Your new post is loading...
 Your new post is loading...

|
Scooped by
Gilbert C FAURE
January 4, 3:53 AM
|
Rheumatoid arthritis is an autoimmune disease that affects ~1% of the global population and leads to joint inflammation, local bone erosions and systemic bone loss. The disability and immobility caused by inflammatory bone loss, joint destruction and fractures in rheumatoid arthritis present a clinical challenge and impose a considerable socioeconomical burden. Osteoclasts have the unique ability to resorb bone and cause bone loss. A comprehensive understanding of the regulatory mechanisms of osteoclasts and their crosstalk with stromal cells, such as osteoblasts, or immune cells during inflammation is essential for the development of targeted therapies to prevent and treat bone loss. The objective of this Review is to present a comprehensive overview of the current knowledge of osteoclast regulation at different levels: from systemic pathways to changes in the bone microenvironment, including the involvement of local cells, to osteoclast-intrinsic regulation such as metabolic adaptations. We also discuss some of the current and emerging therapies that can counteract inflammatory bone loss. The factors and mechanisms that regulate osteoclast-induced inflammatory bone loss are complex. The authors of this Review provide an overview of osteoclast regulation in the context of inflammatory bone loss and rheumatoid arthritis and provide insights into potential treatment strategies.

|
Scooped by
Gilbert C FAURE
December 8, 2024 4:06 AM
|
This eLearning course has been designed to educate healthcare professionals (HCPs) on the management of rheumatoid arthritis with interleukin-6 receptor inhibition therapy, with a specific focus on tocilizumab and its biosimilars.

|
Scooped by
Gilbert C FAURE
February 29, 2024 2:11 AM
|
Rheumatoid arthritis (RA) is a chronic autoimmune disease that affects millions of individuals worldwide, causing pain, inflammation, and joint damage. Despite its prevalence, RA can be misunderstood, leading to challenges in diagnosis and management.

|
Scooped by
Gilbert C FAURE
December 20, 2023 8:37 AM
|
WHAT IS ALREADY KNOWN ON THIS TOPICMonoclonal therapy for one inflammatory disease may paradoxically trigger another inflammatory disease.Recent case reports have implicated an association between anti-IL-5 (IL, interleukin) antibody therapy used to treat severe asthma and the development of rheumatoid arthritis (RA).WHAT THIS STUDY ADDSOut of 142 patients within our asthma service taking anti-IL-5 antibody therapy for at least 1 month, and with a mean duration of 3.5 years on therapy, only one developed RA suggesting that RA is a relatively uncommon complication in the short-medium term.HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICYTreating clinicians should be mindful of the possibility of developing inflammatory arthritis following the initiation of anti-IL-5 therapy and ensure appropriate review and assessment should their patient develop arthralgia as, while uncommon, these could represent a significant source of morbidity.IntroductionThere has been a wide adoption of monoclonal antibody therapy in rheumatology, respiratory medicine, and an increasing number of specialties for the treatment of many inflammatory diseases. Of particular interest is that monoclonal therapy for one inflammatory disease may paradoxically trigger another inflammatory disease. Pertinent examples include tumour necrosis factor inhibitor therapy triggering multiple sclerosis,1 interleukin 17 (IL-17) therapy for psoriasis linked to inflammatory bowel disease2 and more recently IL-4/13 blockade used for atopic dermatitis being associated with de novo psoriasis and arthritis.3 4Arthralgias are a known adverse effect of anti-IL-5 biologics,5 6 however, a few recent case reports have found this association may extend to inflammatory arthritis such as RA.7 8 The prevalence of these findings across a wider cohort of patients remains relatively unknown. Here we present an audit from a large, single-centre’s severe asthma service which looks for the prevalence of RA across all patients being treated with mepolizumab and benralizumab, two commonly used anti-IL-5 therapies.MethodsAll patients with severe eosinophilic asthma across the Leeds Teaching Hospitals NHS Trust’s (LTHT) Respiratory Service, who had received at least 1 month of mepolizumab or benralizumab therapy, were included in this clinical audit.Each patient’s electronic records, including hospital records, clinic letters, general practitioner (GP) records and electronic pathology results were searched. We recorded whether patients had presented with any signs or symptoms of synovitis (eg, joint pain, swelling and tenderness) either prior- or post-commencing biologics, whether their serology (rheumatoid factor (RF) and/or anti-CCP antibody (ACPA)) and acute phase reactants (C- Reactive Protein (CRP) and/or Erythrocyte Sedimentation Rate (ESR)) had been measured and the timing and duration of their symptoms. Using this information, we then calculated the number of points each patient with symptoms would score on the ACR/EULAR 2010 Rheumatoid Arthritis classification criteria.9 We also recorded the dose of routine steroids the patients were receiving prior to starting biologics, and whether they were weaned off steroids within 1 year of commencing biologics. Finally, we recorded whether the patients had been seen in our early arthritis clinic and received a formal diagnosis on an inflammatory arthritis.ResultsA total of 142 patients (57 males, 85 females and mean age 58.2 years old) were being treated with anti-IL-5 biologics under the LTHT’s severe asthma clinic, with a mean duration of 3.5 years on therapy. Eighty-nine were on mepolizumab and 53 on benralizumab. The mean daily dose of steroids prior to starting anti-IL-5 therapy was 6.0 mg prednisolone, reducing to 3.1 mg at 1 year post-therapy. Seventy-five patients were steroid-free after 1 year of therapy.Only one patient among 500 patient years of exposure to anti-IL-5 therapy received a formal diagnosis of RA suggesting an overall annual incidence of 20 cases per 10 000 patients (95% CI 2.8 to 142). This man in his 70s presented to our early arthritis clinic 18 months after having been started on mepolizumab for his severe eosinophilic asthma. Prior to starting biologics, his asthma had been poorly controlled with salbutamol, budesonide/formoterol combination inhaler, tiotropium inhalers and daily low-dose oral corticosteroids. Within weeks, he developed symmetrical arthralgia involving small joints, particularly his wrists and knuckles, as well as significant early morning stiffness lasting more than 1 hour. On examination, he had clinical synovitis in the wrists and metacarpophalangeal joints bilaterally, as well as right shoulder capsulitis with limiting range of motion.Blood tests revealed a raised CRP of 24 mg/L, White Cell Count (WCC) 8.77 10 × 9 /L, RF of 263.2 iu/mL (normal<14.0) and an ACPA of >300 U/mL (normal<2.99). Ultrasound imaging of the hands and wrists showed bilateral grade II grey scale with grade II power Doppler (figure 1) with bilateral wrist erosions. There was hypoechogenicity of the left extensor carpi ulnaris tendon with some associated grey scale and power Doppler. MRI of the left hand revealed extensive subchondral bone marrow oedema (figure 1) and multiple erosions across all carpal bones and carpometacarpal joints (figure 1).<img width="342" alt="Figure 1" height="440" class="highwire-fragment fragment-image" src="https://rmdopen.bmj.com/content/rmdopen/9/4/e003583/F1.medium.gif">Download figure Open in new tab Download powerpoint Figure 1 (A) Fat suppression MRI of the left wrist and MCPs showing extensive bone oedema (white arrows) and joint effusion (black asterisk). (B) T1-weighted MRI of the left wrist showing diffuse erosions of the left wrist (white arrows). (C) Longitudinal ultrasound image showing synovitis of the right wrist with grey scale (white asterisk) and power Doppler (white arrow).He was diagnosed with RA as per the American College of Rheumatology (ACR)/EULAR classification criteria and started on prednisolone 10 mg daily to control the inflammation, followed by sulfasalazine 1 month later as the disease modifying agent. He was followed-up in rheumatology clinic 2 months later and showed significant improvements: the joint pain and swelling had settled, and while he still experienced early morning stiffness, this was less debilitating. His inflammatory markers had also resolved with CRP<5.0 mg/L and WCC 9.31 10 × 9 /L.Of the remaining 141 patients, 16 developed bilateral polyarthralgia of greater than 1 month duration (eight mepolizumab and eight benralizumab), with a median onset of 12 months after commencing a biological therapy. Of these patients 9/16 were tested for RF and ACPA and in all cases, their serology was negative; 15/16 patients had acute phase inflammatory markers measured and these were only elevated in three patients. All 16 of these patients were on a maintenance dose of prednisolone prior to starting the biologic (mean dose 10.1 mg/day), with 10 of them completely weaned off steroids within 12 months.Using the information available from the patient’s electronic records, the mean number of points scored on the ACR/EULAR RA criteria was 3.2 (range 1–6). The patient who scored six points was reviewed in the early arthritis clinic and the symptoms were felt to be more in keeping with osteoarthritis than an inflammatory arthritis. Similarly, none of the other patients had received a confirmed diagnosis of inflammatory arthritis by either their GP or by a rheumatologist.Only one other patient became newly RF positive (17.1 iu/mL), 1 month after commencing mepolizumab; however, this seemed to be an incidental finding as the patient had a broad set of bloods taken while admitted to the intensive care unit for a severe exacerbation of asthma, and at no point since has complained of rheumatological symptoms.We were unable to access the GP records for 37 patients and as such could not review whether they had presented to their GPs with new rheumatological symptoms. However, we were able to access their pathology test records electronically and found no evidence of positive RA serology in any of these patients and no rheumatological referrals to our centre that has a well-developed early RA network.DiscussionThere is an emerging interest in IL-5 blockade and the potential development of RA. We present a single-centre’s experience of 500 patient years on anti-IL-5 monoclonal antibody exposure therapy for severe asthma.As expected, arthralgias were a relatively common side-effect of anti-IL-5 therapy. As for progression to RA, we found only one convincing case. While relatively low, the implied annual incidence of 20 cases per 10 000 patients is several fold higher than the annual incidence of RA in the UK (1.5 per 10 000 men and 3.6 per 10 000 women).10 Given the wide CIs, however, no firm conclusions can be offered in relationship to our single case and to the relative risk of RA following anti-IL-5 therapy.A major confounding variable is the weaning of steroids in most patients started on biologics. This poses a challenge in associating the development of symptoms with the initiation of the anti-IL-5 therapy, as opposed to the withdrawal of steroids unmasking a pre-existing disease. Additionally, one must consider whether the risk of developing RA is modified by the underlying condition, and indeed there is some evidence to suggested that asthma may be positively associated with RA.11 However, these population-based studies look at asthma as a whole, rather than divided into its endotypes (eg, eosinophilic vs neutrophilic asthma) and as such these have not yet challenged the conventional belief that Th1 and Th2 diseases are inversely related.Emerging evidence has implicated a core role for regulatory eosinophils (rEos) in the resolution of RA.12 In murine models of RA, the expansion of rEos in the synovial fluid as a by-product of inducing eosinophilic asthma was sufficient in bringing about remission of arthritis, and inhibiting the IL-5 pathway would subsequently induce relapse of the arthritis.12 Further evidence supporting a role for rEos in RA can be found at a genetic level where Eotaxin-3, one of the main drivers of eosinophil recruitment, has single nucleotide polymorphisms associated with RA13 and from studying the role of IL-5 in Th2 responses to Helminth infections,14 with mouse models of RA also identifying Helminth infections as protective.15 Hence, the suggestion that the expansion of eosinophils in the synovium ‘regulate’ the proinflammatory Th1 pathways driving synovial inflammation.12 This invites the notion that in a patient with subclinical, yet endogenously controlled, synovial inflammation, removing rEos by administering anti-IL-5 therapeutics may tip the balance in favour of inflammation and permit symptomatic disease. However, if there is little proinflammatory Th1 synovial activity in the first place, then inhibiting rEos with anti-IL-5 biologics may be insufficient to precipitate an inflammatory arthritis.Interestingly, there is debate as to whether rEos are depleted to varying degrees depending on the anti-IL-5 biologic used. In mice, inflammatory eosinophils (iEos)—the primary targets of anti-IL-5 biologics in asthma—may be dependent on IL-5 for activity, whereas rEos may not be.16 This would suggest that benralizumab, a high-affinity IL-5 receptor antagonist,17 would deplete both iEos and rEos through NK-mediated killing, whereas mepolizumab, an anti-IL-5 monoclonal antibody,17 may deplete iEos but keep rEos intact. However, this idea has recently been challenged with evidence that anti-IL-5 treatment depletes all populations of eosinophils.18 Whether this distinction would result in a different pattern of adverse effects in patients remains unclear, notably as the patient who developed RA in this report was receiving mepolizumab.As an audit, this study serves to identify the prevalence of a relatively rare complication of anti-IL-5 therapy. We were unable to find clear evidence for a pattern of emergent RA nor other inflammatory arthritis in our cohort of 142 patients. Further studies may be required to characterise the nature and significance of these findings in clinical groups and to identify whether there is an actual association between novel anti-IL-5 biologics and RA.Data availability statementThe data that support the findings of this study are available upon reasonable request.Ethics statementsPatient consent for publicationConsent obtained directly from patient(s).Ethics approvalThis study was registered as a clinical audit and given the retrospective nature of the data collection process did not require formal ethical approval. In completing this audit, full ethical standards were upheld in accordance with the principles of clinical governance. From the one patient whose details were discussed in more detail we have gained full written consent.References↵Sicotte NL, Voskuhl RR. Onset of multiple sclerosis associated with anti-TNF therapy. Neurology 2001;57:1885–8. doi:10.1212/wnl.57.10.1885OpenUrlCrossRefPubMed↵Hohenberger M, Cardwell LA, Oussedik E, et al. Interleukin-17 inhibition: role in psoriasis and inflammatory bowel disease. J Dermatolog Treat 2018;29:13–8. doi:10.1080/09546634.2017.1329511OpenUrlPubMed↵Bridgewood C, Newton D, Bragazzi N, et al. Unexpected connections of the IL-23/IL-17 and IL-4/IL-13 cytokine axes in inflammatory arthritis and enthesitis. Semin Immunol 2021;58:101520. doi:10.1016/j.smim.2021.101520OpenUrl↵Bridgewood C, Wittmann M, Macleod T, et al. T helper 2 IL-4/IL-13 dual blockade with dupilumab is linked to some emergent T helper 17‒Type diseases, including seronegative arthritis and enthesitis/enthesopathy, but not to humoral autoimmune diseases. J Invest Dermatol 2022;142:2660–7. doi:10.1016/j.jid.2022.03.013OpenUrl↵Harrison T, Canonica GW, Chupp G, et al. Real-world Mepolizumab in the prospective severe asthma REALITI-A study: initial analysis. Eur Respir J 2020;56:2000151. doi:10.1183/13993003.00151-2020↵Liu W, Ma X, Zhou W. Adverse events of benralizumab in moderate to severe eosinophilic asthma: a meta-analysis. Medicine (Baltimore) 2019;98:e15868. doi:10.1097/MD.0000000000015868↵Kawabata H, Satoh M, Yatera K. Development of rheumatoid arthritis during anti-Interleukin-5 therapy in a patient with refractory chronic eosinophilic pneumonia. J Asthma Allergy 2021;14:1425–30. doi:10.2147/JAA.S342993OpenUrl↵Dupin C, Morer L, Phillips Houlbracq M, et al. Arthritis, a new adverse effect of anti-Il5 Biologics in severe asthma patients. European Respiratory Journal 2022;60:2432. doi:10.1183/13993003.congress-2022.2432OpenUrlCrossRef↵Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American college of rheumatology/European League against rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–81. doi:10.1002/art.27584OpenUrlCrossRefPubMedWeb of Science↵NICE guideline. Overview: rheumatoid arthritis in adults: management [Guidance, NICE]. 2018. Available: https://www.nice.org.uk/guidance/ng100 [Accessed 25 Sep 2023].↵Rolfes MC, Juhn YJ, Wi C-I, et al. Asthma and the risk of rheumatoid arthritis: an insight into the heterogeneity and phenotypes of asthma. Tuberc Respir Dis (Seoul) 2017;80:113–35. doi:10.4046/trd.2017.80.2.113OpenUrl↵Andreev D, Liu M, Kachler K, et al. Regulatory eosinophils induce the resolution of experimental arthritis and appear in remission state of human rheumatoid arthritis. Ann Rheum Dis 2021;80:451–68. doi:10.1136/annrheumdis-2020-218902OpenUrlAbstract/FREE Full Text↵Guellec D, Milin M, Cornec D, et al. Eosinophilia predicts poor clinical outcomes in recent-onset arthritis: results from the ESPOIR cohort. RMD Open 2015;1:e000070. doi:10.1136/rmdopen-2015-000070↵Mishra PK, Palma M, Bleich D, et al. Systemic impact of intestinal helminth infections. Mucosal Immunol 2014;7:753–62. doi:10.1038/mi.2014.23OpenUrlCrossRefPubMed↵Osada Y, Shimizu S, Kumagai T, et al. Schistosoma Mansoni infection reduces severity of collagen-induced arthritis via down-regulation of pro-inflammatory mediators. Int J Parasitol 2009;39:457–64. doi:10.1016/j.ijpara.2008.08.007OpenUrlCrossRefPubMed↵Mesnil C, Raulier S, Paulissen G, et al. Lung-resident eosinophils represent a distinct regulatory eosinophil subset. J Clin Invest 2016;126:3279–95. doi:10.1172/JCI85664OpenUrlCrossRefPubMed↵Caminati M, Menzella F, Guidolin L, et al. Targeting eosinophils: severe asthma and beyond. Drugs Context 2019;8:212587. doi:10.7573/dic.212587OpenUrl↵Dolitzky A, Grisaru-Tal S, Avlas S, et al. Mouse resident lung eosinophils are dependent on IL-5. Allergy 2022;77:2822–5. doi:10.1111/all.15362OpenUrl

