 Your new post is loading...
 Your new post is loading...
Yips are involuntary wrist muscle spasms that affect athletes. They are often associated with golf, baseball, and sports that involve swinging and throwing motions, such as bowling, darts, cricket, and others. Can understanding the information and causes help diagnose and find the right therapy or training? Yips Yips are involuntary wrist spasms that athletes experience. The term is also used to refer to performance anxiety without physical spasms. Researchers believe they are caused by muscle overuse that leads to dystonia (a condition that causes muscles to contract involuntarily), and combined with psychological factors like performance anxiety and overthinking, can make them worse. (Beacon Health Systems, 2024) Types Researchers have identified three types of yips that affect athletes (Clarke P. Sheffield D. and Akehurst S., 2020) Type I - Muscle spasms
- Freezing up/choking
Type II - Performance anxiety
- Psychological symptoms
Type III - Muscle spasms
- Performance anxiety
A study of over a hundred experienced athletes found that nearly 68% of archers and 40% of golfers experienced yips. (Clarke P., Sheffield D. and Akehurst S. 2020) Symptoms The most common symptom is muscle spasms, often in the hands and wrists. That’s why it is the most common among athletes who play sports that require precision hand and wrist movements. Yips affect fine motor skills. (Aoyama, T. et al., 2021) In addition to muscle spasms, symptoms can also include: (Beacon Health Systems, 2024) - Twitching
- Tremors
- Freezing up
- Psychological distress
Causes Healthcare providers, trainers, coaches, and researchers know that psychological and physical factors cause yips. Underlying physical causes include overusing wrist muscles, which leads to dystonia or involuntary muscle movements. Also known as task-specific dystonia, it can also affect individuals who engage in repetitive muscle movements, like factory and assembly line workers, store check-out clerks, musicians, etc. (Clarke P., Sheffield D., and Akehurst S. 2020). Performance anxiety and psychological stress can worsen dystonia. (Aoyama, T. et al., 2021) Athletes can become so focused on their movements that they overthink their actions and perform worse. Individuals who have anxiety, self-consciousness, or stress about a game or performance often find that their involuntary wrist spasms are worse. (Clarke P., Sheffield D. and Akehurst S. 2020) Increased Risk Yips are most common in athletes who use their hands and wrists for their sport and are likely to impact more experienced, competing, and older athletes. (Beacon Health Systems, 2024) They are more common in athletes focused on smaller movements or shorter distances. For example, golfers commonly experience involuntary wrist spasms when putting, and baseball players are likelier to experience them when throwing less than 20 meters. (Clarke P., Sheffield D. and Akehurst S. 2020) Diagnosis There is no official diagnosis for yips. However, a coach, athletic trainer, sports doctors, and others can observe the pattern of symptoms and behavior and provide an informed diagnosis. Treatment Identifying triggers is important as yips can be triggered by: (Aoyama, T. et al., 2021) - Psychological distress - anxiety and/or fear
- Abnormal sensations
- Symptoms of discomfort and pain
- Mechanical movement/motion adjustments or changes
Once trigger/s are identified, they can be addressed. Treatments that can help include: (Beacon Health Systems, 2024) Alternate Hand Positions - This can provide relief from dystonia and overthinking.
Using Different Equipment or Stabilizers - This allows the immobilization of certain muscles and the activation of different muscles.
Mindfulness - Reducing anxiety and distress can help relax the body.
- Practicing mindfulness before games or tournaments can help reduce psychological triggers.
Botox Injections - Botox injections can treat certain types of dystonia.
Sports Psychology - A sports psychologist is a healthcare provider who studies individual athletes' sports performance and how it affects their minds and skills.
- A sports psychologist can help individuals create a program that reduces stress or anxiety around games and performance.
Injury Medical Chiropractic and Functional Medicine Clinic Yips are common among athletes. It is important to address the physical and psychological components to treat the condition. Talking with a coach or a sports psychologist, other athletes, and supporting staff like trainers can help you find a solution. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Beacon Health Systems. (2024). Yips. https://www.beaconhealthsystem.org/library/diseases-and-conditions/yips/ Clarke, P., Sheffield, D., & Akehurst, S. (2020). Personality Predictors of Yips and Choking Susceptibility. Frontiers in psychology, 10, 2784. https://doi.org/10.3389/fpsyg.2019.02784 Aoyama, T., Ae, K., Souma, H., Miyata, K., Kajita, K., Kawamura, T., & Iwai, K. (2021). Difference in Personality Traits and Symptom Intensity According to the Trigger-Based Classification of Throwing Yips in Baseball Players. Frontiers in sports and active living, 3, 652792. https://doi.org/10.3389/fspor.2021.652792
The iliopsoas muscle is a primary hip flexor that assists in the femur's external rotation and maintains the hip joint's strength and integrity. It also helps to stabilize the lumbar spine and pelvis. Athletes often overuse these muscles with all the sprinting, jumping, kicking, and changing directions when running, causing strains and/or tears. Repetitive hip flexion can result in chronic degenerative tendon changes. Chiropractic care and physical therapy can assist in the early phases of healing, safely transitioning to rehabilitation, and returning to physical activities. Iliopsoas Muscle The hip flexors are the group of muscles, including the iliacus and psoas major muscles/iliopsoas and the rectus femoris/quadriceps. One of the largest and thickest muscles in the body, the psoas, extends from the lumbar vertebrae, crosses in front of each hip, and attaches to the inside top of the thigh bone. The muscle works by flexing the hip joint and lifting the upper leg towards the body. These fibers can tear if tension is more than the muscle can bear. An iliopsoas strain occurs when one or more of these hip flexor muscles become overly stretched or begin to tear. Injury The injury can occur from sports or everyday physical activities. This leads to inflammation, pain, and scar tissue formation. An iliopsoas injury is commonly caused by sudden movements, including sprinting, kicking, and changing direction fast while running. Individuals participating in any sports, especially cycling, running, dance, tennis, martial arts, and soccer, are more likely to experience this injury. Other contributing factors include: - Muscle tightness
- Joint stiffness
- Muscle weakness
- Inadequate core stability
- Not warming up correctly
- Improper biomechanics
- Decreased fitness and conditioning
Individuals will feel a sudden stinging pain or pulling sensation, usually on the front of the hip, groin, or abdominal area. Other symptoms include: - Stiffness after resting.
- Swelling
- Tenderness
- Bruising around the area.
- Anterior hip pain and/or burning sensation.
- Groin discomfort sensations.
- Hip snapping or a catching sensation.
- Discomfort when flexing the leg.
- Walking problems and discomfort.
- Lower stomach and/or back symptoms.
Healing and recovery depend on the severity of the injury. A minor iliopsoas muscle injury can take around three weeks to recover fully. More serious strains and tears take six to eight weeks before returning to activity, as the tissue needs time to repair before starting rehabilitation. Chiropractic Rehabilitation and Recovery The first steps when dealing with this injury should be P.R.I.C.E. protection, rest, ice, compression, and elevation. It is important to rest and seek treatment immediately; if left untreated, the condition could worsen, lead to a chronic condition, and require surgery. A chiropractic treatment and rehabilitation plan will consist of the following: - Soft tissue massage
- Joint mobilization
- A chiropractor may recommend crutches to keep the weight off the hip.
- A brace can help compress and stabilize the hip flexor to expedite healing.
- A flexibility and strengthening program will be implemented to target the muscles around the hip.
- Core strengthening exercises will improve the stability of the pelvis area to prevent any further overuse problems.
- Wearing compression clothing could also be recommended, as the clothing helps maintain muscle temperature.
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Dydyk AM, Sapra A. Psoas Syndrome. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (F.L.): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551701/ Lifshitz, Liran BPt, MSc, PT; Bar Sela, Shlomo BPt MPE; Gal, Noga BPt, MSc; Martin, RobRoy PhD, PT; Fleitman Klar, Michal BPt. Iliopsoas the Hidden Muscle: Anatomy, Diagnosis, and Treatment. Current Sports Medicine Reports 19(6):p 235-243, June 2020. | DOI: 10.1249/JSR.0000000000000723 Rauseo, Carla. "THE REHABILITATION OF A RUNNER WITH ILIOPSOAS TENDINOPATHY USING AN ECCENTRIC-BIASED EXERCISE-A CASE REPORT." International journal of sports physical therapy vol. 12,7 (2017): 1150-1162. doi:10.26603/ijspt20171150 Rubio, Manolo, et al. "Spontaneous Iliopsoas Tendon Tear: A Rare Cause of Hip Pain in the Elderly." Geriatric orthopedic surgery & rehabilitation vol. 7,1 (2016): 30-2. doi:10.1177/2151458515627309
Athletes train and practice constantly to prepare their mind and bodies for the big games, matches, etc. When the game is on, it is normal/natural to feel anxious and nervous, especially at the beginning, but then the athlete settles in and relaxes, letting their training take over. However, for some athletes, the anxiousness and nervousness doesn't go away but intensifies, the heart starts racing, and the individual can't stop thinking about choking, failing, and losing. This is known as sports performance anxiety, or competitive anxiety, and is common. Competitive Anxiety Research shows that 30 to 60 percent of athletes experience the disorder. Doctors divide the signs and symptoms into mental and physical categories. Physical Symptoms Rapid Heartbeat - The stress can cause overproduction of adrenaline and cortisol, making the heart beat rapidly.
Muscle Tension - The muscles can tighten up, become painful, and cause tension and pain in the head.
Trembling - The hands could shake while holding the ball, bat, racket, or foot twitching could present.
Hyperventilation - Individuals report a sensation of choking or being unable to catch their breath.
Digestion Issues - The stress can cause foods to be quickly digested, causing cramping and/or the sudden urge to use the bathroom.
Mental Symptoms Fear of Failing - The athlete imagines themselves losing all the time.
- Worrying about letting the coach and team down or the audience or other athletes criticizing and laughing at your performance.
Unable to Focus - The athlete may have concentration issues and become absorbed in how others react to their performance.
Overthinking - The athlete can temporarily forget how to perform specific actions that are typically automatic.
Self-confidence issues - The athlete can start doubting their abilities.
Stress and Anxiety The Yerkes-Dodson law explains how stress, anxiety, and arousal levels affect performance and how stress levels must be maintained within a range to perform well. Low Arousal - It could be the athlete is not as into the sport as when they began, so they do not put forth the total effort.
High Arousal - This means the sport could be causing so much stress that the athlete panics or freezes up.
- Competitive anxiety sets in.
Optimal Arousal - This means the athlete is fully engaged in pushing themselves to the fullest.
- This can be applied to any performing task like play rehearsals to a tennis match.
- Individuals have different optimal levels of stress.
Recommended Steps Some recommended steps can be taken to handle and prevent sports competitive anxiety when trying to overcome those overwhelming feelings of nervousness and tension. Positive self-talk - Self-talk is having a positive conversation with yourself.
Athletes who practiced positive self-talk reported: - Improved self-confidence
- Reduced physical anxiety symptoms
- Improved sports performance
Listen to Music - When anxious before a meet, game, match, etc., consider listening to some favorite or relaxing music.
Meditation - Meditation has been found to reduce all types of anxiety, including sports.
Chiropractic Chiropractic treatment specializes in the musculoskeletal system and can realign the body and release any muscle tension and restriction through hands-on manipulation techniques and mechanical decompression. Treatment involves manipulating the muscles, ligaments, tendons, fascia, and soft tissues to relieve pain through therapeutic muscle therapies that include: - Massage
- Myofascial release
- Trigger point therapy
- Chiropractic adjustments
- Spinal decompression
One or a combination of therapies can alleviate symptoms related to muscle spasms, delayed onset muscle soreness, fascia restrictions, soft tissue injuries, and pain and dysfunction throughout the body, restoring function, movement, and strength. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, or licensed physician, and is not medical advice. We encourage you to make your own healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Elliott, Dave, et al. "The effects of relaxing music for anxiety control on competitive sport anxiety." European journal of sports science vol. 14 Suppl 1 (2014): S296-301. doi:10.1080/17461391.2012.693952 Ford, Jessica L et al. "Sport-related anxiety: current insights." Open access journal of sports medicine vol. 8 205-212. 27 Oct. 2017, doi:10.2147/OAJSM.S125845 Rice, Simon M et al. "Determinants of anxiety in elite athletes: a systematic review and meta-analysis." British journal of sports medicine vol. 53,11 (2019): 722-730. doi:10.1136/bjsports-2019-100620 Rowland, David L, and Jacques J D M van Lankveld. "Anxiety and Performance in Sex, Sport, and Stage: Identifying Common Ground." Frontiers in psychology vol. 10 1615. 16 Jul. 2019, doi:10.3389/fpsyg.2019.01615 Walter N, et al. (2019). Effects of self-talk training on competitive anxiety, self-efficacy, volitional skills, and performance: An intervention study with junior sub-elite athletes. mdpi.com/2075-4663/7/6/148
When stress is placed on the shins with physical activity from walking, running, or exercise, the connective tissues attaching the leg muscles to the tibia can become inflamed, causing medial tibial stress syndrome, more commonly known as shin splints. This inflammation is caused by tiny tears in the muscles and tendons of the shin. Chronic shin pain could be related to foot arch problems, underlying issues with the muscles, or shoes that don't support the feet properly. Although it usually goes away within a few days, it's important to monitor to ensure that it does not progress into a stress fracture. A chiropractor can offer treatments to relieve the pain and help prevent shin splints from recurring. Medial Tibial Stress Syndrome Medial tibial stress syndrome can impact anyone. It can come from walking far distances or in awkward positions like going downstairs with small steps, jumping rope, and playing with the kids on the playground can all cause burning, tightness, and pain in the shins. Shin splints affect individuals differently. For some, the pain recedes when the triggering activity is stopped. For others, the pain can become a chronic condition that results in continuous pain, even when at rest. The Shin - The shin is a part of the tibia bone in the lower leg.
