Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
May 12, 2021 4:47 AM
|
When it comes to loosening COVID restrictions all eyes are usually trained on the famous R number. But as epidemiologists Julia Gog and Thomas House recently explained to us, there's also another important factor to consider alongside R. That's the prevalence of COVID-19 in the population: the proportion of people who currently have the disease. Put simply, if prevalence has been so high that the NHS is in crisis, then opening up might stretch it to breaking point, even if R is less than 1, or would remain so. If, on the other hand, prevalence is very low, we might be able to tolerate a higher value of R as it would not immediately lead to many cases. This is true particularly if prevalence has been low for some time. We've illustrated this idea in the schematic plot below. The vertical axis measures prevalence and the horizontal axis measures R. Any point on this plot, such as the one we marked in black right in the middle, corresponds to a situation where we have the value of R that lies directly beneath the point on the horizontal axis, and the value of prevalence that lies directly to the left of the point on the vertical axis read this excellent piece at https://plus.maths.org/content/R-not-all?nl=0

|
Scooped by
nrip
May 9, 2021 7:39 AM
|
The WHO Hub for Pandemic and Epidemic Intelligence will be a global platform for pandemic and epidemic intelligence, creating shared and networked access to vital multi-sectoral data, driving innovations in data analytics and building the communities
of practice needed to predict, prevent, detect, prepare for and respond to worldwide health threats. The WHO Hub will be a new global collaboration of countries and partners worldwide, driving innovations to increase availability and linkage of diverse data; develop tools and predictive models for risk analysis; and to monitor disease control measures
and infodemics. The WHO Hub will enable partners from around the world to collaborate and co-create the tools and data access that all countries need to prepare, detect and respond to pandemic and epidemic risks. The World Health Organization (WHO) and the Federal Republic of Germany will establish a new global hub for pandemic and epidemic intelligence, data, surveillance and analytics innovation. The Hub, based in Berlin and working with partners around the
world, will lead innovations in data analytics across the largest network of global data to predict, prevent, detect prepare for and respond to pandemic and epidemic risks worldwide. Critically, the WHO Hub will support the work of public health experts and policy-makers in all countries with insights so
they can take rapid decisions to prevent and respond to future public health emergencies.“We need to identify pandemic and epidemic risks as quickly as possible, wherever they occur in the world. For that aim, we need to strengthen the global early warning surveillance system with improved collection of health-related data and inter-disciplinary risk analysis,” said Jens Spahn, German Minister of Health. Working with partners globally, the WHO Hub will drive a scale-up in innovation for existing forecasting and early warning capacities in WHO and Member States. At the same time, the WHO Hub will accelerate global collaborations across public and private sector organizations, academia, and international partner networks. It will help them to collaborate and co-create the necessary tools for managing and analyzing data for early warning surveillance. It will also promote greater access to data and information. “One of the lessons of COVID-19 is that world needs a significant leap forward in data analysis to help leaders make informed public health decisions,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “This requires harnessing the potential of advanced technologies such as artificial intelligence, combining diverse data sources, and collaborating across multiple disciplines. Better data and better analytics will lead to better decisions.” read the release at the WHO website at https://www.who.int/news/item/05-05-2021-who-germany-launch-new-global-hub-for-pandemic-and-epidemic-intelligence also useful to read the note on the UN website about the same https://news.un.org/en/story/2021/05/1091332

|
Scooped by
nrip
May 4, 2021 3:39 AM
|
Communicable diseases including COVID-19 pose a major threat to public health worldwide. To curb the spread of communicable diseases effectively, timely surveillance and prediction of the risk of pandemics are essential. The aim of this study is to analyze free and publicly available data to construct useful travel data records for network statistics other than common descriptive statistics. This study describes analytical findings of time-series plots and spatial-temporal maps to illustrate or visualize pandemic connectedness. We observed similar patterns in the time-series plots of worldwide daily flights from January to early-March of 2019 and 2020. A sharp reduction in the number of daily flights recorded in mid-March 2020 was likely related to large-scale air travel restrictions owing to the COVID-19 pandemic. The levels of connectedness between places are strong indicators of the risk of a pandemic. Since the initial reports of COVID-19 cases worldwide, a high network density and reciprocity in early-March 2020 served as early signals of the COVID-19 pandemic and were associated with the rapid increase in COVID-19 cases in mid-March 2020. The spatial-temporal map of connectedness in Europe on March 13, 2020, shows the highest level of connectedness among European countries, which reflected severe outbreaks of COVID-19 in late March and early April of 2020. The analysis can facilitate early recognition of the risk of a current communicable disease pandemic and newly emerging communicable diseases in the future. read the study at https://publichealth.jmir.org/2021/3/e27317