|
Scooped by
Gilbert C FAURE
September 9, 2023 5:00 AM
|
Imagine that 100 years from now, your great granddaughter, an eminent rheumatologist, reviews the history of rheumatoid arthritis mimics.

|
Scooped by
Gilbert C FAURE
June 17, 2023 7:02 AM
|
Audio Rheum Editor’s Picks Dr. Earl D. Silverman, MD, shares his monthly Editor’s Picks and their relevance in current clinical practice: June 2023 Featured articles: Kiltz, et al: Clinimetric Validation of the Assessment of Spondyloarthritis International Society Health Index in Patients With Radiographic Axial Spondyloarthritis in Ixekizumab Trials Alduraibi, et al: Clustering Patients With Gout Based on Comorbidities and Biomarkers: A Cross-Sectional Study Primeau, et al: Responders to Medial Opening Wedge High Tibial Osteotomy for Knee Osteoarthritis Kumthekar, et al: Physical Activity Habits Among Older Adults Living With Rheumatic Disease Wohlfahrt, et al: Pain Mechanisms Associated With Disease Activity in Patients With Rheumatoid Arthritis Treated With Disease-Modifying Antirheumatic Drugs: A Regression Tree Analysis May 2023 Featured articles: Cook, et al: Comparative Effectiveness of BNT162b2 and mRNA-1273 Vaccines Against COVID-19 Infection Among Patients With Systemic Autoimmune Rheumatic Diseases on Immunomodulatory Medications Chen, et al: Validation of the Antineutrophil Cytoplasmic Antibody Renal Risk Score and Modification of the Score in a Chinese Cohort With a Majority of Myeloperoxidase-Positive Patients Gorzewski, et al: Predicting Disease Activity in Rheumatoid Arthritis With the Fibromyalgia Survey Questionnaire: Does the Severity of Fibromyalgia Symptoms Matter? Oguro, et al: Effect of Communicative and Critical Health Literacy on Trust in Physicians Among Patients With Systemic Lupus Erythematosus (SLE): The TRUMP2-SLE Project Barber, et al: Investigating Associations Between Access to Rheumatology Care, Treatment, Continuous Care, and Healthcare Utilization and Costs Among Older Individuals With Rheumatoid Arthritis April 2023 Featured articles: Coates, et al: Sex-Specific Differences in Patients With Psoriatic Arthritis: A Systematic Review Johnson, et al: Evaluating the Threshold Score for Classification of Systemic Lupus Erythematosus Using the EULAR/ACR Criteria Gong, et al: The Association Between Quadriceps Strength and Synovitis in Knee Osteoarthritis: An Exploratory Study From the Osteoarthritis Initiative Jatuworapruk, et al: Prevalence, Risk Factors, and Outcomes of Gout Flare in Patients Hospitalized for PCR-Confirmed COVID-19: A Multicenter Retrospective Cohort Study Bosch, et al: Etanercept Withdrawal and Retreatment in Nonradiographic Axial Spondyloarthritis: Results of RE-EMBARK, an Open-Label Phase IV Trial March 2023 Featured articles: Takanashi, et al: Effects of Aging on Rheumatoid Factor and Anticyclic Citrullinated Peptide Antibody Positivity in Patients With Rheumatoid Arthritis Kiltz, et al: Clinically Relevant Deficits in Performance Tests in Patients With Axial Spondyloarthritis Schletzbaum, et al: Age-Stratified 30-day Rehospitalization and Mortality and Predictors of Rehospitalization Among Patients With Systemic Lupus Erythematosus: A Medicare Cohort Study Berard, et al: Canadian Rheumatology Association Recommendations for the Screening, Monitoring, and Treatment of Juvenile Idiopathic Arthritis-Associated Uveitis Schultz, et al: B Cell Reconstitution is Associated With COVID-19 Booster Vaccine Responsiveness in Patients Previously Seronegative Treated With Rituximab February 2023 Featured articles: Macfarlane, et al: Inflammatory Bowel Disease Risk in Patients With Axial Spondyloarthritis Treated With Biologic Agents Determined Using the BSRBR-AS and a MetaAnalysis Gossec, et al: Women With Psoriatic Arthritis Experience Higher Disease Burden Than Men: Findings From a Real-World Survey in the United States and Europe Davis, et al: The Effect of Psychiatric Comorbidity on Healthcare Utilization for Youth With Newly Diagnosed Systemic Lupus Erythematosus Pyo, et al: The Reclassification of Patients With Previously Diagnosed Eosinophilic Granulomatosis With Polyangiitis Based on the 2022 ACR/EULAR Criteria for Antineutrophil Cytoplasmic Antibody–Associated Vasculitis Weng, et al: Adult-Onset Still Disease After ChAdOx1 nCOV-19 Vaccination Mitchell, et al: How to Provide Sexual and Reproductive Health Care to Patients: Focus Groups With Rheumatologists and Rheumatology Advanced Practice Providers January 2023 Featured articles: Kodishala, et al: Risk Factors for Dementia in Patients With Incident Rheumatoid Arthritis: A Population-Based Cohort Study Beauvais, et al: Development and Validation of a Self-Administered Questionnaire Measuring Essential Knowledge in Patients With Axial Spondyloarthritis Orbai, et al: Impact of Physician-Defined Flares on Quality of Life and Work Impairment: An International Survey of 2238 Patients With Psoriatic Arthritis Smitherman, et al: Patient-Reported Outcomes Among Transition-Age Young Adults With Juvenile Idiopathic Arthritis in the Childhood Arthritis and Rheumatology Research Alliance Registry Stull, et al: Cutaneous Involvement in Systemic Lupus Erythematosus: A Review for the Rheumatologist Masi, et al: Reflections for the 50th Anniversary of The Journal of Rheumatology: The Past, Present, and Future of Rheumatology Santos, et al: A Rare Case of Subcutaneous Sarcoidosis in Patient With Psoriatic Arthritis Garg, et al: Timing and Predictors of Incident Cardiovascular Disease in Systemic Lupus Erythematosus: Risk Occurs Early and Highlights Racial Disparities December 2022 Featured articles: Koo, et al: Relationship Between Inflammation and Radiographic Progression in Patients With Ankylosing Spondylitis Attaining a BASDAI of Less Than 4 During Tumor Necrosis Factor Inhibitor Treatment Sun, et al: Development and Initial Validation of a Systemic Lupus Erythematosus–Specific Measure of the Extent of and Reasons for Medication Nonadherence Patterson, et al: Physical Activity Associates With Lower Systemic Inflammatory Gene Expression in Rheumatoid Arthritis Coleman, et al: Long-Term Follow-up of a Randomized Controlled Trial of Allopurinol Dose Escalation to Achieve Target Serum Urate in People With Gout Smith: Rusty and Wooden Tanomogi, et al: Extravascular Necrotizing Granuloma: A Diagnostic Clue for Eosinophilic Granulomatosis With Polyangiitis Isnardi, et al: Immune Response to SARS-CoV-2 Third Vaccine in Patients With Rheumatoid Arthritis Who Had No Seroconversion After Primary 2-Dose Regimen With Inactivated or Vector-Based Vaccines November 2022 Featured articles: Nelson, et al: Narrative Review of Machine Learning in Rheumatic and Musculoskeletal Diseases for Clinicians and Researchers: Biases, Goals, and Future Directions Hermans, et al: Are All Routine Spondyloarthritis Outpatient Visits Considered Useful by Rheumatologists? An Exploratory Clinical Practice Study Kallas, et al: Trajectory of Damage Accrual in Systemic Lupus Erythematosus Based on Ethnicity and Socioeconomic Factors Nozawa, et al: Early Abnormal Nailfold Capillary Changes Are Predictive of Calcinosis Development in Juvenile Dermatomyositis Chevet, et al: COVID-19 Vaccine Uptake Among Patients With Systemic Lupus Erythematosus in the American Midwest: The Lupus Midwest Network (LUMEN) Remize, et al: Melorheostosis or “Dripping Candle Wax” Bone Disease Bermas: The Unintended Consequence of the Overturn of Roe v Wade: Restrictions on Methotrexate Use October 2022 Featured articles: Hazlewood, et al: Canadian Rheumatology Association Living Guidelines for the Pharmacological Management of Rheumatoid Arthritis With Disease-Modifying Antirheumatic Drugs Schneeberger, et al: Simplified Ankylosing Spondylitis Disease Activity Score (SASDAS) Versus ASDAS: A Post Hoc Analysis of a Randomized Controlled Trial Kasiem, et al: A Practical Guide for Assessment of Skin Burden in Patients With Psoriatic Arthritis Tollisen, et al: Personally Generated Quality of Life Outcomes in Adults With Juvenile Idiopathic Arthritis Glintborg, et al: Long-term Behavioral Changes During the COVID-19 Pandemic and Impact of Vaccination in Patients With Inflammatory Rheumatic Diseases September 2022 Featured articles: Cagnotto, et al: Male Sex Predicts a Favorable Outcome in Early ACPA-Negative Rheumatoid Arthritis: Data From an Observational Study Hazlewood, et al: Frequency of Symptomatic Adverse Events in Rheumatoid Arthritis: An Exploratory Online Survey John M. Davis III: The Patient Experience of Drug Side Effects in Rheumatoid Arthritis: Intriguing Data From an Exploratory Online Survey Venkatachalam, et al: Taking the Long View: Patients Perceive Benefits and Risks of Treatment as Multidimensional Wallace, et al: The Association of Illness-related Uncertainty With Mental Health in Systemic Autoimmune Rheumatic Diseases August 2022 Featured articles: Verweij, et al: Whole-Body Macrophage Positron Emission Tomography Imaging for Disease Activity Assessment in Early Rheumatoid Arthritis Nguyen, et al: Secukinumab in United States Biologic-Naïve Patients With Psoriatic Arthritis: Results From the Randomized, Placebo-Controlled CHOICE Study Le Ralle, et al: Patient Acceptable Symptom State for Burden From Appearance Changes in People With Systemic Sclerosis: A Cross-sectional Survey Baggett, et al: Incidence Rates of Psoriasis in Children With Inflammatory Bowel Disease and Juvenile Arthritis Treated With Tumor Necrosis Factor Inhibitors and Disease-Modifying Antirheumatic Drugs Carluzzo, et al: Patient Empowerment Among Adults With Arthritis: The Case for Emotional Support July 2022 Featured articles: Kelty, et al: Mortality Rates in Patients With Ankylosing Spondylitis With and Without Extraarticular Manifestations and Comorbidities: A Retrospective Cohort Study Mease, et al: Baseline Disease Activity Predicts Achievement of cDAPSA Treatment Targets With Apremilast: Phase III Results in DMARD-naïve Patients With Psoriatic Arthritis Kuwana, et al: Tacrolimus in Patients With Interstitial Pneumonia Associated With Polymyositis or Dermatomyositis: Interim Report of Postmarketing Surveillance in Japan Kiadaliri, et al: Gout and Hospital Admission for Ambulatory Care–Sensitive Conditions: Risks and Trajectories McDermott, et al: Demographic, Lifestyle, and Serologic Risk Factors for Rheumatoid Arthritis (RA)–associated Bronchiectasis: Role of RA-related Autoantibodies June 2022 Featured articles: Darabian, et al: Using FibroScan to Assess for the Development of Liver Fibrosis in Patients With Arthritis on Methotrexate: A Single-center Experience Maguire, et al: Central Obesity in Axial Spondyloarthritis: The Missing Link to Understanding Worse Outcomes in Women? Miloslavsky, et al: The Challenge of Addressing the Rheumatology Workforce Shortage Maheswaranathan, et al: Association of Health Literacy and Numeracy With Lupus Knowledge and the Creation of the Lupus Knowledge Assessment Test Emad, et al: Why Do Patients With Gout Not Take Allopurinol? May 2022 Featured articles: Movahedi, et al: Physician- and Patient-reported Effectiveness Are Similar for Tofacitinib and TNFi in Rheumatoid Arthritis: Data From a Rheumatoid Arthritis Registry El Tal, et al: Consensus Approach to a Treat-to-target Strategy in Juvenile Idiopathic Arthritis Care: Report From the 2020 PR-COIN Consensus Conference Thompson, et al: Modifiable Factors and Incident Gout Across Ethnicity Within a Large Multiethnic Cohort of Older Adults Widdifield, et al: COVID-19 Vaccination Uptake Among Individuals With Immune-mediated Inflammatory Diseases in Ontario, Canada, Between December 2020 and October 2021: A Population-based Analysis Van Praet, et al: Acute Perimyocarditis in a Case of Multisystem Inflammatory Syndrome in Adults Chang, et al: Systemic Lupus Erythematosus Increases the Risk of Gestational Diabetes: Truth or Illusion? McCormick and Choi: Racial Disparities in the Modern Gout Epidemic April 2022 Featured articles: Exarchou, et al: Lifestyle Factors and Disease Activity Over Time in Early Axial Spondyloarthritis: The SPondyloArthritis Caught Early (SPACE) Cohort - https://doi.org/10.3899/jrheum.210046 van Vollenhoven, et al: Efficacy and Safety of Ustekinumab in Patients With Active Systemic Lupus Erythematosus: Results of a Phase II Open-label Extension Study - https://doi.org/10.3899/jrheum.210805 Giancane, et al: Anakinra in Patients With Systemic Juvenile Idiopathic Arthritis: Long-term Safety From the Pharmachild Registry - https://doi.org/10.3899/jrheum.210563 Barber, et al: Best Practices for Virtual Care: A Consensus Statement From the Canadian Rheumatology Association - https://doi.org/10.3899/jrheum.211017 Zickuhr and Mandell: Rheumatology Education Needs a Splash of Color - https://doi.org/10.3899/jrheum.211233 Li, et al: Brain Abscess Due to Nocardia in a Patient With Systemic Lupus Erythematosus- https://doi.org/10.3899/jrheum.210971 March 2022 Featured articles: te Kampe, et al: Outcomes of Care Among Patients With Gout in Europe: A Cross-sectional Survey - https://doi.org/10.3899/jrheum.210009 Stransky, et al: Exploring Family Planning, Parenting, and Sexual and Reproductive Health Care Experiences of Men With Rheumatic Diseases - https://doi.org/10.3899/jrheum.210785 Beckers, et al: Performance of 3 Composite Measures for Disease Activity in Peripheral Spondyloarthritis - https://doi.org/10.3899/jrheum.210075 Sun, et al: Long-term Risk of Heart Failure and Other Adverse Cardiovascular Outcomes in Granulomatosis With Polyangiitis: A Nationwide Cohort Study - https://doi.org/10.3899/jrheum.210677 Curtis, et al: Characteristics, Comorbidities, and Outcomes of SARS-CoV-2 Infection in Patients With Autoimmune Conditions Treated With Systemic Therapies: A Population-based Study - https://doi.org/10.3899/jrheum.210888 Gunasuntharam: Why Should It Be Different From the Other Side? A Parent and Pediatrician’s Perspective of a Child With Kawasaki Disease - https://doi.org/10.3899/jrheum.211159 Lazarou, et al: Adult-onset Acute Calcific Discitis - https://doi.org/10.3899/jrheum.210838 Khanna: Remission in Gout: Concepts From a Patient Perspective - https://doi.org/10.3899/jrheum.211285 Coates and Tillett: How Should We Measure Peripheral Spondyloarthritis? - https://doi.org/10.3899/jrheum.211043 February 2022 Featured articles: Rosenbaum, et al: The Interplay Between COVID-19 and Spondyloarthritis or Its Treatment - https://doi.org/10.3899/jrheum.210742 van der Heijde, et al: Radiographic Progression of Structural Joint