- This bone absorbs the shocks when moving through daily activities.
- The muscles that run along the shin support the foot's arch and raise the toes during movement.
- Medial tibial stress syndrome is caused by excessive force on the shinbone and the tissue around it, which causes the muscles to swell and increases pressure around the bone.
- If left untreated, small tears in the muscle and the bone can form, leading to chronic pain and stress fractures.
Medial tibial stress syndrome is more likely to happen from: - Not stretching before physical activity or exercise.
- Constantly walking or running on hard surfaces.
- Wearing the wrong shoes that don't provide enough cushioning or arch support.
- Over-exertion on the body with activity and movement.
- The body is not given the proper amount of time to recover.
- Athletes often experience shin splints when they've intensified their training routine or changed it up.
Symptoms - Pain during exercise or activity.
- Pain in the front of the lower leg.
- Soreness in the lower leg.
- Swelling in the lower leg.
- Shin is hot to the touch.
Treatment Whenever pain is being experienced, some muscles will either get tight or weak in response. By identifying the weak and/or tight muscles, a chiropractor can prescribe stretches and exercises that will help alleviate the pain and prevent it. One of the main principles of chiropractic is to treat the body as an interconnected system. A chiropractor may work on an unrelated part of the body to treat the symptomatic area. For example, they may work to align the spine and pelvis to lessen the impact on the lower legs. Part of a treatment plan may include: Soft Tissue Mobilization - A handheld instrument loosens tight tissues during soft tissue mobilization therapy and breaks scar tissue around the tibia.
- Massaging tight muscles in the leg keeps them loose and alleviates the pain.
- Percussion massage can be added to reduce muscle knots, improve blood flow, and loosen up scar tissue.
- The treatment relieves pain and can help avoid shin splints when returning to normal activities.
Ultrasound and Low Laser Therapy - Ultrasound and low laser therapy use heat to warm the deep tissues in the lower leg gently.
- The treatment eases pain, reduces inflammation, swelling, and increases blood flow.
Kinesio Taping - Applying flexible Kinesio tape to the foot and lower leg can reduce stress on the shins.
- The chiropractor or physical therapist will show how to apply the tape correctly.
Foot Orthotics - Individuals may be more likely to develop shin splints if they have high or low arches or their feet tend to roll inward or outward when walking.
- Prescription foot orthotics can be made to keep the feet properly balanced and supported.
Stretching Exercises - Shin splints could be related to tight muscles in the back of the calf and weak muscles in the front of the lower leg.
- A chiropractor or physical therapist will show stretching and strengthening exercises to maintain muscle balance.
Retaining Water Due To Salt Intake Salt/sodium is everywhere and hard to avoid. It might not be a surprise that a single patty cheeseburger contains over 500 mg of sodium - almost a quarter of the daily recommended level, but it is a surprise to know that the ranch dressing on a salad contains as much as 270 mg or a tablespoon of soy sauce on a healthy, vegetable-only stir-fry has 879 mg of sodium. The Mayo Clinic estimates that the average individual consumes about 3,400 mg of sodium a day: close to double what is recommended. Sodium is linked with water retention, and it is the kidneys' job to expel unneeded sodium out of the body. Until the kidneys activate, an individual will temporarily be retaining extra water. If daily water and sodium intake habits change daily, this can contribute to water retention, causing fluctuations in daily weight. So, if an individual was on a diet but flooded the body with more salt than usual, expect to see a temporary increase in weight. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Bates, P. "Shin splints--a literature review." British journal of sports medicine vol. 19,3 (1985): 132-7. doi:10.1136/bjsm.19.3.132 Chiropractic Economics: The Science Behind Percussion Massage. Gross, ML et al. "Effectiveness of orthotic shoe inserts in the long-distance runner." The American journal of sports medicine vol. 19,4 (1991): 409-12. doi:10.1177/036354659101900416 Heer, Martina et al. "Increasing sodium intake from a previous low or high intake affects water, electrolyte and acid-base balance differently." The British journal of nutrition vol. 101,9 (2009): 1286-94. doi:10.1017/S0007114508088041 McClure, Charles J. and Robert Oh. "Medial Tibial Stress Syndrome." StatPearls, StatPearls Publishing, 11 August 2021.
When dealing with any kind of pain, many types of remedies can help alleviate the source of the pain. Whether muscle pain or cardiac tissue pain, the effects can be long-term if not appropriately treated. Doctors have discovered that low laser therapy can help repair injured muscles that patients have experienced. With low laser therapy, the beneficial effects can help repair injuries that the bodies’ skeletal and cardiac muscles have endured. When the body gets injured, many people endure the pain later or during the accident. Sometimes the pain is short-termed or long-termed, depending on how severe the injury is. Short-term pain or “acute” pain can be simple, like a sprained joint; however, long-term pain or “chronic” pain, it’s more severe to the body and can have lasting effects. Chronic pain can hinder a person’s body from doing the most straightforward task. When people deal with chronic pain, it can drastically affect the body’s musculoskeletal system and even their cardiovascular system. When the body’s musculoskeletal system is damaged, many complications can start affecting the joints in many different parts of the body. Chronic pain can cause inflammation throughout the body, causing a person not to have the energy to do any task they planned for the day. Sometimes the pain can be excruciating where the body just completely shuts down. When doctors see their patients, they ask them, “Where does it hurt?” meaning where the pain feels more excruciating on the person’s body. The patient will always tell their physicians that the pain is on their joints or back. So doctors would recommend low laser therapy. Low Laser Therapy With low laser therapy or phototherapy, the effects from the treatment can alleviate the pain from the body. Studies show that the application of low laser therapy in injured muscles can significantly enhance muscle regeneration in multiple and frequent applications. Low laser therapy does target the injured muscles because it uses irradiation, which targets the affected muscle while increasing the body’s natural antioxidants and cytoprotective heat shock proteins (HSP-70i). Phototherapy can even help reduce muscle fatigue in athletes when they are in a post-exercise routine. Studies have found that physical therapists use phototherapy as another form of recovery treatment for athletes. What the laser does is that when it is placed on the affected muscle and joint pain, the infrared wavelength penetrates the skin and starts to affect the targeted area. The infrared wavelengths cause therapeutic effects by decreasing oxidative stress accumulated by the body while also reactivating oxygen species production, improving the body’s mitochondrial function, etc. Another study also shows that phototherapy can also repair cardiac tissue. The study shows that when doctors use phototherapy, it directly affects the intracellular mechanisms in the heart while also activating heat-independent tissues without causing tissue damage to the heart. The study also shows that phototherapy can be effective in various complications, such as lymphoedema and muscular trauma. Conclusion All in all, low laser therapy has beneficial properties in preventing muscle and cardiac muscle tissue damage. Its infrared radiation can help patients go about their day without the pain and suffering that their body endures. By reducing ventricular dilatation and preserving the body’s mitochondria while elevating the HSP-70i, the body can start on the road to recovery. References: Leal Junior, Ernesto Cesar Pinto, et al. “Effects of Low-Level Laser Therapy (LLLT) in the Development of Exercise-Induced Skeletal Muscle Fatigue and Changes in Biochemical Markers Related to Postexercise Recovery.” Journal of Orthopaedic & Sports Physical Therapy, Aug. 2010, https://www.jospt.org/doi/10.2519/jospt.2010.3294. Kazemi Khoo, Nooshafarin, et al. “Application of Low-Level Laser Therapy Following Coronary Artery Bypass Grafting (CABG) Surgery.” Journal of Lasers in Medical Sciences, Laser Application in Medical Sciences Research Center, 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4291821/. Oron, Uri. “Photoengineering of Tissue Repair in … – Medical Laser.” Photoengineering of Tissue Repair in Skeletal and Cardiac Muscles, 2006, http://medical.summuslaser.com/data/files/91/1585172203_ls8S6pcJwigZfZQ.pdf. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Being physically fit does not mean training for a triathlon. Regular light exercise/activity is all that is needed. Just going for a 30-minute walk around the neighborhood or playing a 20-minute game regularly is highly beneficial to your health. And the more active you are the better for your health. - Skating
- Bicycling
- Jogging
- Swimming
- Walking
- Playing
Regular Activity Whatever the activity, so long as you get at least 20 minutes of exercise a day will go along way in the future. Regular activity/exercise can help prevent diseases and injuries, which include osteoporosis. Nothing crazy, just begin to work some activity little by little into a routine. One way is after some sitting work/schoolwork once the brain has had enough is the perfect time to go outside and move around. Do some chores that require physical movement, like vacuuming, sweeping, hanging laundry, etc and turn it into a workout. A daily routine of light to moderate physical activity strengthens and maintains the body by helping to: - Build healthy bones, muscles, and joints
- Control weight
- Build lean muscle
- Reduce overall body fat
- Prevent the development of high blood pressure hypertension
Here are a few suggestions on how to get 20-30 minutes of daily exercise/activity. - Try an online fitness class.
- Check out your local gym for online to see what classes are available.
- Family time can become a fun activity/exercise time.
- Take a walk with the family, as many are already doing, play basketball, soccer, or other favorite sport together.
- Invite friends to be physically active online, maybe playing a workout video game and workout together.
If regular physical activity is difficult or you have a medical condition, consult your doctor to recommend the appropriate amount of physical activity and exercises that are safe to perform. But if you are a healthy person, but have not exercised for a while then try for 30 minutes of physical activity a day to keep you healthy and strong. Core Exercises That Help With Back Pain Here are some examples of abdominal exercises that can help develop strong abs and help with back pain prevention. These exercises and the number of repetitions are only suggestions. Talk to your doctor before trying these exercises, and remember to listen to your body. If it doesn't feel right, stop right away. Elbow Planks - Lie down on your stomach with your body straight.
- Elbows should be at 90-degrees and close to the body's sides.
- Rest the forearms on the floor and interlace the fingers.
- Gently push your body up using the forearms.
- Don't' let the back fall/drop.
- Stay straight.
- Engage the core muscles during the entire movement.
- Hold this position for 30 seconds, release, and repeat 3 times.
- Do this once a day.
Crunches - Lie on your back with the knees bent and the feet flat on the floor, about hip-distance.
- Interlace the fingers of your hands behind your head with the elbows out wide.
- Inhale and then as you exhale, use the abdominal muscles and not the neck muscles to slowly raise the head, neck, and back off the floor.
- Inhale and slowly lower the upper body back to the floor, and repeat.
- Try for 3 sets of 10 crunches every day.
Push-ups - Lie down on the stomach so your body is straight.
- Place the hands on the floor a little higher/further than the shoulders.
- The hands should be wider than the shoulders.
- Lift your body so that you're balanced on the hands and toes.
- Maintain a straight back, lower your body to the floor, and slowly bend your elbows until at 90 degrees.
- Push back up using arm strength, upper back, and chest muscles, and repeat.
- Try for 3 sets of 10 every day.
- Once the body becomes stronger, you can go for more reps.
Doing these along with other core exercises you will notice your core strength leading to overall and optimal body strength. Other exercise forms that can help develop core strength while keeping the spine safe are yoga and Pilates. A good idea is to work with a physical therapist/chiropractor that can create a specifically targeted exercise plan that involves core strengthening and flexibility exercises to keep the spine healthy and help maintain proper posture.
Recently, there has been an increasing interest in platelet treatment as a remedy for speeding injury recovery. But just how strong is the evidence for the use? Chiropractor, Dr. Alexander Jimenez looks at the latest research... Of All of the injuries suffered by athletes engaging in game, those involving muscle tissue are one of the commonest injuries -- accounting for up to 50% of reported accidents(1,2). Many muscle injuries result from excessive strain on muscle fatigue, during sprinting, jumping or other volatile contractions but they may also be the result of direct blows, or excessive eccentric contraction, even when the muscle develops tension while lengthening. In this kind of injury, the myotendinous junction of the superficial muscles involved is frequently affected --eg the rectus femoris, semitendinosus, and gastrocnemius muscles. Regardless of the high frequency of muscle Injury in athletes, there's still substantial debate among clinicians as to what constitutes the 'best' method of its remedy. Much of course will be dependent on the diagnosis and evaluation of muscle trauma -- normally gained from a thorough clinical assessment. Imagining can provide additional guidance for your physiotherapist, although this often requires a referral between additional cost and time. Despite these caveats above, few Clinicians would argue against the merits of several basic early therapy options to hasten the athlete's return to sport practice. The most commonly used of these include rest, ice, compression and elevation (RICE) with a short period of immobilization through the first post- injury phase. In addition, the short-term utilization of non-steroidal anti-inflammatory (NSAIDs), corticosteroid medications is frequently recommended(3-8). More Than MedicationWhile medications such as NSAIDs and Corticosteroids have their place at the early stages of muscle injury therapy, there has been a growing interest in the use of autologous (cells and cells derived from ego) of biological products as an alternative or additional treatment for muscle injury. One such remedy is the use of blood platelets (blood cells whose purpose, along with the coagulation factors, would be to stop bleeding) as used in platelet therapy. Why platelets? When a muscle is Injured and damaged, it destroys a number of processes as part of the healing/repair process (see figure 1). Through this procedure, there are two Major stages: - The early phase of destruction (inflammatory stage), where affected cells including muscles, blood vessels, connective tissues and intramuscular nerve undergo breakdown and death.