|
Scooped by
nrip
May 2, 2021 11:01 PM
|
National governments worldwide have implemented non-pharmaceutical interventions to control the COVID-19 pandemic and mitigate its effects.
Objective: The aim of this study was to investigate the prediction of future daily national confirmed COVID-19 infection growth—the percentage change in total cumulative cases—across 14 days for 114 countries using non-pharmaceutical intervention metrics and cultural dimension metrics, which are indicative of specific national socio-cultural norms.
Methods: We combined the Oxford COVID-19 Government Response Tracker data set, Hofstede cultural dimensions, and daily reported COVID-19 infection case numbers to train and evaluate five non–time series machine learning models in predicting confirmed infection growth.
We used three validation methods—in-distribution, out-of-distribution, and country-based cross-validation—for the evaluation, each of which was applicable to a different use case of the models.
Results: Our results demonstrate high R2 values between the labels and predictions for the in-distribution method (0.959) and moderate R2 values for the out-of-distribution and country-based cross-validation methods (0.513 and 0.574, respectively) using random forest and adaptive boosting (AdaBoost) regression.
Although these models may be used to predict confirmed infection growth, the differing accuracies obtained from the three tasks suggest a strong influence of the use case.
Conclusions: This study adds to the rapidly growing body of work related to predicting COVID-19 infection rates by introducing an approach that incorporates routinely available data on NPIs and cultural dimensions. Importantly, this study emphasizes the utility of NPIs and cultural dimensions for predicting country-level growth of confirmed infections of COVID-19, which to date have been limited in existing forecasting models. Our findings offer a new direction for the broader inclusion of these types of measures, which are also relevant for other infectious diseases, using non–time series machine learning models. Our experiments also provide insight into validation methods for different applications of the models.
read the entire study at https://www.jmir.org/2021/4/e26628

|
Scooped by
nrip
May 2, 2021 12:37 PM
|
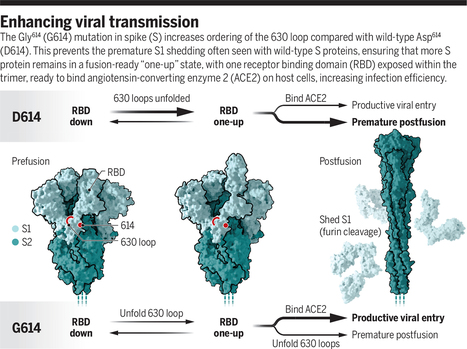
Viruses need entry proteins to penetrate the cells where they will replicate. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) version is called the spike or S protein. The S protein, also the target of the current vaccines, is quickly adapting to its new human hosts. It took its first major step in this direction early in 2020, when its amino acid 614 (of 1297) changed from an aspartic acid (D) to a glycine (G). Viruses bearing this D614G mutation transmit among humans more rapidly and now form the majority in circulation. On page 525 of this issue, Zhang et al. (1) use careful structural analyses to reveal how D614G changed the S protein to accelerate the pandemic. The work of Zhang et al. also reveals more about the natural history of the virus. The notable emergence of D614G suggests that the acquisition of a destabilizing furin site was a recent event. The virus could easily lose this site, as it does frequently in cell culture systems, implying that it in some way facilitates human transmission. This is not a conclusion that most students of human coronaviruses would have anticipated, given that SARS-CoV-1, which transmits with reasonable efficiency, lacks this site, whereas the more distantly related MERS coronavirus bears this site and transmits poorly. How the SARS-CoV-2 furin site promotes new human infections remains a key open question in the field. read the entire article at https://science.sciencemag.org/content/372/6541/466