Damage Over 5 Years of Baricitinib Treatment in Patients With Rheumatoid Arthritis: Results From RA-BEYOND - https://doi.org/10.3899/jrheum.210346 van der Meer, et al: Extraskeletal Manifestations in Axial Spondyloarthritis Are Associated With Worse Clinical Outcomes Despite the Use of Tumor Necrosis Factor Inhibitor Therapy - https://doi.org/10.3899/jrheum.210308 Haddad, et al: The Association of Psoriatic Arthritis With All-cause Mortality and Leading Causes of Death in Psoriatic Arthritis - https://doi.org/10.3899/jrheum.210159 Yazdanyar, et al: Risk of 30-day Readmission After Knee or Hip Replacement in Rheumatoid Arthritis and Osteoarthritis by Non-Medicare and Medicare Payer Status - https://doi.org/10.3899/jrheum.201370 Perez Acosta et al: Cystic Ganglionosis in a 3-year-old Mimicking Juvenile Idiopathic Arthritis - https://doi.org/10.3899/jrheum.210558 Leung: Is Psoriatic Arthritis Associated With Higher Risk of Mortality? - https://doi.org/10.3899/jrheum.210963 January 2022 Featured articles: Bermas, et al: COVID-19 in Pregnant Women With Rheumatic Disease: Data From the COVID-19 Global Rheumatology Alliance - https://doi.org/10.3899/jrheum.210480 Hazlewood, et al: Heterogeneity in Patient Characteristics and Differences in Treatment Across 4 Canadian Rheumatoid Arthritis Cohorts - https://doi.org/10.3899/jrheum.201688 Panopoulos, et al: Anti-interleukin 6 Therapy Effect for Refractory Joint and Skin Involvement in Systemic Sclerosis: A Real-world, Single-center Experience - https://doi.org/10.3899/jrheum.210273 Lieber, et al: Evaluation of a Patient-reported Frailty Tool in Women With Systemic Lupus Erythematosus - https://doi.org/10.3899/jrheum.201466 Philpott, et al: Synovitis Is Associated With Constant Pain in Knee Osteoarthritis: A Cross-sectional Study of OMERACT Knee Ultrasound Scores - https://doi.org/10.3899/jrheum.210285 Fernandes, et al: Tuberculosis Presenting as an Inflammatory Pseudotumor of the Sciatic Nerve in a Rheumatoid Arthritis Patient Taking Etanercept - https://doi.org/10.3899/jrheum.210540 Sammaritano: The Effect of COVID-19 Illness on Pregnant Patients With Rheumatic Disease: Early Reassuring Data - https://doi.org/10.3899/jrheum.211050 December 2021 Featured articles: Kremer, et al: The Clinical Disease Activity Index and the Routine Assessment of Patient Index Data 3 for Achievement of Treatment Strategies - https://doi.org/10.3899/jrheum.200692 Müskens, et al: Does Etanercept Biosimilar Prescription in a Rheumatology Center Bend the Medication Cost Curve? - https://doi.org/10.3899/jrheum.200565 Gladman, et al: Oligoarticular vs Polyarticular Psoriatic Arthritis: A Longitudinal Study Showing Similar Characteristics - https://doi.org/10.3899/jrheum.210434 Showalter, et al: Esophageal Dilation and Other Clinical Factors Associated With Pulmonary Function Decline in Patients With Systemic Sclerosis - https://doi.org/10.3899/jrheum.210533 Holyer, et al: What Represents Treatment Efficacy in Long-term Studies of Gout Flare Prevention? An Interview Study of People With Gout - https://doi.org/10.3899/jrheum.210476 Tam et al: My Hips Hurt: An Unusual Presentation of Bilateral Groin Pain in an Adolescent Boy - https://doi.org/10.3899/jrheum.210362 Ferreira, et al: Definition of Treatment Targets in Rheumatoid Arthritis: Is It Time for Reappraisal? - https://doi.org/10.3899/jrheum.210050 Jacobs, et al: Unravelling the Cost of Biological Strategies in Rheumatoid Arthritis: A Kaleidoscope of Methodologies, Interpretations, and Interests - https://doi.org/10.3899/jrheum.201510 November 2021 Featured articles: Colantonio, et al: Higher Serum Urate Levels Are Associated With an Increased Risk for Sudden Cardiac Death - https://doi.org/10.3899/jrheum.210139 Ochi, et al: Similarity of Response to Biologics Between Elderly-onset Rheumatoid Arthritis (EORA) and Non-EORA Elderly Patients: From the FIRST Registry - https://doi.org/10.3899/jrheum.201135 Tanaka, et al: Effects of Denosumab in Japanese Patients With Rheumatoid Arthritis Treated With Conventional Antirheumatic Drugs: 36-month Extension of a Phase III Study - https://doi.org/10.3899/jrheum.201376 Ye, et al: Measuring Physical Function in Psoriatic Arthritis: Comparing the Multidimensional Health Assessment Questionnaire to the Health Assessment Questionnaire–Disability Index - https://doi.org/10.3899/jrheum.200927 Concha, et al: Changes in Treatments and Outcomes After Implementation of a National Universal Access Program for Juvenile Idiopathic Arthritis - https://doi.org/10.3899/jrheum.210011 Meara, et al: A Case of Chilblains-like Lesions Post SARS-CoV-2 Vaccine? - https://doi.org/10.3899/jrheum.210226 Liu: Serum Uric Acid: A Murderer or Bystander for Cardiac-related Mortality? - https://doi.org/10.3899/jrheum.210695 Berard and Batthish: Addressing Healthcare Quality in Juvenile Idiopathic Arthritis With a Universal Access Program - https://doi.org/10.3899/jrheum.210658 October 2021 Featured articles: Safy-Khan, et al: Current Smoking Negatively Affects the Response to Methotrexate in Rheumatoid Arthritis in a Dose-responsive Way, Independently of Concomitant Prednisone Use - https://doi.org/10.3899/jrheum.200213 Mease, et al: Comparison of Men and Women With Axial Spondyloarthritis in the US-based Corrona Psoriatic Arthritis/Spondyloarthritis Registry - https://doi.org/10.3899/jrheum.201549 Feher, et al: Impaired Myocardial Flow Reserve on 82Rubidium Positron Emission Tomography/Computed Tomography in Patients With Systemic Sclerosis - https://doi.org/10.3899/jrheum.210040 Mohajer, et al: Metabolic Syndrome and Osteoarthritis Distribution in the Hand Joints: A Propensity Score Matching Analysis From the Osteoarthritis Initiative - https://doi.org/10.3899/jrheum.210189 Fernández-Ávila, et al: Impact of COVID-19 Pandemic on Rheumatology Practice in Latin America - https://doi.org/10.3899/jrheum.201623https://doi.org/10.3899/jrheum.201623 Gilvaz et al: A Case of Disseminated Cutaneous Mycobacterium chelonae Infection During Treatment With Tofacitinib - https://doi.org/10.3899/jrheum.200730 Jansen, et al: Smoking and Methotrexate Inefficacy in Rheumatoid Arthritis: What About Underlying Molecular Mechanisms? - https://doi.org/10.3899/jrheum.210217 Leung: Gender Differences in Disease Activity and Impact in Axial Spondyloarthritis - https://doi.org/10.3899/jrheum.210564 September 2021 Featured articles: Myasoedova, et al: Improved Incidence of Cardiovascular Disease in Patients With Incident Rheumatoid Arthritis in the 2000s: A Population-based Cohort Study - https://doi.org/10.3899/jrheum.200842 Karmacharya, et al: Diagnostic Delay in Psoriatic Arthritis: A Population-based Study - https://doi.org/10.3899/jrheum.201199 Clément, et al: Real-world Risk of Relapse of Giant Cell Arteritis Treated With Tocilizumab: A Retrospective Analysis of 43 Patients - https://doi.org/10.3899/jrheum.200595 Master, et al: Joint Association of Moderate-to-vigorous Intensity Physical Activity and Sedentary Behavior With Incident Functional Limitation: Data From the Osteoarthritis Initiative - https://doi.org/10.3899/jrheum.201250 Sheth et al: Improving Pneumococcal Vaccination Rates in Rheumatology Patients by Using Best Practice Alerts in the Electronic Health Records - https://doi.org/10.3899/jrheum.200806 Bathon: Is the Gap in Incidence of Cardiovascular Events in Rheumatoid Arthritis Really Closing? - https://doi.org/10.3899/jrheum.210366 Villiger: Giant Cell Arteritis: Real-life Experience - https://doi.org/10.3899/jrheum.210334 Gazitt, et al: Spinal Stenosis Caused by Calcinosis in a Patient With Systemic Sclerosis - https://doi.org/10.3899/jrheum.201389 De Boer and Goekoop: Posttraumatic Chylous Knee Effusion - https://doi.org/10.3899/jrheum.191050 August 2021 Featured articles: Vu, et al: Impact of Comorbid Conditions on Healthcare Expenditure and Work-related Outcomes in Patients With Rheumatoid Arthritis - https://doi.org/10.3899/jrheum.200231 Taylor, et al: A Phase III Randomized Study of Apremilast, an Oral Phosphodiesterase 4 Inhibitor, for Active Ankylosing Spondylitis - https://doi.org/10.3899/jrheum.201088 Falasinnu, et al: The Problem of Pain in Systemic Lupus Erythematosus: An Explication of the Role of Biopsychosocial Mechanisms - https://doi.org/10.3899/jrheum.200595 Hazlewood, et al: Canadian Rheumatology Association Recommendation for the Use of COVID-19 Vaccination for Patients With Autoimmune Rheumatic Diseases - https://doi.org/10.3899/jrheum.210288 Aljaberi et al: Maintaining Hepatitis B Protection in Immunocompromised Pediatric Rheumatology and Inflammatory Bowel Disease Patients - https://doi.org/10.3899/jrheum.200283 Bechman, et al: The COVID-19 Vaccine Landscape: What a Rheumatologist Needs to Know - https://doi.org/10.3899/jrheum.210106 Rahman: Why Do Patients With Systemic Lupus Erythematosus Suffer Pain? - https://doi.org/10.3899/jrheum.210057 Awqati, et al: Ulcerative Paraneoplastic Dermatomyositis in the Setting of Positive Transcriptional Intermediary Factor 1-γ Antibody - https://doi.org/10.3899/jrheum.200399 Shinoda, et al: Widespread Mechanic’s Hands in Antisynthetase Syndrome With Anti-OJ Antibody - https://doi.org/10.3899/jrheum.201043 July 2021 Featured articles: Pathi, et al: The Rheumatoid Arthritis Gene Expression Signature Among Women Who Improve or Worsen During Pregnancy: A Pilot Study - https://doi.org/10.3899/jrheum.201128 Stovall, et al: Relation of NSAIDs, DMARDs, and TNF Inhibitors for Ankylosing Spondylitis and Psoriatic Arthritis to Risk of Total Hip and Knee Arthroplasty - https://doi.org/10.3899/jrheum.200453 Mehta, et al: Giant Cell Arteritis and COVID-19: Similarities and Discriminators. A Systematic Literature Review - https://doi.org/10.3899/jrheum.200766 Widdifield, et al: Feminization of the Rheumatology Workforce: A Longitudinal Evaluation of Patient Volumes, Practice Sizes, and Physician Remuneration - https://doi.org/10.3899/jrheum.201166 Bachiller-Corral et al: Risk of Severe COVID-19 Infection in Patients With Inflammatory Rheumatic Diseases - https://doi.org/10.3899/jrheum.200755 Ornetti, et al: Perforating Rheumatoid Nodule Mimicking Malignant Soft-tissue Mass of the Forearm - https://doi.org/10.3899/jrheum.201290 Guillaune-Czitrom, et al: A Recurrent Central Band Keratopathy in a Child - https://doi.org/10.3899/jrheum.200462 June 2021 Featured articles: Xie, et al: Benefits of Methotrexate Use on Cardiovascular Disease Risk Among Rheumatoid Arthritis Patients Initiating Biologic Disease-modifying Antirheumatic Drugs - https://doi.org/10.3899/jrheum.191326 Jørgensen, et al: Relation Between Fatigue and ACR Response in Patients With Psoriatic Arthritis Treated With Tumor Necrosis Factor Inhibitor Therapy: A Population-based Cohort Study - https://doi.org/10.3899/jrheum.191107 Dominguez, et al: Relationship Between Genetic Risk and Age of Diagnosis in Systemic Lupus Erythematosus - https://doi.org/10.3899/jrheum.200002 Coffey, et al: Hospitalization Rates Are Highest in the First 5 Years of Systemic Sclerosis: Results From a Population-based Cohort (1980–2016) - https://doi.org/10.3899/jrheum.200737 Singh and Cleveland: Hospitalized Infections in People With Osteoarthritis: A National US Study - https://doi.org/10.3899/jrheum.191383 May 2021 Featured articles: Ozen, et al: The Risk of Cardiovascular Events Associated With Disease-modifying Antirheumatic Drugs in Rheumatoid Arthritis - doi.org/10.3899/jrheum.200265 Ogdie, et al: Descriptive Comparisons of the Effect of Apremilast and Methotrexate Monotherapy in Oligoarticular Psoriatic Arthritis: The Corrona Psoriatic Arthritis/Spondyloarthritis Registry Results - doi.org/10.3899/jrheum.191209 Kim, et al: Lupus Low Disease Activity State Achievement Is Important for Reducing Adverse Outcomes in Pregnant Patients With Systemic Lupus Erythematosus - doi.org/10.3899/jrheum.200802 Mossel, et al: Clinical Phenotyping of Primary Sjögren Syndrome Patients Using Salivary Gland Ultrasonography: Data From the RESULT Cohort - doi.org/10.3899/jrheum.200482 Panwar et al: Whole-body MRI Quantification for Assessment of Bone Lesions in Chronic Nonbacterial Osteomyelitis Patients Treated With Pamidronate: A Prevalence, Reproducibility, and Responsiveness Study - doi.org/10.3899/jrheum.200329 April 2021 Featured articles: Barber, et al: Evaluating Quality of Care for Rheumatoid Arthritis for the Population of Alberta Using System-level Performance Measures - doi.org/10.3899/jrheum.200420 Liu, et al: Physical Activity and Attitudes Toward Exercise in People With Axial and Peripheral Spondyloarthritis - doi.org/10.3899/jrheum.200354 Harkey, et al: A Decline in Walking Speed Is Associated With Incident Knee Replacement in Adults With and at Risk for Knee Osteoarthritis - doi.org/10.3899/jrheum.200176 Mendel, et al: CanVasc Consensus Recommendations for the Management of Antineutrophil Cytoplasm Antibody-associated Vasculitis: 2020 Update - doi.org/10.3899/jrheum.200721 Gkrouzman, et al: Antiphospholipid Antibody Profile Stability Over Time: Prospective Results From the APS ACTION Clinical Database and Repository - doi.org/10.3899/jrheum.200513 March 2021 Featured articles: Almaghlouth, et al: Propensity Score Methods in Rare Disease: A Demonstration Using Observational Data in Systemic Lupus Erythematosus - doi.org/10.3899/jrheum.200254 Faye, et al: Risk of Adverse Outcomes in Hospitalized Patients With Autoimmune Disease and COVID-19: A Matched Cohort Study From New York City - doi.org/10.3899/jrheum.200989 Grosse, et al: Evaluation of Bone Erosions in Rheumatoid Arthritis: The Ultrasound Score for Erosions Versus the Modified Sharp/van der Heijde Score for Erosions - doi.org/10.3899/jrheum.200286 Liew, et al: Cardiovascular Risk Scores in Axial Spondyloarthritis Versus the General Population: A Cross-sectional Study - doi.org/10.3899/jrheum.200188 van Leeuwen, et al: Association Between Centromere- and Topoisomerase-specific Immune Responses and the Degree of Microangiopathy in Systemic Sclerosis - doi.org/10.3899/jrheum.191331 February 2021 Featured articles: Kiltz, et al: Ixekizumab Improves Functioning and Health in the Treatment of Radiographic Axial Spondyloarthritis: Week 52 Results from 2 Pivotal Studies - doi.org/10.3899/jrheum.200093 Sarabia, et al: The Pattern of Musculoskeletal Complaints in Patients With Suspected Psoriatic Arthritis and Their Correlation With Physical Examination and Ultrasound - doi.org/10.3899/jrheum.190857 te Kampe, et al: Sex Differences in the Clinical Profile Among Patients With Gout: Cross-sectional Analyses of an Observational Study - doi.org/10.3899/jrheum.200113 Walscheid, et al: Enthesitis-related Arthritis: Prevalence and Complications of Associated Uveitis in Children and Adolescents From a Population-based Nationwide Study in Germany - doi.org/10.3899/jrheum.191085 Master, et al: Does the 1-year Decline in Walking Speed Predict Mortality Risk Beyond Current Walking Speed in Adults With Knee Osteoarthritis? - doi.org/10.3899/jrheum.200259 January 2021 Featured articles: Fisher, et al: Tofacitinib Persistence in Patients with Rheumatoid Arthritis: A Retrospective Cohort Study - doi.org/10.3899/jrheum.191252 Thomas, et al: Tumor Necrosis Factor Inhibitor Monotherapy Versus Combination Therapy for the Treatment of Psoriatic Arthritis: Combined Analysis of European Biologics Databases - doi.org/10.3899/jrheum.190815 Blaja, et al: The Challenge of Very Early Systemic Sclerosis: A Combination of Mild and Early Disease? - doi.org/10.3899/jrheum.190976 Zhai, et al: Phenylalanine Is a Novel Marker for Radiographic Knee Osteoarthritis Progression: The MOST Study - doi.org/10.3899/jrheum.200054 Koppikar, et al: Improving Hydroxychloroquine Dosing and Toxicity Screening at a Tertiary Care Ambulatory Center: A Quality Improvement Initiative - doi.org/10.3899/jrheum.191265 December 2020 Featured articles: Foers, et al: Circulating Small Noncoding RNA Biomarkers of Response to Triple Disease-modifying Antirheumatic Drug Therapy in White Women With Early Rheumatoid Arthritis - doi.org/10.3899/jrheum.191012 Wade, et al: Serum MicroRNA Signature as a Diagnostic and Therapeutic Marker in Patients with Psoriatic Arthritis - doi.org/10.3899/jrheum.190602 Schwartz, et al: Utility of the Brief Illness Perception Questionnaire to Monitor Patient Beliefs in Systemic Vasculitis - doi.org/10.3899/jrheum.190828 Correll, et al: Identifying Research Priorities among Patients and Families of Children with Rheumatic Diseases Living in the United States - doi.org/10.3899/jrheum.190934 Bitar, et al: Five-year Evolution Patterns of Physical Activity and Sedentary Behavior in Patients with Lower-limb Osteoarthritis and Their Sociodemographic and Clinical Correlates - doi.org/10.3899/jrheum.190854 November 2020 Featured articles: Cañete, et al: Expert Consensus on a Set of Outcomes to Assess the Effectiveness of Biologic Treatment in Psoriatic Arthritis: The MERECES Study - doi.org/10.3899/jrheum.191056 Aguirre, et al: Using Process Improvement and Systems Redesign to Improve Rheumatology Care Quality in a Safety Net Clinic - doi.org/10.3899/jrheum.190472 Stern, et al: Analysis of Anti-RNA Polymerase III Antibody-positive Systemic Sclerosis and Altered GPATCH2L and CTNND2 Expression in Scleroderma Renal Crisis - doi.org/10.3899/jrheum.190945 Langlois, et al: Rituximab and Cyclophosphamide in Antisynthetase Syndrome–related Interstitial Lung Disease: An Observational Retrospective Study - doi.org/10.3899/jrheum.190505 Moore, et al: Role of Neutrophil Extracellular Traps Regarding Patients at Risk of Increased Disease Activity and Cardiovascular Comorbidity in Systemic Lupus Erythematosus - doi.org/10.3899/jrheum.190875 October 2020 Featured articles: Pappas, et al: Effectiveness of Tocilizumab in Patients with Rheumatoid Arthritis Is Unaffected by Comorbidity Burden or Obesity: Data from a US Registry - doi.org/10.3899/jrheum.190282 van Bentum, et al: The Ankylosing Spondylitis Performance Index: Reliability and Feasibility of an Objective Test for Physical Functioning - doi.org/10.3899/jrheum.191063 Walsh, et al: Measuring Outcomes in Psoriatic Arthritis: Comparing Routine Assessment of Patient Index Data and Psoriatic Arthritis Impact of Disease - doi.org/10.3899/jrheum.190219 Liang, et al: Hemophagocytic Lymphohistiocytosis: Prevalence, Risk Factors, Outcome, and Outcome-related Factors in Adult Idiopathic Inflammatory Myopathies - doi.org/10.3899/jrheum.190542 Kelly, et al: Scope of Outcomes in Trials and Observational Studies of Interventions Targeting Medication Adherence in Rheumatic Conditions: A Systematic Review - doi.org/10.3899/jrheum.190726 September 2020 Featured articles: Kuettel, et al: Pain and Self-reported Swollen Joints Are Main Drivers of Patient-reported Flares in Rheumatoid Arthritis: Results from a 12-month Observational Study - doi.org/10.3899/jrheum.190760 Ben-Shabat, et al: Mortality among Patients with Giant Cell Arteritis: A Large-scale Population-based Cohort Study - doi.org/10.3899/jrheum.190927 Tselios, et al: Advanced Chronic Kidney Disease in Lupus Nephritis: Is Dialysis Inevitable? - doi.org/10.3899/jrheum.191064 Putman, et al: The Quality of Randomized Controlled Trials in High-impact Rheumatology Journals, 1998–2018 - doi.org/10.3899/jrheum.191306 Loef, et al: Health-related Quality of Life in Patients with Hand Osteoarthritis from the General Population and the Outpatient Clinic - doi.org/10.3899/jrheum.190781 July 2020 Featured articles: Harrold, et al: Longterm, Real-world Safety of Adalimumab in Rheumatoid Arthritis: Analysis of a Prospective US-based Registry - doi.org/10.3899/jrheum.190260 Bakewell,et al: Imaging Techniques: Options for the Diagnosis and Monitoring of Treatment of Enthesitis in Psoriatic Arthritis - doi.org/10.3899/jrheum.190512 Hoge, et al: Association of Poverty Income Ratio with Physical Functioning in a Cohort of Patients with Systemic Lupus Erythematosus - doi.org/10.3899/jrheum.190991 Dai, et al: Sleep Quality Is Related to Worsening Knee Pain in Those with Widespread Pain: The Multicenter Osteoarthritis Study - doi.org/10.3899/jrheum.181365 Aydin, etla: The Relationship Between Physical Examination and Ultrasonography of Large Entheses of the Achilles Tendon and Patellar Tendon Origin - doi.org/10.3899/jrheum.190169 back to top June 2020 Featured articles: Sepriano, et al: Adherence to Treat-to-target Management in Rheumatoid Arthritis and Associated Factors: Data from the International RA BIODAM Cohort - doi.org/10.3899/jrheum.190303 Zardin-Moraes, et al: Prevalence of Psoriatic Arthritis Patients Achieving Minimal Disease Activity in Real-world Studies and Randomized Clinical Trials: Systematic Review with Metaanalysis - doi.org/10.3899/jrheum.190677 Desbois, et al: Rituximab-associated Vasculitis Flare: Incidence, Predictors, and Outcome - doi.org/10.3899/jrheum.190076 Bollhalder, et al: Magnetic Resonance Imaging Followup of Temporomandibular Joint Inflammation, Deformation, and Mandibular Growth in Juvenile Idiopathic Arthritis Patients Receiving Systemic Treatment - doi.org/10.3899/jrheum.190168 Colaco, et al: Predictive Utility of Cardiovascular Risk Prediction Algorithms in Inflammatory Rheumatic Diseases: A Systematic Review - doi.org/10.3899/jrheum.190261 May 2020 Featured articles: Skougaard, et al: ELECTOR: eHealth in rheumatology - doi.org/10.3899/jrheum.181362 Lee, et al: Cesarean births in AS - doi.org/10.3899/jrheum.190754 Quinn, et al: Exercise echocardiography in SSc - doi.org/10.3899/jrheum.190226 Gibson, et al: FM assessment screenting tool - doi.org/10.3899/jrheum.190277 Qendro, et al: Immunization in rheumatic diseases - doi.org/10.3899/jrheum.181376 April 2020 Featured articles: Keystone, et al: Primary/secondary nonresponse to anti-TNF - doi.org/10.3899/jrheum.190102 Singh and Cleveland: Insurance, income, and TSA outcomes - doi.org/10.3899/jrheum.190287 Mukwikwi, et al: SLE retinal complications - doi.org/10.3899/jrheum.181102 Rosato, et al: SSc renal parenchymal thickness - doi.org/10.3899/jrheum.190165 Elfishawi, et al: Changes in incident gout - doi.org/10.3899/jrheum.190346 Cron and Chatham: The Rheumatologist’s Role in COVID-19 - doi.org/10.3899/jrheum.200334 Peschken: Possible Consequences of a Shortage of Hydroxychloroquine for Lupus Patients Amid the COVID-19 Pandemic - doi.org/10.3899/jrheum.200395 Putman and Ruderman: Learning from Adversity: Lessons from the COVID-19 Crisis - doi.org/10.3899/jrheum.200411 March 2020 Featured articles: Agca, et al: CV risk in RA - doi.org/10.3899/jrheum.180726 Perruccio, et al: PASDAS and MDA in PsA - doi.org/10.3899/jrheum.181472 Bruschi, et al: NET in SLE/lupus nephritis - doi.org/10.3899/jrheum.181232 Cook, et al: Statins and revision arthroplasty - doi.org/10.3899/jrheum.180574 Singh, et al: Effectiveness of allopurinol in gout - doi.org/10.3899/jrheum.190522 February 2020 Featured articles: Jamal, et al: Adverse events and cancer immunotherapy - doi.org/10.3899/jrheum.190084 Ormseth, et al: Plasma miRNA RA panel - doi.org/10.3899/jrheum.181029 Rostami, et al: AS risk prediction - doi.org/10.3899/jrheum.181209 de Vries-Bouwstra, et al: Recommendation agreement in SSc - doi.org/10.3899/jrheum.181173 Bowes, et al: Automated cartilage segmentation - doi.org/10.3899/jrheum.180541 back to top January 2020 Featured articles: Bechman, et al: Placebo response in RA - doi.org/10.3899/jrheum.190008 Yusuf: Editorial - doi.org/10.3899/jrheum.190900 Walsh, et al: axSpA identification methods - doi.org/10.3899/jrheum.181005 Urowitz, et al: AVE in SLE in decades - doi.org/10.3899/jrheum.180986 Ying, et al: VA SSc stroke risk - doi.org/10.3899/jrheum.181311 Mills, et al: Rheumatic diseases and pregnancy - doi.org/10.3899/jrheum.181067 Author Interviews Q & A: Catherine Bakewell, MD, Sibel Zehra Aydin, MD, Lihi Eder, MD, PhD, and Gurjit S. Kaeley, MBBS, MRCP, RhMSUS Editor-in-Chief Dr. Earl Silverman speaks with Dr. Catherine Bakewell from the Intermountain Healthcare Medical Group Salt Lake Clinic, Dr. Sibel Zehra Aydin from the University of Ottawa, Dr. Lihi Eder at the Women’s College Hospital, and Dr. Gurjit S. Kaeley from the University of Florida about their and their co-authors' review article "Imaging Techniques: Options for the Diagnosis and Monitoring of Treatment of Enthesitis in Psoriatic Arthritis". For the full article: Imaging Techniques: Options for the Diagnosis and Monitoring of Treatment of Enthesitis in Psoriatic Arthritis by Catherine Bakewell, Sibel Zehra Aydin, Veena K. Ranganath, Lihi Eder and Gurjit S. Kaeley. [Read the full transcript.] For the video interview: Viewing Rheum Q & A: Daniel K. White, PT, ScD, MSc Editor-in-Chief Dr. Earl Silverman speaks with Dr. Daniel K. White from the University of Delaware about his and his co-authors' editorial "Walk At Least 10 Minutes a Day for Adults With Knee Osteoarthritis: Recommendation for Minimal Activity During the COVID-19 Pandemic". For the full article: Walk At Least 10 Minutes a Day for Adults With Knee Osteoarthritis: Recommendation for Minimal Activity During the COVID-19 Pandemic by Jason T. Jakiela, Esther J. Waugh, and Daniel K. White. [Read the full transcript.] For the video interview: Viewing Rheum Q & A: Dr. Roberto Caricchio, MD Editor-in-Chief Dr. Earl Silverman speaks with Dr. Roberto Caricchio from Lewis Katz School of Medicine, Temple University about his and his co-author's letter Rheumatologists and Pulmonologists at Temple University Weather the COVID-19 Storm Together. For the full article: Rheumatologists and Pulmonologists at Temple University Weather the COVID-19 Storm Together by Roberto Caricchio and Gerard J. Criner. [Read the full transcript.] For the video interview: Viewing Rheum Q & A: Drs. Michael S. Putman, MD, and Eric M. Ruderman, MD Editor-in-Chief Dr. Earl Silverman speaks with Drs. Michael S. Putman and Eric M. Ruderman from Northwestern University about their editorial Learning from Adversity: Lessons from the COVID-19 Crisis. For the full article: Learning from Adversity: Lessons from the COVID-19 Crisis by Michael S. Putman and Eric M. Ruderman. [Read the full transcript.] For the video interview: Viewing Rheum Q & A: Drs. Rosie Scuccimarri, MD, Evelyn Sutton, MD, and Mary-Ann Fitzcharles, MB, ChB Editor-in-Chief Dr. Earl Silverman speaks with Drs. Rosie Scuccimarri from McGill University, Evelyn Sutton from Dalhousie University, and Mary-Ann Fitzcharles from McGill University about their editorial Hydroxychloroquine: A Potential Ethical Dilemma for Rheumatologists during the COVID-19 Pandemic. For the full article: Hydroxychloroquine: A Potential Ethical Dilemma for Rheumatologists during the COVID-19 Pandemic by Rosie Scuccimarri, Evelyn Sutton, and Mary-Ann Fitzcharles. [Read the full transcript.] For the video interview: Viewing Rheum back to top Audio Abstracts Dr. James T. Rosenbaum For the full article: The Effect of HLA-B27 on Susceptibility and Severity of Covid-19 by James T. Rosenbaum, Hedley Hamilton, Michael H. Weisman, John D. Reveille, Kevin L. Winthrop, and Dongseok Choi. [Read the full transcript.] Dr. Niv Ben-Shabat, BMSc For the full article: Mortality among Patients with Giant Cell Arteritis: A Large-scale Population-based Cohort Study by Niv Ben-Shabat, Shmuel Tiosano, Ora Shovman, Doron Comaneshter, Yehuda Shoenfeld, Arnon D. Cohen and Howard Amital Dr. Gisele Vajgel, MD For the full article: Effect of a Single Apolipoprotein L1 Gene Nephropathy Variant on the Risk of Advanced Lupus Nephritis in Brazilians by Gisele Vajgel, Suelen Cristina Lima, Diego Jeronimo S. Santana, Camila B.L. Oliveira, Denise Maria N. Costa, Pamela J. Hicks, Maria Alina G.M. Cavalcante, Carl D. Langefeld, Lucila Maria Valente, Sergio Crovella, Gianna Mastroianni Kirsztajn, Barry I. Freedman and Paula Sandrin-Garcia Dr. Paula Muilu, MD For the full article: Opioid Use among Patients with Early Inflammatory Arthritides Compared to the General Population by Paula Muilu, Vappu Rantalaiho, Hannu Kautiainen, Lauri Juhani Virta and Kari Puolakka. [Read the full transcript.] Dr. Marie Skougaard, MD For the full article: Patients with Rheumatoid Arthritis Acquire Sustainable Skills for Home Monitoring: A Prospective Dual-country Cohort Study (ELECTOR Clinical Trial I) by Marie Skougaard, Henning Bliddal, Robin Christensen, Karen Ellegaard, Sabrina M. Nielsen, Jakub Zavada, Sabina Oreska, Niels S. Krogh, Christian C. Holm, Merete L. Hetland, Jiri Vencovsky, Henrik Røgind, Peter C. Taylor and Henrik Gudbergsen. [Read the full transcript.] back to top Techniques Dr. Edward C. Keystone, MD, FRCP(C) For the full article: The Dorsal 4-finger Technique: A Novel Method to Examine Metacarpophalangeal Joints in Patients with Rheumatoid Arthritis by Mohammed A. Omair, Pooneh Akhavan, Ali Naraghi, Shikha Mittoo, Juan Xiong, Deborah Weber, Daming Lin, Melissa Weber, and Edward C. Keystone. [Read the full transcript.] back to top Contents Author Interviews Audio Abstracts Techniques Editor's Picks Archives Author Interviews Audio Abstracts Editor's Picks 2019 Editor's Picks 2018