- The repair and remodelling stage, in Which undifferentiated satellite cells (in response to several growth factors) proliferate and differentiate into mature myoblasts in a bid to replace the muscle fibre tissue.
- In the inflammatory phase, the Inflammation happening after muscle trauma usually results in the accumulation of inflammatory cells, neutrophils and macrophages. In addition, blood platelet cells in the neighborhood of the wounded site become triggered. These activated platelets undergo 'degranulation' releasing various substances, including growth factors (see box 1), which are stored at the alpha (α) granules inside platelets(9). The accumulation of platelets in the vicinity of a muscle injury should consequently in theory provide more growth variables for the tissue, thereby aiding the repair and remodeling phase. Moreover, platelets contain other important substances requirement for tissue regeneration and repair, such as glue proteins, clotting factors and their inhibitors, proteases, cytokines and tissue glycoproteins.
Theory & PracticeConsidering the discovery that platelets play a vital role in muscle tissue repair, it was not long before researchers wondered if platelet-rich plasma (PRP) injections into the site of an injured muscle could accelerate healing period and so hasten the return to sport of an injured athlete. These platelet-rich therapies are produced by centrifuging a quantity of their patient's own blood and extracting the energetic, platelet-rich, percent. A 2009 study using an animal model revealed that an autologous PRP injection significantly quickened tibialis anterior muscle recovery (from 21 days to 14 days(12). Indeed, prior to the, Sanchez et al introduced a similar finding at the 2005 World Congress on Regenerative Medicine. They noticed that athletes getting PRP injection under ultrasound guidance gained full recovery within half of the expected period(13). However, in 2010, the International Olympic Committee concluded that 'now there's very limited scientific evidence of clinical efficacy and safety profile of PRP use in athletic injuries'(14). This position was underlined with a systematic review article published the next year, reporting 'there's been no randomized clinical trials of PRP impacts on muscle recovery'(15). Fast forward to 2015 and what does the research about the effectiveness or otherwise of PRP medications? Latest ProofAt the last 2-3 years, a flurry of papers has been released on the use of PRP therapy for muscle trauma. A 2013 study on 30 professional athletes with severe local muscle injury seemed to give positive signs for PRP treatment(16). Prior to the intervention, most of the athletes failed and ultrasound and sonoelastography (a kind of ultrasound imaging that shows mechanical properties of tissue) examination. Patients were then randomly assigned to two groups: - Group A received targeted PRP Injection under ultrasound guidance and also additional conservative therapy
- Group B received conventional Conservative treatment only
Pain was assessed based on visual analogue scale (0 to 10), while muscle function was evaluated based on pain on resisted flexion or intensity, and range of movement. Both groups were evaluated in the days 1, 7, 14, 21, and 28 after commencing treatment. Overall, the degree of pain relief has been greater in group A compared to group B Throughout the intervention. At the end of 28-day observation, 93 percent of pain Regression was announced by patients in Group A vs. 80 % of regression of pain in Group B. Also, at 7 and 14 days, significant Improvements in strength and range of Motion for PRP treatment team were observed. By the end of the study, Subjective global function scores improved Considerably in group A in comparison with Group B -- as evidenced by the typical Return-to-sport occasions -- 10 times in group A And 22 days in group B. A 2014 systematic inspection meanwhile produced less encouraging findings about the value of PRP(17). The authors searched the literature for studies assessing the effects (benefits and harms) of platelet-rich therapies for treating musculoskeletal soft tissue injuries and where the primary results were functional status, pain and negative consequences. The analysis included data from 19 trials totaling 1088 participants who contrasted platelet-rich therapy with placebo, autologous whole blood, dry needling or no platelet-rich therapy. These trials coated eight clinical conditions: Rotator cuff tears (arthroscopic fix) (six trials); shoulder impingement syndrome surgery (one trial); elbow epicondylitis (three trials); anterior cruciate ligament (ACL) reconstruction (four trials), ACL reconstruction (donor graft site application) (2 trials), patellar tendinopathy (1 trial), Achilles tendinopathy (1 trial) and acute Achilles rupture surgical repair (one trial). The outcomes were as follows: - Medium-term function statistics at six months from five trials showed no difference between PRP and management teams;.
- Long-term function data at one year pooled from 10 trials showed no distinction between PRP and the control state;
- Information gleaned from four trials that assessed PRP in 3 clinical conditions revealed a small Decrease in short term pain in favour of PRT but the clinical significance of this outcome was marginal;
- Seven trials reported an absence of adverse events after PRP therapy but four trials reported adverse events;
- Pooled data for long-term purpose from six trials through rotator cuff tear surgery revealed no statistically or clinically significant gap between PRP and management groups;
- The evidence for all primary outcomes was thought as being of very low quality not least because the Ways of preparing platelet-rich plasma varied and lacked standardisation and quantification of this plasma applied to the patient;
Fast forward a year and a 2014 analysis investigated the impact of a single PRP shot in treating grade 2 hamstring muscle injuries(18). Twenty- eight patients diagnosed with an acute hamstring injury were randomly allocated to autologous PRP therapy together with a rehab program or a rehabilitation program just. The primary outcome of this analysis was time to return to play. Moreover, changes in pain severity and pain disturbance scores over time were examined. The results showed that patients at the PRP group attained full recovery significantly earlier than controls. The mean time to return to play was 42.5 times in the control group and 26.7 days in the PRP group. Significantly lower pain severity scores were observed in the PRP group throughout the study. But no significant difference in the pain disturbance score was found between the 2 groups. The authors concluded: 'A single autologous PRP injection combined with a rehabilitation program is more successful in treating hamstring injuries than the usual rehab program alone'. Conflicting EvidenceLater the exact same year however, a strict double-blind, placebo-controlled trial on the efficacy of PRP injections for acute hamstring injury brought very different conclusions(19). The researchers randomly assigned 80 competitive and recreational athletes with acute hamstring muscle injuries (as confirmed on magnetic resonance imaging) for intramuscular injections of PRP or isotonic saline as a placebo. Significantly, the patients, clinicians, and physiotherapists were oblivious of study-group assignments. Each patient received two 3-ml injections by means of a sterile ultrasound-guided procedure; the very first injection was administered within 5 days following the injury and has been followed 5 to 7 days after by the next injection. Patients in both research groups conducted an identical, everyday, progressively phased, criteria-based rehabilitation program, which was based on the best available evidence (detailed in the study). The speed of re-injury within two months following the resumption of sport action was assessed as a secondary outcome measure. The result showed that the median time until the resumption of athletics activity was 42 days in the PRP group and 42 days too in the placebo group (see figure two). The re-injury rate was 16 percent at the PRP group and 14% at the placebo group Although statistical evaluation allowed for a small chance there was a clinically relevant between-group gap, the authors concluded in their analysis at least, intramuscular PRP injections provided no advantage over and over a placebo shot. The rigorous design of this study and the comparatively large number of topics casts some serious doubts on the effectiveness of PRP treatment. As if to underline these misgivings, the researchers completed a 1-year follow-up study on exactly the exact same set of athletes (published just last month) to see if there were any longer-term advantages of PRP treatment that might not have been picked up at the initial study(20).) Specifically, they sought to set the re-injury speeds at one year following PRP, and some other secondary outcomes such as alterations in clinical and MRI parameters, abstract patient satisfaction as well as the magnifying outcome score. Analysis of this data revealed that just as at 2 months, one year after there were no substantial between-group differences in the 1-year re-injury speed, or some other secondary outcome measure. Another very recent research into the effectiveness of PRP treatment was printed just a couple of months ago. Researchers discovered the data from 19 previous randomized controlled trials, which had compared PRP treatment in patients with severe or chronic musculoskeletal soft tissue injuries using placebo, autologous whole blood, dry needling, or no PRP(21). The authors concluded: 'While several in -vitro studies have proven that platelet-derived growth factors can promote the regeneration of bone, cartilage, and joints, there's currently insufficient evidence to support using platelet-rich therapy for treating musculoskeletal soft tissue injuries'. And as in the 2013 study emphasized previously(17), they also pointed out that there's a need for the standardization of PRP preparation procedures. The last decision was that the only circumstance where PRP treatment might provide tangible benefits is when conservative treatment has failed and the next treatment option is an invasive surgical procedure. Conclusions & Practical Advice For The ClinicianWhen a clinician has an athlete in their care, minimizing the healing time in order that return to game can take place whenever possible is an essential aim of any therapy. In concept, PRP therapy should accelerate healing and recovery and really, several earlier studies appeared to suggest that PRP is a worthwhile adjunct alongside conventional treatment. However, larger and more rigorously constructed studies have failed to discover good evidence for the benefits of PRP, either in the short or longer duration. One possible reason for the confusing picture is that the preparation of PRP is far from standardized, meaning that the active elements within an PRP treatment could vary tremendously from study to study. As clinicians, our purpose is to use evidence- based practice and on this basis, we must conclude that (as yet) there is simply inadequate evidence for using PRP treatment in treating sports-related muscle injuries. References
1. Am J Sports Med 2001, 29:300–303
2. Br J Sports Med 2001, 35:435–439
3. Curr Sports Med Rep 2009, 8:308–314
4. Sports Med 2004, 25:588–593
5. Clin J Sport Med 2003, 13:48–52
6. Br J Sports Med 2004, 38:372–380
7. J Bone Joint Surg Am 1983, 65:1345–1347
8. J Am Acad Orthop Surg 1996, 4:287–296
9. Thromb Haemost 2011, 105(Suppl 1):S13–S33
10. Br J Sports Med 2008, 42:314–320
11. J Bone Joint Surg Br 2000, 82-B:131–137
12. Am J Sports Med 2009, 37:1135–1142
13. ‘Application of autologous growth factors on skeletal muscle healing’: Presented at 2nd World Congress on Regenerative Medicine, May 18–20, 2005
14. Br J Sports Med 2010, 44:1072–1081
15. Expert Opin Biol Ther 2011, 11(4):509–518
16. Med Ultrason. 2013 Jun;15(2):101-5
17. Cochrane Database Syst Rev. 2014 Apr 29;4:CD010071
18. Am J Sports Med. 2014 Oct;42(10):2410-8
19. N Engl J Med 2014; 370:2546-2547
20. Br J Sports Med. 2015 May 4. pii: bjsports-2014-094250
21. Clin Podiatr Med Surg. 2015 Jan;32(1):99-10
Chiropractor, Dr. Alexander Jimenez takes a look at the anatomy and biomechanics of the adductor magnus, its role in musculoskeletal syndromes and how clinicians can manage tightness and high tone in this muscle. The adductor magnus (AM) is a posteromedial thigh muscle, with a complex anatomical arrangement. It has a number of primary roles, including functioning as a major hip extensor, hip adductor and pelvic stabiliser. The role AM has in producing movement at the hip and pelvis is often misunderstood and underrated. It plays a fundamental role in producing hip extension force when the hip is already in hip flexion. As a result it is commonly found to be tight and overactive in many athletes potentially leading to a host of musculoskeletal issues. AnatomyThe AM is located on the medial side and posterior side of the thigh. It has been suggested that it should be considered as having three separate anatomical and functional components (figure 1 shows the relative origins of the three heads along with the hamstring muscle group): 1. Pubofemoral portion or ‘adductor minimus’ a. The front or anterior part of the muscle, arising from the ischiopubic ramus (where the ramus of both pubic bone and ischium meet). b. Fibres from the pubic ramus are short and horizontal, and insert along the linea aspera just medial to the gluteus maximus. c. This is the hip flexing and adducting part of the AM. 2. Middle part a. The fibres from the ischial ramus are more vertical and lateral, and these insert via an aponeurosis into the linea aspera, being innervated by the posterior branch of the obturator nerve(1).
