 Your new post is loading...
 Your new post is loading...
For the previous five years I have been treating Troy for the injuries he sustains playing soccer/football. Troy is more prone to injury. And unless he's very diligent with his rehab, the more injuries he endures, the more inclined he is to sustain new ones. This is because of the “flow on effect that happens when a body part is not sufficiently mobile or strong to control the forces involved in the client’s chosen activity. Science based chiropractic injury specialist, Dr. Alexander Jimenez discusses the study. Troy plays goalkeeper, for which he must move quickly in any way after long periods of relative inactivity. He takes goal kicks, which require him to create large amounts of muscular torque, too frequently after comparatively relaxed intervals. In one match, Troy hurt his right quadriceps muscle after a goal kick really early on -- but he had, he promised me, warmed up before the beginning. Of interest was what Troy reported had been happening in the days before the game. He has a sedentary occupation, and he'd had some low back pain in the previous week. This was likely postural pain caused by a poor sitting position, but in these cases of prolonged sitting plus pain, I am always curious to look at what might be going on with the muscular system. Then, on the day of the game, Troy had undertaken a two-hour car travel, coming only 30 minutes before the warm up. Following The TrailThe kicking action deploys muscles which stabilize the back, foot and knee together with the ones that provide the power for the approach and kicking of the ball. Since Mark Alexander has reported, the kicking action follows a certain timing and specificity of muscle recruitment. One of people who have lower back pain, one quite common muscular imbalance is that the failure to recruit gluteus maximus at the right time (if at all), in its function of stretching the hip and strengthening the pelvis when standing on one leg. The part of psoas major can be to keep the normal lordosis of the lower spine, especially when people are sitting, but also to stabilize the front of the hip joint to prevent injuries such as labral tears. On the football pitch, it is also very active in the approach to the ball and also the effect phase of the kicking action. It is reasonable to assume that the hip flexors may reflexively shorten if they are weak or not able to work throughout their whole selection. Table 1 shows which muscles may overwork or compensate for the reduction of activation of those stability muscles. In case the psoas is feeble, the athlete may over-recruit rectus femoris to flex the hip, putting extra load with this muscle. What's more, if the hip flexor doesn't have adequate length, it cannot be properly lengthened in the preparation stage of the kick. This may lead to inadequate coordination of the through swing, resulting in poor performance -- and potentially injury. This was certainly the mechanism behind Troy's muscle injury, as Table 2 shows. Troy was unable to stand on one leg for any length of time, especially when he had to swing the opposite leg, as from the kicking action. Correction of this was all a part of his house exercise program. I originally gave him exercises only to trigger the gluteals while lying supine, then standing and sitting. Then we progressed this into the stance leg at the kicking actions. Gluteal exercises1. Single leg stance glute activation • Stand on affected side with good alignment and contract gluteals • Perform three sets of 10 contractions, holding for 10 seconds each time. The athlete should not recruit the hamstring or adductors, but keep them relaxed. 2. Single leg stability against contralateral movement (Fig 1) • Keeping stance knee facing forwards, turn contralateral side of pelvis away and back (counter and clockwise hip rotation) towards the front, using the gluteals. This strongly isolates gluteus medius on stance (affected) leg. • Perform three sets of 10 reps under control. 3. Hip flexor strengthening (Fig 2) • Loop x-band around ankle with weak hip flexor; secure the other end behind client. • Standing on opposite leg, flex hip against the band resistance. • Return leg, keeping it bent so that the foot stays off the ground, and repeat the raise. • Avoid hitching hip on swing leg side. • Perform three sets of 10 reps. The principle which you're only as strong as the weakest link is indeed true here. Troy sustained the rectus femoris strain because of muscular weaknesses away from the injury site. Core muscle control is essential for all sports and it ought to be prioritized in every athlete's health program. It must also be specific to the sport: that is, speed and direction-specific. So that the therapist needs sound understanding of the technical aspects of the client's game and has to relate that back into the joint range and muscular control needed to reduce injury episodes and enhance functionality. In the end, a drop-off in performance is often the first warning sign that something's wrong.
Aaron was a final-year high school student and keen soccer referee. Complaining of mid-back pain, especially after he had refereed three or even four matches in a single day (which he often did). He experienced this same pain when he was sitting studying, but it was more prevalent after refereeing. He also advised me his quadriceps appeared to fatigue a whole lot more than the rest of his muscles after running around a whole lot. Scientific spine specialist, Dr. Alexander Jimenez takes a look at the case. My first assessment of Aaron's spinal posture was that he was quite kyphotic (bent forwards) through his torso, with accompanying cervical spine flexion -- in sitting he simply flexed forward all the way through his spine. He experienced his mid-back pain when he strove to extend or straighten himself up, so when he corrected his stance that the pain came on. The erector spinae muscles in their own mid-back proved very developed and seemed like thick ropes. When I assessed Aaron's lumbo-pelvic stability, things got really interesting. I was seeking the way gluteus maximus and the psoas major muscles were performing, each of which help to control the impartial position of the pelvis under load. He'd shake all around the area. To assess psoas major, I asked Aaron to sit and control the natural arch in his low back (neutral posture) as he lifted and hauled his bent leg in flexion past 90° (just an easy knee elevator). He was not able to maintain the leg even slightly off the floor without slipping together with his low back. Finally I asked him to stand on one leg and feel the gluteal muscle activating on that side, while swinging the other leg through as if he were running. Initially he couldn't trigger his gluteal muscles without a great deal of concentration. When he tried to perform the leg swings without moving his anus, he almost fell over. The runner needs to have quite an upright posture, letting the upper body to flex forward slightly, but not too much. The gluteus maximus gives a small amount of hip extensor muscle torque but much more importantly, it controls the upright position of the pelvis on the hip. Without this the body would just bend ahead. Isolated hip flexion is also necessary, in order that the lower back is kept in its neutral arch when the runner initiates the swing phase. As soon as I examined Aaron's running posture, he had been very flexed at the hip, almost leaning over at about a 25° angle. He was managing to maintain his lower back neutral, however, the erector spinae muscles were working extremely hard in this place. He explained that he could feel this occurring and was hoping to liven up -- but he'd been doing this through his chest. This overuse of the erector spinae muscles are what had led to his growing mid-back pain. The thoracic spine is affected substantially by the placement of the spinal column in all positions, from sitting postures to swinging a golf club, throwing a ball or running. The mid-back requires a stable platform in the lumbar spine where to execute its freedom functions. This is especially important in throwing sports but is also crucial in activities like swimming. Thoracic spine motion in running should mainly involve rotation as this helps to counterbalance the hip flexion moment produced at the opposite hip. Over-activity at the thoracic extensors is counterproductive not only for performance but also for injury. TreatmentBut we also needed to correct the pelvic muscle weaknesses that were acting on the thoracic spine and hip. I instructed Aaron to stand and operate tall throughout his hip place, with his gluteals, to take the load off the thoracic erector spinae. To be able to strengthen the gluteals so that they were up to the job, I made him to carry out the one legged bridges (see Figure 1). And in standing, I tied a piece of tubing around the ankle of one leg, and that he then utilized to mimic the running swing phase while he concentrated on keeping his pelvis fairly still on his stance leg (see Figure 2). We also needed to tackle the quadriceps muscle fatigue. My theory here was that he was overusing his quads as a consequence of poor hip flexion when running. Insufficient hip flexion and upward drive would generate a shallow swing stage. This would cause one to plant his foot early, creating a braking kind of activity which forcibly ceased ahead propulsion of the body. It was like he had been thumping down on the floor with each step rather than maintaining forward momentum. Aaron's symptoms eased up quite quickly once he managed to fix his functioning posture and recruit his stabilizing muscles. I encouraged him to continue his exercises for the next six to eight months so that he would fully integrate the muscular recruitment routines into his running technique.
This case study focuses on the Australian over-105kg weight-lifter Damon Kelly, who injured his left shoulder, which he had jarred while performing a mis-timed snatch. Injury scientist, Dr. Alexander Jimenez takes a look at the case. In the snatch movement, the bar must be lifted above the head to full arm extension at one continuous rapid movement. The weight-lifter should then be held steady until the judges have accepted the lift. While practicing, Damon had captured the pub just too far behind his head, causing a slight "shift within his gleno-humeral joint along with a sharp pain. He immediately dropped the bar and had been resting almost completely from the grab component of his training. Damon currently presented with "stiffness" and pain, largely on reaching across his body (horizontal flexion) along together with his hands behind his back (complete operational internal rotation). All stationary muscle tests were negative, and also his shoulder elevation was ordinary, much to my relief. He reported being able to perform shoulder press with no pain in any way, even in a moderately heavy load for him. He was, however, getting some pain with the grab position under load, and was quite apprehensive about this (it felt "weak in that position). I have generally found that the Queensland weight-lifters I've looked after over the years are utilized to training with pain and have very low anxiety over injury. They are specialists at load- modification and development, appreciate strongly the value of correct technique, and the majority of them understand training periodization fairly intuitively. My provisional identification was a rotator cuff "strain , using a minimum likelihood of this weight-lifter really having ripped any tendon fibers. Posterior impingement of the rotator cuff at the glenoid was a distinct possibility -- hypothetically the pain at the posterior rotator cuff may have been solely due to compressive forces and consequent tendon impingement, maybe not overstrain/ overload at end of scope. There was also a distinct possibility that he had experienced a small anterior subluxation occasion in the snatch position, but given how quickly it was resolving, and that he noted no parasthesia or clunking/ snapping feelings at the joint, I believed that this was unlikely. Feelings of "instability in the snatch position might have had less to do with any disruption to the normal capsuloligamentous restraints into the joint than using inhibition of the rotator cuff (especially the medial rotator, subscapularis), for example that it couldn't hold the "ball as tightly in the socket as usual. The Way The Injury OccurredLet's picture what the position and load of the "snatch needs of the rotator cuff: • The humerus is nearly fully externally rotated, with the supraspinatus, infraspinatus and teres minor wrapping posteriorly under the head of humerus, and even towards the anterior-inferior aspect of the ball. • The subscapularis forms the anterior dynamic barrier to the joint, extended to its full length and playing a critical eccentric role in preventing anterior shear and excessive posterior angulation of the humerus. • The scapula is fully upwardly rotated, elevated and posteriorly tilted. With the bar quickly being forced to grab position by a strong concentric contraction of the external rotators, and abruptly coming to sit above the mind in 1 rotational movement, the strength and timing of subscapularis suddenly having to generate a huge eccentric internal spinning force has to be impeccable. If the time is repeatedly poor, or if the external rotators have slowly become too tight (a common result of some number of training variables), then subscapularis might not perform its job quite nicely enough and the ball will slightly shear anteriorly from the socket. Within a untrained shoulder, an entire spectrum of damage is possible, the worst being anterior shoulder dislocation. TreatmentEmploying deep-tissue massage and trigger- point releases, stretching and dry needling, we focused on repeatedly attaining two effects during the following four weeks, so as to restore normal rotator cuff function in the snatch position: • The external rotators (infraspinatus, teres minor and supraspinatus) were released from excessive tension and tightness. We literally beat them into submission – which, with a guy as big as Damon, takes not a small amount of force! Each session of this treatment managed to clear his pain on horizontal flexion and internal rotation (hand behind back), indicating that the muscles were returning to a normal state of function and length. • We trigger-pointed the internal rotator (subscapularis) to activate it, to bring it to life from its relatively dormant state. Lying deep in the axilla, with overlying layers of superficial muscle and fascia, it is a real challenge to get into this muscle. • We prescribed general theraband exercises, mostly above head height, to activate the rotator cuff, especially subscapularis. This treatment -- subduing overactive external rotators and triggering a dormant subscapularis -- for me clinically forms a common routine in sport injury. Aiding ActivationOn the very first day I saw Damon, I began experimentation by having him hold the bar in the grab position with elastic tube tensioned to pull the bar back over his head behind him (see Figure 1). He found that this instantly gave him a feeling of "security together with his joint under load. The pull of the tubing enhances the stimulation of subscapularis, so it can be used to centralize the job of this gleno-humeral joint by neutralizing the rotational forces of the cuff. In effect it provides a boost to the less powerful or inhibited subscapularis. Damon continued to utilize the tubing for 3 weeks since he slowly increased his holding time in snatch standing and introduced the snatch movement with progressively increasing heaps. Then he used the tubing only during warm-up, and finally weaned himself off it entirely using a week to spare before his next contest. Trainers and gym-goers can certainly use the tubing concept themselves at bench press and shoulder press. First implement a standard shoulder press with the bar, then attach a moderate strength of tensioned tubing to pull the bar from beneath, and see how "smooth and "simple the press movement now feels. It's nearly as though the socket has abruptly been lubricated, as the load requirement for your external rotators is reduced, and the subscapularis has been requested to step up and function. It certainly worked for Damon Kelly, with nearly 200kg over his head.
Fatigue related to a diminished ability to make muscular effort as a result of impairment of the central nervous system and/or peripheral nervous system has commonly been referred to as 'neurological fatigue' (NF). El Paso, TX. Chiropractor Dr. Alexander Jimenez examines the data. NF will not only affect performance in the form of lowered muscle contraction force (see poorer and slower and less spring), but in addition it will lead to longer recovery times, bad sleep patterns as well as altered mood states. What's more, the inability to create voluntary muscle contraction appropriate for the demands of their physical requirement of this sport/activity can then cause injury. It is apparent that the cause of fatigue is complex, influenced by both occasions happening in the central nervous system (CNS) and the peripheral nervous system (PNS). CentralCentral fatigue is neural fatigue originating in the central areas of the nervous system such as the higher cortical areas in the brain, brain stem, spinal cord, or cranial nerves. The exact mechanism for CNS fatigue remains largely unknown but it appears that two primary kinds of central fatigue exist: 1. acute CNS fatigue may occur as a result of decreased reflex sensitivity and or less than optimal output from the motor cortex; 2. chronic CNS fatigue, on the other hand, is likely caused by increased inhibitory drive to the alpha motor neurons. Motivation and psychological states also have been linked to both acute and chronic CNS fatigue, but it is not known if that is a cause or effect relationship. It's generally accepted that acute bouts of exercise causing central fatigue require an average of 48 hours to completely recover from. Chronic central tiredness, however, might take much longer. The common practice amongst coaches is to use a 10-day recovery protocol of low-intensity training to reunite the nervous system into a state of balance and homeostasis. The need that's placed on the CNS is a product of both the volume and intensity of training. CNS fatigue can be brought on by performing a higher quantity of low-moderate intensity training or when compared to a low-moderate volume of high-intensity coaching. Insufficient reconciliation of work and rest intervals coupled with over-ambitious training will probably result in CNS fatigue. However, high-intensity training asserts more for CNS activity. The best way to think of the impact various actions have on the CNS possibly to put the mona continuum. The more intense something is (as a percentage of maximal work or speed), the lower the quantity which can be achieved until the CNS gets fatigued. Central fatigue is a tiredness different from peripheral fatigue (in the muscles themselves). Researchers have discovered that central fatigue is different in the so-called fatigue feeling brought on by physical (muscular) fatigue, and in fact is generated in a state that is not accompanied by physical exhaustion. This is something that is relatively new. External factors like lack of sleep, personal stress, sickness, bad diet, inadequate hydration, and genetics might also give rise to CNS fatigue, especially chronic fatigue. Serotonin levels in brain regions has been indicated as a potential causative factor in the growth of central nervous system exhaustion. It is not likely, however, that single neuro- transmitter levels are responsible for CNS fatigue. It's more probable that a combination of neurotransmitters and the boosters which directly controls CNS fatigue, like dopamine and noradrenaline. Meeuson et al (2006) propose that this revised central fatigue hypothesis implies that an increase in fundamental proportion of serotonin to dopamine is related to feelings of tiredness and lethargy, accelerating the onset of fatigue, whereas a low ratio favors improved performance through the upkeep of motivation and arousal. Possible manipulation of these neurotransmitter levels may then potentially enhance CNS recovery. Serotonin levels have been demonstrated to increase during intense exercise in conducting rats and also to remain high in the point of exhaustion (Meeuson 2007). Dopamine release is also elevated during exercise but appears to fall at tiredness, a response that may be important from the fatigue process. The rate neurotransmitter synthesis chiefly depend on the peripheral access to the amino acids tryptophan and tyrosine, with increased brain delivery raising dopamine and dopamine/ noradrenalin activity, respectively. It's been demonstrated that BCAA ingestion can limit the serotonin levels and tyrosine can increase dopamine/noradrenaline levels in the mind. Although tryptophan levels stay reasonably steady, the intake of large carbohydrate meals, immobilization and stress might cause transient increases in tryptophan levels (Davis 2000). Nybo (2010) states that exercise in hot surroundings challenges not just the cardiorespiratory and fluid foundation balance of their human, but in addition the brain is affected by heat. Exercise-induced hyperthermia is associated with CNS fatigue. Improving dopamine action has been demonstrated to counteract heat-mediated CNS fatigue and improve performance whereas preventing noradrenaline uptake has been shown to aggravate CNS fatigue. Peripheral (or Localized Fatigue)Although occasionally called muscular fatigue, peripheral nervous system fatigue (PNS) is still a sort of CNS fatigue since the CNS controls skeletal muscle function. Unlike central fatigue, however, PNS fatigue is localized into a given body site and tends to be found at the peripheral nerves, autonomic nerves (sympathetic and parasympathetic). There are several potential mechanisms for PNS fatigue, which range from the accumulation of inorganic Phosphate and H+, to the failure of the sarcoplasmic reticulum to release adequate Ca++ because of signaling problems from the T-tubules, to inadequate manufacture and release of Achetylcholine at the neuromuscular junction. Unlike in the case of CNS fatigue, each of these mechanisms are severe and should not produce long-term exhaustion. The truth is it is generally accepted that a span of 24 hours is enough to return the body to homeostasis after PNS fatigue. Factors Contributing To CNS FatigueTraining to collapse accelerates CNS fatigue (peripheral and central) negatively impacting muscular co-ordination. When training it's important to understand that your mind will probably recall the previous set or drill over any other. Therefore, the conventional burnout method, as an example in resistance training, leaves your nervous system remembering a light load that mostly taxed the slow-twitch fibers. This is bad news if it's done week in and week out since you'll lose your maximal strength levels in no time. Complicated Loading ParametersWithin a training program there are many different training variables and external factors that struggle for CNS activity. Using complicated pyramid sets, for instance, may be overly complicated for the CNS and as a result strength development won't be optimized. Excessive Amounts Of Speed trainingSpeed work may encourage CNS fatigue (peripheral and central) several hours after the session has ended. In an exercise-intensity continuum, speed training is the hardest on the CNS. Anything that involves maximal velocity and elevated levels of co-ordinated force (sprinters can use force into the floor up to four times their body weight) compete for CNS activity. It's important, therefore, to employ sufficient rest periods during a rate session for CNS recovery and restoration of high-energy phosphates. Non-Training FactorsIt's well known that external factors like lifestyle stress, work pressure, family stress, poor sleep, alcohol and poor diet all contribute to exhaustion in the athlete. These hormones operate mostly at the system level -- muscle, skin, bone, tendon, heart, lung etc.. However, it is also likely that these hormones affect the integrity of the nervous system, both peripheral and central. Signs Of CNS FatigueThere are some obvious and recognizable signs that may indicate that athlete is experiencing neural fatigue. - Lack of motivation
- Poor memory
- Poor mood states
- Cognitive impairments
- High perceived exertion
- Impaired co-ordination
- Inhibition of central drive to muscles
- Heavy footsteps, a sign of central fatigue
- Impaired grip strength
- 10.Muscle twitches – particularly around the eyes and face
Objective Measures Of CNS FatigueThe commonly used measures which are simple to execute and also provide objective comparable data are: 1. Standing long jump. With feet placed together on a 0cm marker, the athlete leaps as far as possible in a horizontal direction. The measure is then taken. Typically most athletes, depending on sport and the ratio of fast-twitch to slow- twitch fibers, will achieve something around 2m as a standard long jump. These can be measured routinely, usually at the start of the week following a weekend competition, and an objective measure can be obtained. This gives the clinician a global interpretation of neuromuscular function. It may be a depressed PNS that results in poor motor output and thus a poor jump, or it could be accumulative and unrecovered muscle metabolite depletion. These tests can be compared to baseline tests that are done in non-fatigued states. 2. Watt bike power tests. On a stationary bike that has the capacity to measure power output (wattage), perform a simple 3-5 second blast as hard as possible. The best power output is measured in watts is then recorded. Again, these can be compared to baseline results. 3. Force platform jumps. If the equipment is available, then a force platform that measures impulse on a drop and jump can also be used as a measure of motor system excitability. This is measured as a time in contact and force output that provides the impulse measure. If the athlete is fatigued they may spend too long on the platform then the ratio of force to time drops. Similarly, the time in contact may stay the same; however, they may not produce the same force profile, again dropping the ratio. Preventing Or Fixing CNS FatigueFirst signs of central fatigue When someone is over-trained, 10 days of recovery utilizing low-intensity training and therapy are recommended. Training It is important during training (especially strength or speed training) to be aware that there is a huge difference between the 95th and 100th percentile of intensity. Athletes can still develop strength and speed significantly without training at 100%. Athletes may get hurt the next session after they’ve run a personal best (PB) on the track or hit a PB in the weights room: not just because they’re psyched up and trying to beat their PB, more because their CNS hasn’t recovered from the previous session. After strength PB, for example, there should be no attempt at the same PB for at least 10-12 days. Weekly planning There is a common misconception during team sport programs that it is the tactical training sessions that contribute the most to fatigue. However, in relation to the rationale behind the cause of CNS fatigue, team training sessions may be classed as having a moderate effect on CNS fatigue. This is because most of the work done in a team training session will be at moderate velocity speeds and force outputs when compared to speed or Olympic lifting. It is recommended that trainers should first have a look at their own training prescription and decide if there is too much (or too little) high-intensity CNS-fatiguing exercises. Only then can we start to criticize team training sessions. During the week, there has to be a balance between low and high-intensity training in relation to CNS fatigue. If two sessions are done in one day, try to make sure they are not both extremely taxing on the CNS. There also has to be a balance between high and low mental performances. High morale, disciplined sessions should be interchanged with more relaxed fun-type sessions. Know your exercises The higher the CNS demand of an exercise, the less volume or numbers should be done. For example, drop jumps are more CNS taxing than jumps up onto a box. Olympic lifts are more taxing than squats. Usually, any movement that involves more of a ‘shock’ will stress the CNS more. Know your athletes High-intensity training elements must compete for central nervous system energy. A novice sprinter can’t tax the CNS significantly no matter how hard he tries because he cannot output enough force, but as he improves the CNS demand rises exponentially, even if the volume of sprinting remains constant. This relays the importance of differentiating between advanced and novice athletes within a squad. Hot and cold showers To promote blood flow to the brain, hot and cold showers can accelerate CNS recovery. It is important, however, that the head is fully immersed under the shower during this treatment. Replenishment of muscle glycogen Carbohydrate feedings are usually taken immediately post-exercise in an attempt to re-fill depleted muscle glycogen stores. However, it may be more important to ingest carbohydrates at this time in an attempt to prevent CNS fatigue, as carbohydrates are the sole energy fuel for the brain. Recovery of protein balance After training, especially weight training or speed training, protein breakdown goes way up, thus creating a negative protein balance and a good potential for muscle loss. Although this eventually rebounds and the body goes into an anabolic state, in the time immediately following training, muscle can be lost. Since no athlete can afford muscle loss, this is an important focus for recovery and subsequent muscle gain. The protein can also accelerate entry of carbohydrates into the muscle cell. Supplements to combat CNS fatigue Some evidence exists showing that when neurotransmitters like acetylcholine, dopamine, and norepinephrine get depleted, physical and cognitive performance suffers. Since these neurotransmitters can be depleted from intense repeated bouts of strenuous exercise, this can be detrimental to the athlete. Since neurotransmitters can be depleted during exercise and this depletion can cause fatigue and over- training, nutritional strategies may offer some support. Decreased testosterone and increased cortisol is also an indicator of CNS fatigue and any dietary manipulation to increase testosterone levels is recommended. The following supplements are recommended: Tyrosine: Tyrosine also crosses the blood/ brain barrier and competes for the same receptor site as tryptophan (the body’s first line of performance inhibition). Tryptophan is a precursor for the fatigue promoting neurotransmitter, serotonin. To block out the sedating effects of tryptophan, tyrosine has to get there first so it is wise to take it before competition. Tyrosine may also help with dopamine and noradrenaline depletion. Branch Chain Amino Acids (BCAAs): BCAAs also suppress the uptake of tryptophan by the brain. They compete in a similar way as tryptophan for the same receptor site. Lecithin: Lecithin is a compound containing two fatty acids and choline. It's by far the most frequent phospholipid in your system. Phospholipids are cells forming a protective sheath around cells and providing to their own framework. As a supplier of choline, lecithin is needed to maintain cell membrane integrity and to facilitate the movement of fats in and out of cells, in addition to ions, wastes, and nourishment. Also, the neurotransmitter acetylcholine includes lecithin as a component. Due to its choline make-up, lecithin has been touted as a memory booster by improving cognitive function. Supplementation with lecithin may prevent the depletion of acetylcholine found with instruction. Since acetylcholine is energetic in promoting muscular force, memory and consciousness, this would offer both cognitive and performance advantages. Avena Sativa: Avena Sativa is a plant that has chemical properties that increase the levels of free testosterone in the body. Neural Fatigue & InjuryIf the neurological system is depressed (CNS or PNS) then the athlete may not be able to produce either a maximum muscle contraction that might result in poor torque generation around a joint, by way of instance, they might not have the ability to produce enough power to move the body from a standing start quickly enough. Not only will performance endure but also the joints that ought to stay secure and locked in the action of the movement (eg backbone) might also not have sufficient stiffness due to bad muscle recruitment to stabilize. The joints (back for instance) may subsequently suffer undesirable movement in the Shape of a shear force and this force might potentially harm the joint. What's more, if the system is still drained neurologically, the athlete may then suffer an accident (such as a pulled hamstring) if called upon to produce an explosive high-speed movement in training or competition. References
Brasil-Neto et al (1993) Postexercise depression of motor evoked potentials: a measure of central nervous system fatigue. Experimental Brain Research. 93; 181-184
Davis et al(2000) Serotonin and central nervous system fatigue: nutritional considerations. Am J Clin Nutr 2000;72(suppl): 573S–8S.
Davis et al(1997) Possible mechanisms of central nervous system fatigue during exercise. Med Sci Sports Exercise. 29(1); 45-57.
Nybo L (2010) CNS fatigue provoked by exercise in the heat. 1(2); 779-92.
Meeusen R and Watson P (2007) Amino acids and the brain: do they play a role in ‘central fatigue’? Int J Sports Nutr Exercise Metab. 17: supps S37-46.
Meeusen et al (2006) Central fatigue: the serotonin hypothesis and beyond. Sports Med. 36(10); 881-909.