|
Scooped by
Gilbert C FAURE
February 17, 2023 3:25 AM
|
article: Overview of Cochrane Systematic Reviews of rehabilitation interventions for persons with rheumatoid arthritis: a mapping synthesis - European Journal of Physical and Rehabilitation Medicine 2023 Feb 02 - Minerva Medica - Journals...

|
Scooped by
Gilbert C FAURE
August 28, 2022 6:55 AM
|
This week's NEJM has published the efficacy results of a large phase 3 trial of olokizumab, a humanized monoclonal antibody that directly targets IL-6 in patients with rheumatoid arthritis.
This is in contrast to two other marketed IL-6 inhibitors (sarilumab, tocilizumab) that bind to the IL-6 receptor.

|
Scooped by
Gilbert C FAURE
February 21, 2022 4:53 AM
|
Rheumatoid arthritis (RA) is a multifactorial autoimmune disease characterized by chronic inflammation and destruction of multiple small joints which may lead to systemic complications. Altered immunity via pathogenic autoantibodies pre-date clinical symptom development by several years. Incompletely understood range of mechanisms trigger joint-homing, leading to clinically evident articular disease. Advances in therapeutic approaches and understanding pathogenesis have improved prognosis and likely remission. However, partial/non-response to conventional and biologic therapies witnessed in a subset of patients highlights the need for new therapeutics. It is now evident that joint disease chronicity stems from recalcitrant inflammatory synovial environment, majorly maintained by epigenetically and metabolically reprogrammed synoviocytes. Therefore, interference with effector functions of activated cell types seems a rational strategy to reinstate synovial homeostasis and complement existing anti-inflammatory interventions to mitigate chronic RA. Presenting this newer aspect of fibroblast-like synoviocytes and myeloid cells underlying the altered synovial biology in RA and its potential for identification of new druggable targets is attempted in this review. Major leads from i) molecular insights of pathogenic cell types from hypothesis free OMICS approaches; ii) hierarchy of their dysregulated signaling pathways; and iii) knowledge of druggability of molecular nodes i

|
Scooped by
Gilbert C FAURE
January 21, 2022 4:46 AM
|
Abstract. B cell dysfunction and inflammatory cytokine over-production participate in the pathogenesis of rheumatoid arthritis (RA). Here we compared peripheral

|
Scooped by
Gilbert C FAURE
October 13, 2021 11:30 AM
|
The aim of this 18-month retrospective study was to evaluate the differences in outcomes of denosumab with tumor necrosis factor (TNF) inhibitors (TNFis), tocilizumab (TCZ), or abatacept (ABT) treatment in osteoporosis (OP) patients with rheumatoid arthritis ...

|
Scooped by
Gilbert C FAURE
October 12, 2021 5:48 AM
|
To mark Rheumatoid Arthritis Awareness Week 2020, Clinical & Experimental Immunology presents a new virtual issue highlighting some of the cutting edge research and reviews covering all aspects of rheumatoid arthritis.

|
Scooped by
Gilbert C FAURE
October 4, 2021 1:25 PM
|
Researchers at The University of Toledo have developed an experimental vaccine that shows significant promise in preventing rheumatoid arthritis, a painful autoimmune disease that cannot currently be cured.
|

|
Scooped by
Gilbert C FAURE
October 9, 2025 5:57 AM
|
📢 NEW REVIEW
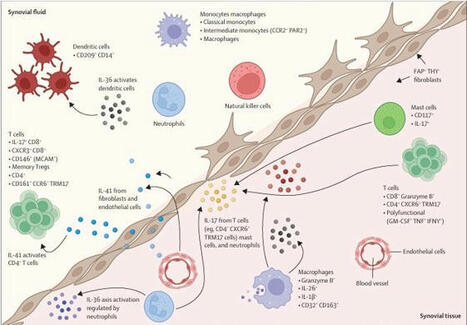
Although psoriatic arthritis and rheumatoid arthritis are both common types of inflammatory arthritis characterised by synovial inflammation, there are distinct molecular and cellular landscapes between these conditions.
In this Review, Ryan Malcolm Hum and colleagues explore how research of the synovium has advanced the understanding of psoriatic arthritis, the potential of identified cell types and cytokines as biomarkers and novel therapeutic targets, how limited sample sizes in high-dimensional studies are hindering clinical translation, and the future directions for synovial research in psoriatic arthritis.
Maria Christofi, Lysette Marshall, NIHR Manchester Biomedical Research Centre (BRC)
Read the full Review here ➡️ https://lnkd.in/eFY6uAbF
Alt text: Previously identified cell types and cytokines implicated in psoriatic arthritis pathogenesis in the synovial fluid and synovial tissue

|
Scooped by
Gilbert C FAURE
November 28, 2024 1:07 PM
|

|
Scooped by
Gilbert C FAURE
January 24, 2024 6:04 AM
|
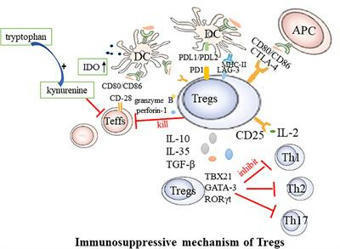
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune condition marked by inflammation of the joints, degradation of the articular cartilage, and bone resorption. Recent studies found the absolute and relative decreases in circulating regulatory T cells (Tregs) in RA patients. Tregs are a unique type of cells exhibiting immunosuppressive functions, known for expressing the Foxp3 gene. They are instrumental in maintaining immunological tolerance and preventing autoimmunity. Increasing the absolute number and/or enhancing the function of Tregs are effective strategies for treating RA. This article reviews the studies on the mechanisms and targeted therapies related to Tregs in RA, with a view to provide better ideas for the treatment of RA.