b. This is the adducting component of the AM. 3. Ischiocondylar portion or ‘hamstring portion’ a. This is the posterior part of the muscle. b. Due to the common nerve supply (sciatic nerve) between this portion and the hamstrings, it is often grouped together with the hamstrings as a hip extensor (sometimes called the ‘4th hamstring’(1)). c. It arises out of the ischial tuberosity, from a well-defined osseous origin located medial to the semimembranosus and conjoint tendons(2). d. Fibres run vertically downwards as a thick and fleshy mass of coarse bundles, and insert onto the adductor tubercle via a rounded tendon. e. This is the hip extending part of the AM. Due to the complex pelvic attachment of the AM, the variable insertion points along the femur, and the geometrical rotation through the shaft of the femur, the AM has a sweep or curved appearance as it descends down the inner thigh to insert along the linea aspera and finally the adductor tubercle. This structure allows it to act as a major stabiliser of the pelvis as we hip flex in weight bearing – eg squatting down and bending over to pick up something. It could be postulated that due to the fact the ischiocondylar (posterior) part of the AM does not cross the knee joint, it is a muscle that can be used to not only control the hip and pelvis as we flex the hip under load (such as squatting and bending over) but which may also be used to stabilise the hip and pelvis. This is because the bi-articular hamstring muscles are influenced by the concurrent knee flexion that may occur during squatting, and can lose their ‘length tension curve’ to control and maintain hip flexion moments. The AM on the other hand is better suited to doing this (along with the gluteals). Considering the role of the AM in comparison to the other hip extensors such as gluteals and hamstrings therefore, the AM is often underrated in its influence in producing movement, and acting as a hip and pelvic stabiliser. AM PhysiologyThe AM is one of the largest muscles in the body (based purely on weight and volume). It appears to be the second heaviest muscle in the lower limb after the gluteus maximus. Ito et al. (2003) found that the gluteus maximus and AM weighed 573.4g and 452.6g respectively(4). Similarly, by reference to cross-sectional area, it is the second largest muscle after the gluteus maximus; the same researchers found that the gluteus maximus and AM were 48.4cm2 and 26.9cm2 in cross-sectional area, respectively(4). Based on muscle volume, AM is also much larger than the other adductor muscles such as adductor brevis, adductor longus, pectineus and gracilis(5). The AM, adductor longus, adductor brevis, gracilis all have substantial hip-adduction muscle-moment arms. The ischiocondylar AM has a large hip extensor muscle-moment arm, making it an unappreciated hip extensor, while the other adductors are hip flexors. The hip-extension moment arm length of the AM changes with hip angle; it is a more effective hip extensor than either the hamstrings or gluteus maximus when the hip is flexed. This means that exercises that have peak contractions in positions of hip flexion (like full squats) can train the AM very effectively. It has been reported that the AM muscle moment arm length for hip extension was 5.7 – 6.1cm at 90 degrees of hip flexion, compared to 4.0 – 4.8cm for the hamstrings, and 3.1 – 3.3cm for the gluteus maximus(6). This makes the AM the most effective hip extensor in hip flexion, which corresponds to the bottom of the squat movement. In strength and conditioning circles, this deep position is known as ‘getting out of the hole’. The AM produces a large part of the hip extension torque in this deep position. Anecdotally, many deep squatters appreciate this the day after a heavy squat session as the most ‘sore’ muscle the next day due to delayed onset muscle soreness (DOMS) is the AM! In contrast, the AM is only a moderate hip extensor when the hip is already extended. Németh and Ohlsén reported that the AM muscle-moment arm length for hip extension was just 1.5 – 2.4cm in the anatomical position, compared to 6.1 – 6.8cm for the hamstrings, and 7.5 – 8.1cm for the gluteus maximus(6) Meanwhile Dostal et al. reported muscle-moment arm lengths of 3.9cm and 5.8cm for the middle and posterior portions, respectively(7). This makes the hamstrings and gluteus maximus much more effective hip extensors than the AM when the hip is extended, as in the upright position. These above findings have implications for the athlete – and also the therapist managing injuries – related to the balance of the hip extensor muscles. The ischiocondylar AM would be an extremely strong and possibly dominant muscle is the following examples: - Sprint starts out of the blocks. They become less important as the sprinter approaches a vertical position.
- Sprint cyclists who assume a curled position of extreme hip flexion.
- Powerlifters, weightlifters or any strength athlete at the start of a deadlift/ clean and jerk movement, or getting ‘out of the hole’ in squatting.
- Hockey players spend a long time in hip flexion positions.
- American football and rugby players. Drive in contact starting from a position of hip flexion.
- Cross fit athletes who perform many movements from deep hip flexion.
- Uphill running and stepping up.
The muscle moment arms for the AM in adduction exceed those of hip extension, showing that this muscle is still definitively a hip adductor as well as a hip extensor(7). The AM does not display a large muscle-moment arm length in the transverse plane, and therefore does not contribute a lot to hip internal or external rotation(7-10). In terms of muscle fibre characteristics, the AM is composed of mixed type 1 and type 2 muscle fibres. This compares with the other hip extensors such as the hamstrings that have higher numbers of type 2 fibres(11,12). The clinical consequence is that the AM is great at producing slow- strength based movements such as heavy deep squats, whereas in faster hip extension movements such as sprinting, the hamstrings have a favourable fibre type for this type of activity. Therefore to summarise the functional roles of the AM: 1. It is a powerful hip extensor at full hip flexion positions.
2. Its role in hip extension reduces as the hip approaches neutral positions. 3. It is an adductor of the hip.
4. It stabilises the hip and pelvis in hip flexion positions such as squatting down and bending forward. AM In Musculoskeletal DysfunctionCompared to other muscles such as the vastus medialis obliquus (VMO), lower and upper trapezius, gluteus medius and transversus abdominus, the research available on the role the AM plays in musculoskeletal dysfunction is sparse and almost non-existent. This may be due to the fact that is a thick and very deep muscle, has a complex anatomical arrangement, and EMG studies may be difficult due to cross talk from neighbour muscles such as the hamstrings and other adductors. Clinically and anecdotally however, it can be postulated that the AM is muscle that is often over-used and develops myofascial restrictions, trigger points and tightness – especially in athletes. Due to the heavy use of the ischiocondylar part of the AM in producing hip extension force from hip flexion positions, it could be argued that athletes may develop imbalances in these muscle groups due to the over reliance on AM to produce movement. The use of the AM to produce hip extension torque would have a significant effect on the lower limb kinematics during such movements. This can sometimes be seen in heavy lifting movements with powerlifters and weightlifters, where the knees medially deviate on the initial part of the ascent during the deep squat. This is often referred to as a ‘valgus collapse’ of the knees. It is thought that this movement is produced by the adduction component of the AM, and is not balanced by the abducting component of the gluteus maximus during the hip drive/extension phase in deep squatting movements. This can be seen in Figure 3. It must be mentioned here that this appearance of valgus collapse is also caused by other factors such as reduced ankle dorsiflexion and other hip muscle imbalances. However, if the knees appear to be aligned over the third toe during the descent of the squat, and then on the change over from eccentric to concentric muscle action a valgus collapse occurs, it may well be likely that the valgus collapse has been initiated by a hip extension muscle with an additional adduction role – ie the AM. Managing AM TightnessConsidering that the AM is often ‘overactive’ in most athletes, it may be argued that it is a muscle that does not need a lot of direct strengthening. It may be more appropriate to stretch and perform myofascial release techniques to the muscle. Below are two examples of how this can be performed. Minimising AM Involvement In SquattingTo minimise involvement, it may be necessary to integrate more gluteus maximus into the squat movement via the use of bands and straps around the knees when squatting. This is a technique made popular by a wide variety of strength and conditioning coaches around the world such as Louie Simmonds and the Westside Barbell Company in the USA. By using an elastic band or strap around the knees during squatting and asking the lifter to actively push out against the strap would in effect require the hip abducting gluteals to perform this action. This may reduce the tendency for the AM to over dominate during the squat movement and create unwanted hip adduction and valgus knee collapse. This exercise can be done in a periodised training cycle (such as in the early general preparation phases) or it may be done as warm up before performing heavy squat movements. SummaryThe AM is a complex muscle that has wide anatomical attachments onto both the pelvis and femur. It has a major role in producing hip extension force from positions of deep flexion, and also adduction in all hip angle positions. AM is often overactive on athletes and thus is a muscle that needs a lot of direct stretching and myofascial release techniques to avoid possible knee and hip joint issues. References 1. Martini F, Timmons M, Tallitsch R. Human Anatomy. Boston, MA: Pearson Benjamin Cummings; 2012.
2. Skeletal Radiol. [published online November 10, 2015]. doi:10.1007/ s00256-015-2291-5 3. The Orthopaedic Journal of Sports Medicine. 2016. 4(1)
4. Okajimas folia anatomica Japonica. 2003. 80(2-3), 47
5. Journal of Applied Physiology. 2012. 113(10), 1545-1559
6. Journal of Biomechanics. 1985. 18(2), 129-140 7. Physical Therapy. 1986. 66(3), 351-359
8. Medical Engineering & Physics. 1998. 20(1), 50-56
9. Gait & Posture. 2000. 11(3), 181-190
10. Journal of Biomechanics. 2001. 34(4), 437-44
11. The American Journal of Sports Medicine. 1984. 12(2), 98-103
12. Archives of Physical Medicine and Rehabilitation. 2004. 85(4), 593
A sprain is medically defined as a stretch or tear of the ligaments, the strong cords of fibrous tissue which connect two bones together at the joints. Sprains most commonly occur on areas of the body which can be injured during a fall or sudden twisting motion, such as the ankle. According to the U.S. National Library of Medicine, approximately 2 million ankle sprains alone occur each year. An incorrect fall or abrupt twist usually causes a sprain because the unusual movement can force a joint into an abnormal position that may wind up stretching or tearing the ligament. Ankles, wrists, knees, and fingers are all frequently sprained areas of the body. A strain is medically defined as a stretch or tear of the muscle or tendon. A tendon is a fibrous band of tissue that connects the muscles to bones. Strains most commonly occur on the lower back and on the hamstring muscle located on the posterior side of the thigh, most commonly as a result of overexertion, trauma, or repetitive movements. Strains most frequently occur on the back, hamstring, and even the shoulder, because these areas are greatly mobile and highly used during strenuous physical activity, leading to a stretch or tear of a single, or multiple, muscle and tendon due to overuse. Although sprains and strains significantly differ from each other, these do share several similarities, which is the main reason individuals generally confuse the two conditions. Both sprains and strains include symptoms of pain, swelling, and limited mobility around the region of the injury. The symptoms can range from moderate to intense, according to the injury’s level of severity. Individual’s who’ve suffered an injury and are experiencing these symptoms can temporarily relieve their pain and discomfort using ice therapy to reduce the inflammation around the affected area as well as getting plenty of rest and elevation.
|
Individuals who engage in sports and physical activities that involve lunging forward while running or jumping can sustain a plantaris muscle injury. Can understanding the anatomy of the back of the leg and the symptoms help diagnose and treat plantar muscle injuries? Plantaris Muscle The plantaris muscle is a long, narrow muscle in the calf that runs along the back of the leg. It's part of the Triceps Surae, a group of muscles in the calf that, along with the gastrocnemius and soleus muscles, makes up the bulk of the back of the leg. It is located in the superficial posterior compartment of the leg. Strains or tears of the plantaris muscle at the back of the leg can cause pain and swelling, similar to a calf strain or Achilles tendon tear. Individuals may feel immediate pain, cramping, and other symptoms. Anatomy The gastrocnemius and soleus muscles are the major muscles, with the soleus located deeper in the leg. Together, they form the Achilles tendon, which blends into a tendon in the back of the heel and attaches to the heel bone/calcaneus. When the calf muscles contract, they point the foot downward, propelling the body forward when walking, running, and sprinting. The plantaris muscle and tendon sit more or less in the center of the calf, between the two heads of the gastrocnemius. Around 7% to 20% of the population are born without plantaris muscles. There are variations, such as having a double- or triple-headed plantaris muscle. (Olewnik Ł. et al., 2020) However, individuals that do not have the muscle or have a variation have not been shown to affect long-term or short-term mobility. Symptoms Plantaris muscle ruptures are the most common injury and occur often during running or jumping. (Spang C. et al., 2016) Many who sustain this injury are athletes who have to lunge forward. Common symptoms include: - Sudden onset pain behind the calf.
- Swelling of the calf muscle.
- Muscle knots or myofascial trigger points of the calf muscle.
- Swelling and bruising in the back of the calf area.
- Cramping in the calf muscle.
- Spasm sensations of the calf muscle.
- Symptoms of a plantaris muscle strain are less severe, with the common signs being tightness and pain during and after physical activity.