In the last few years, there's been a steady growth in the popularity of minimalist running shoes, that claim to offer you the benefits of barefoot running without some of the drawbacks. Science based chiropractor, Dr. Alexander Jimenez investigates. It had been back in the late 1970s that the running boom really got underway. Since that time, tens of millions of individuals around the world have enjoyed recreational and competitive running, equally as a pastime and as means of getting and keeping healthy. However, as any clinician knows, the biomechanical demands of running are such that the prospect of injury is comparatively high in comparison to other endurance sports like swimming or biking. Not surprisingly, as a result, the growth in the popularity of running was accompanied by a growing number of accidents. It's hardly surprising, therefore, that the previous 3 decades has witnessed an explosion in running shoe technologies, together with successive generations of shoes with increasingly complex solutions to guarantee the ideal running gait along with the absorption of their impact forces, that are a particular difficulty when pounding the tarmac or pavements. Bearing this in mind, you might expect that the rate of injury suffered by runners per mile run has been steadily decreasing. However, studies on the prevalence of running-related accidents conducted from 1989 to the present have found a remarkably consistent rate of injury(1). In other words, despite all the technological advances in shoe development over these past decades, the rate of injury has held pretty steady. The Barefoot RevolutionIn more recent decades, some runners have taken a different approach by embracing quitting running. The proponents of barefoot running claim that this manner of running is much more 'natural' and enables the human foot to operate in the manner that Nature meant it to -- something that can't occur when the foot is shod in an artificial shoe. The claimed advantages of barefoot running revolve around the fact that an assessment of seasoned barefoot runners in comparison to shod runners reveals several striking (no pun intended!) differences. Most of these differences stem from the fact that barefoot runners typically land with a mid-foot strike (where the foot lands rather flatly) or forefoot strike (where the ball of the foot contacts the ground first and then the heel is lowered). This contrasts with the fact that 75% of shod runners land with a rear- foot strike in a heel-to-toe fashion(2). The significance of this fact is that the ground response impact forces generated from the collision of their foot together with the surface are typically much higher when a runner heel-strikes -- that the size of the peak impact force during rear-foot attack was shown to function as 1.5 -- 3 times your body weight(3). The use of a cushioned running shoe typically decreases this impact force by approximately 10%, which makes it more tolerable. But a far more effective approach to decrease the size of foot-strike impact forces would be to embrace a mid- or forefoot attack (see Figure 1). It follows that with no cushioning underfoot to decrease the effect of rear-foot attack, barefoot runners obviously embrace a mid- or - forefoot strike, which really turns out to be more effective at reducing impact forces, and so (according the proponents) reduces the risk of injury. Why is it that a mid- or - forefoot strike pattern can reduce the severity of ground impact forces in contrast to some rear-foot strike? Specifically, the researchers looked at the joint kinematics and influence absorption characteristics of the shoulder, hip and knee joints throughout rear-foot strike jogging, forefoot strike running and barefoot running. One of the primary findings was that in rear-foot strike, there was a significantly greater dependence on the knee and hip joints to absorb impact forces compared to barefoot and forefoot strike running. Specifically, the barefoot and forefoot runners demonstrated increased plantar- flexion at initial ground contact, which increased peak ankle energy absorption and decreased peak knee and hip power absorption. However, in both forefoot strike and barefoot running, the forces at initial contact are transmitted through the comparably smaller middle foot muscles and bones as opposed to throughout the calcaneus, talus and tibia straight, which could be a problem with a few runners. While a structurally sound foot may have the ability to consume these forces efficiently, it's very likely that different foot types may respond differently to these increased forces to the forefoot (see Box 1). Barefoot Benefits Or Barefoot Lies?The data on foot attack differences between shod and barefoot runners are widely accepted across the sports science and running community. What this mean concerning injury danger remains a topic of controversy, yet. Barefoot running proponents assert that (provided a slow transition is created) the introduction of barefoot running to a training program may diminish the risk of injury. But this is contested by a number of investigators. By way of example, Craig Payne, a senior lecturer at the Department of Podiatry at La Trobe University in Melbourne, commented at a recent paper: “The barefoot running community has an appalling track record at how they misinterpret, misuse and misquote research. The simple facts are that not one risk factor study on running injuries has linked high impacts to running injuries, yet the barefoot running community claim that the evidence shows this and consider high impacts as the cause of all injuries.(5)” Placing this argument to one side for the moment, there are some other, undeniable drawbacks to barefoot running. For instance, running barefoot on extremely hot pavements/tarmac or at extremely cold conditions may hurt the bottoms of the feet. Additionally, there are risks such as nails, glass, pebbles and other objects that could puncture the soles of feet or lead to stubbed toes. Moreover, even if heel strikes are eliminated by running barefoot, using shorter strides typically found in barefoot runners signifies the feet hit the floor more frequently -- what's gained by reducing the power of impact may be offset by the increase in the frequency of impacts. The evidence to date is that while barefoot running may provide some theoretical benefits concerning reducing foot strike effect by promoting a more mid/forefoot strike routine, there are incontrovertible disadvantages. In something of a halfway-house evolution, therefore, running shoe manufacturers have recently begun to offer so-called 'minimalist' running shoes. Minimalist shoes (sometimes referred to as 'barefoot shoes') have been designed to enable the foot to move through a similar selection and pattern of movement during running as could an unshod foot, while at exactly the exact same time offering some security. Others are slightly more considerable, being designed to help runners slowly transition from rear foot normally shod running to barefoot-style running. The Minimalist PromiseImplicit in the marketing behind minimalist shoes is your guarantee that (providing they are introduced very slowly) their usage will help runners to come up with a more natural working fashion, resulting in fewer injuries, a much more balanced musculature and much better running posture. However, what does the science say about these claims? Among the first studies into the use of minimalist sneakers compared the biomechanics of barefoot running with this of running in minimalist footwear and conventional running shoes(6). In the analysis, the mechanical qualities of this foot/shoe-ground port were investigated in eight experienced barefoot runners to be able to appraise the floor pressure supply, sagittal plane kinematics, and running market. The researchers also sought to discover if a minimalist shoe (Vibram Five Fingers) was effective in mimicking the experience of barefoot running and both these conditions were compared to the usage of conventional running shoes. As mentioned above, it turned out that, when compared with the standard shod condition, when running barefoot the athletes landed at more plantar flexion at the foot, which decreased impact forces and shifted stride kinematics. In particular, significantly shorter stride length, foot contact times, and higher stride frequency were observed. The usage of this Five fingers shoe also led to peak impact forces that were significantly lower than shod running, and much nearer to barefoot running. The lower limb kinematics with Five fingers was comparable to barefoot running, having a foot position which was significantly more plantar flexed than in conventional shoes. The researchers concluded: “The Five fingers shoe seems to be effective in imitating the barefoot conditions while providing a small amount of protection.” Another purported advantage of minimalist shoes is that they allow a more precise estimate of dynamic and static foot position in comparison to wearing a conventional cushioned running shoe. The theory is that this increased 'foot awareness' may help encourage a more efficient running motion, especially over undulating terrain. In a 2011 analysis, researchers looked at the effect of some five- minute minimal protection shoe on dynamic and static ankle position sense (again, Vibram Five fingers shoe) and compared it equally with a conventional shoe and also barefoot running(7). Static ankle joint position sense was assessed from the sagittal and frontal plane by asking fourteen experienced amateur runners to estimate the perceived direction and amplitude of a support incline surface plank placed under their right foot while standing. The energetic measures were performed with all the subjects running on a treadmill at 12kmh and requesting them to assess the treadmill surface slope. The results demonstrated that plantar flexion, dorsiflexion, eversion and inversion moves were underestimated, irrespective of shoe or static/dynamic testing. However, in the static trials there was significantly more angle error underestimation with the running shoe, although no significant differences were found between Five fingers and barefoot condition. While running (dynamic test), the treadmill surface slope was considerably improved estimated with Five hands than with traditional sneakers, or barefoot running. Question MarksThe above studies suggest that the use of minimalist shoes could have its location in a training program; however, more recent study is much less positive. To do so, ground reaction force data and kinematics were collected from 22 highly-trained runners throughout overground running while barefoot and in 3 shod conditions (minimalist shoe, racing level along with the athlete's regular shoe). The results demonstrated that though there were important differences between barefoot and shod conditions for kinematic and kinetic variables at the knee and ankle, there were no differences between shod states -- ie which none of those shod conditions successfully replicated barefoot running. Another study published only a couple of months ago examined the claims that minimalist shoes can promote a more efficient running activity, and so improve running economy(9). This analysis compared minimalist and standard running shoes (along with 'rocker shoes') for their impacts on energy cost and conducting efficiency. Eighteen endurance female runners who were inexperienced at running barefoot or with minimalist sneakers completed a six-minute sub-maximal treadmill running test for every footwear illness, during which oxygen consumption, carbon dioxide production, heart rate and rate of perceived exertion were measured. The main finding was that compared to the typical shoes, the minimalist shoes did not reduce energy expenditure or improve running economy (despite being lighter). The rocker shoes actually increased energy expenditure, something that the investigators put down to the significant extra mass of the shoe design. An even more unfavorable evaluation of the minimalist shoe asserts stems from a brand new US study, published in July of 2013(10). In the study, the researchers set out to determine if running in a minimalist shoe ends in a decrease in ground reaction forces and alters kinematics over standard shoe running. They also looked at whether any 'within- session 'accommodation to a minimalist shoe occurs. Fourteen male, rear-foot striking runners that had never run in a minimalist shoe were analyzed while running at 3.35 meters/sec for ten minutes on a treadmill in minimalist and standard shoes while three-dimensional lower extremity kinematics and kinetics were assessed. Data were accumulated after a minute and then again after ten minutes of running in both shoe types. The first finding was that minimalist shoe running resulted in no changes in step length or step rate. To make matters worse, after ten minutes, the vertical effect peak and moderate vertical loading rate during foot attack improved. To put it differently, the minimalist shoes hadn't only increased impact and loading forces initially, as time moved on, there was likewise no accommodation -- ie things got steadily worse! The researchers concluded: “Running in a minimalist shoe appears to (at least in the short term) increase loading of the lower extremity over standard shoe running. Moreover, the accommodation period resulted in less favorable landing mechanics in both shoes. Our findings therefore bring into question whether minimal shoes will provide enough feedback to induce an alteration that is similar to barefoot running.” Increased Injury RiskGiven that running in minimalist footwear was promoted as a means of eliminating or reducing running accidents by returning to a more natural gait, it may be surprising to learn that the literature includes an increasing number of studies showing an increased chance of harm from minimalist shoe usage. Furthermore, this isn't the injury risk arising as a consequence of switching unexpectedly to minimalist shoes without a gradual transition (see box 1above), but instead appears to be an inherent danger in the usage of these shoes themselves. Patients were interviewed to determine their running history, injury background, transition to minimalist footwear, and also their new injury details. These runners were running an average of 26 miles each week (ie not large mileage) for a mean of 19 decades. After changing into minimalist footwear, an accident occurred in these runners following an average of 2.8 months. Thirty-six experienced recreational runners underwent magnetic resonance imaging (MRI) before and following a 10-week period. Throughout the ten weeks, 17 subjects conducted only in their conventional (cushioned) sneakers while the other 19 gradually transitioned into the Vibram Fivefinger running shoes. A rating of 4 represented a stress fracture. The pre-training MRI scores weren't statistically different between the classes. However, the post-training MRI scores showed that from the Vibram group, 10 of the 19 athletes showed gains in bone marrow oedema in a minimum of one bone following 10 months of running. This implies that even using a carefully structured transition period, minimalist-type sneakers might raise the risk of stress fracture injuries. Summary & ConclusionsWhile barefoot running does appear to decrease impact loadings throughout foot strike, there is much controversy and little scientific agreement about any potential benefit concerning injury reduction this could cause. The evidence for using minimalist shoes, however, is rather more convincing -- but sadly in the wrong direction! While they can improve foot proprioception, there's conflicting evidence about whether minimalist shoes can successfully mimic barefoot running. Indeed, some studies indicate that they might increase impact loadings throughout foot strike. The evidence for their ability to decrease injury rates is rather more damning as a growing number of studies seem to suggest that far from reducing injury risk, using minimalist shoes may actually raise this risk -- even with an extended transition period into minimalist shoe use. References
1. JAMA. 2011;101(3):231-46
2. Nature. 2010 Jan 28;463(7280):531-5
3. Proceedings ISB XXth Congress, American Society of Biomechanics, 29th Annual Meeting. Cleveland. 2005:553
4. Int J Sports Phys Therapy 2012; Vol 7(5) 525-532
5. CMAJ, January 11, 2011, 183(1)
6. J Sports Med Phys Fitness. 2009 Mar; 49(1):6-13
7. J Sports Med Phys Fitness. 2011 Sep; 51(3):401-8
8. Br J Sports Med. 2013 Apr;47(6):387-92
9. J Sci Med Sport. 2013 May 24. pii: S1440-2440 (13)00102-3
10. Med Sci Sports Exerc. 2013 Jul 19. [Epub ahead of print]
11. Foot Ankle Int. 2012 Apr;33(4):262-6
12. Med Sci Sports Exerc. 2013 Jul;45(7):1363-8
13. Orthopaedics. 2011 Jul 7;34(7):e320-23
14. Foot (Edinb). 2013 May 10. pii: S0958-2592 (13)00018-7
Science based therapist, Dr. Alexander Jimenez looks at the several types of SLAP lesions, a few frequent clinical indicators, orthopedic evaluations and explores the very best rehab methods... Overhead athletes (like baseball pitchers, tennis, swimming, water polo and throwing athletes). All put enormous strain on their shoulders when participating in their chosen sport. An elite baseball pitcher's arm was listed at over 7000deg/second which puts it arguably as the fastest human body movement in game. This all happens at a joint that's been likened to a golf ball sitting on a tee -- ie it is structurally unstable. Considering all of this, is it any wonder that shoulder pain is a common occurrence in the overhead athlete? Throwers with shoulder pain will often complain of a "dead arm" which restricts them from throwing at pre-injury velocity/or control. SLAP (Superior Labrum Anterior-Posterior) lesions are common causes of this "dead arm" and will be the focus of this article. What Is A SLAP Tear?A SLAP tear is a tear of the glenoid labrum from anterior to posterior of the long head of biceps tendon. The glenoid labrum is a wedge-shaped fibrous tissue structure that's attached to the edge of the glenoid and its function is to weaken the glenoid cavity, thus improving stability, and it also has a role in muscle control and proprioception(1). The anatomy of the proximal long head bicep tendon is variable but typically it is derived from the posterior superior labrum and is wider and more densely innervated with sensory fibers compared to its distal tendon(5). Snyder has described four main subgroups of SLAP lesions(4) (see Figure 1): Type 1 – the attachment of the labrum to the glenoid is intact but there is some fraying and degeneration. This is not thought to be the cause of many symptoms. Type 2 – involves detachment of the superior labrum and long head biceps tendon from the glenoid rim. This is the most common type of SLAP lesion causing symptoms and often requires surgery. Type 3 – the meniscoid superior labrum is torn away and displaced into the joint but the tendon and labral rim attachment remains intact. Type 4 – the tear of superior labrum extends into the tendon, part of which is displaced into the joint along with the superior labrum. What Is The Mechanism Of Injury?The exact mechanism still remains controversial with three major theories present. The deceleration theory initially proposed that in a throwing athlete a SLAP lesion happened during the deceleration phase of projecting as a result of eccentric contraction of the biceps tendon(7). They suggested that this overloaded the biceps anchor that detached it from its intra- articular attachment. A direct blow to the shoulder has also been believed to be a cause for a SLAP lesion -- for instance, an athlete landing in an outstretched arm might compress/pinch the labrum between the glenoid and the humerus(1). More lately, Burkhart described the acceleration or "peel back mechanism" which occurs when the arm is at the cocked position of abduction and external rotation. They explained that during arthroscopy in shoulder abduction and external turning the thoracic fascia presumes a more vertical and posterior angle which generates a twist at the bottom of their biceps and a torsional force on the anterior superior labrum(1). Kuhn experimentally compared the deceleration and acceleration theories in cadavers models(1). They applied a brute force to the biceps tendon from the follow through place and were able to generate a superior labral avulsion in 20% of his specimens with a massive push. To simulate the peel back mechanism they placed the arm at an abducted and externally rotated position. In 90% of the shoulders analyzed, they could create a type 2 SLAP lesion with 20 percent less force than at the deceleration version. From this it can be proposed that the peel back mechanism is more likely to cause a SLAP lesion than the deceleration model and that the bicep tendon is not pulled but peeled from the bone. What Is The Clinical Presentation?SubjectiveAthletes who have a SLAP tear will often describe pain deep in the shoulder and it can be anterior or posterior. A throwing athlete may describe weakness when they throw and may state that they have lost their “zip”. Often the athletes may still throw, but maybe not at their normal velocity. They may describe a history of tightness on the back of their shoulder and pain/ weakness at the front especially within the coracoid process area(8). They may also clarify a click or pop when they toss and it is important to ascertain whether these symptoms are fresh and/or are painful. From the throwing athlete, it's important to inquire when exactly from the casting action they obtain their pain. As outlined earlier, an athlete that has pain/weakness at the late night phase may have a SLAP tear whereas an athlete who merely explains pain on follow-through may be more inclined to have impingement-type pain. ObjectiveStanding PostureOrdinarily, overhead athletes with SLAP tears will have poor scapula position at rest on their dominant side: Figure 2 shows inferior scapula position in a right-arm thrower. Burkhart explained this asymmetrical scapula position as with a SICK (Scapular malposition, Inferior border prominence, Coracoid pain and dysKinesis of scapula motion) scapula(3). It is also important to note thoracic posture, as increased kyphosis and lack of trunk rotation can also increase load on the shoulder when throwing. Shoulder ROMActive ROM of the shoulder must then be assessed to ascertain any motion restriction or pain. Glenohumeral rotation range ought to be assessed in all overhead athletes. A thrower's shoulder needs to have enough laxity to allow for excessive external rotation (demand of good throwing) with adequate dynamic stability to avoid subluxation. Glenohumeral rotation array is conventionally done in supine with the arm in 90-degree abduction. Commonly these athletes will get an increase in external rotation range (possibly due to repetitive stretching of their anterior capsule at the cocking phase and/ or humeral retroversion when they threw a lot if they were young) and a drop in internal rotation range. This absence of internal rotation range is frequently due to contracture of the posteroinferior capsule contracture and is popularly known as GIRD (Glenohumeral Internal Rotation Deficit). Sleeper stretches (see Figure 3) have been demonstrated to not only reduce GIRD but also to reduce shoulder injuries by around 40% in major league baseball players(1). TreatmentA Case StudyShoulder injuries in the throwing athlete would be initially managed with conservative therapy with therapy focused on improving GIRD and/ or scapula control. In most cases the whole kinetic chain should be assessed and proper exercises should be implemented based upon the requirements of their game. Figure 2 reveals a cricketer who bowls and throws with his right arm. When I first saw him, he complained of pain and "fatigue" in his shoulder when he bowled and threw from the boundary. He also had pain through range on abduction, which resolved if his scapula position was fixed (posterior tilted). He had no reduction of glenohumeral range on his right side. In this case (because of the success of posteriorly tilting his scapula on his pain through the evaluation) treatment focused on lengthening techniques of the muscles that anteriorly tilt his scapula, ie pec minor, and strengthening for his lower and middle trapezius that help to posteriorly tilt his scapula. This player was given a range of exercises in prone to improve his scapula position (see Figures 10 - 11). His pain improved over a four- week period and he is now able to throw in the boundary without any signs. Conservative treatment isn't always effective especially if a type 2 SLAP lesion is current. In such cases operative therapy is required and the athlete can take 9-12 months to return to sport and they'll report that it requires up to two years to go back to their pre-injury level. ConclusionIn summary, SLAP lesions are typical in the overhead athlete and a structured evaluation particularly looking at scapula control, glenohumeral rotation range in addition to orthopaedic tests can help to identify when a SLAP lesion is current and will also help direct therapy. Frequently in elite-level athletes, particularly when a type 2 lesion is present, surgery is needed(4). References
1. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 1: Pathoanatomy and Biomechanics. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No4, 404-420
2. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 2: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No5, 531-539
3. Burkhart S, Morgan C, Kibler B (2003) The disabled throwing shoulder: Spectrum of pathology, Part 3: The SICK scapula, scapula dyskinesis, the kinetic chain and rehabilitation. Arthroscopy: the Journal of arthroscopic and related surgery, Vol 19, No6, 641-661
4. Brukner P and Khan K (2012) Clinical Sports Medicine 4th edition McGraw Hill
5. Krupp R et al (2009) Long head of bicep tendon pain: differential diagnosis and treatment. Journal of orthopaedic and sports physical therapy Vol 39, no 2 55-70
6. McFarland E, Tanaka M, Papp D (2008) Examination of the shoulder in the overhead and throwing athlete, Clinical Sports Medicine 27, 553-578
7. Myers T et al (2005) The resisted supination external rotation test; A new test for diagnosis for SLAP lesions, the American Journal of Sports Medicine, Vol 33, No9 1315-1320
8. Ryu J, Pedowitz R (2010) Rehabilitation of bicep tendon disorders in athletes. Clinical Sports medicine 29 229-246
El Paso, TX. science based chiropractor, Dr. Alexander Jimenez looks at this uncommon problem – and how it can be treated. The true incidence of obturator externus accidents is unknown, as frequently they may be misdiagnosed as hip joint pathology and/ or groin pathology as the website of symptoms as well as also the presenting objective signals may mimic other pathologies such as hip joint labrum pathology, anterior femoral triangle issues and perhaps even gluteal pathology. Injury for this muscle gifts as a deep obscure groin/hip pain and functionally the muscle may still hide direct involvement as a pain generator since it is primarily a equilibrium muscle rather than a force-producing hip muscle. This case study presents an unusual case of hip-related pain in a professional baseball player which also shown itself as an injury to the contralateral adductor longus. The PlayerAs he was wrestled to the floor, his right hip was compelled at a rapid and loaded flexion/internal turning position. His first sensation was pain deep inside the anterior hip/groin area. When he presented to the medical team with the accident, he complained of a profound catching sensation inside the hip joint location. It had been difficult to fully bend the hip and to also twist on the stationary limb (because he did whilst kicking a ball). His prior background consisted of a right-sided inguinal hernia repair five seasons before as well as a few gentle on again/off back osteitis pubis-type signs that would normally flare from the first period as his goal-kicking amounts have been increased. He was obviously a left- footed goal kicker. On examination, he observed that the pain to become worse on passive flexion/internal rotation of the hip (hip walkway test). He was noticeably tight and irritated from the shallow TFL muscle, and also posteriorly across the greater trochanter around the insertion for the gluteals and deep hip rotators. He was also particularly high tone in the right iliopsoas muscle. He was initially diagnosed clinically because of hip joint sprain due to the mechanism of harm being a pressured flexion/internal rotation type position that would always put pressure on the anterior hip joint capsule/labrum. He was treated initially with deep iliopoas muscle sparks and hip joint mobilizations using a seat belt to gap the hip joint. He reacted reasonably well with the therapy and immediately felt more comfortable on a hip joint quadrant test. He was rested from coaching for 2 days and ran on the next day and played a match on the fourth day. But during the match, though his right hip did not create any pain, he'd notice pain on his left adductor source that was more pronounced during kicking. Three days post-game he detected this ongoing left adductor origin pain and it was made worse by kicking again through training. An MRI was performed to Look at the left adductor origin and also the report noted: - Grade 1 left adductor longus strain deep in the
- Grade 2 right obturator externus strain on its femoral attachment
- Grade 1 right iliopsoas muscle strain in the MTJ.
The surprise finding on the MRI of a grade 2 obturator strain prompted the medical team to more formally assess the participant for ongoing hip joint disorder. The particular features to notice from this medical examination were: Subjective● A sensation of weakness and instability in the right hip whilst kicking with the left foot.
● No pain in the right hip with running, even with top-end speed. However, the left adductor longus was symptomatic on running and kicking. Objective● Pain on passive right hip internal rotation whilst in 90-degree hip flexion. This pain was deep anteriorly in the hip, almost presented as a groin problem. ● Some discomfort on resisted right hip flexion/external rotation deep inside the iliac fossa. ● Pain and weakness in the left adductor on adductor squeeze tests. These squeeze tests performed at 0/45/90 degrees of knee flexion with a pressure cuff between the knees. Usual pre-season scores measured 260/260/250. On current testing they measured 150/170/180. Pain was felt at the end of the squeeze. ● Discomfort with prone lie hip passive internal rotation. This pain was more focused around the right greater trochanter posteriorly. PathomechanicsIt had been suspected that this player had endured a secondary injury to the left adductor longus (a muscle used a lot in goal-kicking) due to the inherent failure in bolstering the proper hip throughout the plant phase of the kick due to the inhibition of the right obturator externus, a muscle considered to be an important hip stabilizer and turning control muscle at the hip. With insufficient hip stabilization in kicking, the left hip was required to create more power to compensate for the unstable right hip to gain the length from the kick. Then the left adductor longus failed along with a strain injury led. ManagementThe management of the matter initially centered on the two key features being the left-sided adductor strain and the right- sided obturator externus strain. In the week following the accident, the player was sent to get a series of Actovegin shots to the left adductor longus. This was done according to protocol that was three injections every 48 hours -- Monday/ Wednesday/Friday. In this five-day period the adductor longus was handled with deep tissue flush massage and gentle isometric adduction exercises at supine (chunk squeezes) in the three positions of examining -- 0/45/90 levels of knee flexion -- also as wall squat adductor squeezes in the same positions. The obturator externus was medicated with heavy tissue releases (obtained through the anterior groin region) and direct theraband strengthening of hip external rotation in sitting and in prone. Actovegin shots to the obturator externus are regarded as difficult because of problems with accessing this muscle through the superficial hip musculature. The adductor exercises progressed into through array adduction with theraband resistance (equally with the left leg being the motion leg as well as the stability leg). By 12 days post-injury it had been detected that the obturator externus strength had not improved and the player still had deep- seated right back pain pain. It was rationalised that perhaps the direct treatment to this muscle and also the direct open kinetic chain strengthening was possibly making the muscle texture worse. The choice was made to stop any direct hands-on therapy to the muscle and also to prevent any direct open kinetic chain strengthening. Instead the player lasted with bilateral theraband exercises of both hips into flexion and then abduction and expansion in addition to adduction. The avoidance of lead obturator externus soft tissue treatment and exercise appeared to improve the hip function immediately. The participant started running 20 times post-injury and quickly progressed through running stages over a five-day period of conducting on alternate days. At this point the player's adductor squeeze scores had improved to steps according to pre- season baselines. However, daily the player ran direct adductor strength operate using a Pilates reformer as a slider drill to immediately load into adduction in addition to hammering theraband adduction exercises in standing and in supine lying. By 27 days post-injury the player managed to begin kicking, change in direction and rugby training. He played at 30 times post-injury with no ill effects. DiscussionIt arises immediately around the medial side of the obturator foramen, as well as the inferior ramus of the ischium; it also arises in the lateral two-thirds of this outer surface of the obturator membrane, and also in the tendinous arch which completes the canal to the passage of the obturator nerves and vessels. The action of the muscle is to externally rotate the hip and also helps in hip adduction. It's postulated to also work as a hip balance muscle in one legged stance along with the obturator internus, quadrutus femoris, piriformis and the gemelli muscles. In a practical activity such as kicking, the muscle acts to stabilize or hold the ball of the femur into the socket (acetabulum). The incidence of harm to the obturator externus muscle is unknown because there are only a handful of case reports from the medical literature that highlight injuries for this muscle. Additionally, among the vexing issues is the difficulty in creating the correct clinical diagnosis based on the history and physical evaluation. MRI imaging is needed to correctly picture injuries to this muscle. From the case study introduced, injury for the muscle was a direct result of forceful flexion/internal rotation mechanism to the hip joint. As the muscle primarily functions as a hip stabilizer during jogging, it is possible that a patient can mask symptoms during functioning as the muscle isn't required to produce any hip skate for locomotion. Nonetheless, in this event the muscle has a role in stability of the hip during kicking, and for that reason may have produced a poor pelvic/hip complicated during kicking that then led to an accident to the adductor longus on the other hand. In addition, it seems that direct treatment to the muscle in the form of deep trigger point releases and also direct strengthening may actually delay healing in the muscle in case of injury. This may highlight the value of the muscle as a hip stabilizer instead of a legitimate torque manufacturer in hip rotation.
Swimming is a intricate sport that places huge demands on the body for propelling through the water. The shoulders often suffer as a consequence of this, but, injury chiropractor, Dr. Alexander Jimenez asks, what are the implications of musculoskeletal shoulder asymmetry? OverviewSwimming is a hugely popular game for both recreational and competitive functions. The nature of exercising against the water immunity provides a special setting compared to the field or court in all other sports. Likewise, most other sports utilize a dominant side, whereas in swimming that the repetitive, continuous motions require either side of your system to be coordinated and equally strong. This can place an accumulation of stress physically. The overhead actions of a swimming stroke may notably strain the shoulder joints and around 73% of swimmers will experience shoulder pain at any stage within their career(1). Taking this advice on board, surprisingly, swimmers do not usually develop symmetrically with equal muscle power on each side. And in which there is muscle imbalance, they commonly compensate by using different muscles more than ordinary to guarantee the total force generated is the same(2). Swimming also does not provide that point of contact or source to hold on to enjoy most other sports have. Swimmers rely on their inbuilt strength throughout the body along with the entire kinetic chain to generate maximum force propulsion. Expertise and strategy are important facets to contribute to this, however if there's a natural muscle imbalance then this can further affect technique, however much technique instruction you provide. Asymmetry is defined when there's a muscle imbalance between the left and right sides greater than 10%(two). This means that the muscles on one side are more powerful or more efficient compared to those on the opposite side. A recent study that screened nationwide- level hens found that 85% were asymmetrical(two). Asymmetry usually develops because of the shoulder or whole arm being used wrongly or too often. Excessive repetition with no adequate rest causes the muscles to exhaustion. This decreases muscle activity and induce generation, and eventually causes biomechanical abnormalities as the swimmer attempts to overcome these failing mechanisms(3). A third of those swimmers in the study that were discovered with asymmetry were also identified as having compensatory plans(2). Asymmetry can lead to: - further muscle imbalance;
- compensatory movement strategies, such as using increased hand force;
- muscle injury.