|
Scooped by
Gilbert C FAURE
December 2, 2023 4:35 AM
|
WHAT IS ALREADY KNOWN ON THIS TOPICPatients with rheumatoid arthritis (RA) can be divided into seropositive and seronegative subgroups. The presence of antibodies against post-translationally modified (PTM) proteins such as citrullinated proteins is nowadays used as a diagnostic and prognostic marker in RA. Antibodies directed against carbamylated proteins have more recently been shown to be present in a subset of the seronegative patients and are associated with bone erosions in that group.WHAT THIS STUDY ADDSIn this study, two different anti-PTM antibodies are investigated: anti-advanced glycation end-product modified protein antibodies (anti-AGE) and anti-malondialdehyde-acetaldehyde adduct modified protein antibodies (anti-MAA). These antibodies can be detected in several forms of inflammatory arthritis. Within seronegative RA (negative for rheumatoid factor, anti-citrullinated protein antibodies and anti-carbamylated protein antibodies), 16.9% of patients are positive for anti-MAA and/or anti-AGE antibodies. This subgroup is characterised by an association with HLA-DRB1*03, increased radiographic joint damage and (for anti-MAA) inflammation.HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICYThe presence of anti-PTM antibodies like anti-AGE and anti-MAA in patients with RA and other patients with inflammatory arthritis previously considered to be seronegative, may not only serve as a prognostic marker, but importantly may contribute to understanding the pathogenesis of these conditions, including a subset of RA.IntroductionIn rheumatoid arthritis (RA) around two-thirds of patients are autoantibody positive for rheumatoid factor (RF), anti-citrullinated protein antibodies (ACPA) and/or anti-carbamylated protein (anti-CarP) antibodies.1 The remaining seronegative subgroup of RA is clinically heterogeneous and thus far no reliable biomarkers are available to identify these patients or predict their disease course.1ACPA and anti-CarP are antibodies that recognise proteins that have undergone post-translational modification (PTM), citrullination of arginine and carbamylation of lysine respectively.2 3 However, many other types of PTMs exist.4 Two examples of PTMs that are found to associate with disease are advanced glycation end-products (AGE) and malondialdehyde-acetaldehyde adducts (MAA). AGEs are a result of oxidative stress and tissue damage5 and are, for example, present in patients with diabetes mellitus type 2.6 Interestingly, in these patients also antibodies directed against this PTM were observed.6 MAA modifications are a result of reactive oxygen species that are formed during inflammation and oxidative stress.7 Both MAA-modified proteins and anti-MAA antibodies are found in patients with RA, as well as in other diseases.7 AGE and MAA are both highly immunogenic PTMs.8 9 Therefore, it is plausible that antibodies against AGE and MAA are also present in patients with arthritis.Seronegative RA is associated with HLA-DRB1*03, suggesting a role for immunopathology driven by, for example, B cell immunity.10 Indeed, within the ACPA-negative patients, the presence of anti-CarP was associated with HLA-DRB1*03.11 12 However, it did not yet explain the full HLA-DRB1*03 association, raising the possibility that other anti-PTM responses may be present in ‘seronegative’ RA that are present in the remainder of the HLA-DRB1*03 positive individuals.13 14 On top of this haplotype association, within these patients with ACPA-negative RA, anti-CarP was found to associate with a more severe radiological progression.3 Patients with seronegative RA are a diverse group of patients that in many ways resemble undifferentiated arthritis. Presence of antibodies, like anti-PTM antibodies, might help to better understand and characterise subgroups that possibly belong to this so-called seronegative RA.We therefore investigated whether anti-AGE and anti-MAA antibodies are present in patients with RA and other forms of arthritis, and whether they could potentially close the so-called serological gap1 in seronegative RA.MethodsPatientsOne thousand one hundred eighty-six patients with arthritis of at least one joint and a symptom duration of less than 2 years were included in the Leiden Early Arthritis Clinic (EAC) cohort.15 Data were collected at baseline and follow-up (4, 12 months and yearly thereafter). Patients were being followed as long as the patient remained being seen clinically by the rheumatologist. RA was classified based on the 1987 American College of Rheumatology criteria (n=648).16 Definitive diagnoses other than RA (n=538) were made by the treating physician after 1 year of follow-up and were predominantly psoriatic arthritis (PsA) (n=100), inflammatory osteoarthritis (n=95) and gout (n=93) besides other more rare forms of arthritis. For this manuscript, the following diagnoses were termed autoimmune (AI): RA, PsA, spondyloarthritis, sarcoidosis, systemic lupus erythematosus (SLE) and paraneoplastic arthritis. The diagnoses termed as non-autoimmune (non-AI) were: gout, pseudogout and septic arthritis. Clinical and demographic patient characteristics were collected as described previously.17Genotyping, radiological progression and remissionFrom all patients, HLA genotypes were established as described previously.18 The alleles that were marked as shared epitope-encoding HLA (HLA-SE) positive were: HLA-DRB1*01:01, 01:02, 04:01, 04:04, 04:05, 04:08, 10:01 and 14:02. For the radiological progression analyses, 2853 X-ray sets of the hands and feet of 635 patients with RA were scored as described previously using the Sharp-van der Heijde score (SHS).19 20 Sustained drug-free remission (SDFR) was defined as the absence of clinical synovitis after discontinuation of disease-modifying antirheumatic drug treatment, that persisted for the entire follow-up, being at least 1 year.21Anti-AGE and anti-MAA measurementsAnti-AGE and anti-MAA antibodies were detected using an in-house ELISA based on modified fetal calf serum (FCS) as described previously.22 Briefly, modified and non-modified FCS were coated to a Nunc Maxisorp ELISA plate (430341, Thermofisher). In between each sequential step, plates were washed three times using phosphate buffered saline (PBS)/0.05%Tween (Sigma, P1379). After blocking (PBS/1%bovine serum albumin) for 6 hours at 4°C plates were incubated overnight at 4°C with 1/100 or 1/1000 diluted serum for anti-AGE and anti-MAA, respectively. Each plate contained a standard of anti-PTM positive serum to calculate arbitrary units. After incubation, IgG levels were detected using Rabbit-anti-Human IgG-HRP (Dako, P0214). Plates were developed by incubating with 2,2'-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid (ABTS)/0.015% H2O2 (A1888 and 7722-84-1, both from Merck) and absorbance at 415 nm was measured using a microplate reader (Bio-Rad iMark). The cut-off for positivity was set as the mean arbitrary units plus two times the SD of 80 healthy controls, excluding values higher than 10× the mean.Statistical analysisIndependent samples t-test and Mann-Whitney U tests were used to analyse the baseline characteristics. The association of HLA-DRB1*03 with autoantibodies was assessed with logistic regression, and stratified for anti-cyclic citrullinated peptide 2 (anti-CCP2) and anti-CarP if relevant. Correlations between anti-PTM antibodies and inflammatory markers were calculated using Spearman’s rank correlation. For the radiological progression analyses, a multivariate normal regression model for longitudinal data was used with SHS as response variable. The model controlled for the age, sex and inclusion year of the patients.19 SDFR development until follow-up was calculated using Kaplan-Meier survival analysis and Cox’s regression. All statistical analysis were performed using SPSS statistics V.25 (IBM).ResultsAnti-AGE and anti-MAA in patients with arthritisBaseline characteristics are described in table 1. Anti-PTM antibody levels were measured in RA and non-RA arthritis patients and compared with healthy controls (figure 1A,B and online supplemental table 1). The non-RA arthritis group was divided into subgroups and separately depicted based as AI arthritis (without RA) including PsA, paraneoplastic arthritis, SLE, sarcoidosis and spondyloarthritis and as non-AI arthritis including septic arthritis, gout and pseudogout.Supplemental material[rmdopen-2023-003480supp001.pdf]View inline View popup Table 1 Baseline characteristics of the rheumatoid arthritis (RA), non-RA, autoimmune no RA and non-autoimmune group<img class="highwire-fragment fragment-image" height="440" src="https://rmdopen.bmj.com/content/rmdopen/9/4/e003480/F1.medium.gif"; width="315" alt="Figure 1">Download figure Open in new tab Download powerpoint Figure 1 Anti-AGE and anti-MAA show higher levels in RA and occur in a subgroup of patients with anti-CarP anti-CCP2 negative RA. IgG antibody levels of anti-AGE (A) and anti-MAA (B) in patients with (n=648) and without (n=538) RA. Early patients with arthritis were separately depicted as groups: AI without RA (including psoriatic arthritis, paraneoplastic arthritis, SLE, sarcoidosis and spondyloarthritis) and non-AI (including septic arthritis, gout, pseudogout). (C) Upset plots of groups of patients with RA (n=499*) positive for anti-PTM combinations; anti-AGE, anti-MAA, anti-CarP, anti-CCP2 and RF. *Data for anti-CarP was missing for 149 patients with RA. AGE, advanced glycation end-product; AI, autoimmune; aU/mL, arbitrary units per mL; CarP, carbamylated protein; CCP2, citrullinated cyclic peptide 2; MAA, malondialdehyde acetaldehyde adduct; RA, rheumatoid arthritis; RF, rheumatoid factor.Compared with healthy controls, anti-AGE and anti-MAA were most prevalent in RA (anti-AGE: 7.5% in HC vs 44.6% in RA and anti-MAA: 3.8% in HC vs 46.1% in RA) but were also present in other types of early arthritis. Within patients without RA, anti-AGE and anti-MAA were present in 32.9% and 30.3%, respectively and in non-RA AI arthritis anti-AGE and anti-MAA were found in 38.5% and 41.5%, respectively. These data indicate that the presence of anti-PTM antibodies is not specific for RA. When analysing combinations of autoantibodies, the largest subgroup of patients with RA (n=99) had all four anti-PTM antibodies (anti-AGE, anti-MAA, anti-CarP, anti-CCP2) as well as RF, after which the second largest group (n=63) was characterised by the combination of RF, anti-CCP2 and anti-CarP (figure 1C).Interestingly, 67 (34.0%) and 57 (28.9%) of patients with seronegative (RF negative, ACPA negative and anti-CarP negative) RA were positive for anti-AGE and anti-MAA, respectively. Moreover, 40 (20.3%) of these patients with seronegative RA were positive for both anti-AGE and anti-MAA. These anti-PTM responses may identify a new subgroup in the patients with otherwise seronegative RA.HLA-DRB1*03 associates with anti-AGE and anti-MAA independently of anti-CarP in patients with anti-CCP2-negative RASince HLA class II alleles are known to associate with autoantibody positivity in RA, we sought to investigate the presence of HLA-SE and its association with anti-AGE and anti-MAA antibodies. Of all patients with RA, 63.3% were HLA-SE+ (table 1). Based on the well-known association between HLA-SE and RA, the HLA-SE alleles were assessed and were significantly more prevalent in all RA subgroups compared with healthy controls. In the anti-AGE-positive group, as compared with patients with anti-AGE-negative RA however, the prevalence of HLA-SE alleles was similar (table 2). The same was true for anti-MAA; therefore, both anti-AGE and anti-MAA antibodies were not associated with HLA-SE.View inline View popup Table 2 Association between anti-AGE and anti-MAA antibodies and HLA-SE and HLA-DRB1*03 presence in RA and HLA-DRB1*03 presence in non-RA patients from the Leiden EAC cohortSince HLA-DRB1*03 is associated with seronegative RA and anti-CarP antibodies in this disease subset, we sought to investigate the association of HLA-DRB1*03 with anti-AGE and anti-MAA. In patients with RA, HLA-DRB1*03 was more prevalent in anti-AGE-positive and anti-MAA-positive patients as compared with healthy controls with OR values of 1.34 (95% CI 1.01 to 1.78, p=0.05) and 1.29 (95% CI 0.96 to 1.73, p=0.09), although this did not achieve statistical significance compared with anti-AGE-negative or anti-MAA-negative patients, respectively (table 2, part I). To investigate whether HLA-DRB1*03 is associated with anti-MAA and anti-AGE in anti-CCP2-negative RA, we focused on this subset and stratified the analysis for anti-CarP. Within the patients with anti-CCP2 negative RA, anti-AGE and anti-MAA antibodies were associated with HLA-DRB1*03 compared with healthy controls (OR: 1.98, 95% CI 1.27 to 3.07, p=0.003, and OR: 2.37, 95% CI 1.50 to 3.74, p<0.001, respectively). Anti-MAA was associated with HLA-DRB1*03 in the anti-CCP2 negative stratum independent of anti-CarP (OR: 1.91, 95% CI 1.11 to 3.30, p=0.02) (table 2, part II). In this stratified analysis, anti-AGE showed the same trend for association but did not reach significance (OR: 1.48, 95% CI 0.86 to 2.52, p=0.16). Since anti-AGE and anti-MAA often co-occur, we next stratified the association analysis for these autoantibodies, to dissect whether the observed association to HLA-DRB1*03 could be attributed to one of them in particular. After stratification for anti-AGE or anti-MAA, only patients with double positive RA showed a significant association with HLA-DRB1*03 compared with healthy controls (online supplemental table 2, part I). Since some controversy exists on the association of HLA-DRB1*03 in patients with anti-CCP2 negative RA, we investigated the association between anti-AGE and anti-MAA with HLA-DRB1*03 within patients with HLA-SE negative RA. In both HLA-SE negative and anti-CCP2 negative stratum, we find similar associations with anti-AGE/-MAA and HLA-DR1*03 (table 2, part III).In non-RA arthritis patients, both anti-AGE and anti-MAA showed a similar association with HLA-DRB1*03 with OR values of 2.34 (95% CI 1.58 to 3.47, p<0.001) and 1.94 (95% CI 1.29 to 2.92, p=0.002) compared with healthy controls (table 2, part I). In a comparison within the non-RA arthritis patients, HLA DRB1*03 remained significantly associated with anti-AGE-positive compared with anti-AGE-negative patients (OR: 2.22, 95% CI 1.28 to 3.84, p=0.01), while the association with anti-MAA did not remain significant. To disentangle the effects of anti-AGE and anti-MAA, analyses were again stratified, after which only the presence of anti-AGE in patients with anti-MAA-negative without RA remained significantly associated with HLA-DRB1*03 (online supplemental table 2, part II).Taken together, these data indicate that anti-AGE and anti-MAA associate with HLA-DRB1*03 in RA and non-RA arthritis patients, and that this association (which cannot be ascribed to anti-AGE or anti-MAA in particular) is mainly present in patients with anti-CCP2 negative RA. Similar associations were observed in patients with HLA-SE negative RA.Inflammation markers associate with anti-MAA positivity in RA and non-RA arthritisNext, we sought to investigate whether anti-PTM antibodies correlate with inflammation markers erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) (table 3). Higher inflammation parameters in anti-AGE- and anti-MAA-positive individuals were observed in RA and non-RA arthritis patients, and in both the autoimmune and non-autoimmune subgroups of patients with arthritis. To investigate whether both anti-MAA and anti-AGE were associated with acute phase reactants in RA independently, anti-AGE and anti-MAA were stratified for each other. After this stratification, anti-AGE was no longer associated with either CRP or ESR whereas the association of anti-MAA with these inflammation markers remained significant (online supplemental table 3). These data indicate that anti-PTM responses, especially anti-MAA, is associated with markers of inflammation in early arthritis in both RA and non-RA arthritis patients.View inline View popup Table 3 Association between anti-AGE and anti-MAA antibin RA and non-RA arthritis patientsodies and ESR and CRP levelsAnti-AGE and anti-MAA associate with radiological progression in patients with anti-CCP2-negative RAWe next analysed if the presence of anti-AGE and anti-MAA is associated with radiological progression in RA. Anti-AGE-positive patients displayed more radiographic damage per year than anti-AGE-negative patients (p<0.001) (figure 2A). Data were then stratified for anti-CCP2, which revealed that this association was mainly present in the anti-CCP2-negative subgroup (figure 2B). When anti-CCP2 negative patients were further stratified for anti-CarP, the association between anti-AGE and radiographic progression remained significant (figure 2C). This indicates that in patients with anti-CCP2 negative RA, anti-AGE is associated with radiological progression independent of anti-CarP, suggesting that this anti-PTM antibody could discriminate a different subgroup. Anti-MAA positivity was also associated with radiological progression (p=0.002) (figure 2D). This effect was also observed in the anti-CCP2-negative stratum (figure 2E), although no longer significant after stratifying for anti-CCP2. The latter could be a consequence of power as the effect size (beta) which decreased only slightly to 1.03/year, p=0.16 (figure 2E).