Diagnosis Plantaris muscle tears differ from Achilles tendon tears because the foot can be pointed downward following the rupture, whereas an Achilles tear cannot. Plantaris ruptures can also be confused with a blood clot in the large veins of the calf, called deep vein thrombosis/DVT. (Rohilla S. et al., 2013) Tests like MRI or ultrasound can be performed to confirm or exclude a plantaris rupture. Both can be useful for verifying whether the injury is a strain or tear and identifying other possible causes of calf pain. Treatment Treatment is typically non-surgical. While the injuries can cause pain and disability, the symptoms almost always resolve with conservative treatments and therapies. Rest, ice, compression, and elevation are the first line used and may be all that is needed for a muscle strain. Short-term use of NSAIDs may be recommended for a strain or tear to reduce pain and inflammation. (Morelli K. M. et al., 2018) If the pain is profound or there is a tear, patients may require short-term immobilization or the use of a crutch for the pain to subside. With the assistance of a physical therapist, sports chiropractor, and athletic trainer, gradual increases in mobility and strength can be obtained. Symptoms usually gradually resolve over several weeks. Full recovery may take up to eight weeks, depending on the severity of the injury. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop customized treatment programs through an integrated approach to treating injuries and chronic pain syndromes, improving flexibility, mobility, and agility, relieving pain, and helping individuals return to normal activities. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, don't hesitate to contact Dr. Alex Jimenez or us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Olewnik, Ł., Zielinska, N., Karauda, P., Tubbs, R. S., & Polguj, M. (2020). A three-headed plantaris muscle: evidence that the plantaris is not a vestigial muscle? Surgical and radiologic anatomy: SRA, 42(10), 1189–1193. https://doi.org/10.1007/s00276-020-02478-8 Spang, C., Alfredson, H., Docking, S. I., Masci, L., & Andersson, G. (2016). The plantaris tendon: a narrative review focusing on anatomical features and clinical importance. The bone & joint journal, 98-B(10), 1312–1319. https://doi.org/10.1302/0301-620X.98B10.37939 Rohilla, S., Jain, N., & Yadav, R. (2013). Plantaris rupture: why is it important? BMJ case reports 2013, bcr2012007840. https://doi.org/10.1136/bcr-2012-007840 Morelli, K. M., Brown, L. B., & Warren, G. L. (2018). Effect of NSAIDs on Recovery From Acute Skeletal Muscle Injury: A Systematic Review and Meta-analysis. The American journal of sports medicine, 46(1), 224–233. https://doi.org/10.1177/0363546517697957
Nerves control muscle fibers. Muscle twitching is an involuntary contraction of the muscle fibers. When individuals play sports/work out vigorously or for a long time, they may experience muscle twitching and can often see and/or feel the twitches happening. The most worked-out muscles are likely to twitch, which includes the biceps, thighs, and calves, but twitches can occur in any muscle. Chiropractic care, massage therapy, and functional medicine can help relax the muscles, improve circulation, restore function, and train individuals to prevent future episodes. Muscle Twitching A muscle twitch often occurs after intense physical activity or a hard workout because the muscle or muscles have been overworked, and there is hyper-excitability of the nerve/s that makes the muscle/s continue to contract. - A muscle twitch that can be seen is called fasciculation.
- A muscle twitch that cannot be seen is called fibrillation.
- If there is pain or the twitching is prolonged, it is a muscle spasm.
Causes The most common causes include the following: - Intense exercise and rigorous physical activity build up lactic acid in the muscles.
- Dehydration is a very common factor for shaky muscles.
- Vitamin D and calcium deficiencies could cause muscle spasms in the hand, calves, and eyelids.
- Using caffeinated products to increase physical performance.
- Not enough or a lack of healthy sleep.
- Anxiety or stress.
- Certain medications like estrogen and corticosteroids.
- Nicotine and tobacco use.
Physical Activity/Exercise - Intense exercise and physical activity can cause muscle fatigue.
- Muscle fatigue triggers twitching and cramping in overworked muscle fibers.
- Electrolytes play a role in muscle contraction.
- Electrolyte loss and imbalances within muscle fibers through sweating can lead to twitching.
Dehydration - Muscle mass comprises 75% water.
- Water carries nutrients and minerals to muscles to support function.
- Not being properly hydrated can cause twitching and cramping.
Vitamin D Deficiency - Nerves need vitamin D to relay messages to and from the brain to the body's muscles.
- A vitamin D deficiency can cause muscle weakness and twitching.
Magnesium Deficiency - Magnesium deficiency is known as hypomagnesemia.
- Magnesium plays a role in maintaining nerve and muscle health.
- Magnesium helps transport calcium across cell membranes to support nerve and muscle function.
- A magnesium deficiency can cause twitching anywhere in the body, including the face.
Causes of magnesium deficiency include: - Poor diet
- Diarrhea
- Drinking too much alcohol
- Not addressing magnesium deficiency can increase the risk of cardiovascular disease.
Caffeine - Caffeine is a stimulant.
- Drinking too much coffee, tea, or energy drinks can cause fasciculation.
Not Enough Sleep - Brain chemicals or neurotransmitters transmit information from the brain to the nerves that control muscle contraction.
- Sleep deprivation can affect how neurotransmitter receptors work.
- This means excess neurotransmitters can build up in the brain.
- Lack of sleep can affect neurotransmitter function.
- A common site of fasciculation tiredness occurs in the eyelids.
Anxiety and Stress - Experiencing psychological stress or high anxiety levels can cause excess muscle tension.
- This can lead to muscle twitching.
- Muscle fasciculation caused by stress can occur anywhere in the body.
Certain Medications - Certain medications can lead to involuntary muscle twitching.
- The reaction can be a side effect due to interactions with other medications.
- Individuals should discuss side effects and medication interactions with their doctor when taking a new medication.
Chiropractic Care Chiropractors are experts on the musculoskeletal system and have many techniques to treat muscle fasciculation and spasms. It often depends on the cause/s, and specific treatment varies on a case-by-case basis. Common chiropractic treatments include: - Massage therapy
- Heat and ice therapy
- Manual manipulation
- Joint adjustments
- Ultrasound
- Stretches to keep the muscles flexible
- Exercises to strengthen the muscles
- Nutritional recommendations
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make your own healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Bergeron, Michael F.. Muscle Cramps during Exercise-Is It Fatigue or Electrolyte Deficit?. Current Sports Medicine Reports July 2008 - Volume 7 - Issue 4 - p S50-S55 doi: 10.1249/JSR.0b013e31817f476a Gragossian A, Bashir K, Friede R. Hypomagnesemia. [Updated 2022 May 15]. In: StatPearls [Internet]. Treasure Island (F.L.): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500003/ Küçükali, Cem Ismail, et al. "Peripheral nerve hyperexcitability syndromes." Reviews in the neurosciences vol. 26,2 (2015): 239-51. doi:10.1515/revneuro-2014-0066 Maughan, Ronald J, and Susan M Shirreffs. "Muscle Cramping During Exercise: Causes, Solutions, and Questions Remaining." Sports medicine (Auckland, N.Z.) vol. 49, Suppl 2 (2019): 115-124. doi:10.1007/s40279-019-01162-1 Miller, Kevin C et al. "Exercise-associated muscle cramps: causes, treatment, and prevention." Sports health vol. 2,4 (2010): 279-83. doi:10.1177/1941738109357299 Riebl, Shaun K, and Brenda M Davy. "The Hydration Equation: Update on Water Balance and Cognitive Performance." ACSM's health & fitness journal vol. 17,6 (2013): 21-28. doi:10.1249/FIT.0b013e3182a9570f
Delayed Onset Muscle Soreness - DOMS is when muscle pain or stiffness develops a day or two after playing sports, weight lifting, exercise, or work that involves concentrated physical activity like lifting and carrying objects. DOMS is considered a normal response to extended exertion and is part of the adaptation process that the recovering muscles experience as they undergo hypertrophy or an increase in muscle size. It is common in individuals who have just started exercising, increased the duration or intensity of their workouts, or just beginning a physically demanding job. DOMS When muscle contracts as it lengthens is known as eccentric muscle contractions, which is most associated with DOMS. It is related to increased stress in muscle fibers as they are exerted excessively. This also happens when engaging in movements the muscles are not used to, like a new exercise or helping a friend move heavy boxes, furniture, etc. Examples include: - New exercise or unusual physical task.
- Descending stairs.
- Lifting/Lowering weights or heavy objects.
- Running downhill.
- Deep squats.
Symptoms Individuals will not feel DOMS during the workout or physical activity. Delayed symptoms include: - Swelling in the affected muscles.
- Muscles feel tender to the touch.
- Muscle fatigue.
- Reduced range of motion and movement.
- Pain and stiffness when moving.
- Decreased muscle strength.
Treatment Options Time and waiting for the muscles to repair themselves is the natural healing process, but steps can be taken to ease the soreness, stiffness, and pain. This includes: It is different for everybody; personal experience will determine which works best for the individual. Active Recovery - Active recovery is a technique that uses low-impact aerobic exercise right after a workout to increase blood flow to the muscles.
- The increased blood supply can help relieve the inflammation.
RICE This technique is used for acute injuries but can be applied to delayed onset muscle soreness. It stands for: - Rest
- Ice
- Compression
- Elevation
Chiropractic A chiropractic massage is for healing sore muscles, tendons, ligaments after an intense game, workout, etc. Chiropractic increases the blood and nerve circulation around the muscles delivering added oxygen and nutrients. This type of massage helps loosen the muscles/connecting tissues allowing the body to recover and heal quicker. When Muscles Are Not Rested Not taking time to recover because of overtraining/working can have consequences on the body. Inflammation that is not given the time to heal can lead to: - Injuries.
- Weakened immune system.
- Muscle mass loss.
- Mental health issues.
The body’s immune system cannot function at total capacity during intense physical stress. This causes difficulty when trying to fight off germs and viruses. Studies have found preventing inflammation and injury requires prioritizing rest. Constantly being on the go and under intense physical stress can take a toll not only on the body but the brain as well. This can lead to irritability, frustration, anger, which leads to other health problems generating a vicious cycle. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Cheung, Karoline et al. “Delayed onset muscle soreness: treatment strategies and performance factors.” Sports medicine (Auckland, N.Z.) vol. 33,2 (2003): 145-64. doi:10.2165/00007256-200333020-00005 Guo, Jianmin et al. “Massage Alleviates Delayed Onset Muscle Soreness after Strenuous Exercise: A Systematic Review and Meta-Analysis.” Frontiers in physiology vol. 8 747. 27 Sep. 2017, doi:10.3389/fphys.2017.00747 Reinke, Simon et al. “The influence of recovery and training phases on body composition, peripheral vascular function and immune system of professional soccer players.” PloS one vol. 4,3 (2009): e4910. doi:10.1371/journal.pone.0004910
A sports hernia is a soft tissue injury that happens in and around the groin area. It is a strain or tear of any soft-tissue muscles, tendons, or ligaments in the lower abdomen or groin area. It usually happens during physical sports activities that require fast, quick, sudden changes of direction and/or intense twisting movements. Despite its name, a sports hernia is not a hernia in the classic sense. The condition's proper term is athletic pubalgia. However, a sports hernia can lead to an abdominal hernia. The condition can happen to both men and women. Anatomy The soft tissues most affected by sports hernias are the oblique muscles in the lower abdomen, along with the tendons that attach the oblique muscles to the pubic bone, are the most at risk. In many cases, the tendons that attach the thigh muscles to the pubic bone or adductors are also stretched or torn. Core Muscle Injury A core muscle injury is when the deep layers of the abdominal wall weaken or tear. This can cause nerve irritation and contribute to uncomfortable symptoms of numbness or tingling. The most common causes include: - Planting the feet and turning or twisting with maximum force.
- Constant repetitive hip and pelvic twisting motions.
- Imbalances between the hip and abdominal muscles can also, over time, cause overuse injuries.
- Weakness in the abdominals and improper or no conditioning can also contribute to injuries.
- Aggressive abdominal exercises can cause and/or aggravate a core muscle injury.
Symptoms - Chronic groin pain is the primary symptom of a core muscle injury.
- Sharp groin pain with exertion.
- Basic movements like sitting down or getting out of bed can also present with pain or discomfort.
- Pain on one side of the groin.
- Pain or numbness that radiates into the inner thigh.
- Pain when coughing or sneezing.
- Tenderness or pressure on the lower abdominal area.
- Pain decreases with rest.
Diagnosis A doctor will discuss symptoms and how the injury occurred. They will run a series of strength tests like a sit-up or trunk flex against resistance. If it is a sports hernia, there will be tenderness in the groin or above the pubis, along with discomfort and pain. Further tests will include MRI, ultrasound, or X-rays to rule out hip, low back, or pelvis injuries to confirm a core muscle injury. Non-Surgical Treatment Rest - In the first 7 to 10 days after the injury resting and icing the area is recommended.
- If there is a bulge in the groin, compression or a wrap can help relieve symptoms.
Chiropractic and Physical therapy - Two weeks after the injury, chiropractic adjustments and physical therapy exercises are recommended to improve strength and flexibility in the abdominal and inner thigh muscles.
- For most cases, 4 to 6 weeks of chiropractic and physical therapy will resolve any pain and allow the individual to return to their exercise or sports activity.
Anti-inflammatory Medications - A doctor could recommend non-steroidal anti-inflammatory medications to reduce swelling and pain.
- If the symptoms persist over a prolonged period, a doctor may suggest a cortisone injection.