|
Scooped by
nrip
April 23, 2021 1:26 PM
|
Several new viral respiratory tract infectious diseases with epidemic potential that threaten global health security have emerged in the past 15 years. In 2003, WHO issued a worldwide alert for an unknown emerging illness, later named severe acute respiratory syndrome (SARS). The disease caused by a novel coronavirus (SARS-CoV) rapidly spread worldwide, causing more than 8000 cases and 800 deaths in more than 30 countries with a substantial economic impact. Since then, we have witnessed the emergence of several other viral respiratory pathogens including influenza viruses (avian influenza H5N1, H7N9, and H10N8; variant influenza A H3N2 virus), human adenovirus-14, and Middle East respiratory syndrome coronavirus (MERS-CoV). In response, various surveillance systems have been developed to monitor the emergence of respiratory-tract infections. These include systems based on identification of syndromes, web-based systems, systems that gather health data from health facilities (such as emergency departments and family doctors), and systems that rely on self-reporting by patients. More effective national, regional, and international surveillance systems are required to enable rapid identification of emerging respiratory epidemics, diseases with epidemic potential, their specific microbial cause, origin, mode of acquisition, and transmission dynamics.

|
Scooped by
nrip
April 21, 2021 12:51 AM
|
Simple in structure but advanced in function, viruses exist in a category that lies between the inert and the living. Slightly ovoid in shape and somewhat blurred at the edges, the black splotches were scattered across a mottled gray background, looking much like a postmodern painting. At a meeting of the Medical Society of Berlin in 1938, Helmut Ruska, a German physician and biologist, was presenting the first images ever seen of virus particles. The splotches were members of the poxvirus family, specifically ectromelia, visualized directly in the lymph fluids of infected mice. Thanks to the invention of the electron microscope, then known as the Übermikroscop, scientists could finally observe—actually see—what was already known to exist: the minuscule and mysterious world of viruses. Ruska’s brother, Ernst, a physicist, had built the first prototype of the instrument while completing his Ph.D., but Helmut saw the device’s potential application to the field of biology. Helmut and his colleagues went on to gather nearly 2,000 black-and-white images by the end of 1939. Their collection included a variety of pathogens known to infect humans and plants, including the variola virus (which causes smallpox) and tobacco mosaic virus (the first virus ever discovered). Just over 80 years later, scientists published the first images of SARS-CoV-2, the novel virus that causes COVID-19. To reveal its iconic spike protein, they used an instrument similar to Ruska’s. The black-and-white images visually confirmed that this was a member of the coronavirus family, enabling scientists around the world to begin drawing upon existing knowledge of such viruses from years of prior research. Scientists were able to directly observe this new virus soon after a cluster of patients in China was diagnosed in late December 2019 with a pneumonia of unknown cause. By March 2020, COVID-19 had been declared a pandemic by the World Health Organization. Events moved far more slowly in previous pandemics. The Black Death pandemic in the mid 1300s killed more than one-third of Europe’s population in four years, without anyone knowing what caused it. By the time of the 1918 flu pandemic, scientists understood the disease’s cause but couldn’t see the virus or test for it. When SARS-CoV-2 emerged, the value of basic science research conducted many decades earlier became quickly evident in the form of innovative tools for virus detection. Researchers can now sequence novel viruses and study their genomes, but even so the electron microscope continues to offer a unique “open” view of such pathogens. There may be more viruses than there are stars in the universe. Basic science research being conducted today will play a critical role in helping us to understand their past, present, and future—and better prepare us for the emergence of still more novel viruses. read the entire essay at https://nautil.us/issue/99/universality/the-vast-viral-world-what-we-know-and-dont-know

|
Rescooped by
nrip
from healthcare technology
April 14, 2021 9:48 AM
|
A model has been developed by researchers at Indian Institute of Technology ,Kharagpur predicting alteration in metabolic reaction rates of lung cells post SARS-CoV-2 infection.
"We have used the gene expression of normal human bronchial cells infected with SARS-CoV-2 along with the macromolecular make-up of the virus to create this integrated genome-scale metabolic model. The growth rate predicted by the model showed a very high agreement with experimentally and clinically reported effects of SARS-CoV-2," said Dr Amit Ghosh, Assistant Professor, School of Energy Science and Engineering, IIT Kharagpur who coauthored the paper The research would lead to a better understanding of metabolic reprogramming and aid the development of better therapeutics to deal with viral pandemics, Summary: Metabolic flux analysis in disease biology is opening up new avenues for therapeutic interventions. Numerous diseases lead to disturbance in the metabolic homeostasis and it is becoming increasingly important to be able to quantify the difference in interaction under normal and diseased condition. While genome-scale metabolic models have been used to study those differences, there are limited methods to probe into the differences in flux between these two conditions. Our method of conducting a differential flux analysis can be leveraged to find which reactions are altered between the diseased and normal state. We applied this to study the altered reactions in the case of SARS-CoV-2 infection. We further corroborated our results with other multi-omics studies and found significant agreement. read the paper at https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1008860
|