<img width="393" alt="Figure 2" height="440" class="highwire-fragment fragment-image" src="https://rmdopen.bmj.com/content/rmdopen/9/4/e003480/F2.medium.gif">Download figure Open in new tab Download powerpoint Figure 2 Anti-AGE and anti-MAA associate with radiological progression in patients with RA (n=600). (A) Radiological progression in anti-AGE positive and negative RA. (B) Data stratified for CCP2. (C) Data stratified for anti-CarP in anti-CCP2-negative stratum. (D) Radiological progression in anti-MAA positive and negative RA. (E) Data stratified for CCP2. Data presented as estimate (95% CI), p value. AGE, advanced glycation end-product; CarP, carbamylated protein; CCP2, citrullinated cyclic peptide 2; MAA, malondialdehyde acetaldehyde adduct.Presence of anti-MAA or anti-AGE is not associated with SDFR in RANext, we sought to investigate whether anti-AGE and anti-MAA were associated with SDFR over time (online supplemental figure 3). Anti-AGE was not associated with SDFR, HR 0.93 (95% CI 0.66 to 1.30; p=0.66) which did not differ after adjusting for CCP2 status (HR 1.14, 95% CI 0.81 to 1.61, p=0.46). Anti-MAA-positive patients were less likely to achieve SDFR, compared with anti-MAA-negative patients, HR 0.72 (95% CI 0.51 to 1.00, p=0.053). After adjusting for CCP2 status, there was no longer an association between anti-MAA and SDFR, HR 1.05 (95% CI 0.74 to 1.50, p=0.80).DiscussionIn this study, we demonstrated that anti-AGE and anti-MAA are present in patients with RA, and interestingly also in a substantial part of patients with otherwise seronegative RA. This is not specific for RA, as anti-AGE and anti-MAA antibodies were also present in other forms of early arthritis. Both anti-AGE and anti-MAA are associated with HLA-DRB1*03 in RA, and anti-AGE is also associated with HLA-DR1*03in non-RA arthritis patients. Anti-AGE and anti-MAA are associated with a distinct clinical phenotype: anti-AGE associates with radiological progression in RA whereas anti-MAA only showed a trend with radiological progression but associated with increased inflammatory parameters in both RA and non-RA arthritis.Associations with particular HLA class II alleles have been described to occur in many seropositive AI diseases.13 14 More specifically, HLA-DRB1*03, initially reported to be associated with anti-CCP2 negative RA, was later associated with the presence of anti-CarP, although not all HLA-DRB1*03-positive patients were anti-CarP-positive.10 12 In this study, we observed that HLA-DRB1*03 was associated with anti-AGE and anti-MAA in patients with anti-CCP2 negative RA which was independent of anti-CarP, thereby identifying another subgroup of anti-CCP2 negative RA that is associated with HLA-DRB1*03. In addition, anti-AGE associated with HLA-DRB1*03 in non-RA confirming the robustness of this finding. Together, these observations provide additional insight into the association of HLA-DBR1*03 with (rheumatoid) arthritis; although these alleles are not associated with the presence of ACPA, they do appear to predispose to the formation of other autoantibodies (anti-CarP, anti-AGE and anti-MAA) in a process in which HLA class II-associated T-cell-dependent immune responses are likely to be involved.Interestingly, in RA, anti-AGE associated with radiological progression independent of anti-CCP2 and anti-CarP suggesting an additive value of anti-AGE in determining disease evolution as it could define a new subgroup of patients with RA. Strikingly, anti-AGE was not associated with SDFR. In RA and non-RA, a subgroup of patients is characterised by more extensive inflammation and the presence of anti-MAA antibodies, while a subgroup of patients with CCP2-negative RA is characterised by radiological progression and presence of anti-AGE antibodies. Based on these results, distinct subgroups within RA and non-RA can be delineated based on their specific clinical phenotype.The presence of AGE-modified proteins and anti-AGE antibodies has been observed in diabetes and hypertension.6 23 Also, in synovial tissue and sera of patients with RA, AGE-modified proteins have been detected.24–26 In addition, MAA-modified proteins have been observed before in RA tissue7 and it is clear that both modifications can be induced by inflammation and oxidative stress in the inflamed joint.5 7 Our study now adds that in a subset of the patients with RA antibodies against these PTMs are present. Additionally, anti-AGE and anti-MAA have been found to be associated with ESR in previous studies in RA and SLE.22 PTMs and anti-PTMs such as anti-AGE and anti-MAA add to the understanding that the combined presence of the antigen and the antibody could trigger effector mechanisms and contribute to the overall process of arthritis and joint damage, in RA and also in non-RA. It would therefore be interesting to investigate whether next to carbamylated proteins27 also the modifications AGE and MAA are present in cartilage and synovium. Additionally, experimental pathogenicity studies on anti-AGE and anti-MAA specifically should be performed to elucidate on the contribution of these anti-PTM antibodies to pathogenesis.There are some limitations to our study. Data on anti-CarP antibody levels were missing for 149 patients with RA; therefore, analysis using stratification including anti-CarP could only be performed in a subgroup of all patients with RA. However, this group still consists of 499 patients with RA and therefore still appears a good representation of the RA population. Radiological progression was assessed in 635 patients with RA included before 2006. Thereafter, radiographs have not been scored since radiographic damage has become rare/nearly non-existent with current treatment strategies. This effectively enabled us to detect differences in the, earlier, informative part of the cohort. When stratifying radiological progression data, groups became small and therefore could suffer from insufficient power implicating that significance could not always be reached. It is therefore important to verify associations using different and/or bigger cohorts to be able to generalise findings to the whole RA population. Additionally, in order to verify the results obtained in this study, a replication cohort is needed. In such a study, IgA and IgM responses could be included to elaborate on the full anti-PTM antibody responses in patients with (rheumatoid) arthritis.28 29 One of the strengths of this study is that the EAC is a well-defined cohort containing RA and non-RA early arthritis patients with extensive information on the HLA haplotype and radiological progression for patients with RA.15 Second, antibody responses have been investigated on the PTM-modified proteins and their control proteins. All PTMs were created on the same antigen backbone and reactivity against FCS itself was subtracted from the results. This results in reliable measurements that capture truly PTM-specific signals and decreases the chance of false observations.30 Additionally, correlation analyses were performed (data not shown) and data were stratified for the other investigated anti-PTM and to verify that anti-AGE and anti-MAA are solely responsible for the observed result and not cross-reactive.In conclusion, anti-AGE and anti-MAA antibodies are both prevalent in patients with RA, and other inflammatory rheumatic conditions, and although not specific for RA they each correlate with specific parameters. Anti-MAA associates with HLA-DRB1*03 in CCP2-negative (RA) patients independent of anti-CarP and associates with inflammation. Anti-AGE associates with HLA-DRB1*03 in patients with CCP2-negative RA and is associated with a worse radiological progression especially in patients with anti-CCP2-negative and anti-CarP-negative RA. With this study, we have now characterised a seropositive subgroup within the heterogeneous group of patients with RA that have been thus far been considered seronegative.Data availability statementData are available upon reasonable request. Requests can be sent to l.a.trouw@lumc.nl.Ethics statementsPatient consent for publicationNot applicable.Ethics approvalThe Leiden Early Arthritis Clinic (EAC) cohort was approved by the Medical Ethics Committee Leiden The Hague Delft under reference number: B19.008. For the current study, measurement of anti-PTM antibodies in serum from the EAC cohort is approved under reference number B15.003. Participants gave informed consent to participate in the study before taking part.AcknowledgmentsWe thank Marloes Verstappen and Bianca M. Boxma-de Klerk for their assistance regarding the remission analysis on EAC cohort data.References↵Trouw LA, Mahler M. Closing the serological gap: promising novel biomarkers for the early diagnosis of rheumatoid arthritis. Autoimmun Rev 2012;12:318–22. doi:10.1016/j.autrev.2012.05.007OpenUrlCrossRefPubMed↵Schellekens GA, de Jong BA, van den Hoogen FH, et al. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest 1998;101:273–81. doi:10.1172/JCI1316OpenUrlCrossRefPubMedWeb of Science↵Shi J, Knevel R, Suwannalai P, et al. Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci U S A 2011;108:17372–7. doi:10.1073/pnas.1114465108OpenUrlAbstract/FREE Full Text↵Xu H, Wang Y, Lin S, et al. PTMD: a database of human disease-associated post-translational modifications. Genom Proteom Bioinform 2018;16:244–51. doi:10.1016/j.gpb.2018.06.004OpenUrl↵Schmidt AM, Yan SD, Yan SF, et al. The multiligand receptor RAGE as a progression factor amplifying immune and inflammatory responses. J Clin Invest 2001;108:949–55. doi:10.1172/JCI14002OpenUrlCrossRefPubMedWeb of Science↵Nikolov A, Blazhev A, Tzekova M, et al. Serum levels of antibodies to advanced glycation end products in patients with type 2 diabetes mellitus and hypertension. Folia Med (Plovdiv) 2020;62:295–301. doi:10.3897/folmed.62.e47788OpenUrl↵Thiele GM, Duryee MJ, Anderson DR, et al. Malondialdehyde-acetaldehyde adducts and anti-malondialdehyde-acetaldehyde antibodies in rheumatoid arthritis. Arthritis Rheumatol 2015;67:645–55. doi:10.1002/art.38969OpenUrl↵Buongiorno AM, Morelli S, Sagratella E, et al. Immunogenicity of advanced glycation end products in diabetic patients and in nephropathic non-diabetic patients on hemodialysis or after renal transplantation. J Endocrinol Invest 2008;31:558–62. doi:10.1007/BF03346408OpenUrlPubMed↵Thiele GM, Tuma DJ, Willis MS, et al. Soluble proteins modified with acetaldehyde and malondialdehyde are Immunogenic in the absence of adjuvant. Alcohol Clin Exp Res 1998;22:1731–9.OpenUrlCrossRefPubMed↵Verpoort KN, van Gaalen FA, van der Helm-van Mil AHM, et al. Association of HLA-DR3 with anti-cyclic citrullinated peptide antibody-negative rheumatoid arthritis. Arthritis Rheum 2005;52:3058–62. doi:10.1002/art.21302OpenUrlCrossRefPubMedWeb of Science↵Regueiro C, Rodriguez-Rodriguez L, Triguero-Martinez A, et al. Specific association of HLA-Drb1*03 with anti-carbamylated protein antibodies in patients with rheumatoid arthritis. Arthritis Rheumatol 2019;71:331–9. doi:10.1002/art.40738OpenUrl↵Jiang X, Trouw LA, van Wesemael TJ, et al. Anti-carp antibodies in two large cohorts of patients with rheumatoid arthritis and their relationship to genetic risk factors, cigarette smoking and other autoantibodies. Ann Rheum Dis 2014;73:1761–8. doi:10.1136/annrheumdis-2013-205109OpenUrlAbstract/FREE Full Text↵Kirino Y, Remmers EF. Genetic architectures of seropositive and seronegative rheumatic diseases. Nat Rev Rheumatol 2015;11:401–14. doi:10.1038/nrrheum.2015.41OpenUrlCrossRefPubMed↵Cruz-Tapias P, Pérez-Fernández OM, Rojas-Villarraga A, et al. Shared HLA class II in six autoimmune diseases in Latin America: a meta-analysis. Autoimmune Dis 2012;2012:569728. doi:10.1155/2012/569728↵de Rooy DPC, van der Linden MPM, Knevel R, et al. Predicting arthritis outcomes--what can be learned from the Leiden early arthritis clinic Rheumatology (Oxford) 2011;50:93–100. doi:10.1093/rheumatology/keq230OpenUrlCrossRefPubMedWeb of Science↵Arnett FC, Edworthy SM, Bloch DA, et al. The American rheumatism association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. doi:10.1002/art.1780310302OpenUrlCrossRefPubMedWeb of Science↵van Aken J, van Bilsen JH, Allaart CF, et al. The leiden early arthritis clinic. Clin Exp Rheumatol 2003;21:S100–5.OpenUrlPubMedWeb of Science↵Huizinga TWJ, Amos CI, van der Helm-van Mil AHM, et al. Refining the complex rheumatoid arthritis phenotype based on specificity of the HLA-DRB1 shared EPITOPE for antibodies to citrullinated proteins. Arthritis Rheum 2005;52:3433–8. doi:10.1002/art.21385OpenUrlCrossRefPubMedWeb of Science↵Knevel R, Krabben A, Brouwer E, et al. Genetic variants in Il15 associate with progression of joint destruction in rheumatoid arthritis: a multicohort study. Ann Rheum Dis 2012;71:1651–7. doi:10.1136/annrheumdis-2011-200724OpenUrlAbstract/FREE Full Text↵van der Heijde D. How to read radiographs according to the sharp/Van der heijde method. J Rheumatol 2000;27:261–3.OpenUrlPubMedWeb of Science↵Verstappen M, van Steenbergen HW, de Jong PHP, et al. Unraveling heterogeneity within ACPA-negative rheumatoid arthritis: the subgroup of patients with a strong clinical and serological response to initiation of DMARD treatment favor disease resolution. Arthritis Res Ther 2022;24:4. doi:10.1186/s13075-021-02671-z↵Monahan RC, van den Beukel MD, Borggreven NV, et al. Autoantibodies against specific post-translationally modified proteins are present in patients with lupus and associate with major neuropsychiatric manifestations. RMD Open 2022;8:e002079. doi:10.1136/rmdopen-2021-002079↵Aso Y, Inukai T, Tayama K, et al. Serum concentrations of advanced glycation endproducts are associated with the development of atherosclerosis as well as diabetic microangiopathy in patients with type 2 diabetes. Acta Diabetol 2000;37:87–92. doi:10.1007/s005920070025OpenUrlCrossRefPubMedWeb of Science↵Drinda S, Franke S, Canet CC, et al. Identification of the advanced glycation end products N(Epsilon)-carboxymethyllysine in the synovial tissue of patients with rheumatoid arthritis. Ann Rheum Dis 2002;61:488–92. doi:10.1136/ard.61.6.488OpenUrlAbstract/FREE Full Text↵de Groot L, Hinkema H, Westra J, et al. Advanced glycation endproducts are increased in rheumatoid arthritis patients with controlled disease. Arthritis Res Ther 2011;13:R205. doi:10.1186/ar3538↵Ligier S, Fortin PR, Newkirk MM. A new antibody in rheumatoid arthritis targeting glycated IgG: Igm anti-IgG-AGE. Br J Rheumatol 1998;37:1307–14. doi:10.1093/rheumatology/37.12.1307OpenUrlCrossRefPubMed↵Verheul MK, Janssen GMC, de Ru A, et al. Mass-spectrometric identification of carbamylated proteins present in the joints of rheumatoid arthritis patients and controls. Clin Exp Rheumatol 2021;39:570–7. doi:10.55563/clinexprheumatol/0ms5pkOpenUrlPubMed↵van Delft MAM, van der Woude D, Toes REM, et al. Secretory form of rheumatoid arthritis-associated autoantibodies in serum are mainly of the Igm Isotype, suggesting a continuous reactivation of autoantibody responses at mucosal surfaces. Ann Rheum Dis 2019;78:146–8. doi:10.1136/annrheumdis-2018-213724OpenUrlFREE Full Text↵Mikuls TR, Duryee MJ, England BR, et al. Malondialdehyde-acetaldehyde antibody concentrations in rheumatoid arthritis and other rheumatic conditions. Int Immunopharmacol 2018;56:113–8. doi:10.1016/j.intimp.2018.01.022OpenUrl↵Åhlin E, Elshafie AI, Nur MAM, et al. Anti-citrullinated peptide antibodies in sudanese patients with leishmania donovani infection exhibit reactivity not dependent on citrullination. Scand J Immunol 2015;81:201–8. doi:10.1111/sji.12265OpenUrl