Every one of these can alter technique and thus performance execution. This might be the difference between finishing first and finishing second in competition. Screening For Shoulder AsymmetryScreening is the process of assessing a variety of characteristics that are significant with the game. This allows the identification of possible flaws and muscle imbalances. Strengthening applications to rectify such findings may provide optimum strength, functionality and prevention of injury. Table 1 details the key screening tests for identifying asymmetry in shoulder power for swimming. This scale details if the athlete can move against gravity (tier 3), then resist your force (grade 4), and supply full strength to resist (grade 5). Shoulder flexion is not listed here as a screening test as it's been found that it doesn't have any effect on shoulder asymmetry(2). This implies that many swimmers all have an equal stroke length. It seems to be the abduction, adduction and rotational components which become imbalanced and make the asymmetry of the shoulders. Arm dominance and breathing side can also be often considered significant factors in procedure perfection; however studies have not found these to have any consequences on performance(two). For more technically precise ways to assess these functions with dynamometer, see the original research articles(1,2). Even though these are significant testing purposes, it's just as important to look elsewhere when trying to identify potential weaknesses. The surrounding muscles like the latissimus dorsi should be considered. Latissimus Dorsi StiffnessThe latissimus dorsi is your largest muscle of the trunk and is responsible for all pushing and pulling type activities. The repetitive character of swimming and thus overuse of the latissimus dorsi usually means that this muscle may be prone to stiffness. Figure 2 shows the latissimus dorsi, which attaches to the mid spine at T7, the lower ribs and down to the pelvis at the iliac crest. It inserts into the top of the shoulder called the bicipital groove and also to the lower part of the shoulder blade. It inserts into the top of the shoulder called the bicipital groove and also to the lower part of the shoulder blade. It's these insertion points that allow the muscle to control shoulder blade motion. A study that investigated the effects of latissimus dorsi stiffness on scapular movements among swimmers found that the muscle stiffness caused three significant problems with scapular mechanisms(1) (see Table 2). Each of these issues alters the way the shoulder blade operates mechanically. This modified mechanics can then develop injuries as other structures become caught or pinched within the shoulder joint distances. These injuries will influence technique as the shoulder will slowly lose power and strength. Have the athlete in crook lying with their back flat against the bed. Ask them to lift their arms over their head. If there is latissimus dorsi stiffness they'll struggle to fully stretch the arms overhead, and/or their spine will lift up away from the mattress. For a more accurate and technical evaluation method refer to this analysis by Illinois University(1). Power Exercises For Fat LossThe added resistance that the water provides requires strengthening exercises to be carried out in similar motions to replicate the coils. This may improve the specificity and ensure the correct muscles have been targeted. Key exercises for scapular strengthening that carry over ideally for swimming are shown below. 1. BreaststrokeThis is all about the scapular setting. The shoulder blades are activated as the arm extends forwards, then pull backwards just like the swimming stroke(10). 2. SwimmingThe athlete raises their opposite arm and leg up while maintaining the shoulder blades in the neutral position. The opposite side is then performed(10). 3. Low rowUsing a resistance band tied to a door handle in front, the athlete pulls the band backwards past their hip and slowly returns to the start position. 4. Front crawl simulationThis exercise involves having a resistance band from one hand around the back of the body and held in the other hand (like wearing a jacket). The affected arm is then taken through a front crawl stroke while pulling the resistance band tightly. The shoulder blades should be kept in neutral throughout and avoid the desire to throw the shoulder forwards. Summary- Asymmetry is a difference in muscle balance between the right and left sides and can lead to weakness, poor technique, compensatory strategies, and injury.
- Swimmers are susceptible to asymmetry due to the repetitive use of the shoulders. Specific screening tests can be performed to identify where weaknesses lie. Shoulder abduction, adduction, and rotations are the main culprits because of their repetitive use within every stroke.
- Treatment consists of strengthening and stabilizing the scapular muscles over a period of weeks, and making the exercises powerful to replicate the force required to battle through the water.
References:
1. Phys Ther in Sport. 2013; 14:50-53.
2. Phys Ther in Sport. 2013; http://dx.doi.org/ 10.1016/j.ptsp.2013.02.002
3. Rehab Res and Practice. 2012; ID:853037; 1-9.
4. McKesson Healthcare Solutions. 2004. www.mckesson.co.uk
5. Phys Ther in Sport. 2004; 3:109-124.
6. Musculoskeletal assessment. 2000. 2nd Ed; 150-156.
7. Clinical Sports Med. 2006. 3rd Ed; .246-247.
8. http://www.shoulderdoc.co.uk/article.asp?article=1381
9. http://www.youtube.com/watch?v=AcPZEtWP1x4 (2013).
10. APPI Pilates Matwork Handouts manual.2012. www.ausphysio.com
Most of us will experience it at some point, but how does it influence on athletic performance? Chiropractic injury specialist, Dr. Alexander Jimenez investigates. Research postulates that 80 percent of the populace will undergo an acute onset of back pain at least once in their lifetimes. This adds a considerable financial burden not just on the medical system (physician consultations, prescribed drugs, physiotherapy) but also the financing of the workforce in lost employee hours and loss in productivity. The types of lower back pain that an individual may experience include (but are not limited to): 1. Lumbar spine disc herniation with/ without sciatica 2. Lumbar spine disc bulges 3. Lumbar spine disc degeneration 4. Lumbar spine disc annular tears 5. Ligament sprains 6. Muscle strains, particularly quadrutus lumborum 7. Osteoarthritis 8. Inflammatory arthritis such as rheumatoid and anklyosing spondylitis 9. Facet joint sprains 10. Bone injuries such as stress fractures, pars defects and spondylolisthesis. The focus for this paper will be on the previous group -- that the bone injuries. This may be simply postural (slow onset repetitive trauma) or related to sports; for instance, gymnastics. The two demographic groups that tend to endure the most extension-related low back pain are: 1. People who endure all day, for instance, retailers, army, security guards etc.. Prolonged position will obviously force the pelvis to start to migrate to an anterior tilt management. This may begin to place compressive pressure on the facet joints of the spinal column as they also change towards an expansion position since they accompany the pelvic tilt. 2. Extension sports such as gymnastics, tennis, swimming, diving, football codes, volleyball, basketball, track and field, cricket fast bowlers. This is more pronounced in sports that involve extension/rotation. PathomechanicsWith normal extension of the lumbar spine (or backward bending), the facet joints begin to approximate each other and compress. The articular processes of this facet above will abut the articular process of the facet below. This is a normal biomechanical movement. However, if the extension ranges are excessive, the procedures will impinge quite aggressively and damage to the cartilage surfaces within the facet joint can result. Sports such as gymnastics, functioning in tennis, and handling in American Soccer may all involve uncontrolled and excessive extension. It would be unlikely that a bone stress response or even a stress fracture could be brought on by an isolated expansion injury. It would be more likely that a sudden forced extension injury may damage an already pre-existing bone strain reaction. Similarly, if an individual stands daily and the pelvis migrates into lateral tilt, then the aspects will be placed under low load compression but for extensive intervals. With ongoing uncontrolled loading, stress is then transferred from the facet joint to the bone below (pars interarticularis). This originally will manifest as a pressure reaction on the bone. This bone strain may advance to a stress fracture throughout the pars if uncorrected. This fracture is also referred to as a "pars flaw", or spondylolysis. It was initially considered that stress fractures of the pars was a congenital defect that introduced itself at the teenage years. However, it is now agreed that it is probably obtained through years of overuse into extension positions, especially in young sportspeople involved with expansion sports. What's more, one-sided pars defects often occur more commonly in sport which also included a rotational component such as tennis serving or fast bowling in cricket. The stress fracture can then advance to impact the opposite side, causing a bilateral strain fracture, with anxiety subsequently being transferred to the disk in between both levels. Spondylolisthesis features bilateral pars defects which could possibly be a result of repetitive stress into the bilateral pars in extension athletics, but more likely it is an independent pathology that manifests in the early growing stages (9-14) as this pathology is often viewed in this age category. If they become symptomatic in later years because of involvement in expansion sports, it is exceedingly likely that the defects were there by a young age but presented asymptomatically. As a result of rapid growth spurts in teenage years and the high-volume training experienced by teenaged athletes, it is possible that these dormant spondylolisthesis then pose as 'acute onset' back pain in teenage years. In summary, the progression of this bone stress reactions tends to follow the following continuum: 1. Facet joint irritation 2. Pars interarticularis stress response 3. Stress fracture to the pars 4. Pars defect (or spondylolysis) 5. Spondylolisthesis due to activity or more likely congenital and found later in teenage years due to participation in extension sports. The landmark publication related to spondylolysis and spondylolisthesis was presented by Wiltse et al (1976) and they classified these injuries as follows: 1. Type I: dysplastic – congenital abnormalities of L5 or the upper sacrum allow anterior displacement of L5 on the sacrum. 2. Type II: isthmic – a lesion in the pars interarticularis occurs. This is subclassified as a. lytic, representing a fatigue fracture of the pars,
b. elongated but intact pars, and c. acute fracture. 3. Type III: degenerative – secondary to long-standing intersegmental instability with associated remodeling of the articular processes. 4. Type IV: traumatic – acute fractures in vertebral arch other than the pars. 5. Type V: pathological – due to generalized or focal bone disease affecting the vertebral arch. The vast majority of spondylolysis and sponylolisthesis accidents are Type II -- the isthmic variety. For the purposes of this paper, we will refer to the above stages as the posterior arch bone stress injuries (PABSI). EpidemiologyIt is a lot more widespread at the L5 level (85-90 percent). It's a high asymptomatic prevalence in the general population and is often found unintentionally on x ray imaging. Nonetheless, in athletes, particularly young athletes, it is a common reason for persistent low back pain. From the young athlete, the problem is often referred to as 'active spondylolysis'. Active spondylolysis is normal in virtually every gamenevertheless, sports such as gymnastics and diving and cricket pose a much greater danger due to the extension and turning character of the sport. The progression from an active spondylolysis into a non-union type spondylolisthesis has been associated with a greater prevalence of spinal disk degeneration. Early detection through screening and imaging, therefore, will highlight those early at the bone stress phase and if caught early enough and managed, the progression to the larger and more complicated pathologies are avoided as a result of therapeutic capacity of the pars interarticularis in the early stages. It is more common to find teens and young adults afflicted by PABSI. This will highlight the rapid growth of the spine through growth spurts that is also characterized by a delay in the motor control of the muscle system during this period. Furthermore, it's thought that the neural arch actually gets stronger in the fourth decade hence possibly explaining the low incidence of bone stress reactions in mid ages. The incidence of spondylolysis has been reported to be around 4-6% in the Caucasian population (Friedrikson et al 1984). The rates seem to be lower in females and also in African-American males. It has also been suggested that a link exists between pars defects and spina bifida occulta. The incidence of spondylolysis seems to be higher in the young athletic population than in the general population. Studies in gymnasts, tennis, weightlifting, divers and wrestlers all show disproportionately high incidence of spondylolysis compared with the general population of age-matched subjects. TennisThe tennis serve generates excessive extension and rotation force. In addition, the forehand shot may also produce elevated levels of spinning/ extension. The more traditional forehand shot demanded a great deal of weight shift through the legs to the torso and arms. However, a more favorite forehand shot is to currently face the ball and also generate the force of this shot utilizing hip rotation and lumbar spine extension. This action does increase ball speed but also puts more extension and compressive loads on the spine potentially resulting in a greater degree of stress on the bone components. GolfThe most likely skill component involved in golf that may cause a PABSI are the tee shot with a 1 wood when forcing for distance. The follow-through of this shot entails a significant quantity of spine rotation with maybe a level of spine expansion. CricketFast bowlers in cricket are the most susceptible to PABSI. This will occur on the opposite side to the bowling arm. As the front foot engages on plant stage, the pelvis abruptly stops moving but the spine and chest continue to proceed. With the wind-up of this bowling action (rotation), when coupled with expansion this can place large forces on the anterior arch of the thoracic. More than 50% of fast bowlers will create a pars stress fracture. Young players (up to 25) are most vulnerable. Cricket governments have implemented training and competition guidelines to avoid such injuries by restricting the number of meals in training/games. Field EventsThe more common field events to cause a PABSI would be high leap followed by javelin. Both these sports create enormous ranges of backbone extension and under significant load. Contact SportsSports like NFL, rugby and AFL all require skill components that need backbone expansion under load. Gymnastics/DancersIt goes without saying that gymnastics and dancing involves a substantial amount of repetitive spine expansion, particularly backflips and arabesques. It has been suggested that nearly all Olympic degree gymnasts could have suffered from a pars defect. Many organizing bodies now put limits on the number of hours young gymnasts can instruct to prevent the repetitive loading on the spine. DivingSpine extension injuries occur mostly off the spring board and on water entrance. Diagnosis Of PABSI In AthletesClinical investigation These can pose as preventable injuries. Research shows that the incidence was emphasized from the general population that have nil indicators of back pain. But, individuals will typically complain of back ache that is deep and generally unilateral (one side). This may radiate into the buttock area. The most offending movements tend to be described as expansion moves or backward bending movements. This may be a slow progression of pain or might be initiated by one acute episode of back pain in a competitive extension motion. On clinical examination: 1. Pain may be elicited with a one-leg extension/rotation test (standing on the leg on the affected side) – stork test. 2. Tenderness over the site of the fracture. 3. Postural faults such as excessive anterior tilt and/or pelvic asymmetry. The one-legged hyperextension test (stork test) was suggested to be pathognomonic for busy spondylolysis. A negative evaluation was stated to effectively exclude the diagnosis of a bone stress-type injury, thus creating radiological investigations unnecessary. But, Masci et al (2006) examined the connection between the one-legged hyperextension test and gold standard bone scintigraphy and MRI. They discovered that the one-legged hyperextension test was neither sensitive nor specific for active spondylolysis. Moreover, its negative predictive value was so poor. Thus, a negative test can't exclude energetic spondylolysis as a possible cause. Masci et al (2006) go on to indicate that the bad relationship between imaging and the one-legged test may be because of a number of factors. The extension test would be expected to move a significant extension force on to the lower back spine. In addition to putting substantial strain on the pars interarticularis, it might also stress different regions of the spinal column like facet joints as well as posterior lumbar disks, and this may subsequently induce pain in the existence of other pathology such as facet joint arthropathy and spinal disc disease. This will explain the poor specificity of the test. Conversely, the inadequate sensitivity of the test may be related to the subjective reporting of pain by issues performing the maneuvre, which may vary based on individual pain tolerance. Additionally, this evaluation can preferentially load the fifth cervical vertebra, and so bone stress located in the upper lumbar spine may not test positive. Grade 1 spondylolisthesis are normally asymptomatic; nonetheless, grade 2+ lesions often present with leg pain, either with or without leg pain. On examination, a palpable slip could be evident. ImagingClinical assessment of active spondylolysis and the more severe pars defects and spondylolisthesis can be notoriously non-specific; this is, not all patients suffering PABSI will present with favorable abstract features or positive signs on analyzing. Thus, radiological visualization is important for diagnosis. The imaging methods available in the diagnosis of bone stress injury are: 1. Conventional radiology. This test is not very sensitive but is highly unique. Its limits are partially because of the cognitive orientation of the pars defect. The oblique 45-degree films may show the timeless 'Scotty Dog' appearance. Spondylolisthesis can be looked at simply on a lateral movie x-ray. 2. Planar bone scintigraphy (PBS) and single photon emission computed tomography (SPECT). SPECT enhances sensitivity in addition to specificity of PBS than straightforward radiographic study. Comparative research between PBS and conventional radiology have shown that scintigraphy is more sensitive. Patients with positive SPECT scan must then undergo a reverse gantry CT scan to assess whether the lesion is active or old. 3. Computed tomography (CT). The CT scan is considered to be more sensitive than conventional radiology and with higher specificity than SPECT. Regardless of the type of cross-sectional image utilized, the CT scan provides information on the state of the flaw (intense fracture, unconsolidated flaw with geodes and sclerosis, pars in procedure for consolidation or repair). The "inverse gantry" perspective can evaluate this condition better. Repeat CT scan can be used to track progress and recovery of the pars defect. 4. Magnetic resonance imaging (MRI). This technique shows pronounced changes in the signal in the amount of the pars. This is recognized as "stress response" and can be classified into five different degrees of action. MRI can be helpful for evaluating elements that stabilize isthmic lesions, for example intervertebral disc, common anterior ligament, and related lesions. The MRI isn't as specific or sensitive as SPECT and CT combination. Therefore, the current gold standards of investigation for athletes with low back pain are: 1. bone scintigraphy with single photon emission computed tomography (SPECT); if positive then 2. limited reverse-gantry axial computed tomography . MRI has many advantages over bone scintigraphy, for instance, noninvasive nature of the imaging along with the absence of ionizing radiation. MRI changes in active spondylolysis include bone marrow edema, visualized as increased signal in the pars interarticularis on edema-sensitive sequences, and fracture, visualized as reduced signal in the pars interarticularis on T1 and T2 weighted sequences. However, there is greater difficulty in detecting the changes of busy spondylolysis from MRI. Detecting pathology from MRI relies on the interpretation of distinct contrasts of signals compared with normal tissue. Unlike stress fractures in different parts of the body, the little region of the pars interarticularis may make detection of those changes harder. However, unlike MRI, computed tomography has the capability to differentiate between acute and chronic fractures, and this differentiation might be an important determinant of fracture healing. Accordingly, in areas using pars interarticularis fractures discovered by MRI, it might nonetheless be necessary to execute thin computed tomography slices to determine whether or not a fracture is severe or chronic -- an important factor in fracture resolution.
Science based chiropractor, Dr. Alexander Jimenez demonstrates that foot injury as a consequence of the foot/pedal interface is amazingly common and under-reported... Cycling injury research can be broadly collated into two groups: trauma-related, which happens as a consequence of a crash or collapse, and non-trauma-related, which entails overuse-type injuries. The epidemiology of collision/impact injuries in cycling has brought a relatively large amount attention from investigators, presumably because of their life- threatening possible. However, the data indicates that despite the acute dangers of accidents and drops, cyclists are more likely to suffer with accidents resulting from the action of biking. A 2006 research on cycling injuries reasoned that the prevalence of non-traumatic harm was as high as 85 percent(1). Although coaches, chiropractors, physiotherapists and coaches can not do much about the former, overuse-type injuries are amenable to treatment and prevention. A survey of the literature about non-traumatic cycling injuries demonstrates that much of this research thus far has been focussed on injuries of the trunk, neck, arms, hands, buttocks, perineum and knees(two). This is perhaps understandable; cyclists interface with the bike at three distinct points -- the handlebars, the saddle and the pedals. Incorrect handlebar shape/settings, saddle design/height or framework geometry could lead to excessive loading on muscles and joints as well as undesirable motion biomechanics, significantly increasing the probability of harm (see Box 1). Overlooked FootOne area which may have been overlooked, however, is your pedal port, especially because it is the foot/pedal interface which typically encounters the greatest forces during cycling. Unlike other overuse biking accidents mentioned above, there's very little peer-reviewed research accessible on foot injuries, with those foot accidents that are reported in the literature being mainly descriptions of foot numbness, metatarsalgia, achilles tendonitis and plantar fasciitis(3-5). A study by Dettori and Novell (2006) reported about the prevalence and incidence of lower leg/foot cycling injuries collated by a meta-review of non-traumatic bicycling accidents(1). The data were presented as self-reported heights of pain gathered from cyclists engaging in tour rides, ranging from the shortest distance of 545km over a six-day occasion to the longest distance of 7242km within an 80-day event. The incidence of reduced leg/foot harms was reported to be 7 percent, 13 percent and 22% respectively, with an incidence rate of 24 percent. Nonetheless, this data believed both the lower leg and the foot to be one homogeneous unit rather than separate anatomical regions, which consequently negates its usefulness as meaningful foot pain data for the wider cycling population. Simply speaking, there's very little research concerning the frequency, etiology and/or management of foot discomfort in cycling available to direct the clinician. The little amount of available literature that's available tends to be descriptive non-systematic literature reviews or view. Moreover, where data are reported, participants have yet to be sampled robustly and research have tended to concentrate only on elite cyclists instead of those engaged in club, recreational and fitness cycling (that the huge majority of cyclists). New Research On Foot Pain IncidenceGiven the abundance of anecdotal evidence suggesting that foot injuries in cyclists are more common than is often reported, a 2012 study set out to try and identify typical kinds of foot injuries suffered by cyclists and just how common these are(6) In the study, Australian researchers set out to answer the following questions about foot injuries in cyclists: - what is the distribution of age, gender, foot/pedal interface use and distances cycled amongst cyclists who experience foot pain?
- what type of pain and in what region of the foot do cyclists typically experience pain?
- what techniques do cyclists use to try and cope with/overcome foot pain caused by cycling?
- are there key groups of cyclists at greater risk of foot pain than others?
To do so, an electronic survey was utilized to collect data from cyclists within South Australia, during December 2010. Cyclists were invited to take part and fill out the questionnaire if they were riding a non-stationary, vertical bicycle at least one time per week for no less than one continuous hour, and so were at least 18 decades old. The sample of cyclists analyzed numbered 397, attracted from Bike SA (the main representative body for South Australian riders) in addition to Mega Bike (a massive bicycle store in Adelaide) and personnel and pupils of the School of Health Sciences in the University of South Australia. The cyclists were requested to give details about their level of cycling participation, the pedal port utilized (clip less/toe straps) and the kinds of foot pain endured. A number of critical findings became evident, the first of which was that over half of the cyclists (53.9 percent) reported experiencing foot pain whilst biking. The cyclists normally described the pain as 'burning' or 'numbness.' The most usual methods of dealing with this kind of pain comprised stopping for a period of time through the ride, shoe removal, walking round and massaging/ stretching the foot. This analysis shows exactly how common foot pain may be among recreational cyclists. The fact that 'cleated-in' shoes increased the danger of pain is perhaps no surprise; studies have already shown that these types of shoe have a tendency to localize plantar pressures, which in turn can be detrimental to blood and nerve supply integrity in that area(2,7). Another implication that follows is that cycling shoe design and choice could be just as essential as saddle and saddle options for pain-free cycling. Evaluation Of The Foot-Pedal InterfaceThe foot-pedal port is the sole guide website for energy transport from the fisherman into the bike. In a 'cleated-in' pedal port (one having clip less pedals and shoes or toe clips and straps), all of the body's power to make the bicycle move forward is moved to the pedal through a really small contact area (typically around 60mm2), and there is consistent anecdotal evidence that forefoot pain at this stage of energy transfer is common(2,7). The most obvious issue this raises therefore is if the use of particular sorts of biking shoe structure, insole substances or contoured surfaces can decrease the incidence of pressure hot spots by spreading the load more evenly. Indeed, this approach is embodied by specific cycling shoe makers like Specialized, who utilize a combination of particular material types and contoured surfaces to attempt to minimize forefoot distress. Looking at shoe building first, a current trend has been the movement towards stiffer and stiffer cycling shoe construction and especially the use of carbon fiber. The reasoning is that higher shoe stiffness contributes to less shoe bend and therefore less electricity wastage during the power transfer. To look into this specific query, US scientists conducted a study into cycling shoe stiffness on forefoot pressure(7). Plantar pressure data have been recorded in two different shoe types to ascertain the effect of cycling shoe stiffness on peak plantar forefoot pressure in cyclists. Two pairs of shoes of the same size and manufacturer, indistinguishable except for outsole material and stiffness, were analyzed. Shoe stiffness measurements were gathered under controlled conditions and in two different configurations using a dynamic hydraulic tensile testing machine. Measurements of plantar pressure were assembled using 'Pedar' capacitive-based detector insoles while issues pedaled in a seated position in a restricted power output of 400 watts (hard!) . The pressure distribution in carbon fibre composite sneakers during cycling was compared to that of cycling shoes made with (cheaper) plastic soles. Concerning stiffness, the carbon fibre sneakers were surely stiffer -- 42% and 55% more pliable than plastic sneakers when subjected to longitudinal bending and bending bending, respectively. During pedaling, the carbon fibre shoes generated peak plantar pressures 18 percent higher than people of plastic design, and the authors concluded that competitive cyclists afflicted by metatarsalgia or ischemia must be particularly careful when using carbon cycling shoes because the shoes increase peak plantar pressure, which might aggravate these foot ailments. Jumping To ConclusionsHowever, more recent research suggests that assessing a shoe's possible to cause foot pain based purely on its structure may lead to incorrect decisions. This originates from an interesting study published annually by German researchers, who contrasted the effects of carbon fiber foot orthoses with standard cycling shoe inserts on plantar pressure distribution through biking(8). In the study, 11 pain-free triathletes were examined on a cycle ergometer at two different cadences (60 and 90 rpm) and at two unique workloads -- both 200 and 300 watts. These were: - a cycling shoe with its standard insole (control condition);
- the same shoe but with carbon fibre foot orthoses.
Using carbon fibre for the construction of this orthoses was important; due to its inherent stiffness and capacity to be worked into complex shapes, it is possible to make carbon fibre orthoses that don't yield, even under the greatest loads. This consequently means that the foot has been held more securely in its desired position/orientation regardless of loading. Throughout the trials, the investigators recorded the mean peak pressure, both to the entire foot region and for particular foot areas (rear, mid, esophageal foot (medial, central, lateral) and toe area). As Figure 1 reveals, peak pressures recorded in the total foot area ranged from 70-75kPa at 200 watts power output, and out of 85-110kPa in 300 watts. Regardless of being stiffer, the carbon fibre foot orthoses reduced peak pressures by approximately 4.1 percent compared to the standard insole. Within separate foot regions, back foot peak pressure was decreased by 16.6 percent, mid foot strain by 20.0 percent and forefoot strain by 5.9 percent. It was mentioned, however, that in the toe region, peak pressure with the carbon orthoses was raised by approximately 16%. Regardless of which fit was utilized, when it came into the forefoot it also had been the lateral forefoot that showed the maximum peak pressures when compared to lateral and lateral forefoot (34 percent and 59% greater for the carbon and standard inserts respectively). The authors concluded that carbon fiber can serve as a suitable material for foot orthoses in biking partly because plantar pressures don't grow as a result of the stiffness of the carbon and also because with person customization, there's the possibility to further peak pressure in some specific foot places. Surely, it looks like in regards to stress reduction, form/ contouring is more important than orthotic stiffness. By the exact same token, simply substituting padded insoles in an overly embarrassing biking shoe is not likely to result in an automatic treatment for foot discomfort. Conclusions & RecommendationsThe US researchers mentioned previously concluded from their study that the plantar pressures recorded during seated biking were within the range listed for ordinary walking, despite cycling being considered an extremely low impact game(7). If a fisherman poses with foot pain, consequently, the problem of plantar pressures in biking shouldn't be dismissed as the potential origin. This is particularly true for competitive cyclists that will potentially 'push' around 40 million pedal cycles throughout their career! Excessive plantar pressure is not something that happens in isolation, and much more study is needed about the use of other factors in precipitating foot discomfort during cycling. These include bicycle set-up (saddle height, saddle distance, cleat position), type of cycling shoe (type of cleat, material of sole), shoe fit (too tight, too narrow, attached too tightly), foot type of the cyclist (pes planus, pes cavus), presence of any lower limb biomechanical or structural deformities (genu varum, forefoot supinatus, ankle joint equinus), differences in body mass, the typical cycling terrain (hills or flat terrain) the preferred pedaling cadence and use of low/high gearing, as well as the experience and fitness of the cyclist. For now, however, coaches, physiotherapists, chiropractors and coaches must know that foot discomfort during cycling is surprisingly common and much more likely associated with plantar pressure issues. Box 2 gives some practical recommendations that can be offered to cyclists in their own care. References