|
Scooped by
nrip
May 9, 2021 9:57 AM
|
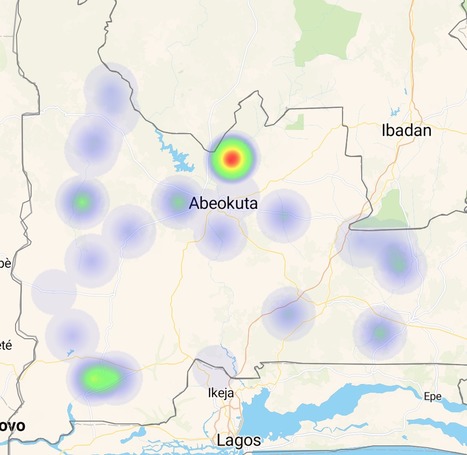
The COVID-19 pandemic consistently demonstrated a pattern of growing community transmission worldwide, even with the adoption of social distancing measures (lockdown or voluntarily shelter in place) in January and early May 2020. The continuing transmission of the virus despite the policy measures adopted in some countries was an important point of debate and investigation in the scientific community and among authorities. Unexpected forms of transmission (atmospheric) associated with the social distancing policy became the central question for the infectious transmission modeling of SARS-CoV-2 and predictive methods. Daily new COVID-19 cases from January to April 2020 demonstrate varying patterns of SARS-CoV-2 transmission across different geographical regions. China and South Korea successfully and quickly flattened their COVID-19 curve. To understand why this was the case, this paper investigated possible aerosol-forming patterns in the atmosphere and their relationship to the policy measures adopted by select countries.
Objective: The main research objective was to compare the outcomes of policies adopted by countries between January and April 2020. Policies included physical distancing measures that in some cases were associated with mask use and city disinfection. We investigated whether the type of social distancing framework adopted by some countries (ie, without mask use and city disinfection) led to the continual dissemination of SARS-CoV-2 (daily new cases) in the community during the study period.
Methods: We examined the policies used as a preventive framework for virus community transmission in some countries and compared them to the policies adopted by China and South Korea. Countries that used a policy of social distancing by 1-2 m were divided into two groups. The first group consisted of countries that implemented social distancing (1-2 m) only, and the second comprised China and South Korea, which implemented distancing with additional transmission/isolation measures using masks and city disinfection. Global daily case maps from Johns Hopkins University were used to provide time-series data for the analysis.
Results: The results showed that virus transmission was reduced due to policies affecting SARS-CoV-2 propagation over time. Remarkably, China and South Korea obtained substantially better results than other countries at the beginning of the epidemic due to their adoption of social distancing (1-2 m) with the additional use of masks and sanitization (city disinfection). These measures proved to be effective due to the atmosphere carrier potential of SARS-CoV-2 transmission.
Conclusions: Our findings confirm that social distancing by 1-2 m with mask use and city disinfection yields positive outcomes. These strategies should be incorporated into prevention and control policies and be adopted both globally and by individuals as a method to fight the COVID-19 pandemic.
read the study at https://publichealth.jmir.org/2021/4/e20699/

|
Scooped by
nrip
May 9, 2021 3:50 AM
|
The Centers for Disease Control and Prevention (CDC) warned in a document published Friday of "repeatedly documented" instances of coronavirus spreading through the air to people more than 6 feet away under certain conditions. The new document explaining the latest understanding of how the virus spreads is part of a shifting emphasis towards airborne transmission of the virus. "Transmission of SARS-CoV-2 from inhalation of virus in the air farther than six feet from an infectious source can occur," the new document says in large letters, while noting it is "less likely than at closer distances." Some experts have been pushing the CDC for months to place a greater emphasis on airborne transmission and the need to improve ventilation, even with something as simple as opening the window in a room. Experts have also long said that outdoors is far safer than indoors. The CDC acknowledged last year that the virus can spread through airborne transmission, but there has since been a growing emphasis on that method of transmission. The agency emphasized that while it is updating its understanding of how the virus spreads, the same methods for keeping safe still apply. Wearing a mask, distancing from others, avoiding crowded indoor areas and allowing adequate ventilation are recommended. read the story at https://thehill.com/policy/healthcare/552406-cdc-warns-virus-can-spread-more-than-six-feet-under-certain-conditions