|
Rescooped by
Gilbert C FAURE
from Laboratory Medicine
June 29, 2023 4:02 AM
|
Should you Assess Rheumatoid Factor Serially? Save Dr. Jack Cush discusses abstract OP0272 at EULAR 2023 in Milan, Italy. ADD THE FIRST COMMENT If you are a health practitioner, you may Login/Register to comment.Due to the nature of these comment forums, only health practitioners are allowed to...

|
Scooped by
Gilbert C FAURE
April 5, 2023 4:19 AM
|
Glucocorticoids are recommended for short-term use in rheumatoid arthritis (RA), but many patients remain on long-term therapy. We evaluated the variability in glucocorticoid prescribing across rheumatologists to inform interventions to limit long-ter

|
Scooped by
Gilbert C FAURE
December 2, 2022 11:19 AM
|
Glycosylation has a profound influence on protein activity and cell biology through a variety of mechanisms, such as protein stability, receptor interactions and signal transduction. In many rheumatic diseases, a shift in protein glycosylation occurs, and is associated with inflammatory processes and disease progression. For example, the Fc-glycan composition on (auto)antibodies is associated with disease activity, and the presence of additional glycans in the antigen-binding domains of some autoreactive B cell receptors can affect B cell activation. In addition, changes in synovial fibroblast cell-surface glycosylation can alter the synovial microenvironment and are associated with an altered inflammatory state and disease activity in rheumatoid arthritis. The development of our understanding of the role of glycosylation of plasma proteins (particularly (auto)antibodies), cells and tissues in rheumatic pathological conditions suggests that glycosylation-based interventions could be used in the treatment of these diseases. Glycosylation is a common modification that can affect protein stability and interactions. In this Review, the authors discuss the role of glycosylation in rheumatic diseases, as well as the therapeutic potential of glycosylation-based interventions.

|
Scooped by
Gilbert C FAURE
June 15, 2022 8:51 AM
|
AbstractObjectives Immune and stromal cell communication is central in the pathogenesis of rheumatoid arthritis (RA) and psoriatic arthritis (PsA), however, the nature of these interactions in the synovial pathology of the two pathotypes can differ.

|
Scooped by
Gilbert C FAURE
February 10, 2022 8:57 AM
|
Antibodies targeting the activation marker CD83 can achieve immune suppression by targeting antigen-presenting mature dendritic cells (DC). This study investigated the immunosuppressive mechanisms of anti-CD83 antibody treatment in mice and tested its efficacy in a model of autoimmune rheumatoid arthritis. A rat anti-mouse CD83 IgG2a monoclonal antibody, DCR-5, was developed and functionally tested in mixed leukocyte reactions, demonstrating depletion of CD83+ conventional (c)DC, induction of regulatory DC (DCreg), and suppression of allogeneic T cell proliferation. DCR-5 injection into mice caused partial splenic cDC depletion for 2–4 days (mostly CD8+ and CD83+ cDC affected) with a concomitant increase in DCreg and regulatory T cells (Treg). Mice with collagen induced arthritis (CIA) treated with 2 or 6 mg/kg DCR-5 at baseline and every three days thereafter until euthanasia at day 36 exhibited significantly reduced arthritic paw scores and joint pathology compared to isotype control or untreated mice. While both doses reduced anti-collagen antibodies, only 6 mg/kg achieved significance. Treatment with 10 mg/kg DCR-5 was ineffective. Immunohistological staining of spleens at the end of CIA model with CD11c, CD83, and FoxP3 showed greater DC depletion and Treg induction in 6 mg/kg compared to 10 mg/kg DCR-5 treated mice. In conclusion, DCR-5 conferred protection from arthritis by targeting CD83, resulting in selective depletion of mature cDC and subsequent increases i

|
Scooped by
Gilbert C FAURE
October 13, 2021 11:32 AM
|
Glucocorticoids (GCs) remain regularly used drugs in patients with chronic inflammatory rheumatic diseases. As long-term intake at high dosages is associated with harm, it is generally advised that GCs be tapered and stopped.

|
Scooped by
Gilbert C FAURE
October 13, 2021 11:29 AM
|
Rheumatoid arthritis (RA) and osteoarthritis (OA) are two most common rheumatic diseases in the world. Although there are standard methods for the diagnosis of both RA and OA, the differentials in some cases are poor.

|
Scooped by
Gilbert C FAURE
October 8, 2021 6:30 AM
|
|


 Your new post is loading...
Your new post is loading...
 Your new post is loading...
Your new post is loading...