If the pain comes back when resuming the physical activities, surgery could be needed to repair the torn tissues. Surgical Treatment Repairing the torn tissues can be done with a traditional open procedure that involves one long incision or a minimally invasive endoscopic procedure. In an endoscopy, the surgeon makes smaller incisions and uses a small camera, called an endoscope, to see inside the abdomen. The results of traditional and endoscopic procedures are the same. Most individuals can return to sports and physical activities 6 to 12 weeks after surgery. Muscle Gain Individuals can't lose fat forever. At some point, they need to work on developing muscle or work to preserve the muscle that is already present. This requires a different diet and exercise plan than one designed for fat loss. Instead of getting the body into a catabolic state, the body needs to be in an anabolic state where the body builds tissue instead of breaking it down. To build muscle, the body needs resources meaning proper nutrition and sufficient protein intake to increase muscle mass. Maintaining an energy surplus of around 15% is appropriate for developing musculature, meaning a moderately active individual with a BMR of 1,600 calories would want to their intake to about 2,852 calories a day. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Hoffman, Jay R et al. "Effect of protein intake on strength, body composition and endocrine changes in strength/power athletes." Journal of the International Society of Sports Nutrition vol. 3,2 12-8. 13 Dec. 2006, doi:10.1186/1550-2783-3-2-12 Larson, Christopher M. "Sports hernia/athletic pubalgia: evaluation and management." Sports health vol. 6,2 (2014): 139-44. doi:10.1177/1941738114523557 Poor, Alexander E et al. "Core Muscle Injuries in Athletes." Current sports medicine reports vol. 17,2 (2018): 54-58. doi:10.1249/JSR.0000000000000453 Thorborg, Kristian et al. "Clinical Examination, Diagnostic Imaging, and Testing of Athletes With Groin Pain: An Evidence-Based Approach to Effective Management." The Journal of orthopedic and sports physical therapy vol. 48,4 (2018): 239-249. doi:10.2519/jospt.2018.7850 Tyler, Timothy F et al. "Groin injuries in sports medicine." Sports health vol. 2,3 (2010): 231-6. doi:10.1177/1941738110366820
The body's muscles function to produce force and motion. The trapezius muscle is one of the largest, which makes it highly susceptible to injury/s and spasms. A trapezius muscle spasm is when the muscle starts to contract. This muscle group is based around the neck and shoulders and is used to move the scapula shoulder bone. Causes of Trapezius Muscle Spasms A few causes for this muscle to become inflamed/irritated include: - Poor posture
- Injury
- Stress
- Tension
- Improper lifting
Symptoms The effects feel similar to a pulled shoulder muscle. Common symptoms include: - Upper body stiffness
- Shoulder pain
- Neck pain
- Arm numbness/tingling
- Lack of shoulder flexibility
Spasm and Pinched Nerve Difference A muscle spasm and pinched nerve might seem or feel similar, but they are different. A muscle spasm makes the area tight and can cause muscle twitching. They vary in intensity with some spasms being mild and others excruciating. In some cases, a spasm can cause a nerve to get pinched if the knot contorts tightly around a nerve and if it is big enough. Conversely, a pinched nerve can also cause twitching, but it typically results in severe pain. Pinched nerves can also cause tingling sensations and numbness depending on the severity it could cause muscle spasms. Treating The Spasms There are a few ways to treat this naturally. Heat and Ice Therapy One way to calm a muscle spasm is using heat and ice. The heat will increase nerve and blood circulation keeping the muscles flexible, and the warmth will soothe the injury. This helps prevent the muscles from spazzing and generating pain. Ice therapy also increases blood circulation but the focus is on reducing inflammation. The nerves become slightly frozen which stops the tingling, significantly reducing the pain. If pain presents around the trapezius, immediately put an ice pack on. It should be applied every few hours in 15-minute sessions. Once the pain subsides, heat therapy can be applied. A heating pad placed around the area, a warm/hot bath, or standing in the shower if possible with a massage setting letting the warm/hot water hit the muscle. But it must be consistent, doing it for about 20-minute sessions three times a day. Stretches and Exercises Stretches and exercises can help keep the muscle flexible and prevent any tightening. Upper Trapezius Stretch This stretch will move the upper trapezius area, promoting flexibility and preventing the muscle from becoming stiff. - Sit in a chair with proper posture
- Holding onto the chair with the left hand, wrap the right arm over the top of the head so that the hand touches the left ear.
- Gently pull the head toward the right and hold.
- Slowly move the head back and repeat with the other hand.
Shoulder Shrugs - Moving the shoulders up and down throughout the day stretches the trapezius.
- It releases tension and strengthens the muscle to protect it.
- This exercise should be done every few hours for about a minute or two.
- Also occasionally rolling the shoulders will help stretch the smaller components of the trapezius.
Cobra Pose This yoga pose is for relieving tension. - It can be very helpful for those suffering from severe spasms or from a pinched nerve.
- The first thing is to lie face-down on the floor.
- Keeping the feet straight behind, use the hands to gently push the upper body up so that the spine slightly curves.
- Make sure that the hands are situated in front of the body and firm on the ground.
- Hold for a few seconds and then release.
- Repeat the process three more times.
Therapeutic Massage - The soothing motions from a massage will calm irritated areas and encourage them to heal quicker.
- At first, because of the tenderness around the area, a massage could present with pain.
- The massage therapist needs to press on the area to increase blood circulation so that toxins get flushed out.
- While it might hurt the individual soon notices that the swelling and pain are reducing.
Some massage techniques include: Chiropractor Chiropractors specialize in the musculoskeletal system and understand how the muscles, bones, and joints all work together. For muscle spasms, they investigate the problem and look at other areas of the body that could be contributing to or worsening the condition. For some, muscle spasms could be brought on by a misplaced joint pressing on the area. A chiropractor will palpate the areas to ensure this is not the case. And if there is a problem, they will perform a joint manipulation. This realigns the joint back in place and reduces muscle spasm symptoms. Over time the muscles become healthier because chiropractic releases toxins and improves the range of motion. Anti-Inflammatory Diet Often, muscle spasms are the result of inflammation. When a muscle swells, it can place pressure on surrounding nerves. The more intense the inflammation the more pressure/stress on the nerves. This can make moving and functioning very difficult because of the pain. To naturally reduce inflammation consider an anti-inflammatory diet. This type of diet is filled with antioxidants, vitamins, and minerals that will work to reduce swelling. Although it might not completely repair the muscle injury, it can reduce symptoms and stop oxidative stress. Foods to eat more of are: - Cherries
- Tomatoes
- Almonds
- Blueberries
- Oranges
- Salmon
- Kale
- Turmeric
Dr. Alex Jimenez’s Blog Post Disclaimer The scope of our information is limited to chiropractic, musculoskeletal, physical medicines, wellness, and sensitive health issues and/or functional medicine articles, topics, and discussions. We use functional health & wellness protocols to treat and support care for injuries or disorders of the musculoskeletal system. Our posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate and support directly or indirectly our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. We understand that we cover matters that require an additional explanation as to how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. The provider(s) Licensed in Texas& New Mexico* References Finley JE. Physical Medicine and Rehabilitation for Myofascial Pain. Medscape. https://emedicine.medscape.com/article/313007-overview#showall. Updated May 21, 2017. Accessed July 16, 2018. Rodante JA, Al Hassan QA, Almeer ZS. Myofascial Pain Syndrome: Uncovering the Root Causes. Practical Pain Manag. https://www.practicalpainmanagement.com/pain/myofascial/myofascial-pain-syndrome-uncovering-root-causes. 2012;6. Last updated on October 5, 2012. Accessed July 16, 2018. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.656.582&rep=rep1&type=pdf
Chiropractor, Dr. Alexander Jimenez summarizes the anatomy and biomechanics of pectoralis minor, how tightness can create Injuries to the shoulder, and also powerful stretching and loosening procedures with this muscle... The pectoralis minor (PMi) is a muscle located on the anterior chest wall which directly impacts movement an important consideration for proper movement that was scapulohumeral, of the scapula. It's been suggested that tightness in the PMi can adversely affect scapula function(1-3), especially in limiting upward rotation, external rotation, and cerebral tilting(4), leading to shoulder injuries like impingement syndrome(1,5), and rotator cuff pathologies(6,7), internal impingement(7), glenohumeral instability(8) along with adhesive capsulitis(9). Anatomy & BiomechanicsPMi is a wide triangular shaped muscle that originates from the second to fifth ribs as well as their costal cartilages through aponeurotic slips that are continuous with the facia covering the intercostal muscles(10). Within an old but comprehensive cadaver study, Anson discovered that 42 percent of those slips are connected from the second to the fifth ribs(10). However, this origin may be reduced to 3 or even to 2 ribs between the second to fifth ribs. Overall 91.5 percent of cadavers showed that the PMi arose from all or a few of the ribs between the fifth and the second. Cases where the source extended beyond the land of the next to the fifth ribs composed but 8.5 percent of the total amount. From here the fibers course upwards and laterally and converge to insert onto the anteromedial and superior surface of the coracoid process. The PMi is found deep into the more superficial pectoralis major muscle, whereas the axillary blood vessels and brachial plexus lie posterior to the muscle (see Figure 1). In a further study, it had been discovered that in some cadaver specimens, the PMi limb comes with an ectopic insertion, which is, somewhere away from the corocoid process(11). These ectopic insertions were described as being of three varieties: - Type 1 -- happens when the entire PMi tendon passes through the superior margin of the process to fit on websites like one of the tubercles of the head, the coracoacromial ligament, the tendon, or the labrum.
- Type 2 -- this variant is seen when a few portion of the thoracic has normal insertion into the process and another portion has insertion.
- Type 3 -- happens when the muscle itself (as opposed to this tendon) inserts anomalously without attaching to the coracoid process.
This study indicated that patients with an insertion had considerably thicker fibrotic scar tissue at the rotator interval. These scar changes around the coracoid process including the adrenal period could have a physiological or pathological mechanism which leads to adhesive capsulitis. The overlying tendon working on top of the process could cause structures in the rotator period or friction against the coracoid process during motion. PMi FunctionThe functions of the PMi (see Figure 2) have been to: 1. Protract the scapula (along with the serratus anterior). 2. Downwardly rotate the scapula (along With rhomboids and the levator scapulae). 3. Anterior tilt the scapula (along with rhomboid and levator scapulae). 4. Depress the scapula (along with the Poor trapezius). 5. Rotate the scapula. 6. Help the inspiration muscles during breathing (because of its attachment on the rib cage). Sporting/ training activities that involve these motions in the scapula (racquet sports, swimming, weight lifting etc) can theoretically result in overuse of the muscle, especially in the existence of training errors, poor technique or a rapid increase in training load, frequency and/ or length. Furthermore, the muscle can become constant reaching with one hand or shortened due to postural positions like sitting in a computer. These may all lead to tightness in the muscle, which will prevent complete scapular motion during overhead motions as it may limit upward bending and posterior tilt of the scapula, movements that are necessary for clearance of the acromian procedure away from the humeral head during arm elevation(3). Injuries & Tightness In PMiDue to its attachment on the coracoid Prevent upward rotation, elevation and posterior tilting of the scapula, which is required for shoulder elevation, and a shortening of PMi, process will result in anterior rotation of the scapula. Sahrmann (2002) has clarified a number of clinical syndromes that are associated with a shortening of PMi(15). These include; thoracic outlet syndrome, scapular winging and tilting syndrome, scapular abduction syndrome, scapular depression syndrome and scapular downward rotation syndrome. Bhatia et al (2007) suggested an injury Defined as an insertional tendinopathy of PMi brought on by bench pressing and called that 'Bench Presser's Shoulder'(16). They argue it's a cause of shoulder pain in weightlifters/ sportsmen. PMi Trigger Point ReferralTrigger points in the PMi can create pain in and around the shoulder. The quintessential reference point for whatever myofascial and trigger point related is Simons and Travell (1999)(17). They explain a pain referral pattern of PMi as pain over the anterior deltoid region and spilling over into the subclavicular and pectoral areas. The pain can extend down the medial aspect of the arm, forearm, and into the ulnar supply of the third and their hand, fourth, and fifth digits. Lawson et al (2011) introduced a case study on how PMi trigger points generated pain like angina in a cross country skier(18). Meanwhile, Fitzgerald (2012) presented a situation whereby stiffness in PMi can also be a causative element in thoracic outlet syndrome(19). Thoracic outlet syndrome is the result of compression or irritation as they pass from the cervical spine into the arm, through the axilla. If the PMi muscle is involved, the patient may present with chest discomfort, along with pain and paraesthesia. The symptoms were replicated on both digital pressure within the PMi muscle and muscle on testing for thoracic outlet syndrome. Treatment therefore should focus on the PMi muscle. SummaryThe PMi has been identified as a muscle that is implicated in scapula dysfunction and following shoulder pathologies. Tightness in the muscle can limit full Scapula upward rotation elevation -- movements which are required to Enable clearance of the acromian Process away from the humeral head in elevation rankings. Stretching exercises for the PMI have been provided to Lengthen and decrease tone problematic muscle. References
1. Phys Ther. 2000; 80(3):276-291
2. Sports Medicine and Arthroscopy Review. 2012; 20(1):39
3. J Orthop Sports Phys Ther. 2005; 35(4):227-238
4. Phys Ther. 2009; 89(4):333-341
5. J Orthop Res 2001; 19(6):1192-1198
6. J Shoulder Elbow Surg. 2005;14(1 SupplS):58S-64S
7. J Orthop Sports Phys Ther. 2006; 36(7):485-494
8.Am J Sports Med. 2007; 35(8):1361-1370
9. J Biomech. 2008; 41(2):326-332
10. J.Anat. 1938; 72(4); 629-630
11. Korean J Radiol. 2014;15(6):764-770
12. Int J Sports Physical Ther. 2013; 8(1);25-33
13. BMC Musculoskeletal Disorders 2007; 8:64
14. J Shoulder Elbow Surg. 2006; 15(3):324-330
15. Sahrmann S: Diagnosis and treatment of movement impairment syndromes. London: Mosby; 2002
16. Br J Sports Med. 2007 Aug;41(8):e11
17. Simons DG, Travell JG, Simons LS. Travell & Simons’ myofascial pain and dysfunction. The trigger point manual volume 1. Upper Half of Body. 2nd ed. Baltimore, MD: Williams & Wilkins; 1999
18. J Chiropractic Med 2011; 10, 173–178
19. J Can Chiropr Assoc. 2012 Dec;56(4):311-5
Chiropractor, Dr. Alexander Jimenez examines the relevant anatomy and biomechanics of the tensor fascia latae. He explains, what role it plays in pain and dysfunction, and what can be done in the presence of a tight and overactive TFL muscle. The tensor fascia latae (TFL) is a hip muscle that is well known to rehabilitation therapists and allied health practitioners. It is a muscle that may play a role in pain and dysfunction in the lower limb, pelvis and spine. It is however poorly understood, as the research studies that exist on this muscle are few and far between. Furthermore, much of the research and opinions have simplified the exact anatomy of, not only the TFL, but also its anatomical relationship to the iliotibial band (ITB). TFL is a muscle that has a complex anatomical arrangement with the ITB, and it performs various functional roles – not only in producing hip movement, but also imparting fascial tension through the fascia latae of the thigh and the specialised ITB. Therefore TFL also plays a key role in not only postural support during one legged stance, but also in limiting the tensile stress on the femur caused by the combination of bodyweight, ground reaction force and how these create unique bending forces on the femur. Regional AnatomyDiscussing the anatomy of the TFL cannot be done in isolation without also discussing the anatomy of the iliotibial band/tract (ITB or ITT). Pare et al (1981) have presented arguably the most comprehensive anatomical and electomyographical study (EMG) study on the TFL to date(1). This followed a much earlier study in 1958 when Kaplan presented an exhaustive study on the TFL and iliotibial tract(2). Interestingly, Kaplan extended his study further by comparing the TFL and ITB in humans to other primate and mammals and discovered that human beings are the only mammals to have a defined ITB. Gottschalk et al (1997) also added a substantial amount of knowledge regarding the anatomy and function of both the TFL and ITB(3). In this millennium, Fairclough et al (2006)(4) and Feto et al (2002)(5) have provided even further knowledge of the TFL and its relationship to the ITB via cadaveric and biomechanical modelling studies. TFL & MLLThe general consensus is that the TFL originates on the iliac crest starting at the ASIS (just lateral to the origin of the sartorious), and extends posteriorly along the iliac crest about 2 to 5 cm to incorporate both bony investments into the iliac crest and investments onto the gluteal fascia(1-3). Pare et al (1981) highlights that the muscle actually has two functionally and anatomically distinct heads – the anteromedial (AM) and posterolateral (PM) head(1). These will be discussed in detail later.