|
Scooped by
nrip
May 3, 2021 12:50 AM
|
The spread of SARS-CoV-2, originating in Wuhan, China, was classified as a pandemic by the World Health Organization on March 11, 2020. The governments of affected countries have implemented various measures to limit the spread of the virus. The starting point of this paper is the different government approaches, in terms of promulgating new legislative regulations to limit the virus diffusion and to contain negative effects on the populations. Objective: This paper aims to study how the spread of SARS-CoV-2 is linked to government policies and to analyze how different policies have produced different results on public health.
Methods: Considering the official data provided by 4 countries (Italy, Germany, Sweden, and Brazil) and from the measures implemented by each government, we built an agent-based model to study the effects that these measures will have over time on different variables such as the total number of COVID-19 cases, intensive care unit (ICU) bed occupancy rates, and recovery and case-fatality rates. The model we implemented provides the possibility of modifying some starting variables, and it was thus possible to study the effects that some policies (eg, keeping the national borders closed or increasing the ICU beds) would have had on the spread of the infection.
Conclusions: In line with what we expected, the obtained results showed that the countries that have taken restrictive measures in terms of limiting the population mobility have managed more successfully than others to contain the spread of COVID-19. Moreover, the model demonstrated that herd immunity cannot be reached even in countries that have relied on a strategy without strict containment measures.
read the study at https://medinform.jmir.org/2021/4/e24192

|
Scooped by
nrip
May 2, 2021 10:53 PM
|
Sentinel surveillance of influenza-like illness (ILI) in Egypt started in 2000 at 8 sentinel sites geographically distributed all over the country. In response to the COVID-19 pandemic, SARS-CoV-2 was added to the panel of viral testing by polymerase chain reaction (PCR) for the first 2 patients with ILI seen at one of the sentinel sites. We report the first SARS-CoV-2 and influenza A(H1N1) virus co-infection with mild symptoms detected through routine ILI surveillance in Egypt.
This report aims to describe how the case was identified and the demographic and clinical characteristics and outcomes of the patient.
Conclusions: This case highlights the possible occurrence of SARS-CoV-2/influenza A(H1N1) co-infection in younger and healthy people, who may resolve the infection rapidly. We emphasize the usefulness of the surveillance system for detection of viral causative agents of ILI and recommend broadening of the testing panel, especially if it can guide case management.
read the paper at https://publichealth.jmir.org/2021/4/e27433

|
Scooped by
nrip
April 27, 2021 1:01 AM
|
The authors propose that it is a scientific error to use lack of direct evidence of SARS-CoV-2 in some air samples to cast doubt on airborne transmission while overlooking the quality and strength of the overall evidence base. There is consistent, strong evidence that SARS-CoV-2 spreads by airborne transmission. Although other routes can contribute, the authors believe that the airborne route is likely to be dominant. The public health community should act accordingly and without further delay. Summary: If an infectious virus spreads predominantly through large respiratory droplets that fall quickly, the key control measures are reducing direct contact, cleaning surfaces, physical barriers, physical distancing, use of masks within droplet distance, respiratory hygiene, and wearing high-grade protection only for so-called aerosol-generating health-care procedures. Such policies need not distinguish between indoors and outdoors, since a gravity-driven mechanism for transmission would be similar for both settings. But if an infectious virus is mainly airborne, an individual could potentially be infected when they inhale aerosols produced when an infected person exhales, speaks, shouts, sings, sneezes, or coughs. Reducing airborne transmission of virus requires measures to avoid inhalation of infectious aerosols, including ventilation, air filtration, reducing crowding and time spent indoors, use of masks whenever indoors, attention to mask quality and fit, and higher-grade protection for health-care staff and front-line workers. Airborne transmission of respiratory viruses is difficult to demonstrate directly. Mixed findings from studies that seek to detect viable pathogen in air are therefore insufficient grounds for concluding that a pathogen is not airborne if the totality of scientific evidence indicates otherwise. Decades of painstaking research, which did not include capturing live pathogens in the air, showed that diseases once considered to be spread by droplets are airborne. Ten streams of evidence collectively support the hypothesis that SARS-CoV-2 is transmitted primarily by the airborne route.