1. Sports Med. 2006;36(1):7-18.
2. J Bodywork Movement Therapies 2005; 9:226-236.
3. Sports Medicine 1994; 17:117-131 .
4. Sports Medicine 1991; 11:52-70.
5. American Podiatric Medical Association 2000; 90:354-376.
6. Journal of Science and Cycling 2012; 1(2): 28-34.
7. Foot and Ankle International 2003; 24:784-788.
8. Sportverletz Sportschaden. 2012 Mar;26(1):12-7.
Science chiropractor, Dr. Alexander Jimenez has a look at a patient with pain in her calf -- and brand-new jogging shoes. A 33-year-old female presented to the clinic with a tight and painful medial aspect of the left calf. The patient complained that she believed she had been suffering from 'shin splints'. The pain had begun after an especially challenging course run over rocky and hilly terrain. No pain was noticed during the running session nevertheless, the pain began the following day. There was no pain in the arch or ankle of the foot. On clinical examination, the pain has been concentrated on the muscle belly of the flexor hallucis longus (FHL) muscle because it divides out from underneath the soleus. The pain was exacerbated by shoving off through walking and was evident on stretching ankle dorsiflexion with associated big toe dorsiflexion. Contraction of the large toe into plantar flexion although the ankle was also plantar bending also caused pain. She had been diagnosed with a strain of this FHL muscle. She had been back to complete running in 3 weeks. What was intriguing to notice in this individual was that she had recently purchased new running shoes. The shoes she had bought (Asics Gel Kayano) would be the same ones she generally conducted with. However, she remarked that those she had bought were a half size bigger than the previous pair. When I asked her why she had purchased a larger pair of shoes, she clarified that the sales rep at the shoe shop had measured her foot length and noticed that the ideal foot was a half size larger than the left, and argued that she had a pair of shoes to match the larger foot to protect against any forefoot compression in the shoe. What was important to me was the fact that the larger shoe on the left had actually resulted in the FHL muscle strain. The reason, I concluded, was that when operating on tight irregular surfaces, her left foot would have been sliding in the shoe more than the right foot as a result of excess length in the left shoe. This always would have led to her overusing the FHL to 'claw' her big toe into the sole of the shoe to reduce the shear and slipping of her foot. This could have overloaded the FHL sufficiently to cause a muscle strain. The FHL MuscleIt's a flat bipennate muscle which courses obliquely under the soleus to appear over the medial side of the tibia. It's located in the deep posterior compartment of the lower leg with all the tibialis posterior and the flexor digitorum longus (FDL). All three tendons of the muscles emerge on the medial ankle to form what is known as ‘Tom, Dick and Harry’ (Tib Post, FDL and FHL). The tendons course through the tarsal tunnel on the medial side of the ankle and the FHL continues under the arch of the foot to insert onto the underside of the big toe. The FHL classes very closely into the posterior process of the talus, through the fibro-osseus tube across the medial calcaneus and the inferior part of the sustentaculum tali of the calcaneus. The FHL limb then crosses the FDL tendon at the Master Knot of Henry (also a source of impingement and irritation). This can also represent a site of friction. Cadaveric studies also show that in some people an attachment slip of the FHL muscle moves inferiorly to the anterior ankle (this has sometimes been known as the 'beef of their heel'). This accessory slide of muscle can also be irritated and impinged in the back of the ankle. FHL InjuriesStenosing tenosynovitis of the FHL is very common in ballet dancers on account of the replicate plantar flexion position that ballet dancers get into. This causes the tendon to constantly friction and interrogate against the bony structures of the talus and calcaneus. The identical difficulty has also been reported in athletes who spend a good deal of time in plantar flexion for example leaping athletes, equestrian athletes and space runners between numerous mountain runs. The tendon of the FHL can also develop nodules and little intrasubstance tears. What compounds these problems from the thoracic as it courses around the back of the ankle is the existence of a bony os trigonum that functions as a possible source of impingement into the FHL tendon. Of further interest is that the uncommon muscle-tendon arrangement of the FHL that can project deep to the anterior ankle. The musculotendinous junction may become thickened and entrapped in the fibro-osseous tunnel -- the cork from the bottle syndrome. Finally, injuries to the FHL musculo-tendinous junction and FHL limb has regularly been reported on MRI in post-ankle sprains. The mechanism of injury for this makes sense when one believes that the usual plantar flexion/inversion mechanism of ankle sprain will impinge the tendon in the posteromedial ankle and possibly harm the tendon and sheath construction. DiagnosisOften the pain at a FHL tendon begins insidiously and is found in the postero- medial ankle and it might radiate distally to the lateral arch (often being confused for plantar fasciitis). Often these patients are not going to have the early morning pain and stiffness evident with plantar fasciitis, so these may be utilized as a diagnostic tool in identifying FHL tendon injuries versus plantar fasciitis. Swelling may be present in the medial ankle and the presence of a positive Tinels sign (tapping the posterior tibial nerve which reproduces foot tingling) are also evident. The imaging methods of choice at FHL injuries is MRI to visualise both muscle and tendon injuries and tenography for tendon issues like stenosing tenosynovitis and stomach tears. En pointe lateral foot x-rays are required in dancers to exclude anterior impingement syndromes. Dynamic ultrasound of the FHL tendon may also demonstrate a stenosis of the thoracic or a low-lying attachment slide of the FHL muscle. TreatmentNormally the conservative management of FHL tendon problems originally involves modified action, NSAIDS, protective arch strapping with hallux dorsiflexion check straps, trigger point releases of their FHL muscle, direct strengthening of their FHL correction and muscle of any subtalar or talocrural joint dysfunctions. To stretch the FHL, the foot is placed up against a rolled towel or step so that the ball of the foot is on the floor however the big toe is forced to dorsiflexion. Then bend the knee and knee to spend the ankle into dorsiflexion. Push the foot against the towel resistance into ankle plantar flexion and big toe plantar flexion. Surgical treatment in the form of surgical tendon sheath discharge was proven to be successful in treating chronic stenosing tenosynovitis. The most common site of stenosing tenosynovitis is at the posterior area of the ankle in which the tendon courses around the talus. Os trigonum excision has additionally worked well if the os is your source of impingement into the tendon and the sheath. ConclusionFHL tendon injuries are a common injury in professional dancers, less common in athletes and almost non-existent in non-athletes. It can be impinged by continuous plantar flexion positions particularly if the ankle has a sizable or medially displaced os trigonum or when the muscle belly of the FHL jobs deep down into the posterior ankle. Impingements poor to the ankle and at the arch are much less common. The case study presented highlighted an unusual but intriguing mechanism of harm into the FHL muscle building. Wearing shoes which are too large will create a 'sliding' or ' 'shear' of the foot in the shoe. This may result in excess FHL action as the big toe 'grips' the shoe to prevent this excessive sliding and shear.
Science based chiropractor, Dr. Alexander Jimenez has a look at the legends and the realities of this very common injury. IntroductionThis paper targets one of the most famous body part injuries -- the Achilles tendon (AT). Injuries to the AT possess a somewhat mythical foundation. It is highly likely that the legendary Greek warrior Achilles ruptured his AT when shot by the bow fired by Paris, King of Troy. A sudden heel drop at a bud hole whilst conducting, a quick take-off in tennis or a sudden hop are mechanics that usually cause tendon rupture. Due to the exceptional strength of the AT, it's been suggested that rupture of the tendon is almost impossible without prior degeneration from the tendon, and that, coupled with a high mechanical force that's essential to rupture the tendon, may account for the greater incidence in the 30-40-year-old age category. Only recently has surgery on the AT become the preferred choice of treatment. It was just following the First World War that surgery was attempted on a ruptured tendon; prior to this, distinct kinds of immobilization was utilized to attain a favorable result in a ruptured AT. In contemporary sports medicine, a lot more is known concerning the histological and biomechanical influences in AT rupture and much more is also known on the outcomes of surgical versus non-surgical repairs of this tendon. This paper will present an in-depth explanation on the human anatomy and biomechanics of the AT, how an AT could be deciphered, what are the presenting symptoms and signs and the way the injury is best handled and rehabilitated. AnatomyThe AT is the biggest tendon in the human body. It's formed from the conjoined tendons of the gastrocnemius and soleus muscles. The gastrocnemius extends downwards towards the heels and combines together with all the AT about 11-26 cm over the heel bone. The soleus extends further down to combine using the AT about 3-11 cm over the heel bone. Furthermore, the tendon of the vestigial plantaris muscle also blends with the AT on the medial side of the tendon. Since the tendon runs down to the heel bone it rotates 90° so that the gastrocnemius muscle fibers turn into operate anterolaterally and the soleus fibers turn to run posteromedially. The AT continues to the heel bone and inserts onto the calcaneus. It spreads because it approaches the heel bone so that it's wider at its insertion than at its own mid-portion. A little bursa sits posterior to the AT insertion and it protects it from any rubbing against an external surface (such as a shoe). The mid-portion of the tendon is the most interesting since it's postulated that it is here that a relative avascular zone exists that may result in a rupture zone. As the thoracic receives a blood supply from the north side through the muscle and also on the south side via the heel bone insertion, the mid-zone between the 2 areas signifies a 'water drop' zone that has poor arterial nutrition. The arterial supply in this mid-zone comes from the fatty tissue that surrounds the tendon. With high mechanical pressure in the shape of tensile and compressive pressure, the tendon fibers can break down and degenerate. Due to this comparative avascular nature of the tendon inside this zone, the thoracic may enter a state of disrepair and become diminished and thus act much like a frayed rope which eventually snaps. At length, the tendon is coated by a thin paratenon and epitenon and doesn't have a true synovial sheath. These structures include fatty tissue, thin membranes, blood vessels and connective tissues. These anatomical structures are also subject to harm and may be a source of pain in the AT. Biomechanics Of The Achilles TendonIt has been suggested that if it had been possible to dissect a healthy AT and bolt it to the ceiling, it would be possible to hang on a one-tonne weight before it would fail and rupture. Under load it will stretch and presume that a linear orientation. This happens at as little as 2% elongation, is subject to elevated load at 4 percent elongation along with the tendon will neglect macroscopically at 8% elongation. The cross-sectional area of the tendon is correlated to the magnitude of the calf muscle complex and also height and age of the individual; that's is, the larger the calf and/or the individual, then the larger the tendon. The tendon (such as all tendons) is subject to loading and certainly will change and alter its internal architecture depending on the loads imposed upon it. It'll undergo hypertrophy in exercise-induced wealthy situations. Histologically, the tendon is constituted of extracellular proteins such as elastin, proteoglycans and other molecules as well as fibroblasts (collagen manufacturers). The turnover time for this type 1 collagen is slow, and it takes about 50-100 weeks to the tendon fibers to flip over. Hence a balance exists between breakdown and synthesis in the veins that are healthy. It speeds up synthesis during growth spurts and following injury and it slows down through immobilization. This histological fact modulates the clinical choice to avoid long periods of immobilization post harm and to promote early movement from the thoracic to stimulate synthesis. The tendon increases its potency from adolescence until about 30 years of age, after which it steadily declines in strength. It's believed that it is only about 60 percent as strong at age 60. Therefore, gross stomach injury happens in the over-30-year- old group and it's this group that endures the high percentage of tendon ruptures. Types Of InjuriesThere are quite a few possible pathologies that behave on a continuum in the event of an Achilles tendon rupture. The initial pathology is usually an irritation of the peritendon that develops into an injury to the tendon substance. As the tendon becomes more damaged, it will weaken and may then finally rupture. The defining features of these pathologies are: 1. Peritendinosis a. Edema and scarring of paratenon (fatty areolar tissue around tendon); b. Acute pain and swelling; c. Seen in runners who increase distance or change surface. 2. Tendinosis a. Intra-substance degeneration of tendon; b. Occurs when the tendon is subjected to high cyclic loads and does not repair between loads. 3. Tears (partial or complete) a. Vulnerable zone of avascularity 2-6cm above calcaneal insertion. DemographicsThe normal sufferer of an AT rupture is a 35-40-year-old male. Males rupture their ATs in a ratio of 10:1. This might be partly hormonal and mostly behavioral (that is, this age group may generally still be quite active). AT rupture in this age category is much younger than in other tendons such as the supraspinatus from the shoulder which will dominate from the 50+ age category. In the end, AT ruptures can often happen in middle aged men who have had some time away from competitive sport for a 5-10 year period who subsequently return to social sport. Ball sports like tennis and basketball have a tendency to control the cohort of those suffering an AT rupture since these sports involve abrupt dorsiflexion or plantar flexion force from a dorsiflexed position. Common offending functional moves might be stepping right into a pot hole, sprinting off the baseline in landing or tennis and leaping. This mechanical force is usually coupled with a degenerative element that ends in a weakened tendon because of repetitive micro-trauma and hypovascularity of this tendon. The inherently weaker limb using a sudden implemented force then ruptures. Interestingly, professional athletes only form a small fraction of those suffering rupture, together with recreational athletes comprising the majority of ruptures. Furthermore, it has also been proven that quinolone antibiotics and long-term corticosteroid use might increase the risk of tendon rupture. Finally it's been found that the COL1A1 TT genotype protects an athlete from an acute soft tissue rupture, AT ruptures included. This could drive future studies in using chemical analysis to predict high risk groups for tendon rupture (Collins et al 2009). Signs & SymptomsSubjective The vast majority of acute ruptures clarify no preceding symptoms of malfunction or pain from the Achilles. Although Achilles pain isn't a predictive indication of future tendon rupture, the proportion of patients who have pre-rupture symptoms does rise with age. The majority of ruptures are typical with respect to their own symptoms and physical signs and also the mechanism is generally straightforward. The first sensation is really a sharp pain and they may feel/hear a snap- ping sensation. The sufferer will commonly complain that they've taken a hit to the back of the calf as though they have been kicked or hit with a tennis racket. This may replicate a sharp stabbing pain that then subsides to no pain, and it's possible that up to a third of patients have painless ruptures. But, walking can then replicate the pain especially as they try to push off the toes and they will be grossly weak in their push-off. Objective Often the clinician will feel a real difference in the tendon with potential instant swelling where the AT should be. They may observe that the calf muscle can pack up into the calf; however, this may be jaded by swelling and edema after a few hours. The website of this palpable defect is usually 2-6 cm above the heel bone. Functionally they will hobble and find it hard, if not impossible, to push up on the foot. But a percentage of ruptures may be missed since the individual may continue to have the ability to push off using their toe flexors or if the plantaris has been uninjured. This is achieved by squeezing the calf to mimic a jet contraction that then should transmit pressure to the Achilles and make plantar- flexion in the foot. With no Achilles, force isn't sent and plantar flexion does not occur. ImagingIt's also useful for viewing the total amount of tendon available that can allow approximation of the tendon ends with an allograft if surgery is the preferred treatment option. Ultrasound will reveal thickening and hypoechoic areas in partial thickness tears. Full thickness tears will show posterior shadowing (because the sound beam is refracted in the thoracic ends) and also reveal retraction with tendon debris. Ultrasound may also show fat herniation. On the MRI a torn tendon will reveal equilibrium on the T2 picture whereas in degenerated tendons they will show a dark area on T2. Differential DiagnosisAlthough diagnosis of a whole tendon rupture should be relatively simple, a few differential investigations may confuse the examiner. These include: 1. Flexor hallucis longus tendon rupture; 2. Plantaris rupture; 3. Tibialis posterior rupture; 4. Calcaneus fractures. TreatmentConservative cast immobilization The decision to manage a ruptured AT depends on a number of interacting factors. These include: 1. The length of the tendon diastasis (separation) – anything below 5mm diastasis may do well with conservative management; 2. Sport – surgeons tend to lean towards surgery in power athletes (sprinters, foot- ballers, rugby players) as the amount of tendon force encountered due to calf muscle contraction will be high. Although the tendon will still heal quite well if managed conservatively, it is felt that functionally a conservatively managed tendon will ‘stretch’ out and this will affect force transmission across the myotendinous junction. Inactive individuals may do well with conservative management; 3. Age–older patients tend to be less active than their younger counterparts therefore exposure to high tendon force will be less in the older population; 4. Country – it is still common for Scandanavian countries and some European countries to prefer conservative management in AT rupture. Conservative functional management still has great results when compared with surgically-repaired tendons. Thermann and Zwipp (1989) compared 19 operative tendons versus 25 functionally-managed ruptures with a specialized walking boot and also found that results are comparable if the flaw is less than 5mm in length. After 25 weeks, patients in the two groups had complete healing free of re-rupture and the role- ally controlled group resumed sport much sooner than the operated group. Mattila et al (2013) collected information over a 25-year period in Finland and found that the speed of surgically-treated AT ruptures had declined markedly through the years, suggesting that surgeons are leaning towards non- operative treatment more frequently and enjoying good functional outcomes. More modern walking boots together with the capacity to control the angles of dorsiflexion have led the progress of competitive operational rehab in conservative AT management. The standard protocol may be to cast immobilize for 2-3 months and then to remove the cast and employ a functional prop (Aircast or CAM walker) with the ankle originally limited to 10-20 degrees of plantar- flexion (or even utilizing heel wedges in an Aircast) and then gradually opened up (or wedges gradually removed) over an additional six- week interval. Therefore, the individual will be liberated to mobilize normally 8-10 weeks post injury. The subsequent strength program will be like this program described further on in the surgical management of AT rupture. SurgeryThe decision to work to surgically repair a ruptured AT depends on the factors mentioned above under conservative management. In the end, if the clinical decision for surgery is indicated, the results are fairly similar to conservatively managed patients. The kind of operation used and the immediate immobilization protocol will fluctuate depending on the surgeon and the anticipated compliance of the patient. It's common practice now to allow operational mobilization post-surgery through use of a functional walking boot (see Aircast previously). Surgery followed by early mobilization at a functional walking boot has shown better results than just immobilizing the tendon using a cast for 2 weeks. Early mobilization reduces re-rupture rates and also individual compliance is better using a practical walking boot. The post-surgical limb is braced at a situation of plantar flexion originally to offload any stretch to the tendon via the use of heel wedges, and the wedges have been gradually removed over the interval the practical boot is worn. When the boot is eliminated, it is frequently suggested that a single wedge is utilized and slowly removed two months after removal of this boot. Most surgeons will utilize one of two variants for surgery: either open or percutaneous. The vast majority of surgeons will urge post-surgical blood thinners (warfarin) and antibiotics. RehabilitationThe approved time frame to come back to pre- accident levels ranges from 5-9 months depending on the athlete. Just like most long-term rehab protocols, the rehab stages can be broken down into progressive six-week stages (described below). The particular goals post- surgery are: 1. Range of movement This is purposely limited initially to allow full tendon healing; therefore, the patient will be functionally limited to avoid dorsiflexion in the early stages. However, long term the range of movement does return quickly and it is uncommon to suffer long-term stiffness in the AT. The biggest threat to a good outcome is tendon elongation, thus it is important to limit dorsiflexion range in the early part of the rehab process. 2. Strength This is the most significant complication of an AT rupture. It is important to start some gentle isometric calf exercises early in the rehab process and to progress the calf muscle contractions quickly through the rehab process. It is not uncommon to see a permanent 10-30% strength deficit from the non-affected side. 3. Function The earlier post-surgery the patient is able to weight bear and mobilize safely in a walking boot, the less complication they will have when they start running. ConclusionAT rupture is a relatively uncommon long- term accident suffered primarily from the 30-40- year- old male. The causative factors include pre-existing limb degeneration combined with high mechanical pressure due to forced dorsiflexion and/or strong plantar flexion from a dorsiflexion posture. Therefore it's more widespread in mid sized runners, tennis players and basketball players. The AT rupture may be handled either conservatively through utilization of a practical boot such as an Aircast boot or CAM walker, or operatively via a number of surgical options. In either case, the rehabilitation period is protracted and may take as little as five months or as long as nine months based on type of direction and physical characteristics of their athlete and the game involved. The key feature of return to game post- injury will be gross strength, tendon elongation and how these influence on purpose. The majority of post-injured AT ruptures return to game within six months and the risk of re-rupture is comparatively tiny. References
1. Thermann H and Zwipp H (1989) Achilles tendon rupture. Orthopade. 18(4); 321-333.
2. Mattila et al (2013) Declining incidence of surgery for Achilles tendon rupture follows publication of major RCTs: evidence-influenced change evident using the Finnish registry study. British J of Sports Medicine. 0; 1-4.
3. Collins et al (2009). The COL1A1 gene and acute soft tissue ruptures British Journal of Sports Medicine. 44; 1063-1064.
Swimming is renowned as a fantastic all-round sport with a low risk of injury -- but this doesn't equate to 'no' danger. Scientific chiropractor, Dr. Alexander Jimenez looks at what the current study has to say. Swimming is a really low-impact sport where the loading is spread across a wide range of muscles and joints: hardly surprising, therefore, that it is often recommended since the low-injury threat sport for a vast range of participants. However, the low-impact nature of swimming does not signify that swimmers -- especially aggressive swimmers -- are immune from injury risk. A glance at some numbers shows why: in a typical two-hour swimming session, an elite-level competitive swimmer could normally be anticipated to swim between 5,000 and 6,000 meters. This soon mounts up, with many competitive swimmers clocking up an average yearly mileage between between 20 and 40 kilometers -- that the aerobic equivalent of conducting 80 to 160 miles! Broken down to limb movements, the figures are even more startling. On a typical training day, an elite swimmer can be expected to perform between 1,500 and 4,000 stroke cycles, which equates to anything up to 1,000,000 stroke cycles per training year(1,2). And because female swimmers, normally, have shorter arm strokes, they can execute an additional 660,000 stroke cycles per year -- ie over a 1.5 million annually(3)! The causes of shoulder pain (that we'll look at in more detail later) are multifactorial but include the athlete's gender, their swimming experience, training space, stroke choice and workout intensity, the total amount of hand paddle use (that increases loading), and their upper-body strength and flexibility, and of course their prior trauma history(4,5). Prevalence Of Shoulder PainSince then, other studies have looked into the incidence of shoulder pain among swimmers. A 1998 survey by McMaster and his colleagues looked at the correlation between shoulder laxity (see Box 1) and pain that interfered with instruction in a sample of competitive swimmers(7). It found that 35 percent of senior federal and Olympic swimmers experienced shoulder pain which prevented them from training efficiently. Other studies have variously noted that shoulder pain is the most frequent esophageal injury in swimmers, with a reported prevalence of between 40 percent and 91%(8-13). Meanwhile, a 2012 study looked in the risk factors associated with shoulder pain and disability throughout the life span of competitive swimmers(16). The swimmers answered questions about any other game they participated in and the quantity of swimming training they played on a weekly basis. Data was also gathered about the amount of months per year that they practiced and the number of years they had engaged in competitive swimming. This information was subsequently correlated with the amount of shoulder pain that the swimmers experienced and how much Feedback this caused them. Pain was rated in rest, with regular activities (eating, dressing, bathing etc), and with strenuous pursuits. The DASH sports module instructs participants to rate four objects (physical ability with sport technique, participation, satis- faction, and frequency), using a five-point scale, with '1' indicating no difficulty along with '5' signaling unable to participate within the last week. Furthermore, several of physical steps were taken, including: - passive range of movement (PROM) of both shoulders using an inclinometer for shoulder flexion in neutral rotation with the participant lying supine
- shoulder flexion, with the elbow maximally flexed for long head triceps tightness
- shoulder flexion, with the humerus externally rotated, knees and hips flexed, and abdominal muscles actively contracted for latissimus dorsi tightness
- internal and external rotation, with the shoulder abducted to 90 degrees
- maximal isometric force production for internal and external shoulder rotation with the participant lying prone and the shoulder abducted to 90 degrees
- scapular motion patterns during shoulder flexion and abduction, where the researchers looked for winging or dysrhythmia (using the scapular dyskinesis test – SDT)
- core muscle endurance using the side bridge, the prone bridge and the closed kinetic chain upper extremity stability tests (see Figure 1)
- pectoralis minor length measured from rib 4 to the coracoids process in a normal standing position (pectoralis minor length at rest) and when under- going a stretch.
When the data was examined, several findings emerged. Primarily, it was clear that the issue of shoulder pain was very common indeed. Twenty-one percentage of swimmers aged 8 to 11 decades, 18.6% of swimmers aged 12 to 14 years, 22.6% of high school swimmers, and 19.4 percent of masters swimmers had shoulder pain and disability. Of these, high school swimmers were the most symptomatic and incurred the greatest load in terms of hours swum a week and annually. Across all age groups, shoulder pain issues and disability increased with enhanced upper extremity usage -- either via swimming or water polo. Meanwhile, participation in another game -- particularly football in youngsters and walking or running in older swimmers -- diminished the amount of shoulder pain and impairment. The predisposing variables towards pain were not the same across all age groups; symptomatic swimmers who were less than 12 decades old tended to have diminished shoulder versatility, feebleness of the middle trapezius and shoulder internal rotators and latissimus dorsi tightness. By comparison, symptomatic swimmers that were 12 years of age or older tended to have pectoralis minor stimulation and decreased core endurance. Shoulder Pain CausesAs was mentioned earlier, the reason behind shoulder pain in swimmers is very often multifactorial and includes(17,18): - incorrect stroke biomechanics
- overuse and fatigue of muscles of the shoulder, scapula, and upper back
- glenohumeral laxity with subsequent shoulder instability.
However, to fully appreciate the stresses experienced in the shoulder region area, it's helpful to break down the biomechanics throughout the stroke activity. The front crawl is the fastest and most efficient stroke through the water, which is why it is universally used in a diverse assortment of contest environments like pool swimming pool, open-water swimming and triathlon. It's also the stroke most utilized during exercise swimming sessions. Figure 2 shows the four stages of the front crawl stroke, the position of the shoulder in every stage, and then muscles are all loaded. What's apparent is that even with near flawless stroke procedure, there's ample opportunity for a shoulder injury to develop. Impingement, Fatigue & LaxityImpingement -- Shoulder impingement in competitive swimmers is usually brought on by altered kinematics because of muscle fatigue or laxity instead of pathological changes, which can be observed in other patient populations. Subacromial impingement can occur when the bursal surface of the rotator cuff impinges from the anteroinferior acromion. At the point when the hand enters the water, the hydrodynamic force applied on the hand by the water creates a massive moment in the shoulder joint, causing elevation of the humeral head and following impingement. The hyperextension of the upper extremity in the late pull-through phase (submerged portion) of the stroke compels the humeral head anteriorly and moves it internally, which may aggravate an impingement when muscle fatigue is currently present. Muscle fatigue -- Because the shoulder is an inherently unstable joint, adequate muscle strength is vital in order to maintain stability, appropriate stroke appropriate movement, and painless function. Much of the propulsive force in swimming is generated by adduction and internal rotation of the upper extremity due to pectoralis major and the latissimus dorsi muscles. Unfortunately, the training-induced adduction and internal rotation strength in swimmers can cause a strength imbalance, which leads to decreased glenohumeral stability. The reason for this is that the teres minor muscle provides an external rotation pressure and stabilizes the humeral head in combination with the pectoralis major. The repeated contraction of those smaller stabilizing muscles during swimming makes them prone to exhaustion, increasing instability since they are less able to counteract the forces produced by the larger pectoral and latissimus muscles. Laxity -- In most competitive swimmers, shoulder laxity with enhanced lateral movement of the humeral head could be seen(18). Although, there might be a hereditary element on the job in these swimmers, just around 20 percent of the subgroup meets the criteria for generalized ligamentous laxity(19). It's more probable the laxity increases over time as a result of continual overuse during competitive swimming. A certain level of glenohumeral laxity may be advantageous by allowing a swimmer to achieve both a body posture that reduces drag and a greater stroke length, both of which may help boost speed through the water. However, the diminished passive stability given by the glenohumeral ligaments in much more lax shoulders means that a greater contribution in the thoracic muscles is required to control the glenohumeral translation. This might cause muscle overload and subsequent muscle fatigue, with all the issues described previously. Some common tests used to identify frequent shoulder pathologies in competitive swimmers are displayed in Table 1 below. Shoulder Pain PreventionAs well as optimizing stroke biomechanics (see Box 2), a comprehensive program of stretching, strengthening, and endurance training ought to be considered as an essential part of each competitive swimmer's instruction program. Since musculoskeletal injuries in swimmers undergoing heavy training loads normally result from cumulative, repetitive injury, so it is critical that coaches and physicians carefully track each swimmer's training volume, intensity, and duration. This can help to minimize overuse injuries and identify people at risk. Endurance training of the heart muscles is a vital part in any injury prevention program. Therefore, abdominal strengthening should be emphasized from the dry-land training program, the aim of which is to develop increased control of the pelvis by preventing excessive anterior pelvic tilt and lumbar lordosis, which in turn will enhance body alignment in the water. Meanwhile, scapular muscle strengthening can also be recommended to help improve glenohumeral stability. An endurance training and strengthening program for your shoulder and periscapular muscles, with emphasis placed on the serratus anterior, rhomboids, lower trapezius, and subscapularis, may assist in preventing injuries(17). Individual swimmers should be evaluated to determine endurance, strength, or flexibility shortages. As soon as any swimmer experiences increased shoulder pain, their training program needs to be altered accordingly: - Warm-ups should be extended with reduced intensity;
- The intensity, distance, and frequency of any subsequent training should be reduced;
- Painful strokes or positions (typically freestyle and butterfly) should be temporarily avoided (absolute rest is rarely indicated because it results in rapid de-conditioning of the elite swimmer);
- Hand paddles and pulling sets should be discontinued as they place stress on the shoulder and can exacerbate any injury;
- As an alternative, kick boards may be used with the elbows flexed to prevent shoulder impingement (this position may need to be modified to avoid forward shoulder elevation);
- Fins may also be used to maintain good body position while decreasing upper body stress;
- Pull buoys may also be useful as they can change the position of the shoulder in the water and reduce drag;
- Dry-land upper extremity weight training should be modified or eliminated;
- A strap placed around the upper arm over the biceps muscle (counterforce strap) may be useful to diminish the loading on the tendon.