The contentious issue however, is where the muscle ultimately inserts. It appears from available research, that the muscle has both a bony insertion onto the femur and a fascial insertion onto the ITB – or more specifically onto the specialised portion of the middle longitudinal layer (MLL) of the fascia lata of the thigh which we know as the ITB (see figure 1).
The ITB, also called the ‘band of Maissiat’, was originally studied in 1843 and was perceived to be a ligament that connected the ilium with the knee and was responsible for maintaining the balance of the body in stance and in motion(5). Later work by Kaplan (1954)(2) showed that human beings are the only mammals to own a distinct facial lateral band down the thigh highlighting further that the ITB may play a role in bipedal stance and balance(2). This view was further supported in biomechanical models suggested by Feto et al (2002)(5).
However, much later cadaveric studies showed that the exact anatomy of the ITB and its relationship to the TFL and gluteals was in fact far more complex. The fascia lata of the thigh has a rather multifaceted array of layers that all interconnect. Of particular importance to the TFL, is the middle longitudinal layer (MLL) of the fascia lata. The MLL is a thick, longitudinal connective tissue, commencing on the iliac crest and extending downwards to have several insertions. A large portion of the MLL blends with the inner transverse layer of the fascia lata to insert directly onto the femur. The MLL also has superficial fibres that extend all the way down to insert about the knee. Anteriorly at the hip, the MLL envelopes the TFL so that this muscle is effectively joined and sandwiched between the superficial and deep MLL. It also has fibres that directly blend with the superficial fibres of the gluteus maximus The MLL therefore is joined in part to the gluteus maximus, and in part to the TFL. To make things even more complex, as well as being enveloped by the MLL, some of the distal fibres of both heads of the TFL then insert into the MLL. The anteromedial fibres of the TFL blend with the MLL and course down the thigh to insert onto the lateral patella retinaculum. Therefore, this may influence somewhat the patella position in relation to the femoral trochlear groove. However, none of these anteromedial fibres cross the knee joint to insert onto Gerdy’s tubercle, therefore they have no effect on motion at the tibia; the primary role appears to be at the hip. Some of the fibres (not all) of the posterolateral TFL, along with those superficial fibres of the gluteus maximus, invest onto the MLL and insert all the way down onto the lateral tubercle of the tibia. They therefore do cross the knee joint and thus may have a role in a stabilising the pelvis and the lower limb. Inner TFLWhat needs to be pointed out about the MLL, is that as it courses down the thigh it blends quite heavily with the inner transverse layer of the fascia lata(4). The inner transverse layer is quite developed and dense in the upper third of the thigh. These transverse fibres run obliquely to anchor strongly to the femur(4). These transverse layers represent part of the fibres that constitute the deep, thick intermuscular septum of the femur. This septum effectively forms an osteo-fascial wall between the anterior quadriceps muscle group and the posterior hamstring muscle group. Fibres from the inner transverse layer also accept the superior fibres of the gluteus maximus to form an ascending tendon. The portion of the posterolateral TFL that did not blend with the MLL also blended with this ascending tendon to insert directly onto the intermuscular septum – and thus the femur. In other words, the majority of the TFL indirectly inserts onto the femur via the ascending gluteal tendon, and indirectly via the blending of the MLL to the thick transverse layer. Further down the thigh, the ITB remains a thickened portion of the fascia lata, creating the fascial barrier between the anterior quadriceps and the posterior hamstrings. It completely surrounds the thigh, is anchored to the distal lateral femoral shaft by strong obliquely directed fibrous strands that can represent a tendon enthuses, and is continuous with the patellar retinaculum(4). The presence of these fibrous anchoring strands divides the ITB into a proximal ‘tendinous’ portion and a distal ‘ligamentous’ portion(4). Therefore Fairclough et al (2006) argue that the TFL has very little involvement in tibia movement and knee function and its role is primarily directed at the hip(4). Based on the current anatomical understanding of the TFL, the following points can be summarised; - The anterolateral fibres of the TFL blend with a component of the MLL that inserts onto the lateral patella retinaculum.
- The posterolateral fibres insert into essentially 2 parts:
1. MLL component that inserts onto the tibia 2. Femur via the ascending gluteal tendon - The superficial MLL appears to course downwards to insert either onto the patella or the tibia.
- The deep MLL inserts onto the femur, via its thick blending with the deep transverse layer of the fascia latae.
This complex arrangement of insertions effectively influences the way the muscle works around the hip and knee. Function Of The TFLAnteromedial fibres (AM)The main role of this functional head is to flex the hip in open kinetic chain movements such as hip flexion during the swing phase of gait. This has been confirmed via EMG and electrical stimulation experiments(1). The muscle becomes silent upon heel strike, suggesting that the muscle needs to be inactive to allow hip extension to occur during stance phase. The muscle is most active during the acceleration phase of running, again suggesting its main role is as a powerful hip flexor(1). In pure open kinetic-chain movement, the AM fibres are most active in hip flexion movements and also in abduction movements. It is silent however if the hip is externally rotated whilst abducting – an important consideration when prescribing hip rehabilitation exercises for the gluteals and other hip external rotators(6). Posterolateral fibres (PL)These fibres are most active during stance phase of gait. This suggests the muscle acts as a major hip stabiliser in single leg stance by activating its hip abduction role. Interestingly the superior portion of the gluteus maximus is also active during this walking phase. Considering that the PL head has fibres that join the tendon coming from the superior gluteus maximus, this suggests that the PL fibres and superior gluteus maximus work synergistically to control pelvic stability in stance phase(1). Both the TFL and gluteus maximus exert their influence as a hip muscle through the investments they have with the MLL, the deep transverse layer of the fascia lata and the intermuscular septum. They effectively insert onto the femur via this complex web of fascia and are thus considered muscles originating at the pelvis and inserting onto the femur. In pure open kinetic chain movements, the PL fibres are active in all hip internal rotation movements and in abduction movements. Similar to the AM fibres, the PL fibres stay silent if the hip is abducting whilst in external rotation(6). Role At The kneeMost of the comprehensive studies investigating the role of TFL in influencing knee movements and patella stability find it difficult to identify a direct role for the TFL in knee function. It almost certainly does not contribute to knee extension, flexion or rotation(4). Therefore, all previous descriptions of the TFL being a synergistic knee extender with the quadriceps or an externally rotator of the tibia can almost certainly be discarded. It is also doubtful that the TFL plays an active role in pulling the patella laterally. The most likely role the TFL has in knee patella stability is indirectly, through maintaining the tension in the fascia lata and thus the distal portion of the ITB that blends with the patella retinaculum(10). The TFL As A ‘Fascial Tensioner’It has been suggested that the TFL also acts on the fascia latae of the thigh by maintaining fascia tension during movement. Mike Benjamin in 2009 highlighted how extensive the fascia lata of the thigh is(7). It is a complex arrangement of fascial planes that have variable thickness and development over the thigh. It has a loose anterior and posterior layer, which cover the quadriceps and hamstrings respectively. The loose anterior superficial layer would most likely ‘bunch up’ during knee extension movements if there did not exist some manner of tensioning system for the fascia to maintain the fascial envelope. Similarly, the posterior fascia latae would most likely bunch up during knee flexion movements. The most likely muscles to maintain this fascial tension during knee movement, based on their anatomical arrangement with the fascia lata would be the TFL anteriorly and superior gluteus maximus posteriorly. That is, the TFL would become slightly active in knee extension to gradually retract the fascia upwards whilst the knee extended – to prevent crimping and buckling of the anterior fascia. Similarly, the gluteus maximus can maintain fascial tension during knee flexion movements. Femur Tensile ForceOne of the most fascinating roles assigned to the ITB is the role it has in reducing the bending and tensile force on the lateral femur. Humans walk on two feet, and for a part of the gait cycle they are in one-leg stance. This can create large lateral femur tensile forces and medial femur compression forces, which if left unchecked, would create a varus effect of the femur and effectively ‘bow’ the femur. In 1982, Jacob and Huggler (1982) investigated the function of the ITB and concluded that the varus bending forces on the femur could be partially relieved by tensioning the ITB(8). Even earlier than this, Rybicki et al (1972) looked at the stresses on the femur caused by the varus force on the bone and also found that by increasing the tension in the ITB the lateral tension force and the medial compression force on the femur would both be reduced(9). The attached musculature such as the TFL and gluteus maximus would further tension the ITB and reduce this lateral tension force on the femur. Feto et al (2002) provide a comprehensive biomechanical review of the role that the ITB and associated muscles play on creating a ‘compression gradient’ along the lateral femur – effectively preventing distortion of the lateral femur due to the tensile effect of downwardly directed gravity on the varus forces acting on the femur(5). TFL DysfunctionFor all the problems that the TFL poses to patients and therapists alike, almost nothing exists in the literature that highlights the role this muscle has in dysfunction. All theories and ideas are based on clinical reasoning and assumptions. The most interesting observation regarding TFL and dysfunction is the role it has in causing hip internal rotation/flexion during the stance phase of gait. It is common and habitual for patients complaining of lower limb overuse injuries or low back/SIJ pain to demonstrate an exaggerated hip flexion/ internal rotation position during functional movements on one leg. That is, they demonstrate a positive Trendelenberg sign during one-leg stance (opposite side of pelvis drops down) and the stance hip assumes an internally rotated and flexed position. It appears as if they are ‘dropping out the back pocket’ on their stance leg. This pathomechanic then creates a valgus collapse at the knee joint, and this has a direct mechanical influence on the ‘Q angle’ of the knee. With an increase in the ‘Q angle’ the patella has a tendency to drag laterally and compress against the lateral femoral condyle. This may then lead to patellofemoral pain at the knee. The most plausible explanation for the Trendelenburg sign and the valgus knee collapse is that the TFL maintains pelvic stability in one-leg stance by initiating its abduction role. However if unchecked, the TFL will also exhibit its hip flexion/internal rotation role. The gluteus maximus and other hip external rotators should in theory check this flexion/internal rotation by providing and equal and opposite external rotation/extension role. Gottschalk et al (1989) highlighted how the gluteus medius and minimus primarily act on the hip joint by providing a compressive and stabilising role. They do little to assist in maintaining a stable pelvic position. This role is assigned to the TFL and gluteus maximus(3). The underlying principle behind why the TFL is such an influential muscle in pelvic dysfunction, is that the TFL has the greatest mechanical advantage to influence the pelvis and hip joint. It is the most anterior muscle at the front of the hip. It therefore has the greatest leverage advantage to induce a flexion posture or an anterior tilt of the ilium. Viewing the hip from in front, the TFL is also the most lateral muscle on the hip. It also therefore has the greatest leverage to affect abduction of the hip. This explains why such as small muscle can have such a large influence. ManagementAssessing tightness in the TFL can be performed using an ‘Ober Test’ or a ‘Thomas Test’. Ober test (see figures 2a and 2b)Start position – The client is positioned in side-lying, with the unaffected side down. The pelvis and spine are in neutral alignment, with the bottom leg flexed for support. The uppermost leg is extended and needs to be above the horizontal. The hip is laterally rotated and extended, as far as no lumbar extension occurs. Movement – The client actively flattens the waist towards the floor and holds the leg in slight abduction and lateral rotation. He/she client is then instructed to slowly lower the leg towards the floor until the TFL-ITB hangs on the greater trochanter and cannot lower any further. The key to an accurate test is not letting the pelvis move, either into lateral tilt, anterior tilt or rotation. As the leg lowers, the hip should not flex or medially rotate. It’s essential to maintain the laterally rotated position of the hip. Ideally, the leg should lower into at least 10 to 15 degrees adduction without loss of proximal control of the pelvis or hip. The TFL-ITB lacks extensibility if the leg does not adduct sufficiently. Thomas test (see figure 3)On a plinth, the patient lies supine, with the untested leg held in hip flexion. The tested leg is then forced into extension and adduction. If the tested leg is unable to attain a horizontal alignment and is held in flexion and/or abduction, this is indicative of tightness in the TFL. Managing Tightness In The TFLManaging the overactive/tight TFL comes with 2 important criteria: it must be stretched and it must be massaged/ manipulated. The most effective stretch for the TFL is in the knee-down hip flexor stretch (see figure 4). If you are stretching the left TFL: 1. Kneel on the left knee with the right leg at 90 degrees hip flexion and knee flexion. 