|
Scooped by
nrip
April 23, 2021 1:14 PM
|
More than two dozen virologists, epidemiologists, and others responded to STAT's question about what they still most wanted to know. In the 16 months since the SARS-CoV-2 virus burst into the global consciousness, we’ve learned much about this new health threat. People who contract the virus are infectious before they develop symptoms and are most infectious early in their illness. Getting the public to wear masks, even homemade ones, can reduce transmission. Vaccines can be developed, tested, and put into use within months. As they say, where there’s a will, there’s a way. But many key questions about SARS-2 and the disease it causes, Covid-19, continue to bedevil scientists. What accounts for the wide variety of human responses to this virus? How much immunity is enough immunity? How often will reinfections happen and what will they be like? how long will immunity last? How are viral variants going to impact the battle against Covid-19? What is long Covid, who is at risk of developing it, and can it be prevented? What’s the deal with Covid and kids? How big a role do asymptomatically infected people actually play in SARS-2 transmission? What does the future hold for SARS-2, evolutionarily and otherwise? Can we figure out who might become a superspreader? Can we learn more quicker from the study of the genetic sequences of SARS-2 viruses? What is the impact of the nonpharmaceutical interventions? What are the barriers to compliance of proven public health interventions and how can that problem best be addressed? what are yhe differences between SARS-2 and its older cousin, SARS-1 Where did SARS-2 come from? Read more at https://www.statnews.com/2021/04/20/we-know-a-lot-about-covid-19-experts-have-many-more-questions/

|
Scooped by
nrip
April 14, 2021 9:59 AM
|
Research into how some HIV-positive people keep the virus at bay promises to yield new treatment possibilities, from vaccines to gene therapies Since the early 1990s, case studies had begun to emerge of patients who tested positive for HIV, but displayed no symptoms, and were later found to have extremely low levels of the virus in their bodies. The general consensus among the medical community was that these were freak incidents, and the patients were fortunate enough to have been infected with a faulty strain of HIV, which contained mutations preventing it from replicating itself. Over the following decade Joel Blankson ran a series of experiments to test his idea that there might be something special about these people that enabled their immune system to suppress HIV. He found it that the virus within them was perfectly fine. It was the patients that were special.More than 20 years on, we now know that a small proportion of HIV patients can naturally suppress the virus, and thus avoid developing symptoms, without requiring medication. Scientists call these people elite controllers, and while they make up less than 0.5% of the 38 million HIV-infected people on the planet, they represent the forefront of research into the disease. The concept of viral control exists for almost all infectious diseases, with asymptomatic Covid-19 patients being another example of elite controllers. For most common viruses such as the Epstein-Barr virus, which is present in more than 90% of people around the world, the majority of people are controllers, and it is only a small proportion of vulnerable individuals who cannot suppress it. However, HIV is a particularly exceptional case. Unlike for Epstein-Barr, HIV controllers are the exceptions, not the rule.
The reason why HIV elite controllers are so interesting is that while antiretrovirals can help the other 99.5% of HIV patients suppress the virus, these drugs have to be taken for life, and are toxic to the body. It is common for patients to develop liver damage and even heart disease, and if they stop the therapy, reservoirs of HIV genomes hiding out in various cells and tissues spring to life again, flooding the bloodstream within weeks. But understanding how elite controllers manage to keep HIV at bay may yield a wealth of new treatment possibilities. From vaccines that can boost the immune response in people newly infected with HIV, to gene therapies that can help put the virus into a permanent deep sleep, these approaches aim to share the secrets of elite controllers with the rest of the HIV-infected population. Read the original article at https://www.theguardian.com/society/2021/apr/04/the-elite-controllers-who-can-naturally-suppress-hiv