Stretch Or Not?Finally, it is worth mentioning extending. Most swimmers stretch but there is evidence that stretching may be more detrimental than useful(20). For example, the majority of the stretches which swimmers do stretch the lateral capsule of the shoulder. If the capsule is overstretched, the risk of uncertainty and subsequent injury increases, maybe permanently(19). Any extending, therefore, ought to be specific to the patient and designed to correct particular muscle or capsular tightness. Because swimmers generally have a relatively tight posterior capsule, which may encourage impingement pain, swimmers without pain should concentrate on extending the posterior capsule and anterior torso muscles. To selectively extend the posterior capsule without even stretching the scapular stabilizer muscles, it is necessary to stabilize the scapula. The easiest way to do so is to stretch the shoulder while lying supine, partially rolled onto the lateral border of the scapula. In swimmers who've kyphotic posture due to tight anterior chest and shoulder musculature, stretching those muscles without stretching the anterior capsule helps reduce the forward shoulder posture and increase the subacromial area(5). Swimmers with shoulder pain ought to be instructed to stop all anterior capsule extending and rather focus on posterior capsule extending. Swimmers with multidirectional instability or a background of subluxation should steer clear of all extending -- notably 'spouse extending' -- because it can easily force a shoulder beyond its normal limit and promote additional anatomic damage(19). For swimmers in whom extending is contraindicated, a gentle warm-up is sufficient to increase blood circulation to the muscles and get ready for the workout. SummaryCorrect stroke technique is crucial to help prevent harm and trainers should ensure that they carefully track training loads and identify stroke adjustments that may cause or change pain. Abdominal, core, scapular, and rotator cuff muscle strengthening exercises should be highlighted in a accident prevention program, and should the swimmer experience any shoulder pain, training intensity, distance, and frequency ought to be adjusted accordingly. Stretching is only recommended when a particular need has been identified. References
1. Am J Sports Med 1997;25(2):254-260
2. Clin Sports Med 1999;18(2):349-359
3. Scand J Med Sci Sports 1996;6(3):132-144
4. Clin Sports Med 2000;19(2):331-349
5. Sports Med 1996;22(5):337-347
6. Orthop Clin North Am 1977;8(3):583-591
7. Am J Sports Med 1998;26(1):83-86
8. Clin J Sport Med. 2010;20(5):386-390
9. Am J Sports Med. 1997;25(2):254-260
10. Scand J Med Sci Sports. 2007;17(4):373-377
11. Clin Sports Med. 1986;5(1):115-137
12. Br J Sports Med. 2010;44(2):105-113.
13. Int J Sports Med. 1995;16(8):557-562.
14. Stedman’s Concise Medical Dictionary for the Health Professions, ed 3. Baltimore, Williams & Wilkins, 1997, pp 446-446, 480
15. Arch Orthop Trauma Surg 2002;122(8):472-487
16. J Athletic Training 2012:47(2):149–158
17. Rodeo SA. Swimming. In: Krishnan SG, Hawkins RJ, Warren RF, eds. The Shoulder and the Overhead Athlete. Philadelphia, PA: Lippincott, Williams & WIlkins; 2004:350
18. Clin J Sport Med. 1996;6(1):40-47
19. Orthop Clin North Am. 2000;31(2):247-61
20. Physician and Sports medicine 2005; vol 33, no. 9
|
For many athletes following any major endurance event they will return to their houses, to recover, celebrate, reflect and rebuild to their next career step. Some, like the athlete in this case study will need to now focus attention on delayed decisions concerning whether to go under the knife to sort out a chronic injury. El Paso, TX's Injury scientist, Dr. Alexander Jimenez takes a look at the study. My client has been competing in triathlon for 10 or more years, although his career has included a range of serious injuries which have kept him from races for months on end. In the previous two to three decades, however, he's enjoyed a sustained period of injury-free training and racing, and has climbed to the peak of the world rankings. But the emergence of hip pain has seen him once more return to the physio's table. The triathlete's accident history highlights a common pattern among sportspeople: 2 tibial stress fractures, a femoral neck stress fracture and a serious ankle sprain -- every one of these on his right side. The significant contributing element to the bone stress injuries is a 1.5cm leg-length gap (his right leg is shorter). He'd first experienced comparable hip pain in 2004; it kept him from running for three months. At that time, nothing was detected on a bone scan or MRI, or so the pain went paralyzed. An intra-articular cortisone injection (CSI) elicited no improvement. The athlete remembers that he chose to train on his painful hip, never allowing the symptoms to settle. The nearest he ever came into an investigation was a hypothesis that he could have a little, undetected, labral lesion. The present episode of hip pain began initially at night after a hard three-hour bicycle ride. Earlier this, however, he hadn't cycled for five times. He described his initial symptom as a profound hip tightness (lateral and lateral), together with slight pain in his groin. He was able to continue to train however, was feeling that the hip tightness and pain following both cycling and running (swimming was symptom-free). A week later his symptoms dramatically worsened when he flew from Australia to Singapore, on his way to a French high- altitude camp. As he got off the airplane, he felt deep hip pain as well as the tightness. As elite athletes tend to do, he coached anyway, running a tricky track session, which made the hip much worse: he was unable to ride or run without pain. He instantly started a course of anti- inflammatories. I met him in Singapore and evaluated him in the airport, initially ruling out any prospect of a disease or systemic matter. He explained he had been feeling an ache during the night, lying in bed; on waking, the hip would be OK, but got worse the longer he walked. On assessment, he had the following physical signs: • walking with obvious limp
• pain on hopping (6/10)
•painful right hip quadrant/impingement test (full hip flexion/adduction)
• reduced right hip flexion (-10 degrees compared to left)
• reduced right hip internal rotation (-10 degrees compared to left)
• increased tone on palpation of TFL, adductors, hip flexors, gluteal, piriformis and deep rotators
• lumbar spine and SIJ were OK
• femoral shaft bone stress test was OK • leg length discrepancy (right side 1.5cm shorter)
• right innominate (pelvis) anteriorly rotated
• weakness in right hip abductors/extensors
• reduced calf endurance on right side (-5 reps)
• ankle dorsiflexion range of movement was OK
• reduced proprioception on right (single leg stance, eyes closed). I thought the differential diagnoses were: • femoral neck stress fracture • labral tear, possibly with hip synovitis • FAI (femoro-acetabular impingement), possibly with hip synovitis. I initially treated the triathlete with soft- tissue techniques to reduce the tone around the hip joint. Trigger-point releases were performed on his TFL, adductors, gluteals, piriformis, deep rotators and iliopsoas. This reduced his jump pain into 3/10. Manual long-leg grip further decreased the strain on hopping (2/10). He still had pain and stiffness on walking but it sensed "simpler. As he prepared to embark on his long run flight to Europe, I counseled him to not sit for too long and maintain his stylish as straight as possible to decrease any potential impingement from hip flexion. Luckily, the hip didn't get worse throughout the flight. On arrival at the French high-altitude training centre, we initiated a strategy of two swims and two intensive treatments a day, aiming at reducing muscle tone, restoring his range of hip movement and normal muscle control and stamina. We had been expecting that the problem was not a stress fracture, but just minor hip synovitis that could settle quickly. Following a week of conservative treatment, though, we were just able to keep his hop pain in 2/10, and that he still could not run 20 meters without any pain and limping. In collaboration with medics, we flew to London to see a sports doctor and get MRI scans. The scans revealed no bone stress reaction, fracture or labral ripping -- which was a big relief; however, it did show signs consistent with FAI (femoro-acetabular impingement). He had hip synovitis with a rectal lesion on his femur. Hip injuries aren't much reported among triathletes -- in fact they are notably absent from reports on Olympic and Ironman triathlons, which mention knee, back, H/ Achilles, lower leg, ankle and shoulder as the most common accidents (1-3). In this state, when the hip is in maximum flexion and internal rotation, the labrum and cartilage abut and impinge; damage to the articular cartilage and acetabular labrum results from this pathologic bony contact. The contact generally results in a structural abnormality of the femur ("camera impingement") along with the acetabulum ("pincer impingement") or a combination of both ("mixed impingement"). Over time, via repetitive micro-trauma, the aggravating motion hurts the hip cartilage or labrum (or both) during normal joint motion. This happens along the anterior femoral neck and the anterior--superior acetabular rim. FAI is a possible trigger of early hip joint degeneration (4). Arthroscopic surgery is the direction of choice for FAI if symptoms do not settle; however as his next Competition was only three and a half a year off, surgery was not an option. Instead, over a five-day interval, the athlete had two cortisone (CSI) and local anesthetic injections into the hip joint (under ultrasound guidance) to settle the indicators. Our aim was to grow the hip range of motion and extend the capsule to reduce any additional impingement, slowly returning to regular training. Following the competition, the athlete would then should see a hip arthroscopic surgeon to acquire a surgical opinion to the best option for long-term direction. Injection ReliefAfter both shots my customer felt sore for five days. The initial CSI settled his pain on hopping to 1/10 and after seven days he managed to operate without symptoms. But minor hip stiffness and aching at the end of the day prevented him from progressing to optimal training, so that he then underwent a second steroid injection. This settled the hop pain into 0/10 and decreased the aching; so after five times he returned to mild cycling and after seven days he started running again, also. The athlete admitted that, following the first shot, he had done more and gone tougher in training than directed, as he had felt "good. This mistake of "too much too soon -- all too common in elite athletes -- had led to excessive inflammation and aching in the hip nightly after training. After the next injection he returned to normal intensity slower and more gradually. My client built his training up to regular levels by four months following the final injection (swimming five times per week, cycling four days and running six to seven days). He began with very easy cycling on a wind trainer for 30 minutes, building slowly to 90 minutes before cycling on the street. He cycled two days on and one day away and avoided hills to the first two weeks. He started jogging on the apartment for 15 minutes and slowly built up to 90 minutes after three weeks. He did not run hills or about the track; and as he ran only on every single day, he would diligently concentrate on technique. From week six to week 11, my client remained on anti inflammatory medication and underwent two treatments a day. The hands-on treatment continued to: • increase hip range of movement
• stretch the hip capsule
• normalise pelvic symmetry and hip muscle tone
• improve muscle control and strength • improve proprioception
• ensure optimal biomechanics via video assessment (cycling and running). Eleven weeks after he first felt his hip pain, the triathlete returned to racing; however he failed to finish the first race, partially because of minor hip stiffness but mainly due to "fitness. Fortunately there were not any prolonged symptoms after the race and a week after he successfully returned to competition, coming second in a really strong field. His very minor ongoing symptoms were handled with anti-inflammatory drugs and hands-on treatments. If this athlete wants to pursue a long- term triathlon career up to the London Olympics, then he will now require surgery. The arthroscopic surgical technique initially assesses the cartilage and labral surfaces, debrides any abnormalities of the hip joint cartilage and hip labrum, removes the non-spherical segments of the femoral head and any prominent sections of the anterior femoral neck and bony growths on the acetabular rim that may continue to contribute to hip joint impingement. The alternative is early joint degeneration and onset of osteoarthritis. References:
1. Wilk B et al: “The incidence of musculoskeletal injuries in an amateur triathlete racing club”. J Orthop Sports Phys
Ther 1995 Sep;22(3):108-12.
2. Collins K et al: “Overuse injuries in triathletes. A study of the 1986 Seafair Triathlon”. Am J Sports Med 1989 SepOct;17(5):675-80.
3. Korkia PK et al: “An epidemiological investigation of training and injury patterns in British triathletes”. Br J Sports Med 1994 Sep;28(3):191-6.
4. Ganz R. et al (2003): “Femoroacetabular impingement: a cause for osteoarthritis of the hip”. Clin Orthop Relat Res. 417:112–120. For more information see: www.hipfai.com
A 35-year-old man with what his sports physician described as "left periscapular pain of unknown origin." The sports doctor was hoping that a physiotherapy test and subsequent treatment would settle the symptoms. Chiropractic injury specialist Dr. Alexander Jimenez investigates... This gentleman had a 15-year history of work from the sheeting department of a local hardware store. His job took him to lift and load on to trucks around 200 plasterboard sheets daily. The store man was also an energetic outrigger canoeist, currently in heavy training for an upcoming long-distance event. In outrigger canoeing six paddlers sit at a 14m canoe built of Kevlar, graphite and S glass (a magnesiaalumina- silicate glass with high tensile strength). The kayak design comprises an elongated arm (the outrigger), which helps to balance the canoe in open water. The canoeists use 4--5ft paddles, and possess a specific paddling sequence where they change sides every 15--20 strokes. He described a vague persistent pain in the left periscapular area proximal to the medial edge of the scapula (ie, only by the long border of the shoulder blade close to the spine). The pain was severe enough to be preventing him from sleeping through the night. Upon questioning he stated he thought the pain had been mildly gift for the best part of ten years. Employer records confirmed that he had complained of a similar pain seven decades before but had chosen not to seek treatment, having thought that the symptoms in the time to be too gentle for any intervention. However, the symptoms had lately become far more acute -- to the point where he could no longer physically carry the plasterboard sheets at work. A few days prior to visiting me, the store guy's symptoms had significantly slowed following a lengthy paddling session (20km). The final straw came in the close of the session when group members had to carry the 145kg canoe about 50m to load it on into the back of a trailer. He had been carrying the kayak with his left hand and the pain radiating from his mid spine area had become excruciating. He decided to take illness leave out of work and cease all of his coaching. Upon examination, I could see that he had a very long and gloomy left scapula, with hypertonicity (overdevelopment) in the left posterior shoulder muscles and right-sided paraspinals. The costo-transverse joints of the third to seventh ribs on the left side were especially hypomobile. All active motions of the shoulder and cervical spine were normal selection and all of the muscle tests round the shoulder and cervical spine seemed to offer normal results. The customer described no history of significant left knee or cervical spine injury or injury. He demonstrated that the lift and carry technique he was using with all the plasterboard sheets. He also carried the sheets on his left side with his left arm fully externally rotated and elbow in extension so he could hold the base of the sheet. This activity seemed to force his scapula to a depressed and protracted position. He would then elevate the right arm above his head to hold the top of the sheet. In this manner he can "hang the sheet off his left arm, together with his right hand to balance it. On palpating the offending area, I found he had two spots of exquisite tenderness. The first was just under the medial edge of the scapula; the second on the rib angle of the fourth or fifth rib. Due to the severity of his symptoms, the night pain and point tenderness about the rib angle, I called him to get further investigation (x ray and bone scan) to rule out any stress fractures of the rib. The x-rays came back negative, so I guided my therapy at mobilization, muscle energy techniques to address the rib hypo-mobility, and soft-tissue therapy and acupuncture for the rhomboids, back shoulder and upper trapezius. Following two weeks my canoeist showed no improvement in symptoms and his night pain continued. I referred him for a CT scan to rule out degenerative changes in the thoracic spine, costo-transverse or costo-vertebral joints. So two weeks farther on, without a clear diagnosis and no actual improvement in symptoms, I routed the store guy for an MRI scan to rule out any additional soft-tissue harm to rhomboids or middle trapezius, and to investigate the cervical spine to exclude virtually any radiculopathies in that area that might mimic soft-tissue injury in the periscapular area. After consulting with the referring doctor, we all agreed that the store man could vanish for a while off on a much needed holiday. I sent him off with directions to self-manage the injury, using a tennis ball to the rhomboids, a thoracic roller to mobilize his thoracic spine and some scapular-setting/ stabilization exercises. He returned three weeks later (seven months after his initial trip to the clinic) at exactly the exact same state as when he'd left. Client and physiotherapist both being exasperated with the lack of progress, we decided to take the plunge and see whether the sports physician could diagnostically block the pain, with a regional anesthetic infiltration. The sports physician palpated the painful place thoroughly and determined that the most tender stage was the spot under the lateral border of the scapula, which he believed corresponded to tendon material of their rhomboid. Miraculously, the pain at the periscapular area fully disappeared with the local anesthetic -- despite there was no evidence of degenerative or inflammatory modification on the MRI. The physician followed this up with a corticosteroid injection in the same spot. Fourteen days after the patient was ongoing to become symptom free so we began a progressive rehabilitation program to re-strengthen that the rhomboids and proceeded to handle the thoracic spine and rib joint hypomobility. Following six weeks (16 months from initial presentation), he returned to perform and paddling, and although perhaps not 100% symptom-free, was able to resume sheet- carrying at work and was back into paddling long distances without any ill effects. An Unusual Tendinopathy?Even the rhomboid muscles (minor and major) are described as strong retractors and downhill rotators of the scapula. There is very little from the literature on pathologies affecting the rhomboids, which makes it apparent that these deep bending shoulder muscles are not often injured in either sporting or occupational environments. This case shows that the rhomboid muscle and its bony scapular attachment can be just as vulnerable to pathological tensile and compressive loading as other more common culprits (like Achilles tendon), provided the right mixture of repetitive and traumatic stress. For me this was an extreme blend of occupational and sporting stress that had led to an isolated instance of "rhomboid tendinopathy , although the exact origin of the pain still remains a mystery, as nothing ever showed up on the MRI. Perhaps the magnetic strength of the MRI (1.5 Tesslar) was not powerful enough to pick up high signal density at the rhomboid tendon, or perhaps that the MRI results returned as a false negative, a case occasionally seen in chronic patellar/ Achilles tendinopathies. It seems that the recurrent protraction and melancholy of the scapula brought on by carrying and holding heavy plasterboard sheets over many years -- and exacerbated by the repeated action of the paddling -- had contributed to an inflammatory or degenerative process in the thoracic and attachments of the rhomboid muscle on to the scapula. Upon release the individual still exhibited a somewhat protracted and gloomy scapula. It is likely that this imbalance may never be completely solved with the scapular retraining exercises; the protracted period of time that his scapula was subjected to the unbalancing forces could have led to permanent length-tension changes from the rhomboids and upper trapezius.
Chiropractic back pain specialist, Dr. Alexander Jimenez looks at new study on muscle activation timing in the postural muscles and the implications for lower back pain in sportsmen and women. Lower back pain (LBP) is a common illness among athletes (see Box 1). However, since our understanding of the etiology of back pain has improved, so have the prevention and treatment approaches. A good instance of this has been the growing emphasis throughout the last 15 years on functional training to the postural muscles of the back -- an approach to LBP treatment/prevention that's now quite widely recognized among clinicians and coaches. But though some research has emphasized advantages of the mode of training for those who have back pain and for carrying out regular activities, less research has been done on the benefits of core training for elite athletes and how this training ought to be carried out to maximize athletic operation. Really, there are many articles in the literature which promote core training programs and exercises for performance enhancement with no solid scientific rationale of their effectiveness, particularly in the sporting context. Core Training & Muscle ActivationMany elite athletes undertake core stability and core strength training as part of their training program, despite contradictory findings and conclusions regarding their efficacy. This is principally due to the absence of a gold standard way of measuring core stability and strength if performing everyday tasks and sporting movements. A further confounding factor is that due to the diverse demands on the core musculature during regular tasks (low load, slow movements) and sporting activities (large load, resisted, dynamic movements), study conducted in the rehabilitation sector can't be put on the sporting environment and, subsequently, data regarding core training programs and their effectiveness on athletic performance are lacking. 1 aspect of postural muscle function that has received special attention in recent years is muscle activation patterns. Understanding how a particular sort of movement triggers (or fails to trigger) postural muscles in the trunk is vital to unravelling the part of the postural muscles in trunk stabilization. Much of the initial work in this field has tended to focus mostly on the magnitude and patterns of electromyographic (EMG) activation in postural muscles, and this knowledge has proved invaluable to physiotherapists and sports physiologists looking for a better knowledge of LBP. More recently, there has been a developing interest in the timing of these action, and its connection to LBP. The ability to rapidly modulate the timing of muscles in response to sudden postural perturbations is deemed paramount for maintaining posture and equilibrium, and thus in boosting good lower back health. The literature indicates that, in comparison with healthy controls, besides demonstrating reduced EMG activity, people with chronic LBP also demonstrate delayed activity reaction to both expected and unanticipated postural perturbations(4,5). Moreover, acute experimentally-induced LBP in healthy people has been proven to change trunk muscle activity during trunk flexion--extension, in addition to attaining and quick arm-movement tasks. Simply speaking, sufferers with acute or chronic LBP seem to be at increased risk of further injury in response to unexpected external perturbations(6,7). Timing & PainOne criticism of these kinds of studies was that they employed protocols aimed at approximating 'real-life' perturbations but, in reality, these protocols were not sufficiently realistic to enable meaningful conclusions to be drawn. Nonetheless, these criticisms were answered by a 2011 study by Danish scientists, which examined automatic postural reactions in the presence of experimentally induced LBP to quickly, functionally applicable, complete body perturbations(8). These perturbations were created by a computer-controlled platform which enabled movement in 3- dimensions to generate tilting or sliding perturbations closely mimicking 'tripping over an obstacle' or 'slipping on a wet surface'. In the study, the researchers analyzed the activation of the erector spinae and external oblique muscles in response to unanticipated, bi-directional postural perturbations prior to and after the induction of acute LBP in healthy individuals. Each experimental session consisted of a baseline, control, and also an acute LBP condition. For the management and acute LBP condition, isotonic or hypertonic saline, respectively, was inserted to the ideal erector spinae muscle. In each condition, participants stumbled on a moveable platform during which 32 randomized postural perturbations were conducted. These consisted of eight repetitions of four perturbation types achieved within a period of 4-5 minutes -- 8cm anterior slides, 8cm posterior slides, 10 anterior tilts, and 10 posterior tilts. Throughout those perturbations, bilateral EMG was recorded by the erector spinae and external oblique muscles as well as the subjective pain experienced by these subjects. The results demonstrated that compared to the 'no back pain' condition (control), back pain delayed the beginning time of both erector spinae and external obliques to the forward and backward slipping perturbations (although only the onset time of the erector spinae systematically varied with all the differing perturbation types and directions). It was also evident that in the back pain illness, the EMG amplitude was reduced bilaterally for all perturbations (see fig 1a 1d). The findings of the aforementioned Danish study appear to be encouraged by people from a US study on modified electromyographic activation patterns in response to perturbations of standing balance, also published in 2011(9). In this study, researchers evaluated the intermuscular patterns of EMG activations from 24 individuals with and 21 people with no history of chronic and recurrent LBP in reaction to twelve directions of support surface translations. Specifically, the aim was to characterize more thoroughly the shift in muscle activation patterns of people with LBP in response to a perturbation of standing balance, and to gain insight into the influence of early versus late-phase postural responses (differentiated by quotes of voluntary response times). The results of this experiment indicated that the subjects with LBP exhibited: ● higher baseline EMG amplitudes of the erector spinae muscles before perturbation onset; ● fewer early-phase activations at the internal oblique and gastrocnemius muscles; ● fewer late-phase activations at the erector spinae, internal and external oblique, rectus abdominae, and tibialis anterior muscles; ● higher EMG amplitudes of the gastrocnemius muscle following the perturbation. The authors concluded that a history of LBP is related to higher baseline muscle activation and also that EMG responses are modulated by the activated state, rather than exhibiting acute burst activity from a quiescent state (perhaps to circumvent trunk displacements) as is true in areas without LBP. Late Onset Muscle Activation In AthletesThe research above looked at start activation instances in (differently) healthy but sedentary individuals. But what are the consequences for athletes? Unfortunately, the literature in this regard is very thin on the ground. However, a brand new study published in 2013 has looked in the reflex reaction of shallow trunk musculature in athletes with chronic low back pain(10) to check whether similar patterns of delayed muscle activation onset exist within the athletic body. In particular, the investigators sought to compare long latency reflex response (happening between approximately within 40ms to 100ms) in athletes with chronic LBP against asymptomatic athletes. To do this, 24 athletes with chronic LBP were compared with 25 hepatitis athletes. At the position rankings, perturbations were introduced equally expectedly and unexpectedly while the surface EMG of the rectus abdominis and erector spinae muscles were listed. The latency of the onset of muscle activation and the root mean square (RMS) amplitudes within the response length were compared between the two groups. In comparison with the asymptomatic athletes, the latency of onset has been postponed from the LBP athletes when the athlete underwent unexpected perturbations. However, during the anticipated perturbations, no modification was observed. The investigators went on to conclude that 'chronic LBP athletes exhibit a delay in onset latency to unexpected perturbations and decreased long latency response amplitudes to perturbation tasks compared to asymptomatic athletes. These modifications can induce athletes to recurrent low back pain and further injury.' QuestionsIf muscle activation time is a significant element in LBP, an obvious question to ask at this stage is if a core training program (which often creates the staple of many a lower back injury rehabilitation program) can help normalize muscle activation patterns. There is a paucity of research in this area but a study published in 2012 is revealing(11). In this study, researchers sought to investigate feed- forward activation or timing of abdominal muscle activation in response to rapid spinal flexion following an eight-week plan of core stability exercises, sling exercises, or overall exercises. Of specific interest was the effect on muscle activation onset (listed bilaterally from m-mode ultrasound imaging) at the deep abdominal muscles in response to quick shoulder flexion in the chronic nonspecific LBP patients. In the conclusion of the eight-week instruction period, there were only insignificant or very modest improvements in the LBP subjects. The baseline-adjusted 'between group' differences showed a 15 millisecond advancement with sling training relative to core stability training, and a 19 millisecond advancement relative to general exercise training. To put it differently, eight months of core stability training produced hardly any advancement in the start of abdominal muscle contractions. Conclusion & ConclusionDespite our growth in understanding along with the widespread take-up of core training work, low back pain is still a significant issue among athletes. Recent study on muscle activation patterns suggests that the late onset of stimulation in postural muscles is likely to be a contributing factor in the etiology of chronic low back pain and rehabilitation/ prevention programs relying only on core activation could be insufficient to help normalize postural muscle activity. References
1. Spine (Phila Pa 1976). 2004 Feb 15;29(4): 449-54
2. Neurosurg Focus. 2006 Oct 15;21(4):E7
3. Br J Sports Med. 2003 Jun;37(3):263-6
4. Brain Res 2001; 141:261–266
5. Spine 2000; (Phila Pa 1976) 25:947–954
6. Exp Brain Res 2003; 151:262–271
7. Spine 2007; (Phila Pa 1976) 32:E801–E808
8. Exp Brain Res 2011; 210:259–267
9. J Neurophysiol. 2011 Nov;106(5):2506-14
10. J Back Musculoskelet Rehabil. 2013 Apr 29. [Epub ahead of print]
11. Spine (Phila Pa 1976). 2012 Jun 1;37(13): 1101-8
Injury chiropractic specialist, Dr. Alexander Jimenez Looks in the best ways to monitor and reduce injury within this high pressure, high-stakes world... IntroductionFootball, otherwise known as soccer or association football, is the most popular team game played across the world. The four- yearly FIFA World Cup is the 2nd most watched sporting event behind the Olympics. It is thought that the origin of association football or football (and all the offshoot football sports like NFL, Rugby, AFL etc) started from the Greater Public Schools of England sometime in the 15th and 16th century and evolved to organized sports as they were taken globally around the world through the British Empire. As a consequence of multimillion dollar TV rights deals, the ownership of clubs by wealthy billionaire football fanatics and the unparalleled popularity of soccer, players are exposed to rapidly increasing amounts of professionalism. The ordinary team participant in elite soccer plays 34 games per year, and training intensity levels have increased to match the increased requirement to have fitter and faster players. In essence, the purpose of soccer would be to kick a ball into a goal to score a point. To do this the ball has to be held within the field of play (which holds 11 players per group) with just the goalkeeper permitted to handle the ball within the area of play. The game requires endurance, speed, agility, power and leaping ability, along with a robust musculoskeletal system to defy the rate, turning/pivoting and contact components of the sport. Therefore injury levels in football are high and harms are mostly limited to the lower limb. Interestingly, the amount of potential studies into the epidemiology of professional soccer is relatively sparse. On the other hand, the professional bodies governing the English Premier League (EPL) and the Union of European Football Associations (UEFA) perform conduct long- term harm audits in their respective jurisdictions. Profile Of A Modern Professional PlayerThis study also monitored match and training data to comprehend exposure in the contemporary professional elite footballer. This long- term study collected data on 2,226 gamers within the seven-year interval. What they found over the seven decades of data set was that the ordinary player played 34 games annually and engaged in 162 training sessions. The mean overall per year was determined to be 213 hours of instruction and 41 match hours. It is anticipated that on average each player will endure at least two injuries during the course of the season that will necessitate removal from play or training for a minimum of one day; along with also an elite group of 25 players may expect about 50 accidents per season with half of these minor and resulting in fewer than seven days' absence. A previous study conducted by Hawkins et al (2001) on 91 English football clubs (spread over four branches) over a two-year period found trauma rates to be less at just 1.3 accidents per player in a season normally. They also discovered that slight (two to three times) to moderate injuries (four to seven times) accounted for 68 percent of injuries and acute injuries (more than 28 months) accounted for 9 percent of accidents. Hawkins et al (2001) concluded that handling, being handled and collisions accounts for 38 percent of complete injuries and the remaining 62 percent of injuries are a consequence of non-contact mechanisms. This is quite similar to studies in rugby union (Brookes et al 2005) who also have found that slight injuries (fewer than seven times) account for more than half the total injuries (54%). Injury AttributesVery similar to cohort research in rugby union (Brookes et al 2005), it's evident that game accidents account for the vast majority of injuries suffered by the elite professional player in comparison with instruction. Ekstrand et al at 2011 concluded that although coaching time much outweighed playing/match time a year (212 versus 41 hours) over half (57%) of injuries were really match-related. This represents a significant weighting towards match associated injuries when exposure time is believed (about a seven-fold growth when exposure time is a variable). This is encouraged by Hawkins et al (2001) who found that 34 percent of harms were training-related but match injuries accounted for 63%. Interestingly, foul play in games accounted for 21% of those injuries such as ankle sprains, knee sprains and contusions in the Ekstrand study. Not enough for soccer, 87 percent of all injuries were related to the lower limb. The breakdown of those injuries are as follows (Ekstrand et al 2011): - Thigh injuries 17% (hamstring 12% and quadriceps 5%)
- Adductor strain 9%
- Ankle sprain 5%
- Medial ligaments injuries (MCL) 5%.
