pathogenicity. Mutations in the S protein can impact viral entry and fusogenicity. Mutations in proteins such as NSP2, NSP5, NSP14, and ORF7a can alter the virus’s ability to suppress host protein synthesis and innate immunity. Mutations in NSP3, NSP4, NSP6, N protein, NSP5, and NSP12 may alter viral replication efficiency. The combined effects of mutations in the S protein and NSP6 can significantly reduce viral replication. In addition, various viral proteins, including ORF3a, ORF8, NSP4, Spike protein, N protein, and E protein, directly participate in the inflammatory process. Mutations in these proteins can modulate the levels of inflammation following infection. Collectively, these viral protein mutations can influence SARS-CoV-2 pathogenicity by impacting viral immune evasion, replication capacity, and the level of inflammation mediated by infection. In conclusion, the evolution of SARS-CoV-2 pathogenicity is likely determined by multiple virulence factors. Published in J. Virology (Jan. 29, 2025): https://doi.org/10.1128/jvi.02049-24
|



 Your new post is loading...
Your new post is loading...