|
Scooped by
nrip
April 1, 2021 12:45 AM
|
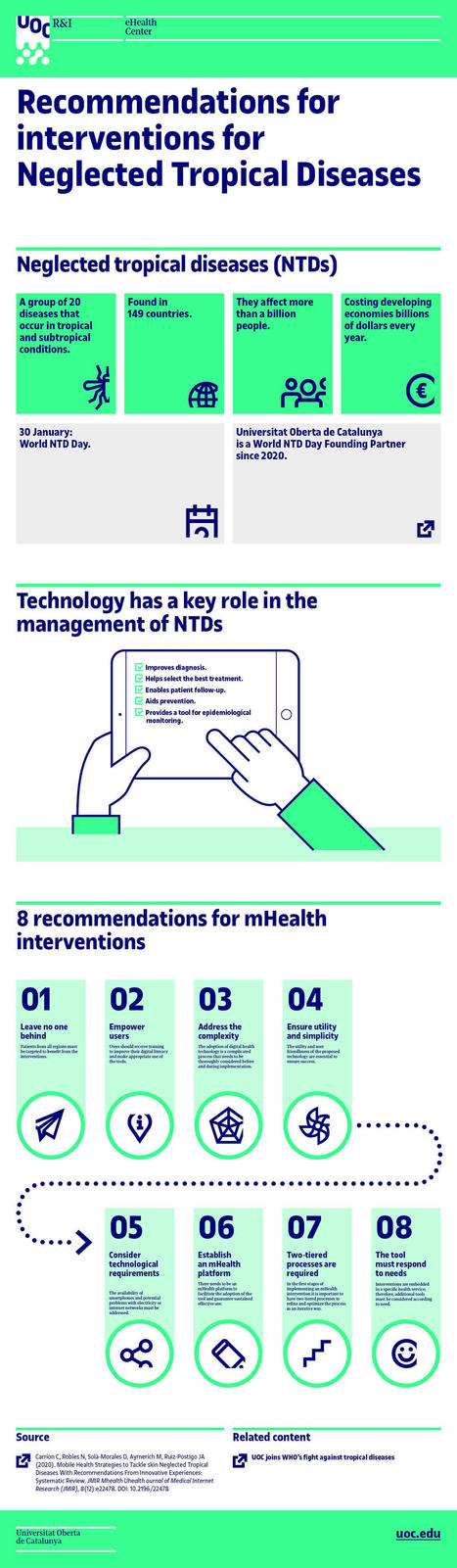
Neglected tropical diseases affect more than a billion people and cause hundreds of thousands of deaths every year. In spite of this, most people still know very little about them. A study performed by the Universitat Oberta de Catalunya (UOC) provided eight recommendations for improving the online technology to help with the treatment and diagnosis of neglected tropical diseases (NTDs). The goal was to standardize and improve the apps developed for controlling and monitoring neglected tropical diseases of the skin. The analysis was performed by UOC researchers Carme Carrion and Marta Aymerich from the eHealth Lab and Noemí Robles from the eHealth Center, together with José Antonio Ruiz Postigo from the World Health Organization and Oriol Solà de Morales from the Health Innovation Technology Transfer Foundation. In the study, the authors looked at the context of the existing apps and identified their weaknesses. The recommendations are outlined in the infographic prepared by the UOC eHealth Center, which is attached with this post. The recommendations provide an initial base for improving the efficiency in the development and social uptake of apps designed for the control and treatment of NTDs. These recommendations are summarized in eight points : - Nobody should be left out: patients from all regions should be selected to benefit from the proposed interventions. This requires translating the tools into different languages.
- Users must have control: the interventions' end users (health professionals and patients) must be given sufficient training to improve their digital literacy and make effective use of the tools that are provided.
- Complexity must be adequately catered for: integrating e-health-related technology is a complicated process that should be considered in depth both before and during implementation.
- Utility and simplicity must be there, and, what is more, they must be seen: health professionals, patients and healthy citizens must be able to understand the proposed technology's utility and ease of use. In other words, it must be a facilitator, not a barrier.
- The technological requirements must be considered from the beginning: the availability of adequate mobile devices, the potential problems with electricity supply or internet networks, and other technical issues must be considered as part of a comprehensive strategy with a specific objective.
- A long-term m-health platform must be established: an m-health intervention's success depends on the existence of a platform that makes it easier not only to implement the tool but also guarantees its sustained, effective use.
- Split-level processes are required to improve: in the early stages of implementation of an m-health system, the processes must be divided into two levels in order, first, to refine the process and, then, to optimize it iteratively.
- The tool must meet the stated needs: interventions are integrated in a specific health service; accordingly, additional tools should be considered as required.
read more at https://medicalxpress.com/news/2021-01-apps-neglected-tropical-diseases.html
|



 Your new post is loading...
Your new post is loading...