Similarly the Hawkins et al (2001) two-year study came up with the following statistics: - Thigh 23% (hamstrings being two-thirds more common than quadriceps).
- Knee 17%
- Ankle 17%
- Lower leg 12%
- Groin 10%
Therefore hamstring injury in the modern professional elite player is the most frequent injury, suggesting that the high- intensity nature of professional European soccer can predispose players to hamstring injuries. This finding is agreement with Wood et al (2004) that found that more than two seasons with four divisions of English football teams involved, they also found hamstring accidents to account for 12 percent of injuries. 1. It involves very little upper-body contact compared to other sports such as rugby and gridiron, therefore trauma and upper limb injuries are therefore relatively uncommon. 2. Footballers cover significant mileage in a game. Prozone data of players in the EPL show that midfield players can cover 10-12km a game, with 1.5km of that at light sprinting to full sprint. 3. Footballers sometimes have to play twice in a week with little recovery between matches. 4. Footballers tend to have very short preseasons due to the competition running into late May, and most clubs will have marketing trips and exhibition matches as part of their pre-season build-up through July. Therefore the opportunity to develop soft-tissue conditioning is limited. Injury VarianceEkstrand et al (2011) found that it was more common to suffer traumatic match injuries the more the pliers wore on, possibly suggesting that fatigue is connected to these injury injuries. Also, they discovered that at the pre-season (July and August), overuse-type accidents predominated; and also in season, (September to May) trauma accidents seemed to summit. This concurs with the prior work by Hawkins et al (2001) who also found that injury rates were highest in the first portion of the year and dropped off since the year wore on. Furthermore, they discovered that injury rates are somewhat more common in the past 15 minutes of their first half and last 30 minutes of the next half. It's been postulated that the well-funded European teams have well-resourced medical/rehabilitation personnel allowing for much more personalized rehabilitation of individual players. It is not uncommon for top English clubs to possess four full time physios and four full-time therapists for a group of 25 players. Interestingly, a player suffering an accident in a year has a three-fold increase in suffering another injury (new injury unrelated to the initial) throughout the subsequent season. This has implications not only for full and appropriate treatment but also for clubs registering players moving from 1 club to another (in Ekstrand 2008). Hamstring InjuriesWoods et al (2004) provides a comprehensive analysis of hamstring injuries over a two-year period using four divisions of English players. From this hamstring injury study, they also found that: 1. 57% were from running and around 15% from stretching. 2. Each club sustained an average of five hamstring injuries per season. 3. Peak incidence of training injuries was in July-August (pre-season) 4. Peak incidence of match injuries was November and January. 5. Only 5% were investigated with MRI. 6. 67% occurred in match play. 7. Almost half (47%) of the injuries occurred in the last third of each half. 8. Reinjury rate for hamstrings was 12%. 9. Biceps femoris was the most frequently injured hamstring. Prevention Of Injuries In SoccerIt is unrealistic to expect that all contact- established accidents (from tackling, being tackled and crashes) are avoidable. Whenever crashes at high speed are involved, the possibility of injury exists. Therefore, ankle and knee ligament injuries, though not common in soccer, are basically contact- based injuries and the potential for injury is down to pure chance. However, a percentage of those ankle/knee injuries will probably be non-contact-related and due to twisting/ turning in non-contact situations. Ankle and knee proprioceptive programs are generally used as part of 'pre-hab' in group sports and potentially they may reduce injury risk, particularly re-injury hazard. Injuries such as hamstrings and quadriceps injuries may be deemed as being preventable and laborious because the majority of these are endured in non-contact situations. So active steps that a professional soccer program may implement to Prevent soft-tissue Injuries like hamstrings, quadriceps and hamstrings really are as follows and will be discussed individually: 1. Recognizing ‘red flag’ playersPart of the early pre-season monitoring will include a thorough medical examination and past injury history summary. The risk factors for hamstring injuries that will ‘red flag’ a player as being a potential for hamstring injury are: a. Age. Older athletes tend to suffer higher incidence of hamstring injuries. b. Previous hamstring injury also increases the chance of another injury. c. Associated pathology such as lumbar spine disc injuries, sacroiliac joint injuries and sciatic nerve injuries. d. Players returning from lengthy lay-off periods where they have not been able to run. 2. Musculoskeletal monitoringDaily or next day measures that may be useful in catching players That Are showing subclinical signals include: a. Sit and reach tests. If done regularly a baseline range of movement may be recorded. If the athlete falls out of the window of normal range, then measures need to be introduced to find out why and treatment instituted to correct this. Sit and reach is a basic measure of spine/ hip/ hamstring/neural flexibility. b. Pelvic assessments. Joint play tests of the sacroiliac joints can pick up if players are starting to ‘tighten’ or ‘tone’ through the pelvic girdle muscles. This can have implications for motor patterns in the lower limb including hamstrings/groins/ quadriceps. c. Strength tests. Isometric tests with a dynamometer in hamstring loading positions can help identify if players are losing strength in the hamstrings. These can be compared on a regular basis to pre-existing data for that player. Similarly, hand-held dynamometer studies on adductor strength have been shown to be useful in predicting the onset of exercise- related groin pain. d. Range of motion tests. Verralletal (2005) have shown how decreasing levels of hip internal rotation usually precede the onset of groin pain. Again, second daily monitoring will be useful in identifying players who have started to lose hip rotation and as a result may become predisposed to groin pain. e. Muscle tone. Massage staff can be instructed to grade the feel of the muscle tone through hamstrings/calves/ quadriceps/adductors. Again, if things change compared to the normal for that player, they will need to be assessed and treated to clear the tone changes. 3. Fatigue monitoringExpensive monitoring units have now been developed and promoted as the new kingdom of quantifying biological markers of exhaustion. Systems like the Omegawave system use sophisticated screens on the athlete such as ECGs, muscle and brain detectors to rapidly collect information on an athletes' biological profile like heart- rate variability, cardiac readiness, hormonal readiness and fundamental system readiness. 4. Periodization and planningThe problem most professional soccer teams face is adequately preparing and planning training loads throughout this season. The pressure of numerous tournaments and enjoying twice-weekly games makes it difficult to strategy overload progressions throughout this season. As an instance, a high degree EPL team for example Chelsea will play 38 Premiership matches a year, six matches in the Champions League pool phases and maybe up to three games in the FA Cup. This represents at least 47 games available to be played during the competitive season. On average, players will play around 34 games at the year with injuries, form and enforced rest which makes it improbable that players will participate in all matches. However, during a trying period of the season such as Champions League finals stages and high-priority EPL matches, players might want to play with 4-5 times in a two-week period, it's these dividers of high-intensity games back to back in which the player is the most susceptible to soft-tissue injuries. But, top-performing teams such as Chelsea have the human resources to rotate players throughout the season for games; therefore, it makes it less likely to make soft-tissue fatigue in these players. 5. Preventative strength training.Players in the elite level are not known for their tendency to being gym junkies. The contemporary elite players' perception is that weight training will 'slow you down' and my resources in elite degree EPL soccer inform me that the non-English players tend to harbor this belief that the most. Thus, having multimillion pound players get to the whole preventative health strengthening may be a difficult sell for the rehab and performance personnel. I'm advised, however, that long-term injured players are more likely to agree to a time of strength training as part of the rehabilitation procedure. However, some simple bodyweight-type exercises may be used from the soft tissue preparation of the player. These just need to be carried out once per week, instead of the conclusion of a session if the player has no match to perform the following day and they can manage to carry some tissue soreness. This small circuit can be performed post-training and will take no more than 15 minutes. a. Bridge at 0 degrees
Start with the heel on a bench and the knee straight. Hold the other leg in flexion so that the foot is in contact with the inside of the knee. Lift the hip off the ground until the body is horizontal. Perform one set of 15 repetitions. b. Bridge at 45 degrees
Same as above; however, the knee starts 45 degrees bent. Again one set of 15 reps. c. Bridge at 90 degrees
Finally start with the knee at 90 degrees flexion. One set of 15. d. Nordic hamstring exercises
There exists some research Brooks et al. (2006) show that this exercise is a great preventer of hamstring injuries as well as a strengthening exercise post-injury. e. Swiss ball leg curls This is a great screening test to determine if an athlete is sufficiently strong to return to sport. If the athlete can perform three sets of six then this demonstrates significant hamstring strength. The athlete places a foot on the Swiss ball and drags the ball back towards the hips until the knee reaches 90 degrees flexion. They then slowly extend again back to the start position. The extension places significant load on the hamstring. Minimize this to one set of 10 repetitions. ConclusionSoccer is a fast, dynamic and possibly injurious sport played all over the world with top level athletes making large sums of money for their capacity to have the ability to kick a ball into a target. Injury rates, although generally not severe, are common in most players within a group. Research highlights the way the lower limb is the most susceptible area, and in particular delicate tissue thigh injuries -- hamstrings and quadriceps -- would be the most usual. Although time missing from play is reasonably small, preventative steps in the kind of frequent monitoring and screening in addition to scheduled rest periods coupled with some small quantity preventative exercises appear the best way to manage soft tissue injuries from the soccer player. References
Ekstrand et al (2011) Injury incidence and injury patterns in professional football: the UEFA injury study. Br J of Sports Medicine. 45; 553-558.
Woods et al (2004).The football association medical research programme: an audit of injuries in professional football – analysis of hamstring injuries. Br J of Sports Med. 38: 36-41.
Hawkinset al (2001) The association football medical research programme: an audit of injuries in professional football. Br J of Sports Med. 35: 43-47.
Ekstrand J (2008) Epidemiology of football injuries. Science and Sports. 23. 73-77.
Brookeset al (2005) Epidemiology of injuries in English professional rugby union: part 1 match injuries. British Journal of Sports Medicine. 39; 757-766.
Brookeset al (2005) Epidemiology of injuries in English professional rugby union: part 2 training injuries. British Journal of Sports Medicine. 39; 767-775.
Verrallet al (2005) Hip joint range of motion reduction in sports related chronic groin injury diagnosed as pubic bone stress injury. J Sci Sport; 8:1 77-84.
Brookset al (2006) Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. American Journal of Sports Medicine. 34(8) 1297-1306.
When the northern hemisphere winter approaches, millions head for the slopes. With that in mind, El Paso, TX. Chiropractor, Dr. Alexander Jimenez looks at what recent research has to say regarding injury and injury prevention... Skiing and (increasingly) ski have become mass-participation sports, appreciated by participants of all ages and skills. Moreover, the popularity of family holidays means that snow sports are not only appreciated by adults, but by younger participants also. Studies have demonstrated that 20% to 30% of snow game participants are children and teens, while an estimated 15 percent of Canadians over the age of 12, and 4 percent of the US population over the age of seven, reported participating in Alpine skiing, cross- country skiing or snowboarding at least one time in 2008-2009(two). But with increasing snow sport participation comes an elevated rate of traumatic injury as well as the information points to a substantial risk. Figures from US ski hotels revealed that in 2002, an estimated 77,300 ski and 62,000 ski injuries were treated in US emergency departments alone, such as 10,700 traumatic brain injuries(3). Still another study found that snowboarding is responsible for an estimated 25% of non-fatal outdoor injuries requiring emergency care(4). Studies conducted in a number of countries across Europe and North America have suggested that the risk of injury for skiers and snowboarders is approximately 2 to 4 injuries per 1000 participant times, with the maximum threat in snowboarders(5-9). Children and teens at the 7-17 years age bracket appear to have higher rates of injury than younger and older participants(2). There is recent evidence that the incidence of traumatic brain injury and spinal cord injury in skiing and snowboarding is increasing worldwide. This growth in severe injuries may be associated with greater risk-taking, such as jumping and acrobatic activities, both on new terrain and in snow resorts/parks specifically made for snowboarding(15). Typical Injuries Sustained In Snow SportsA number of reviews have been published that summarize the epidemiology of skiing and snowboarding injuries. Skiers tend to maintain injuries to the lower extremities; snowboarders, on the other hand, are much more likely to sustain injury to the upper extremities (see Figure 1)(16-17). Knee injuries are the most frequent type of injury in ski and constitute around 36% of all ski injuries, according to the literature(18). Snowboarders sustain more ripped ligaments and sprains/strains, brought on by a) position sideways on the board and b) that the absence of a safety binding that opens on its own in the event of a collapse. In a snowboard autumn, the wrists are particularly vulnerable to trauma, especially on impact. It reported that in Alpine skiing, the most common injury site is the lower extremity (40% to 60 percent of all injuries); knee injuries (eg fractures and sprains) are common and observed more frequently in younger children. Other typical injuries are to the head and neck (10% to 20 percent), upper extremity (15% to 25%), and thumb (10% to 20%). In ski, the most commonly injured site is that the wrist (22%), together with upper-extremity accidents (like wrist injuries) at roughly 50 percent of cases. Of them, 10% required emergency treatment and 30% to 40% requiring following admission for trauma treatment. Personal details, snow sports-related factors, diagnosis, and treatment have been recorded, and control data were gathered at random from uninjured people at all three areas. A total of 732 accidents were listed at 674 people and the injury rate for the study was 3.7 injuries per 1000 skier days -- very much in accordance with the studies above(5,6,8). Yet again, snowboarders lasted more injuries to the upper limb and axial areas than their skiing counterparts, also ski- boarders and snowboarders also suffered a higher incidence of fracture. Table 1 demonstrates how these injuries were broken down by sport type and anatomical location. Much of the information on snow sports injury was collected in the late 1990s and early 2000s -- coinciding with a time of rapidly growing popularity. But have the injury tendencies changed over time and what would be the implications for injury prevention? A current (2012) US study looked at snow- boarding injury trends at a ski resort in Vermont within a span of 18 seasons (1988-2006) and compared these with Alpine skiing injuries over precisely the same interval(21). The researchers also looked at the differences in injury patterns between snowboarders and Alpine skiers according to age, experience, and sex. The injury rates were assessed as mean days between injuries (MDBI -- the lower the number, the greater the injury rate). The findings were as follows: ● The average MDBI for all harms among snowboarders has been 345 as compared with 400 for skiers. The most frequent type of harm for snowboarders was a wrist injury (MDBI, 1258), although for skiers it had been an anterior cruciate ligament (ACL) sprain (MDBI, 2332). ● Wrist injuries accounted for 27.6% of all snowboard injuries and 2.8 percent of skiing injuries. ● ACL injuries composed 1.7% of all snowboard injuries and 17.2% of skiing injuries. ● Among snowboarders, more wrist injuries, shoulder soft tissue injuries, ankle injuries, concussions, and clavicle fractures were seen, while skiers had more ACL sprains, medial collateral ligament (MCL) sprains of the knee, lateral collateral ligament (LCL) sprains of the knee, lower extremity contusions, and tibia fractures. ● There was a trend towards an increased incidence of clavicle fractures and a decrease in MCL injuries and ankle injuries among snowboarders over time. ● Skiers had a decrease in thumb metacarpophalangeal-ulnar collateral ligament (MCP-UCL) injuries and MCL injuries of the knee over time. ● The highest rate of injury was among young, inexperienced, female snowboarders. Overall, whilst injury rates in snowboarders have fluctuated over time, they now remain higher compared to skiers. This may be partly because of changing demographics -- snowboarding is frequently portrayed as a youthful, 'trendy' sport and the data indicates that injured snowboarders were significantly younger, less experienced, and more likely to be female than wounded skiers or snowboard management participants. The growth in rates of clavicle fracture might be connected to a heightened interest in snowboarding acrobatic/airborne maneuvers. Injury Prevention In Snow SportsSnowboarding equipment -- Since its inception, snowboarding has always been associated with a higher incidence of upper limb injuries compared to alpine skiing, with the wrist being the single commonest site of injury. In case of a collapse, the natural tendency for a snowboarder is to stretch out (and land on) the hand. Back in 1999, the evidence indicated that less than 10% of snowboarders were utilizing wrist guards to defend the wrist in these falls, despite there being a few epidemiological and laboratory evidence to support their use(22-24). With an increasing emphasis on security, you may think that the situation now is radically different but the evidence is less encouraging. A 2011 meta-study by US researchers studied all of the published literature about wrist guard use, trauma prevention, the biomechanical effects of wrist guards, and the various kinds of wrist guards commercially accessible for snow- boarders(25). The authors concluded that the use of protective equipment for the wrist is a helpful method for preventing injury. However, they pointed out that while numerous studies looked at the impact of wrist guards, there was no consensus about which particular kind of wrist guard would be most effective; the vast majority of the studies did not mention a brand name or a description of the type of wrist protector that was used by participants. It was also apparent that the literature generally reported low usage of wrist guards by snowboarders -- as low as 6 percent -- possibly because of aesthetics, societal acceptance, match or wrist guard and availability. Some research has suggested that using wrist guards might increase the possibility of sustaining an elbow, upper arm or shoulder injury -- by transferring the loading during a fall further up the arm. On the other hand, the evidence for this can be conflicting and has not yet been confirmed in a controlled trial or well-designed prospective study and the present best guidance for snowboarders is to use a wrist guard to help avoid injury. Skiing equipment -- Injury prevalence among skiers has declined over a few decades, largely because of improvements in ski gear, particularly boots and bindings; proof proves that modern bindings decrease the incidence of foot, ankle and lower tibial injuries providing they are properly mounted, adjusted and maintained(26,27). Many accidents are the result of poorly adjusted bindings; in one analysis of adult lower extremity equipment- related injuries it had been determined that in 96% of cases the ski bindings did not release when the accident happened(28). Non-release of bindings has also been reported as an injury contributor in different studies of the two youths and adults. In one study, skiers younger than 13 decades of age with poorly adjusted bindings were much more likely to be injured than children with correctly adjusted bindings(29). Unsurprisingly, therefore, some investigators have proposed that a professional should adjust children's and beginners' ski bindings at the start of every lesson and that these groups should be taught to check their bindings at the beginning of each ski day(30). Snowboarding and skiing equipment -- One place where there's little doubt over powerful equipment-based harm prevention is helmet use. A new systematic review found that helmets significantly lessen the risk of head injury(31). Skiers and snowboarders wearing a helmet were far not as likely to have a brain injury, and this threat was further reduced when research which included children younger than 13 decades of age were included. Overall, the pooled results showed that helmet use reduces the chance of head injury by around 35%. Some researchers have raised concerns that while helmet use during skiing and snowboarding reduces head injury rates, it may increase the risk of cervical spine injuries. However, these concerns are not supported by many of case control studies(32-35) and also a 2010 systematic review also concluded that helmets weren't related to an increased risk of neck injury(31). Moreover, there's also no proof that helmet usage in skiing and snowboarding is connected with riskier behavior (36,37). The obvious conclusion here is that helmet usage ought to be considered compulsory at all times where safety is an issue. Physical Conditioning: Snow Sports & Injury PreventionPower, endurance and cardiovascular fitness are all central components in sports injury prevention throughout a vast range of sports, and yet in snow sports, there appears to be a much greater emphasis on equipment-based and third party alternatives. A comprehensive and systematic overview of the literature printed in 2013 looked at injury prevention recommendations specific to recreational Alpine skiers and snowboarders. The attention was to discern recommendations that concentrated physical fitness, exercise and/or training in preventing musculoskeletal injuries in these two sports(38). Studies were included if they dealt with injury prevention, recreational Alpine skiing or snow- boarding and musculoskeletal injuries and articles on elite athletes were excluded. Overall, 80 recommendations for the prevention of musculoskeletal injuries in recreational Alpine skiers and snowboarders were identified and classified into five main categories: ● Equipment use(n=24) ● Education and knowledge(n=11) ● Awareness and behavior ● Experience(n=10) ● Third-party involvement(n=20) Amazingly, there was no research that made recommendations pertaining to physical fitness, exercise and/or training per se, or its role in preventing injury! The authors commented thus about the frequent recommendations for preventing ski and snowboarding injuries by an equipment-based or third party approach: "The dominance of equipment-related steps in the injury prevention literature may be rationalized from a sports biomechanics perspective, because these activities involve high velocities and impact forces. Nonetheless, this also suggests a need for proper levels of power, conditioning and endurance to fulfill the technical requirements of the sports." To put it differently, while it makes sense to take precautionary measures regarding proper equipment use, consciousness, behavior etc, neglecting essential physical conditioning could be counterproductive. Unfortunately, there are no peer-reviewed studies about which type of conditioning system is the most suitable for snow sport injury prevention, but some of the general principles that are very likely to be useful are summarized in Box 2 below. OverviewSkiing and snowboarding by their very nature carry a substantial risk of injury, which could sometimes be serious. The most common injuries are to the knees in skiers and wrists in snowboarders, and the rate of injury is greatest in novices, the less experienced and the young. Along with equipment-based measures, (eg bindings when skiing and wrist guards when snowboarding) is critical for reducing injury risk. Helmet use is also vital to reduce the incidence and severity of head injury in both skiers and snowboarders. In addition a proper pre-skiing/snowboarding conditioning system may also play an important part in ensuring a visit to the slopes is memorable for all the right reasons. References
1. National Ski Areas Association. Kottke National End of Season Survey 2010/11: Final Report. Table 6: Estimated US Ski Injury Skier Visits by Region 1978/79 – 2010/11. http://www.nsaa.org/nsaa/press/historical-visits.pdf
2. Inj Prev 1996;2(4):286-9
3. J Trauma 2005;58(1):112-8
4. Wilderness Environ Med 2008;19(2):91-8
5. Br J Sports Med 2004;38(3):264-8
6. Sports Med 2004;34(2):133-9
7. Br J Sports Med 2002;36(2):135-40 8. Am J Sports Med 2004;32(1):96-103
9. Am J Sports Med 1995;23(5):597-600
10. Am J Surg 2009;197(5):560-4.
11. Inj Control Saf Promot 2004;11(4):281-5
12. Injury 2003;34(12):892-6
13. National Ski Areas Association. Facts About Skiing/Snowboarding Safety: Updated March 2006. http://www.nsaa.org/nsaa/press/0506/facts-about-skiing-andsnowboarding.asp
14. Sports Health. 2009 Nov;1(6):486-92
15. Inj Prev 2007(6);13:368-75
16. Acta Orthop Scand 2001; 72: 657–660
17. Am J Sports Med 1999; 27: 94–97
18. Am J Sports Med 1999; 27:381–389
19. Schweiz Monatsschr Zahnmed. 2013;123 (7-8):655-9
20. Paediatr Child Health 2012;17(1):35-6
21. Am J Sports Med. 2012 Apr;40(4):770-6
22. Skiing trauma and safety. 12th volume. Philadelphia: American Society for Testing and Materials, 1999:141–9
23. Am J Sports Med 1998;26:825–30.
24. J Trauma 2000;48:1109–14
25. Bulletin of the NYU Hospital for Joint Diseases 2011;69(2):149-57
26. Sports Med 1999;28(1):35-48.
27. Aust Fam Physician 2003;32(7):499-502.
28. J Orthop Sci 2002;7(1):1-5
29. Am J Sports Med 1999;27(5): 644-50.
30. Sports and Recreation Injury Prevention Strategies: Systematic Review and Best Practices; Executive Summary. Vancouver: BC Injury Research and Prevention Unit, 2001.