2. Push the left hip forward until the slack is taken up (this takes up the flexion component). 3. Place your hands on the right thigh and twist the trunk around to the right whilst the pelvis remains facing forward (this induces an external rotation of the hip which adds to the rotation component of the stretch). 4. If you have any slack left, push the left outwards (this takes up the abduction component). 5. Finally, isometrically contract the right hamstring by attempting to drag the left heel backwards (this induces posterior pelvis tilt that takes up the anterior tilt component). To self massage or trigger the TFL (figure 5), have the client lie on their side and place a trigger ball/Muscle Mate/Posture Pro under the TFL and apply gentle pressure. The hip, knee and ankle need to stay in a straight line with the body. This can be performed as a rolling type movement or as sustained pressure to relieve the trigger points within the muscle. ConclusionTFL is a muscle that acts both on the hip joint to create hip/pelvic dysfunction and it also acts on creating tension in the fascia latae and its specialised portion known as the ITB. Overactivity in this muscle can create a direct mechanical effect that creates excessive lateral tension on the patella and thus patellofemoral pain and it can also be implicated in low back syndromes that are caused by excessive anterior pelvic tilt and lumbar spine extension. It is a muscle that needs regular massage and stretching. References
1. Journal of Bone and Joint Surgery. 1981. 63: 1457-1471
2. Journal of Bone and Joint Surgery. 1958. 40: 817-832
3. Journal of Anatomy. 1989. 166: 179-189
4. J of Anatomy. 2006. 208; 309-316
5. J Orthop Sci. 2002. 7:724–730
6. Journal of orthopaedic & sports physical therapy. 2013. 43(2); 54-65
7. Journal of Anatomy. 2009. 214: 1-18
8. Jacob HA, Huggler AH. In vivo investigations of the mechanical function of the tractus iliotibialis. In Huiskes R, von Campen DH, de Wijn JR, editors. Biomechanics, principles and applications: selected proceedings of the 3rd
General Meeting of the European Society of Biomechanics, Nijmegen, The Netherlands, January 1982. The Hague: Nijhoff; 1982
9. J Biomech. 1972;5:203–15
10. Journal of Arthroscopic and Related Research. 2007. 23(3): 269-274
In the first part of his two-piece review on psoas major (PM), Dr. Alexander Jimenez discussed the relevant and complex anatomy and biomechanics of this unique and misunderstood muscle. In part two, Dr. Jimenez looks at how PM dysfunction may manifest as a musculoskeletal problem, and the corrective interventions a therapist can use to manage PM dysfunction.
PM & Lumbar Back Pain
Anecdotally, many therapists clinically find that patients with acute low back pain have myofascial trigger points in the PM when the muscle is palpated. Often deep trigger point releases into the PM can help alleviate and reduce the symptoms of low back pain. However, it is unclear whether the clinical correlation between low back pain and PM hypertonicity is causative. Is the hypertonic PM the cause of the back pain, or does it reflexively tighten up in the presence of back pain as a protective mechanism?
In the ageless text ‘Myofascial Pain and Dysfunction’ by Janet Travel and David Simons, the iliopsoas is referred to as the ‘hidden prankster’(1). They argue that the muscle is deep, hard to locate and can often hide trigger points that can masquerade as low back pain, which extends up and down the spine on the same side as the PM dysfunction (see Figure 1 below).
Often patients who complain of PM trigger points will complain of a deep unilateral low back pain that radiates up and down the spine, with possible referral into the anterior thigh and groin area. Often the pain is felt to be worse when standing upright, lying flat on the back and relieved by sitting down.
The primary weakness in this clinical view is that the differentiation between PM and iliacus is not made. It is possible that if the PM and iliacus are indeed separate functional muscles then these myofascial trigger points may exist in the iliacus and not necessarily the PM. What is also interesting is that Travel and Simons do note the close association between the PM and nerves such as the ilioinguinal, iliohypogastric and obturator. Due to the close proximity of the PM to these nerves, it may be also clinically argued that hypertonicity in the PM may compress and/or irritate these nerves, and this may manifest with the client complaining of groin pain or pain into the perineum area.
These ideas are further supported by Johnson et al (1998), who stated that myofascial pain from the PM muscle will often present as anterior hip and/or lower back pain(2). Referral areas include the anterior thigh. The PM muscle can be considered as a pain source in athletes, office workers or anyone who spends much of their day sitting. PM myofascial pain is thought to be prevalent in certain sports including soccer, dance, and hockey.
More recently there has been some research that highlights the association between low back pain and PM dysfunction. Some of the findings of these studies are as follows:
1. In a cohort study examining the cross- sectional area of the PM in healthy volunteers and subjects with unilateral sciatica caused by a disc herniation, most patients with a lumbar disc herniation showed a significant reduction in the cross-sectional area of the PM on the affected side only and most prominently at the level of the disc herniation(3).
2. This was further supported in a study that investigated the cross-sectional area of the PM in the presence of unilateral low-back pain through the utilisation of magnetic resonance imaging (MRI). It was found that the cross-sectional area of the bilateral PM was on average 12% smaller on the side of the low-back pain. Furthermore, there was a positive correlation between a decreased cross-sectional area of the PM and the duration of symptoms(4).
3. These studies correlate well with other studies that have found specific atrophy in multifidus in patients with low-back pain. The same mechanism of inhibition due to perceived pain may be responsible for the PM atrophy(5).
Assessment Of PM Dysfunction
Due to the deep position of the PM and the difficulty in accessing the muscle directly, PM dysfunction is often inferred based on clinical signs and symptoms. These include the location of low-back pain (usually believed to be alongside the spine in a vertical direction), the primary positions of discomfort such as lying flat on the back or standing up straight, and perhaps also in the presence of poorly functioning transversus abdominus that may lead the PM to ‘overcompensate’ in its role as a lumbo-pelvic stabiliser.
A simple clinical assessment would be to palpate the PM, and apply gentle ischaemic pressure to the muscle to relieve some active myofascial trigger points. Painful movements can then be reassessed to determine the role that PM trigger points may have in the presentation of the patient’s low-back pain.
PM also has a role to play in creating lumbar spine stiffness due to its action as an axial compressor of the spine. This function can directly be assessed in terms of the ability of the client to activate the PM, with the therapist then assessesing joint play of the vertebrae before and after activation (Gibbons 2007)(6). This process is described below under retraining of the PM.
Managing Myofascial ‘Tightness’ In The PM
As mentioned above, it is a long-held historical clinical belief that PM may become tight and develop myofascial trigger points, and be the source of, or consequence of low-back pain. With this in mind, many clinicians and therapists apply direct massage techniques, digital pressure ischaemic techniques and stretching exercises to directly manage the myofascial trigger points and tightness.
These approaches can be performed in many ways. However one of the preferred ways is to have the client lie on their side. This is a comfortable position for the client to lie in as the abdominals relax and it is easier for the therapist to palpate the PM. Furthermore, the abdominal organs will displace medially in this posture, which means the therapist is unlikely to be creating discomfort to the intra- abdominal organs. This technique is shown in Figure 2.
Retraining PM Function
The credit for the following content on retraining PM weakness and dysfunction is given to Gibbons, who has collated a comprehensive exercise battery on retraining PM dysfunction(6). In this extensive review on PM retraining, Gibbons explains how the specific motor control and stability exercises for the PM involve axial shortening, or attempting to bring the insertion closer to the origin along its vertical axis.
This action creates axial compression along the lumbar vertebral segments, thus increasing lumbar spine rigidity, which in turn increases stability. Furthermore, the femoral insertion of the PM will displace the head of the femur up in the acetabulum and create hip joint stability, and prevent excessive anterior shear forces acting on the hip joint. Therefore, an effective PM contraction will stabilise and resist translational movements in the hip joint, sacroiliac joint and lumbar spine joints.
The essential cue for the therapist to teach the client is an action of ‘pulling in the hip’ or ‘shortening the leg’. This movement needs to be very specific to the hip joint and not created by lateral tilt or ‘hitching’ of the pelvis, anterior or posterior tilt of the pelvis or rotation of the pelvis. Moreover, this needs to be performed against a background of sound diaphragmatic breathing control.
It is beyond the scope of this paper to describe in detail the multi-stage system of retraining PM function. The reader is therefore directed to the reference given for more precise details on how this system is utilised in retraining PM function. However, in summary, the primary points to note in each stage opposite.
Conclusion
The PM is a unique, complex and misunderstood muscle that has for many years been described as primarily a hip flexor along with iliacus. However, new research suggests that the PM is quite complex in its anatomical arrangement with the lumbar spine, pelvic rim/brim and femur, and also its attachments to the diaphragm, pelvic floor and iliacus.
It is now thought that the PM has many functional roles and these are primarily due to the unique anterior and posterior fascicle arrangement. This suggests that the posterior fascicles are important lumbar spine stabilisers, and work in connection with other spine stabilisers as an integrated complex of myofascial tissue.
Dysfunction of the PM may manifest as hypertonicity in the muscle, which may suggest to a clinician that the muscle is compensating for dysfunction in other lumbar stabiliser muscles. It may also become dysfunctional in motor control and not provide sufficient axial compression of the lumbo-pelvic girdle. A series of motor retraining exercises can be used to regain this function.
References
1. Travel and Simons. Myofascial Pain and
Dysfunction. The Lower Extremities (Volume 2).
Lippincott Williams and Wilkins. Philadelphia.
2. Sports Med. 1998; 25(4):271–283
3. Spine. 1998; 23(8):928-931
4. Spine. 2008; 33(26): E983–E989.
5. Spine. 1994; 19(2):165-172
6. Gibbons SGT 2007 Assessment and
rehabilitation of the stability function of psoas
major. Manuelle Therapie. 11:177-18
|



 Your new post is loading...
Your new post is loading...








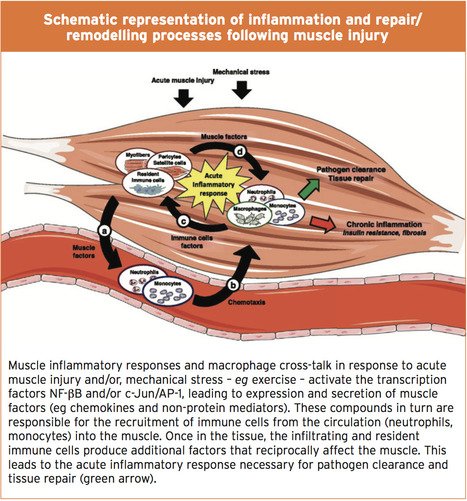
















Uncover the mystery of muscle spasms, performance anxiety, and more. Learn how athletes can overcome this frustrating condition. For answers to any questions you may have, call Dr. Alex Jimenez at 915-850-0900 or 915-412-6677