31. CMAJ 2010;182(4):333-40
32. BMJ 2005;330(7486):281
33. Semin Neurol 2000;20(2):233-45
34. Epidemiology 2008;19(2):270-6
35. JAMA 2006;295(8):919-24
36. Accid Anal Prev 2005;37(1):103-8.
37. Inj Prev 2007;13(3):173-7
38. Sports Med. 2013 May;43(5):355-66
39. Br J Sports Med. 2008 Jun; 42(6):394-412
It was once believed that inflammation caused impairments such as plantar fasciitis, tendonitis and iliotibial band syndrome -- but new research shows that may not be the case. Injury specialist Dr. Alexander Jimenez examines the data. The body was made to move; however, moving too far or too often in a repetitive way can overexert tissues. New research is now calling into question the concept that inflammation causes these conditions -- and this may affect our understanding and treatment to what had been considered tendonitis and fasciitis. Connective TissueLigaments, tendons, ligaments and fascia hold the bony skeleton together. Quite simply, the muscles move the manhood; the tendons connect muscles to bones; the fascia encases the musculotendinous unit, and sometimes become a functional part of the unit, as is true for the iliotibial band and the gluteus maximus and tensor fasciae latae muscles; and the ligaments connect bones to bones. An athlete might have the occasional ligament strain or inherent ligament laxity, but the tissue itself typically either does its job or doesn't. Current thought on the causes and therapy of the chronic injury of those tissues may change the way you exude your endurance athletes. Fascinating FasciaFascia exists as an uninterrupted matrix of collagen that extends throughout the entire body, forming a web of covering and connection between all organs and muscles. Therefore, it is nearly impossible to isolate and name a region of the continuum in any other way than its nearest anatomical structure. It's three- dimensional and contains freedom in all three planes of motion(1). While one continuous membrane, fascia has distinct inherent characteristics based on its location and function. Fascia that exists among muscles aids to transmit forces in addition to absorb strain.Studiesinlive specimens with ultrasound reveal that fascia is viscoelastic -- using both viscous and elastic characteristics when deformed -- and is therefore able to slip independently of the contraction of the muscle that it surrounds(1). Fascia is composed of at least nine of the 28 types of known collagen. Collagen gives construction, durability and strength to the tissue. The extracellular matrix of fascia includes the elastic fibers which provide flexibility. Myofibroblasts are also present in fascia, leading, hypothetically, to its contractility, tension, and equilibrium(1). Fascia has a characteristic fiber arrangement parallel to the common force vectors to which it can be exposed. Tendons are also viscoelastic structures, composed primarily of type-I collagen fibers, using a little amount of type-III and type-X as well(2). The collagen fibers lie in a parallel structure, with a resultant tensile strength capable of transmitting large forces. The fibroblasts within the tendon, known as tenocytes, lie along the collagen fibers and provide the structure for collagen cross- links. Their sensitivity allows them to regulate the protein synthesis within the extra-cellular matrix dependent on the changes from the load encountered by the tendon. It is the unloading and loading of the tendon that activates the chemical and structural changes in the thoracic structure, which may be why specific types of exercise are important in tendon rehabilitation and recovery. Mechanism Of InjuryTendon and fascial injuries both result from overloading. Acute injuries are usually considered as resulting after a one-time incident of intense loading. A chronic injury, subsequently, is considered something that occurs after repeated excessive strain. However, some theories assert that acute accidents occur due to chronic underlying micro-stress into the tissue(two). In any case, nearly 50% of sports injuries reported from the USA are the result of overuse(3). Traditionally, both tendon and fascial injuries were considered inflammatory processes and were consequently named tendonitis and fasciitis. As more is understood concerning the mechanics of both injury and healing, this nomenclature is now called into question. Tendinopathy is the catch-all phrase that covers any abnormal state of the tendon. Tendonitis refers to some true inflammatory reaction due to bleeding within the gut as a result of an intense event. Tendinosis is the condition of tendon degeneration that develops over time in the lack of a true inflammatory response. It's considered a state of overuse, however, though, can coexist with an inflammatory process from the paratenon. Actually, degeneration along various points on this spectrum can be found all within exactly the same tendon. A barbell with tendinosis differs histologically from tissue that is healthy. The collagen alignment in tendinosis is no more parallel and the distance between the collagen bundles increases. The tenocytes become much more notable. The quantity of type-III collagen additionally increases when compared to type-I, which generally composes 90 percent of the collagen in healthy tendon(3). Despite an increase in fibroblasts, there are no inflammatory cells present in the extra-cellular matrix. There is an infiltration of blood vessels and nerves, which is referred to as neovascularisation. These microscopic findings are indicative of a fix process gone awry, resulting in further tendon degeneration. It appears that in response to excessive strain or overuse, the tendon attempts to initiate a healing process that fails to regenerate and really further degenerates the tissue. Some theorize that inflammation occurs initially, but that the repetitive nature of the mechanical stress results in interruption of the normal recovery procedure. When inflammation occurs within a healthy tendon the tenocytes turn into myofibroblasts. The myofibroblasts then normally undergo cell death; however, in tendinosis, the repeated stress may interrupt this process, causing a proliferation of myofibroblasts which cause fibrosis of the tissue. Hypoxia can interrupt the homeostasis of this extra-cellular matrix, which causes an increase in blood vessels and corresponding nerve pathways. The gain in sensory nerve pathways at the neovascularisation process is thought to be the cause of greater pain in tendonosis(3). The pain of this neo- vascularisation may cause an athlete to insufficiently load the tendon to activate the normal tenocyte reaction to strain, thus further inhibiting healing. The lack of repair contributes to microscopic tears which can finally cause tendon rupture. TreatmentFasciitis and tendinopathy are often considered difficult conditions to deal with because of the poor outcomes when using conventional inflammation combating strategies. Understanding that an athlete's condition might not really be an inflammatory process is important when choosing the proper healing modalities. The exact same is true with the usage of non-steroidal anti-inflammatory medications (NSAIDs). While maybe mediating the pain, they don't improve the condition. Masking the pain might cause additional harm as the athlete continues to execute the offending action. Treatment with NSAIDs must be undertaken acknowledging the lack of evidence of efficiency, in addition to the risks related to such drugs, most especially gastro-intestinal upset. Some modalities are found to be useful in the management of tendinosis and fascial injuries. Intense friction massage, using a tool or merely manually, is often used to evoke changes in the tissue through a physical manipulation that triggers a recovery reaction. True randomized controlled studies are lean for its treatment of tendinosis, and lacking altogether about fasciitis. However, case studies show great results with friction massage when utilized as an adjunct to other therapeutic methods(4). The use of low-level laser therapy (LLLT) is controversial at best. An overview of six distinct systemic literature reviews on the use of LLLT with tendinopathy came to the conclusion that there isn't enough conclusive evidence to advocate its use in the therapy of tendinopathy(3). The same holds true in the case of ultrasound treatment. While thought to trigger recovery through adrenal effects, ultrasound hasn't been found to be beneficial. The accession of drugs through using ultrasound (phonophoresis) or electric impulses (iontophoresis) conveys nearly the very same effects as LLLT and ultrasound alone. Studies conflict as to the effectiveness of all of these modalities. What's New?New on the horizon is the use of extra- corporeal shockwave therapy (ESWT) for the treatment of tendinosis and fascial injuries. Shockwaves are delivered via electromagnetic, electro hydraulic, or piezoelectric sources. The tech for ESWT is a derivative of the lithotripsy used as a treatment for kidney stones. The waves are significantly more focused and intense than those by an ultrasound device. Initial studies of the use of ESWT in the treatment of resistant tendinopathy show excellent results, especially with athletes(3). The same is true from the preliminary research treating plantar fasciitis with ESWT. Patients report better outcomes in pain relief and operate with ESWT than with operation or corticosteroid injections(5). But, because of the need for more large and long-term studies on its efficacy, it is not advocated as a first line treatment. Another new treatment is the use of exogenous nitric oxide (NO). NO is thought to assist in cell signaling and in the modulation of the immune reaction. Animal studies demonstrate that treatment with exogenous NO contributes to higher collagen synthesis and recovery inside joints, and also depleting NO has a negative influence on the strength and size of a healing tendon(3). The Food and Drug Administration believe the use of exogenous nitric acid to deal with tendinopathy or fasciitis, via a glyceryl trinitrate patch, an off-label usage in america. But, studies show that using a 5mg/24-hour glyceryl trinitrate patch, divided into quarters, is effective in controlling pain and assisting in tendon healing. Treatment lasts from eight weeks to six months, and also the quarter-patch is put directly over the thoracic and changed everyday. Side effects are typically the same as treatment with nitroglycerine -- headache and dizziness due to hypotension -- and therapy using concurrent active therapeutic exercise is recommended. A Shot In The Arm, Leg, Or Ankle...A well known method of handling inflammation, corticosteroid shots have long been used with limited success in the management of tendinopathies and fasciitis. The reason for the limited success must now be nicely apparent. Theoretically, tendon degeneration may result in inflammation of the paratenon, which leads to the pain of the injury. Injection adjoining to the injury can help with the inflammation there, but the root cause of degeneration is not assisted whatsoever. If shots are undertaken, they need to be achieved with the assistance of fluoroscopic guidance to assure that the delivery of this steroid is adjacent to the tendon, not inside. Despite a dearth of evidence to support its use, corticosteroids are still a first line treatment for fasciitis, particularly plantar fasciitis. A British Medical Journal Clinical Evidence report even went so far as to say that steroid injections might be injurious to the plantar fascia through the years(6). This lack of evidence prompted researchers in the section of rheumatology in Musgrave Park Hospital in Belfast to compare the use of ultrasound guided corticosteroid injection to that of non-guided injection and placebo injection in the treatment of plantar fasciitis(7). Results revealed considerable improvement utilizing corticosteroid as opposed to placebo at six and twelve months, although no gap between guided and unguided injection was shown. But, glaringly absent in this research is a description of concurrent or previous treatments undertaken by the participants, or restrictions from the same. Additionally, knowing that, oftentimes, plantar fasciitis is self-limiting, together with progress generally in three to six months, more studies are required to encourage the regular use of steroid injections in treating fasciitis. Platelet-rich plasma (PRP) is just another process of injection therapy that's gaining in popularity. A concentration of platelets is drawn from an individual's own blood and re-injected at the site of injury. The theory is that the lab-activated platelets will activate enhanced collagen production and promote healing. There aren't any dependable, controlled studies now that reveal PRP to be greater compared to other injectables or physical therapy alone, in treating tendinopathy and fasciitis(3,5). Better-regulated research are required before clinical evidence as to the efficacy of the injection-based treatment approach can be revealed. First-Line Treatment & Last-Ditch EffortOverwhelming evidence exists to support the use of eccentric exercise in the treatment of tendinopathy(2,3). Loading the injured tendon appropriately appears to be crucial in preventing the degenerative cascade and initiating proper recovery. The specific mechanism through which eccentric exercise can reorganize the tendon structure isn't well understood; however, it's thought to nourish the tenocytes and reunite the extracellular matrix into homeostasis. Surgery is considered in hard cases as a last resort. What is consistent, however, is that return to sport after surgery can be a four- to - 12-month time frame, and invasive procedures are not without their own set of risks, including unsuccessful outcomes(3). Frustrated Yet?Indeed, that is how many coaches, therapists and athletes believe about the nagging injury that, despite everyone's best efforts, just won't go away. The new comprehension of connective tissue structure and function challenges how typical overuse injuries are treated. No longer considered inflammatory in nature, unless very obviously acute, tendon and fascial injuries call for a novel approach to treatment. In order to bring about healing, a change has to be triggered in the harmful physiological cascade that leads to tissue degeneration. Eccentric exercise, ESWT, transdermal NO, and possibly deep friction massage, are all demonstrating the best results thus far in causing tendon healing and halting degeneration. The specific mechanism by which these treatments work isn't well known. Other remedies methods ought to be inspected, and possibly discarded, until study reveals their efficacy. Truly halting the progression of an overuse connective tissue harm needs the expert eye of a physiotherapist, trainer, and coach to evaluate musculoskeletal status and motion routines, technique, training schedule, and gear. Very often, there's an offending component that's been overlooked. Once corrected, the connective tissue strain will be eliminated and curative intervention will have a chance to get the job done. In overuse injuries, a more comprehensive approach has to be taken to avoid additional tissue degeneration and injury. References
1. J Can Chiropr Assoc. 2012;56(3):179-91
2. J Bone Joint Surg Am. 2013;95:1620-8
3. Prim Care Clin Office Pract. 2013;40:453-73
4. J Sport Rehabil. 2012 Nov;21(4):343-53
5. J Fam Pract. 2013 Sep;62(9):466-71
6. Clin Evid 2008. 2008:1111
7. Ann Rheum Dis. 2013;72:996-1002
Chiropractic scientist, Dr. Alexander Jimenez has a look at this painful condition which can be the cause of a lot of lost playing time. Last year, rugby union player Anthony Allen of the Leicester Tigers endured what he believed was a reasonably straightforward blow to the exterior of his shin -- but it ended up being a nightmare which would keep him out for four weeks of rugby. In October 2013, he thought he'd sprained his ankle in a match, as he did not recall sustaining a direct blow to the surface of the shin. Over the ensuing days, he noticed that the pain was worsening and he was experiencing swelling and pain sensations further down the shin away from the website of the accident, with some minor paraesthesia into the top of the foot. He alerted the medical staff to his worsening illness and they immediately referred him to an orthopaedic surgeon who watched the leg using an ultrasound (to exclude a deep vein thrombosis), after which an MRI, which confirmed that the participant was suffering from an acute compartment syndrome in the lower leg. They conducted an operation to successfully alleviate the pressure from the leg, and he was told that the rehabilitation following this harm could be 3-4 weeks. What Is Compartment Syndrome?When a body part receives a direct blow because of an external object, muscle damage can ensue. The outcome is a hematoma, which is a swelling inside the muscle due to blood accumulation -- a consequence of the direct bleeding of this muscle as little venules and possibly arterioles are damaged and 'leak' blood to the region, which then collects into a mass. A hematoma can grow within the muscle or external to the true muscle and involving the fascial sheaths that surround the muscle. The majority of those hematomas are benign and, although painful for 7-21 days, they finally resolve and the sufferer regains full purpose. The origin of the direct blow may be the sufferer contacting another person forcefully, as in being kicked in soccer or martial arts or a direct blow due to a tackle in football. These are commonly known as 'contusions', ' 'corks' or ' 'charley horses'. This is called the osteofascial compartment. This growth in volume within a enclosed space eventually compresses the blood vessels and nerves that run through the compartment and symptoms have been exacerbated. Who Can Get Compartment Syndrome?Most cases of compartment syndrome are a result of high velocity trauma like motor vehicle accident or falling out of a quick- moving bike/horse. These generally involve a bone fracture like the tibia in the upper leg or the radius in the forearm. The amount of blood discharged from the bone will collect in the osteofascial compartment. But, they may also be caused by lead high-force 'crush'-type injuries which do not break bones but do end up damaging a lot of muscle tissue. This can be because of a direct hefty blow that spreads the pressure across a wide region and does not violate any underlying bone. Severe burns may also lead to compartment syndromes. Young males are the most likely victims as ordinarily they're involved in sport and pastimes that may expose them to high velocity or high-force trauma that may cause this pathology. Individuals on anti-coagulant blood thinners are also more vulnerable. Because the fascia of the compartment does not stretch, a little increase in blood volume can result in large increases in pressure. This rapidly compresses the nerves and blood vessels (typically veins) and the normal late signs of compartment syndrome like needles and pins and deficiency of pulses may then result. Arteries are usually spared as the systolic blood pressure in the gut is usually too high to be compressed by the compartment pressure. Chronic compartment syndromes which are not medical emergencies may occur in athletes because of a slow growth in muscle size because of hypertrophy with an overlying fascia that doesn't stretch. This impacts runners, cyclists and even bodybuilders. Signs & SymptomsThe usual signs and symptoms of an acute compartment syndrome are called the 6 Ps: - Pain (out of proportion to expected tissue damage). Usually a deep pain and is aggravated by stretch of the muscle;
- Paralysis due to compression of motor nerves;
- Pallor due to blood vessel compression;
- Paraesthesia due compression of nerves.;
- Pressure elevation (measurable);
- Pulselessness (rare and usually only if severe compression).
The pain and neurological disorders (pins and needles) have been early signals; diminished or absent pulses and paralysis are late signs. Pallor may come with a swollen and tense muscle because of the collection of blood at the underlying muscle compartment. DiagnosisThe most direct measure for compartment syndrome is a compartment pressure test. In such examples, it has been recommended that the compartment decompression may be necessary. TreatmentThis involves an incision into the thoracic fascia, similar to how a sausage on the BBQ may be sliced to discharge juices from a swelling sausage since it is being heated. It is common place to perform a fasciotomy on all the compartments in the area affected. As a result of sudden onset of elevated compartment pressure, if the injury isn't dealt with immediately, catastrophic permanent damage to the muscle, nerves and blood vessels can result, leaving permanent scarring in these types of structures and generally rhabdomyolysis may ensue, leaking toxins into the blood stream that might result in kidney damage. RehabilitationFollowing operation, the time frame for return to straightforward activities like walking is generally quite quick and the individual might be functional with this particular capacity in 4-6 weeks. They might require gentle soft tissue massage to stop excessive scarring and adhesions, and gentle progressive strength training to recover lost muscle functioning. The athlete needs a longer time frame to return to perform as they will need a more systematic rehabilitation protocol which takes them from walking to running to sprinting and ultimately explosive movements such as jumps and take-off moves. They'll require longer to regain strength and full stretch in addition to other high-level capacities such as proprioception and balance control.
Chiropractor, Dr. Alexander Jimenez investigates this very common knee injury... IntroductionMeniscal tears can result in a great deal of time lost from bodily activity or employment, and therefore understanding the risk factors for meniscal tears may allow for a quicker and more accurate diagnosis. Meniscal lesions normally occur in the athletic arena as a result of dynamic demands placed on the knee through specific movements. Additional a meniscal tear can also result due to the numerous repetitive places continuing within the work area. Normal positions adopted in a work environment such as standing, lifting, squatting, kneeling and sitting have all been suggested to influence the danger of meniscal damage(2). Furthermore, the period between anterior cruciate ligament (ACL) rupture and surgical reconstruction has also been recognized as a risk factor for a meniscal lesion(3). Various risk factors are recognized to contribute to a meniscal lesion nonetheless, there is limited study within the literature to support them(4). A systematic review, together with some meta-analysis, was published in 2013 by scientists in the University of Amsterdam(4) who investigated some of the key risk factors for meniscal tears. The purpose of the present review is to outline the findings based on a number of the articles which were included in that distinct systematic research review whilst also drawing on the results from other study also. Furthermore, the current review may also assist a physiotherapist or sports therapist within their own clinical evaluation by identifying key risk factors that may help form their identification. The menisci are just two semilunar form- like structures which sit positioned on the medial and lateral surface of the tibial plateau (see Box 1) (5). Additionally, the menisci allow the transference of weight and absorption of shock during dynamic motions, whilst acting to protect the articular cartilage(5). Meniscal lesions could be either acute or degenerative in nature and might present in different kinds, ie a bucket handle tear, a flat equilibrium or a degenerative tear. Degenerative Risk FactorsBody mass index (BMI) was identified in 2 research studies and has been shown to be important with degenerative meniscal changes(4). Scientists from Boston University(5) analyzed the BMI of 991 (565 females and 426 men) participants also found that females with a meniscal tear had a significantly higher BMI (29.9) than females with no meniscal damage (27.9). It had been reasoned, through statistical analysis, that a BMI greater than 25 kg/m2 yielded a greater propensity for meniscal damage than people with a lower BMI(4). It is important to remember that this doesn't just involve those of more obese proportions but those who have a larger muscle mass therefore increased body mass too. Age is considered to be a significant risk factor as identified in 2 research(4). Researchers have(5) determined that the older the individual the higher the meniscal injury, for example 19 percent of females and 32% of males aged 50-59 had meniscal destruction(5). This is compared to 51 percent of guys and 56% males aged 70-90 years presenting with meniscal trauma. It was reasoned that individuals over 60 years of age were significantly more likely to sustain a degenerative meniscal tear compared to a person under 60 years of age(4 years). But, that doesn't suggest that a younger person can't maintain a meniscal lesion. Gender is regarded as a three-fold risk factor for a meniscus tear in men as identified in three articles(4). Additional study completed at Boston University studied the connection between meniscal tears, pain and atherosclerosis in 154 patients symptomatic of knee osteoarthritis(7). The results obtained by MRI scans ascertained that 91 percent of individuals had a lateral or lateral meniscal tear and of this group males had a significantly greater incidence of meniscal lesions than females. The second study compared the qualities of meniscal lesions in 991 participants through MRI(5). Males again revealed significantly higher prevalence of meniscal tears in all age groups even though females combined with greater meniscal degeneration in the 70-90 years old class(5). Whether the greater incidence in men is due to greater participation in game or by occupational activities was not determined. Kneeling and squatting in the office are often places adopted by those in certain professions or trades such as carpentry, electrician and pipes which are largely occupied by men. Three newspapers were identified that analyzed these sustained places and found that kneeling and squatting for longer than one hour per day is considered to be influential in the development of meniscal tears(4). Research carried out at Southampton University (England) found that 59 respondents experienced bending of their knee with 29 being exposed to kneeling and with 30 exposed to squatting in their workplace (see Box 2)(8). Of these 59 patients (several may cross over in both groups), 69 percent and 73% respectively had consulted with an orthopedic surgeon. These participants participated in repetitive kneeling and squatting through their job but had also reported participation in soccer too which is thought of as another risk factor. Sitting for longer than two hours or longer per day has been believed to decrease the risk of meniscal tears(4). The 2 studies, carried out by the same lead writer from Southampton University(8, 9), the two identified to assess the probability of sitting. Prolonged sitting may also predispose an individual to additional knee-related conditions such as patellofemoral pain (known as movie/theatre sign) whereby sitting is regarded as a risk factor(10). Though sitting does not increase the risk of meniscal damage, it has the capability to cause problems elsewhere in the knee. Standing or walking for longer than two hours per day for 12 weeks ahead of the beginning of symptoms, in contrast to less than two hours per day, were regarded as influential in the growth of meniscal lesions. Two studies were found to have evaluated the effects of prolonged walking or standing(8), 9). The results found that from 71 patients that were subjected to prolonged walking or standing for longer than two hours every day, 54% had consulted an orthopedic surgeon with symptoms of meniscal damage (see Box 2). In contrast, standing and walking are considered to be effective from different perspectives in terms of energy expenditure, mechanical bone loading, cardiovascular fitness and general wellbeing and shouldn't be compromised unless symptoms decide. Walking longer than two kilometers per day (in the 12 months before the onset of symptoms) was identified by 2 studies(8, 9) where this variable was thought of as a very low risk for a meniscal lesion(4).) Again, the health benefits of walking outweigh the probability of meniscal lesions, and should not be negotiated unless symptoms prevent. Climbing more than 30 flights of stairs every day (in the 12 months before the beginning of symptoms) has been contrasted by two studies(8, 9). 17 male patients complained of meniscal-related symptoms (locking) on stair climbing using 59 percent resulting in a consultation with an orthopedic surgeon (see Box 2)(8). Snoeker and coworkers(4) concluded that there was a significant effect that lifting or carrying in excess of 10kg, 25kg and 50kg more than 10 times each week substantially increased the risk of a meniscal lesion. The incidence of degenerative or acute meniscal lesions have been investigated(8) and have been known to frequently in the present study. This research study contacted a community sample of 2,806 men, at the south of England, by way of a questionnaire. Of the sample contacted, 1,404 reacted with 762 having complained of past knee-related symptoms. Of the 762 patients with symptomatic knees, 127 had reported symptoms of bending during one or more of the occupational pursuits that had lasted for longer than 24 hours (see Box 2). It was considered important to illustrate the findings in this particular study as we're all exposed to these activities of daily living to some extent(8). This ascertains the risk of a potential meniscal lesion inside the 20-59 age bracket. Acute Risk FactorsWeight posture during injury is considered to be a moderate risk factor for the incidence of meniscal tears that was identified in one study(4). Researchers from Lund University in Sweden(11) ascertained that patients using an ACL injury who participated in non-weight posture were not as likely to maintain meniscal damage. Frequently ACL trauma is continuing in load bearing positions leading to greater joint compression forces of the tibio-femoral compartment and therefore the well-known term 'miserable triad' has more suitably been termed 'the unhappy compression' harm(11). It is essential to stabilize the knee joint during conservative or surgical ways to prevent further compression to the meniscus. It was concluded that weight bearing during trauma exposed a moderate threat to meniscal trauma but the authors were not able to decide whether a substantial effect existed(4). Sport in general is regarded as a relatively large risk factor for meniscal lesions(4). Two studies were identified that analyzed the prevalence of meniscus damage during football, rugby, swimming and running(8,9). Soccer and rugby were concluded to be major risk factors in the incidence of meniscal damage(4). Compared swimming and 'other sports' (Snoeker and colleagues(4) did not determine which athletics) were thought of as moderate risk factors in the incidence of meniscal tears(4). What's more, there was a paucity of evidence available for running to be regarded as a risk factor for meniscal damage(4). It is not hard to appreciate why soccer and rugby expose a knee to higher meniscus trauma due to the demands of this transference of mass and the rotational forces implemented. Anterior cruciate ligament injury followed by a protracted interval until cosmetic surgery has been well recorded to induce a patient to meniscus damage(3). An ACL-deficient knee demands the menisci to be a stabilizing component in the posterior-anterior, valgus-varus and internal and external rotation movements(12). Snoeker and colleagues(4) research coincided with previous research, in that the ACL deficient knee vulnerable a threat to meniscus trauma but recognized that this was in agreement with the medial, but not lateral meniscus. The authors said the reason for this shift in consistency was a result of the medial meniscus being repaired to the joint capsule. In contrast, the lateral meniscus isn't firmly attached to the joint capsule and so possesses more freedom within the joint which explains this gap in injury occurrence(4). It was identified that by 3,475 patients having a history of ACL injury that 1,638 (47 percent) had presented with a meniscal tear(3). The authors added that for each month that passed after ACL rupture there was exponential risk of 1 percent of meniscal injury. In addition, the presence of a degenerative meniscal lesion demonstrated with 1.6-2.0% heightened risk of sustaining additional trauma to the knee. OverviewThe current review according to Snoeker and colleagues'(4) systematic review has identified a number of factors which could predispose someone to a greater incidence of meniscal injury. A meniscal lesion could be sustained amongst a broad population and should not be ruled out in any 1 sub-group based on the analysis presented. However, those risk factors identified could predispose an individual to higher chance of a meniscal lesion. Even though the study by Snoeker and colleagues is very recently published and covers a large number of risk factors, the study is extremely restricted due to some factors just being supported by just one or two studies. References
1. Open Acc J of Sports Med, 2010, 1: 45-54.
2. J Occup Rehabil, 2010, 20: 489-501.
3. The Am J Sports Med, 2009, 37 (5): 955-961.
4. J Orthop Sports Phys Ther, 2013, 43 (6): 352-367.
5. N Engl J Med, 2008, 359: 11, 1108-1115.
6. Skeletal Radiol, 2012, 41: 633-641.
7. J Bone Joint Surg Am, 2003, 01;85(1):4-9
8. Occup Environ Med, 2003; 60:794–797
9. J Rheumatol, 2002, 29: 557-563
10. Am Family Phys, 2007, 15, 75 (2), 194-202
11. Knee Surg Sports Traumatol Arthrosc, 1995, 3:144-147.
12. Clin Sports Med, 1993, 12 (4): 771-796.
Injury specialist, Dr. Alexander Jimenez looks at the latest study about concussion in sports, especially regarding early/on-field assessment and diagnosis of this condition. The proper medical definition of concussion is: a clinical syndrome characterized by immediate and transient change in brain function, including alteration of mental illness and level of consciousness, resulting from mechanical pressure or injury. But, it is more commonly described as an injury to the brain caused by a blow to the head (eg an uppercut in boxing, a clash of heads in soccer or a fisherman moving over the handlebars on the ground etc), which leads to temporary loss of normal brain function, including disturbances in memory, judgment, reflexes, speech, balance and muscle coordination. A less obvious cause is an indirect blow where the force is transmitted up to the head from a different portion of the body -- for example when a stationary rugby player is tackled from behind causing his head to abruptly flick back, with a number of the force of the tackle passing through his brain; the participant may end up concussed without ever taking a direct blow to the head. While bruises and cuts might be present on your face or head as a consequence of this blow, in most cases a person with a concussion never loses consciousness. Because of this, less experienced coaches and sports physicians may not immediately assume concussion, or if they do they presume that it's unlikely to be a cause for concern. But, though some concussions are less severe than others, there's absolutely no such thing as a 'minor concussion'; while a single concussion should not result in permanent damage, another concussion shortly after the initial one doesn't have to be very powerful for its consequences to be fatal or permanently disabling. Animal and human studies support the concept of this so-called 'post-concussive vulnerability', showing that a second blow before the mind has regained results in worsening metabolic changes within the cell(1). This explains the crucial importance of correctly and immediately identifying when a concussion has occurred because it affords the opportunity of this athlete to be taken out of the field of play, thereby ensuring a second concussion cannot happen. Initial Diagnosis Of ConcussionAs soon as an athlete suffers a blow to the head, the first priority should be that someone qualified is available to assess whether concussion has occurred. In an ideal world, this assessment could always be performed by a physician specifically trained in this area. In many sporting events (eg a small league football game), it is unlikely that such a individual will be there standing on the sidelines. However, as stated by the America Medical Society for Sports Medicine (AMSSM), the competence to execute this assessment also needs to be decided by training and experience and not purely dictated by specialty(1). To put it differently, with the right training and expertise, coaches, trainers and health care professionals are more than capable to perform a concussion examination. The AMSSM additionally points out that the identification of concussion is ideally created by a healthcare provider who is not only knowledgeable in the recognition and analysis of concussion but also familiar with the person concerned. The reason for this is that while standardized sideline tests are a useful framework for making an appraisal, the validity and reliability of these tests are greatly reduced without some type of individual baseline test result with which to compare, and some other baseline rating will vary based on the individual athlete concerned. AMSSM New GuidelinesThe primary recommendations were assembled by reviewing the evidence over a number of years and are summarized as follows: - Any athlete suspected of having a concussion should be stopped from playing and assessed by a qualified healthcare provider trained in the evaluation and management of concussion and ideally someone who is familiar with the athlete (for the reasons given above). The recognition and initial assessment of a concussion should be guided by a symptoms checklist, cognitive evaluation (which should include orientation, past and immediate memory, new learning and concentration), balance tests and further neurological and physical examination.
- Coaches/physicians/healthcare providers should take note that while balance disturbance is a specific indication of a concussion, it isn't very sensitive. In particular, performing equilibrium testing about the touchline may yield substantially different results than baseline evaluations simply because of differences in shoe/cleat-type or surface, use of ankle tape or braces, or the presence of other lower extremity injuries that might have also happened during the episode involving the head injury.
Any athlete suspected or diagnosed with a concussion should be monitored for deteriorating physical or mental status. Importantly, there should be NO same day return to play for an athlete diagnosed with a concussion injury. Meanwhile, imaging should be reserved for athletes where intracerebral bleeding is suspected. - Even though most concussions can be managed appropriately without the use of neuropsychological (NP) testing, those with athletes in their maintenance ought to bear in mind that NP evaluations are an objective measure of brain- behavior relationships and, as such, are somewhat more sensitive for subtle cognitive impairment than a straightforward clinical examination. However, NP testing should be used only as part of a extensive concussion management plan and should not be utilized in isolation. Also, the ideal timing, frequency and type of NP testing have not been completely ascertained.
- Computerized NP testing should be translated by health care professionals educated and comfortable with the type of test and also the individual test limitations. Paper and pencil NP evaluations are both valuable and are able to test different domain names and assess for different conditions, which may masquerade as or reevaluate evaluation of concussion.
- Concussion symptoms must be resolved before returning to perform with (RTP) and RTP after concussion should happen just with medical clearance from an experienced health-care supplier trained in the analysis and management of concussions -- see Box 2. An RTP progression entails a gradual, step-wise increase in bodily demands, sports-specific activities and the danger of contact. If any signs recur using action, the progression ought to be stopped and resumed in the previous symptom-free step. In the brief term, the principal concern with early RTP is diminished reaction time resulting in an increased risk of a repeat concussion or additional injury and prolongation of symptoms. In the long run, there's a growing concern that head impact exposure and recurrent concussions can contribute to long-term neurological complications and a number of studies have indicated an association between previous concussions and chronic cognitive impairment.
- Physicians should be prepared to offer counseling regarding potential long-term consequences of a concussion and continuing concussions. However, there are currently no evidence-based guidelines for disqualifying/retiring an athlete from a game after a concussion. More commonly, greater efforts are needed to educate involved parties, such as athletes, parents, coaches, officials and school administrators and health care providers to boost concussion recognition, prevention and management.
Recent Findings: On-Field & Same Day AssessmentMake no mistake, but the first assessment of concussion in the mature athlete is tough, given that the elusiveness of harm, the sensitivity and specificity of their sideline assessment tools along with the evolving nature of concussive injury. A very current (2013) review newspaper systematically examined the evidence related to on-field concussion assessment and considered questions related to same day return to play, what to do if no doctor is available onsite, as well as the benefit of distant notification of future concussive events(3). It concluded that the on-field test of sport-related concussion is often a challenge, especially given the elusiveness and variability of presentation, the strain to create a quick diagnosis (as an instance, in the middle of an important match in which the concussed athlete was making a significant contribution), the specificity and sensitivity (or rather lack of) of this on-field assessment tools, along with the dependence on symptom presentation. However, they cautioned that a range of assessments over a brief time period tend to be necessary and, since signs and symptoms may be postponed, erring on the side of caution (ie maintaining an athlete from participation whenever there's a distress for harm) is important. In addition, they concluded that although a standardized evaluation of concussion is beneficial in the evaluation of the athlete with suspected concussion, it should NOT take the place of the clinician's conclusion. These findings have been very much in agreement with another 2013 review research on instruments currently utilized in the evaluation of sport-related concussion on the day of injury -- consequently 'same day' assessment tools(4). In this review, a total of 41 research on sports concussion were pooled and their findings analyzed. The authors concluded that several well- supported tests are acceptable to be used in the evaluation of acute concussion from the athletic athletic environment and that these evaluations can provide significant data on the symptoms and functional impairments that clinicians can integrate in their diagnostic formula. But they also cautioned that such tests should not solely be used to diagnose concussion. SCAT3 Assessment ToolAs mentioned above, the first evaluation of an injured athlete with suspected concussion remains predominant in determining subsequent action. There are a number of diagnostic tools available, but undoubtedly among the most admired is when there is no one with medical training available to tend to an injured athlete, it is recommended that the ‘Sport Concussion Recognition Tool’ be used instead (seeBox 3). The SCAT3 assessment tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf. The SCAT3 is a standardized instrument for evaluating injured athletes for concussion, and is intended for use by medical professionals. SCAT3 supersedes the first SCAT and SCAT2 published in 2005 and 2009 respectively. Importantly, baseline testing together with the SCAT3 can be beneficial for translating post-injury test scores at a later date. The SCAT3 evaluation tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf SCAT3 is a detailed tool that assesses the following areas: background, symptom evaluation, cognitive and physical function, neck trauma, balance and coordination. According to the SCAT guidelines, the first indications through a sideline evaluation are critical and any of the following warrants triggering emergency procedures and barbarous transport to the nearest hospital: - a Glasgow Coma score of less than 15 (see Box 4)
- deteriorating mental status
- potential spinal injury
- progressive, worsening symptoms or new neurologic signs.
It is important to highlight, but that scoring on the SCAT3 shouldn't be utilized as a stand-alone process to diagnose concussion, quantify recovery or make conclusions regarding an athlete's readiness to come back to competition after concussion. Additionally, since signs and symptoms can evolve over time, it's very important to consider repeat evaluation from the acute evaluation of concussion. Finally, it needs to be stressed that the identification of a concussion is a medical judgment, ideally created by a medical professional. The SCAT3 shouldn't therefore be used solely to make, or exclude, the diagnosis of concussion in the absence of clinical judgement. An athlete could have a concussion even if their SCAT3 score is 'normal'. References
1. Br J Sports Med. 2013 Jan;47(1):15-26. doi: 10.1136/bjsports-2012-091941
2. Am J Sports Med. 2012 Apr;40(4):747-55
3. Br J Sports Med. 2013 Apr;47(5):285-8
4. Br J Sports Med. 2013 Apr;47(5):272-84
5. Br J Sports Med 2013 47: 259
6. downloadable from: http://bjsm.bmj.com/content/47/5/267.full.pdf
Science based chiropractor, Dr. Alexander Jimenez looks at frequent mechanical causes of heel pain -- and how they can be seen and treated. Plantar heel pain is a frequent presentation to sports clinicians and might be result of mechanical, neurologic, traumatic or other systemic illnesses(9). Plantar fasciitis is undoubtedly the most common pathology in this area seen by cliniciansnonetheless, other causes of heel pain has to be considered when assessing a customer with heel pain. Up to two million Americans report heel discomfort each year at a price estimated to be up to $400million(5). Despite this, little is known about the pathophysiology and etiology of plantar heel pain. This article will discuss plantar fasciitis in addition to other frequent mechanical causes of heel pain such as plantar fascia tears/rupture, heel pain of neurological source, calcaneal stress fracture and atrophy of the heel pad. The anatomy of each of those illnesses will be discussed as well as diagnostic criteria and potential treatment choices will be summarized. Plantar FasciitisThe plantar fascia is fibrous aponeurosis that spans from the calcaneal tuberosity to the proximal phalanges(6) (see Figure 1). Plantar fasciitis most commonly occurs by mechanical disturbances because of either bio- mechanical flaws, obesity or work habits(10). The plantar fascia will help to encourage the lateral longitudinal arch and acts as a shock absorber(3). Support of the lateral longitudinal arch is reached via both passive tensioning of the plantar fascia (the Windlass mechanism) as well as lively tension of the plantar intrinsic foot muscles (includes flexor hallicus brevis, adductor hallicus and plantar interossei) and the tibialis posterior. As strength testing of those muscles is very difficult, Chang used volume estimations of their intrinsic foot muscles and tibialis posterior muscles to find out whether there was a gap in quantity of those muscles in individuals with knee pain. He found no difference in muscle mass of tibialis posterior and just 5% difference in the forefoot volume of the intrinsic foot muscles as well as the asymptomatic foot(5 pounds). Further studies will need to be done to determine whether that is of clinical importance and whether strengthening of those intrinsic foot muscles decreases load onto the plantar fascia. Assessment & DiagnosisPatients presenting with plantar fasciitis most often complain of pain on the first few steps in the morning when getting out of bed or after prolonged rest(2). This has been termed "post- static dyskinesia"(2). Maximal tenderness is over the origin of the plantar fascia on the medial calcaneal tuberosity(2). Jack’s test, which involves passive extension of the first MTP joint, tests the integrity of the plantar fascia and the Windlass mechanism (see Figure 2). It has been shown that reduced dorsiflexion ROM, improved BMI and bad biomechanics are risk factors for plantar fasciitis(4). This could include but should not be limited to: - midtarsal, subtalar and ankle ROM
- calf flexibility
- gait assessment
- footwear inspection.
Generally diagnosis is completed via ultrasound although weight-bearing radiographs may be useful to determine the existence or absence of calcaneal spur in addition to the elevation of this calceneal fat pad(10). In the case of plantar fasciitis, ultrasound guided examination of the plantar fascia at its proximal insertion shows: 1) fascial thickening greater than 4-5mm, 2) deceased echogenicity, 3) perifascial effusion may occasionally be seen(4). An infra-calcaneal spur might be present but these also have been observed in asymptomatic individuals also, and elimination of the spur doesn't appear to add to the achievement of plantar heel pain surgery(10). TreatmentThe Heel Pain Committee of the American College of Foot and Ankle surgeons, based on available evidence in 2010, determined three tiers of treatment modalities for plantar fasciitis(10). They said that Tier 1 treatment options must be trialled first, which include: - padding and strapping of foot
- stretching exercises of calf and foot
- home cryotherapy
- avoidance of barefoot or flat shoes
- over-the-counter arch supports/heel cup
- oral anti-inflammtories
- corticosteroid injection
- weight loss.
If no response was noted after six months with these modalities afterward Tier 2-based treatments should commence whilst continuing Tier 1 remedies. Tier 2 choices included: - night splints
- further injections
- immobilization
- prescription orthotics.
The combination of using foot orthotics and dorsiflexion night splints was shown to be more effective than use of orthotics alone(12). Following these recommendations, they reported that 85-90 percent of patients will respond to treatment within 8-12weeks and have full resolution at the same year. The Tier 3 treatment option they explained was operation, which should only be considered in those patients who neglect Tier 1 and two treatment pathways. Traditionally corticosteroid has been the injection of choice with respect to plantar fasciitis; however, some evidence points to short-term relief only. As well as poor long-term effects, other risk factors related to corticosteroid injection (CSI) such as fat pad atrophy, osteomyleitis of the calcaneus and iatrongenic rupture have all been reported(2). Platelet rich plasma (PRP), which is a concentration of platelets derived from the plasma part of autologous blood (like growth factors), has also been trialled as a treatment option for plantar fasciitis. Aksahin compared CSI and PRP and reported comparable results at three months and six months (approx 50% drop in VAS scores) also claimed that contemplating the risk factors related to CSI PRP might be a better alternative option(1). Diaz-Llopis compared botulinum toxin type A (botox) with CSI and revealed that the botox group was slightly better at one month but considerably better than the CSI team at both six and twelve months(7,8). Additional research has to be conducted on which injection modality gets the best results over both the short and long term. Plantar Fascia Tears/RuptureIntense strains of the plantar fascia occur quite frequently and normally, should they happen in isolation, react relatively quickly to treatment. They may be associated with plantar fasciitis, particularly if a CSI was trialled. Clients with an acute tear describe a sudden beginning heel pain and may have localized tenderness over the plantar fascia, along with a palpable lump might be present in case a partial or total rupture is present(4). In the case of significant tears that they are going to have pain on weight bearing. Treatment is symptomatic and involves initially a non-weight posture boot and innovative weight bearing with inviting taping and/or orthotics as pain allows. Heel Pain Of Neural OriginUp to 15-20 percent of individuals with plantar heel pain is brought on by entrapment of branches of the tibial nerve(2). This nerve can get entrapped in the possible sites: 1) where the nerve passes at the sharp edge of the abductor hallicus; 2) just distal to the medial edge of the calcaneus; 3) due to compression between the abductor hallicus and the quadrates plantae muscles. The second most frequent cause of heel pain of neural origin is entrapment of the medial calcaneal nerve which innervates the heel fat pad and superficial tissues overlying the inferior calcaneum(two). Most branches of the nerve lie superficial to the intrinsic muscles of the foot so it is less likely to be compressed within these muscles, but might be compressed or irritated following heel pad atrophy(2). Assessment & DiagnosisMuch like plantar fasciitis, their pain is most often worse after intervals of rest but might also occur at rest and at non-weight bearing positions. Although paraesthesia or anesthesia is infrequent, it may be reported around the medial or plantar surfaces of the heel(2). On physical examination, nerve entrapment should be suspected if the site of maximum tenderness is over the nerve. Neurodynamic testing may play a part in the identification of nerve involvement of plantar heel pain. Altered straight-leg increase testing that additional dorsiflexion, eversion and toe extension increased strain on the tibial nerve and LPN and when hip flexion was inserted no additional load on the plantar fascia has been noted(2). Differentiation of the plantar fascia as well as the tibial nerve may be carried out with the addition of hip flexion. Figure 3 shows the modified SLR for the tibial nerve and its branches. TreatmentDespite its various pathophysiology and etiology, current study suggests the treatment of plantar heel pain of neurological source should be similar to that for plantar fasciitis. This absence of specific treatment options for your differing presentations may be among the reasons why plantar heel pain may be so recalcitrant. It could be suggested, like nerve entrapments in different parts of the body, "port" function and nerve gliding or sliding exercises may be useful to cure and prevent ongoing entrapment. Further studies need to be done in order to determine the most effective treatment for all these neural entrapment syndromes of the foot. Fat Pad Atrophy/ContusionThe calacaneal fat mat comprised of elastic fibrous tissue and carefully packed fat cells that act as a shock absorber on heel strike(4). This problem is often related to plantar fasciitis but can be an isolated thing. Patients with fat pad atrophy may report pain aggravated with walking particularly in hard shoes or on hard surfaces(4). Commonly due to the heel strike pattern, pain is felt more over the lateral aspect of the heel that helps to differentiate it from plantar fasciitis. Stress fractures of the calcaneum are quite common and mainly occur at the upper posterior margin of the os calcis or adjacent to the medial calcaneal tuberosity(4). Patients with a calcaneal stress fracture will report insidious onset heel pain which unlike other plantar fasciitis worsens with activity(4). On palpation they'll be tender over the lateral or lateral aspect of the calcaneum and pain will be replicated by the squeeze test (see Figure 4). Plain X-ray or MRI could be used to validate the diagnosis. Remedy of calcaneal stress fractures involves a period of non-weight bearing rest until the pain disappears; walking and then gradual return of activity can occur after using soft heel pads and coaching to improve biomechanics. ConclusionThis article has outlined several pathologies that needs to be considered when assessing clients with heel pain. Treatment modalities should be aimed at preventing pain and fixing potential predisposing factors. References
1. Aksahin E et al (2012) The comparison of the effect of corticosteroids and platelet rich plasma (PRP) for the treatment of plantar fasciitis. Archives of Orthopaedic Trauma and Surgery. Vol 132 781-785.
2. Alsahmi A, Souvlis T, Coppieters M (2008) A review of plantar heel pain of neural origin: Differential diagnosis and management. Manual therapy vol 13 103-111.
3. Anderson J, Stanek J (2013) Effect of foot orthoses as treatment for plantar fasciitis or heel pain. Journal of Sport Rehabilitation Vol 22 130-136.
4. BruknerP and Khan K (2012) Clinical Sports Medicine 4th edition McGraw Hill.
5. Chang R, Kent Bruan J, Hamill J (2012) Use of MRI for volume estimation of tibialis posterior and plantar intrinsic foot muscles in healthy and chronic plantar fasciitis limbs. Clinical Biomechanics. Vol 27 500-505.
6. Chen C, Lew H Chu N (2012) Ultrasound guided diagnosis and treatment of plantar fasciitis. American Journal of Physical and medical Rehabilitation, Vol 91 (2) 182-184.
7. Diaz-Llopis I et al (2011) Randomised controlled study of the efficacy of the injection of botulinum toxin type A versus
corticosteroids in chronic plantar fasciitis: results at one and six months. Clinical Rehabilitation Vol 26 (7) 594-606.
8. Diaz-Llopis et al (2013) Botulinum toxin type A in chronic plantar fasciitis:clinical effects one year after the injection. Clinicla Rehabilitation Vol 27 (8) 681-685.
9. Dizon J et al (2013) Effectiveness of extracorporeal shock wave therapy in chronic plantar fasciitis: A meta-analysis. American Journal of Physical Medicine and Rehabilitation Vol 92 no7 606-620.
10. Thomas J et al (2010) the diagnosis and treatment of heel pain: A clinical practice guideline-revision 2010. The Journal of Foot and Ankle Surgery. Vol 49 S1-S19.
11. Wearing S et al (2010) Plantar enthesopathy: thickening of the enthesis is correlated with energy dissipation of the plantar fat pad during walking. The American Journal of Sports Medicine Vol 38 (12) 2522-2527.
12. Winson L, Wong W, Kung E, Leung A (2012) Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis Vol 49 (10) 1557-1564.
Injury chiropractic scientist, Dr. Alexander Jimenez looks at how knees can be hyperextended and hurt during sport -- and the way they can be treated. Knee hyperextension injures could be chronic or acute in their presentation and are often very painful. Structures that are most frequently injured because of knee hyperextension are the infrapatella fat pad (IPFP) or in the event of an acute hyperextension injury (for example when being handled in rugby) trauma to the anterior cruciate ligament (PCL) and/or the posterior lateral corner (PLC) of the knee. This article will talk about both chronic and acute hyperextension injuries of the knee. Additionally, it will outline the anatomy of this infrapatella fat pad, the PCL and the posterolateral corner (PLC). Injury mechanics will be discussed in addition to treatment options. Infrapatella Fat PadAnatomyThe infrapatella fat pad is an extrasynovial structure which sits on the anterior aspect of the knee only distal to the patella. It is portable and its form, pressure and quantity all alter with knee movement(two) It is attached anteriorly to the proximal aspect of the patella tendon and inferior pole of the patella and posteriorly it attaches to the intercondylar notch of the femur and in some people the ACL(2) (see Figure 1). It is a richly vascularized arrangement and is innervated by branches of the obturator, saphenous and common peroneal nerve(2). Its nociceptive fibers are most dense in the central and lateral parts(two). Mechanism Of InjuryBoth of these conditions can be quite painful and debilitating. These customers will frequently have knees that hyperextend and may walk with inadequate quad core control and knee hyperextension. The IPFP can also be injured by trauma to the knee. This may either be through blunt effect or through shear injury with a patella dislocation or ACL rupture. Iatrogenic causes also have been clarified as a result of location of arthroscopy portals and possible for fibrosis. AssessmentOn evaluation a patient with a disorder of the IPFP will often clarify a sharp, burning and or aching pain profound and on each side of the patella tendon. Pain- provocative activities include maximal knee extension or actions that need active knee extension, moving upstairs or prolonged knee flexion(1). Several clinical evaluations are used to differentially diagnose IPFP disorders from other pathologies about the knee. Patients with IPFP ailments will often have swelling inferior to the patella and may describe that they have "bloated" knees (see Figure 2). Objective tests include: 1) Hoffa’s test: The IPFP is palpated (either side of the patella tendon) with the knee in 30-degree flexion. The knee is then fully extended (passively) and increased pain in the IPFP indicates a positive test (see Figure 3). 2) Passive knee extension test: The patient lies supine and the knee is passively extended. Pain inferior to the patella indicates a positive test. 3) Differentiation test: This test is to help differentiate between IPFP and patella tendon disorders. The location of most tenderness is palpated in 30-degree knee flexion. Whilst continuing to palpate the location of most tenderness, the patient is then asked to gently activate the quadriceps muscle, and the clinician resists this movement. Isometric activation of the quadriceps “lifts” the patella tendon off the IPFP which would decrease the pain on palpation if the IPFP is the cause of the pain. ImagingWhen imaging is required, MRI is the modality of choice for suspected injuries to the IPFP. Increased T1 or T2 hypointense signals may indicate fibrosis of the fat pad. T2 weighted images that that show hypointense signal may indicate inflammation or acute haemorrhage or oedema. TreatmentDisorders of the IPFP most commonly respond quite well to traditional therapy. The main goal of treatment is to de-load the fat pad to reduce pain and permit quadriceps strengthening to occur. Fat pad de-loading tape ought to be educated to the patient so continual impingement of the fat pad is prevented (see Figure 4). Both posture and gait retraining should occur early so knee hyperextension is averted during these actions. Muscle retraining ought to be based around quadriceps strengthening exercises particularly in closed kinetic chain rankings. Exercises which can be beneficial in the rehabilitation process include wall squats, splits squats, squats but exercises that involve complete knee extension should be avoided. In the elite athlete where resting from instruction is tough, a CSI may be practical to help decrease pain. Posterior Cruciate Ligament (PCL) InjuriesThe PCL, though most commonly injured when the knee is flexed, may also be hurt in a forced hyperextension of the knee (rugby tackle). It's been estimated that about 60% of PCL injuries also have the posterolateral corner and this may be higher in injuries that demand knee hyperextension(1). AnatomyIt comprises of an anterolateral bundle which can be most tight in knee flexion and a posteromedial package which is tight in extension(3). The posterolateral corner (PLC) consists of their poplitues muscle, the lateral collateral ligament, bicep femoris tendons along with also the popliteofibular ligament (see Figure 5). Isolated harm to the PLC is rare but is frequently associated with PCL injuries. AssessmentThe patient with PCL injury will frequently complain of poorly defined knee pain and often with minimal swelling. Several tests are Utilized to help determine whether harm to the PCL exists: 1) Posterior drawer: This test involves the patient lying supine with the knee bent to 90 degrees. The position of the tibia relative to the femur is noted with posterior-positioned tibia indicative of a PCL injury. 2) Posterior sag: The patient lies supine with hips flexed to 90 degrees and knee bent to 90 degrees. The practitioner supports under the lower calf of both legs and looks for posterior sag of the tibia (see Figure 6). 3) Quad contraction test: If posterior tibial translation is suspected with the patient in supine and the knee bent to 90 degrees. The clinician holds the lower shin and asks the patient to contract quads. If a posterior sag is present then contraction of the quadriceps will lead to anterior translation of the tibia. PCL injuries are rated from 1-3 and are best quantified with the knee in 90-degree flexion in which the tibia normally lies 1cm anterior to the femoral condyles. The grading process is outlined below: G1: the tibia lies anterior to the femioral condyles but this distance is diminished to 0-5mm; G2: the tibia lies flush with the condyles; G3: the tibia can be pushed beyond the medial femoral condyle. As stated before, injuries to the posterolateral corner may also occur with injury to the PCL once the knee is hyperextended. Several tests have been described to help identify if a posterolateral corner injury is present: 1) External rotation recurvatum (hyperextension) test: The patient lies supine and stabilizes the distal thigh with one hand whilst lifting the great toe with the other. If more hyperextension is noted in the affected knee then a posterolateral corner injury is suspected (see Figure 7). 2) Dial test: The patient lies prone with the knees flexed to 30 degrees. The clinician externally rotates the tibia of both legs (ensuring the thighs remain stabilized). An increased range of external rotation of greater than 10 degrees indicates a positive test (see Figure 8). This test can also be done with the knees flexed at 90 degrees and if there is still increased range then a combined injury to the PCL and PLC is suspected. Gait assessment also needs to be undertaken and those patients with instability of their posterolateral corner have varus gapping in foot attack when their knee is extended. ImagingPCL and PLC injuries generally occur in the acute injury. In case of a substantial acute injury x-rays could be warranted to rule out bony avulsion of the PCL from its tibial insertion. If this is present then surgical repair should be undertaken. MRI might again be beneficial to identify PCL and PLC accidents. TreatmentResults reveal that patients with isolated PCL tears have a fantastic functional outcome (even though continuing laxity) with a structured rehabilitation program. The literature does suggest, however, that PCL lack does lead to greater joint contact pressure on both the patellofemoral and tibiofemoral joints. Surgery is indicated if PCL injury happens in combination with other structures (including PLC) or even if important instability exists. If the PCL injury is important (grade 3) then the customer should be immobilized in extension for 2 months(1). If a slight injury (grade 1-2), then a graduated rehab program ought to be commenced with specific emphasis on quadriceps strengthening. Table 1 outlines a rehabilitation program following a regular 1-2 PCL injury. These timeframes should be used as a guide only and progression throughout the rehabilitation program should be decided by the customer's ability as opposed to a predetermined timeframe. ConclusionHyperextension injuries at the knee may not occur commonly but may be significant. Unless multiple constructions have been hurt, a well-structured rehab program gives very good results. References
1. Brukner and Khan (2012) Clinical Sports Medicine 4th Edition. McGraw Hill.
2. Dragoo J, Johnson C, McConnell J (2012) Evaluation and treatment of disorders of the infrapatella fat pad. Sports Medicine. 42 (1) 51-67.
3. Grassmayr M, Parker D, Coolican M, Vanwanseele B (2008) Posterior cruciate ligament deficiency: Biomechanical and biological consequences and the outcomes of conservative treatment A systematic review. Journal of Science and Medicine in Sport. 11 433-443.
Injury specialist, Dr. Alexander Jimenez reviews the middle and forefoot anatomy -- also discusses several common athletic injuries. The foot consists of 26 interconnecting bones. The intricate anatomy of the foot makes it to be both a passive service structure and an active vehicle for force production (see Figure 1). The mid foot begins at the transverse tarsal, or midtarsal, combined. The talus, navicular, calcaneus, and cuboid bones include this joint. The connections between these bones form an 'S'-shaped single joint line across the waist of the foot, with the navicular bone itself function as the structural link between the forefoot and hindfoot. The multiple articulations within the joint permit the forefoot to move independently in response to hindfoot movement. All five rays, comprised of the metatarsals and phalanges, work in concert to maximize foot stability. Navicular Stress FractureA once obscure identification, navicular stress fractures, now account for 14% to 35 percent of all reported stress fractures(1). It's a particularly widespread investigation in runners, and athletes that execute volatile jumping, as in track and field sports. Suspect a navicular stress fracture in an athlete that complains of obscure mid foot pain but who can not remember actually hurting his foot. Palpation of the apex of the dorsal aspect of the navicular, called the 'N' place, causes pain in 81 percent of patients having a stress fracture(1). The navicular lies at the crossroads of their longitudinal and transverse arches, and thus endures a unique utter stress in the middle third of the bone, where it's the most susceptible to fracture. The center third of the navicular is also the area with the least amount of vascularization. For this reason, fracture in this website resolves slowly. Treatment requires at least fourteen days in a non-weight posture throw(1). One to 2 weeks following boot elimination, begin running and sport-specific training as tolerated, with weekly clinical evaluation of the navicular. If tenderness over the palpated navicular yields, refer for further immobilization or surgery. With conservative therapy, athletes typically return to game in five to six months, compared to three to four weeks for people who undergo surgical fixation(1). Lisfranc Joint InjuryNamed after Napoleon's field surgeon Jacques Lisfranc, who first observed this mid foot injury in men who had dropped from their horse in battle, this injury is due to forced plantar flexion at the joint. In today's sports, the mechanism of trauma is an axial load put on the elevated heel, usually from a fall or tackle by a different player (see Figure 2). Lisfranc injury is not uncommon in American football players (especially lineman in blocking stance, up on feet), football players, bicyclists, surfers, and equestrians. In sports which require feet in straps or clips, a Lisfranc injury may result in the entrapped forefoot in a fall. An injury to the Lisfranc joints most commonly occurs medially, with a consequent separation of the first and second metatarsals, along with a dorsal displacement of the second metatarsal on the next cuneiform. Trainers with a Lisfranc injury normally present with significant pain, moderate to severe swelling, and bruising at the mid foot. Initial radiographic studies don't detect joint diastasis in up to a third of cases; therefore, weight bearing x-rays are justified if Lisfranc injury is suspected(2). An uncommon harm to the lateral Lisfranc joints happens as result of forced supination, and usually with no dislocation of the fracture or joints. When just the ligaments of the joint are injured, care for the sprain conservatively. Begin weight bearing as tolerated but protect the joint by hammering the foot, using an orthotic shoe insert, or, in severe circumstances, immobilizing the joint using a walking fracture boot. Advance the athlete to cross- training activities, like swimming or biking, as soon as possible to keep fitness. Progress rehab to shut chain activities as tolerated. The athlete might need to utilize joint protection through taping, a shoe insert, or a stiff- soled shoe for up to 12 months(3). If the injury does not significantly improve after several weeks, ask repeated x-ray assessment in a weight bearing position. Post-operatively, the athlete is generally non-weight posture for three to six weeks; however, encourage range of motion exercises with the feet, even while immobilized from the post-operative splint. Screw removal takes place between three to four months post-procedure, depending upon individual protocols. Rehabilitate with speed, strength, and endurance training as well as tolerated. Return to play just when the athlete illustrates closed-chain plantar flexion strength and single limb equilibrium appropriate for their sport, normally within four to six months. Metatarsal Stress FractureDuring extended periods of training, muscles on the bottom of the foot fatigue and fail to protect the metatarsals from floor reaction forces. With no plantar muscles to dissipate this stress, the bones suffer recurrent micro-trauma that results in stress fractures. Athletes complain of obscure forefoot pain that resolves with rest, but intensifies with continued instruction. The forefoot might be bloated and bruised. X-rays performed shortly after symptoms begin may not demonstrate a fracture; however, a bone scan or magnetic resonance image (MRI) often reveals the severe injury. These fractures usually respond well to conservative therapy with weight bearing as tolerated but restricted activity for four to six weeks. Following six weeks, restart game training as tolerated and track for a return of symptoms. Using custom orthotics corrects biomechanical problems, such as flat feet, which could induce the athlete to repeated injury. Dancer's FractureAn avulsion fracture at the tuberosity at the base of the fifth metatarsal may be known as a 'dancer's fracture'. Within an avulsion fracture, the athlete complains of pain, bruising, and swelling in the base of the fifth metatarsal. This injury often accompanies a foot sprain. Simple avulsion fractures respond well to conservative treatment of rest, ice, compression and protection. Permit weight bearing as tolerated at a splint or walking boot. Symptoms usually improve within six to eight months, at which time progressive return to sport training begins. Monitor the athlete clinically for any signs of mal-union of the fracture. Avulsions with displacement are treated surgically. Jones FractureAcute fractures of the shaft of the fifth metatarsal are known as Jones fractures, called after Sir Robert Jones who first described this fracture in his own foot in 1902(4). Jones fractures happen if the heel is off of the floor and also a force is applied to the forefoot in the lateral direction, causing the ankle to reverse and roll cartilage. This region is minimally vascularized and are also the website of repetitive micro-trauma. This sort of fracture happens in amateurs, footballers, baseball and hockey players, who commonly pivot to a plantar flexed foot. An athlete with a Jones fracture poses with pain, swelling, and bruising at the bottom of the fifth metatarsal. Weight bearing may be difficult. Fractures are categorized into three kinds. Type I is a serious fracture with clean margins and no displacement, and responds well to conservative therapy. Because of the decreased blood supply to that area of the bone, recovery takes at least six to eight months, and upward of 20 weeks to get complete calcification. A fracture with delayed recovery is classified as a Type II. The fracture line is widened and X-ray reveals increased bone reabsorption at the margins of the fracture. A Form III is absolute non-union of the fracture. Types II and III may be because of repetitive micro trauma at the website prior to a serious event, or even the lack of vascularization which delays recovery from a serious injury. Post- surgical protocols differ, but most progress to partial weight bearing in a walking boot in one or two weeks. Athletes may start partial weight bearing activities, such as aquatic biking and training, at about fourteen days post-op and start working with shoe alterations or orthotics at six to eight weeks after surgery. Most return to sport by 12 weeks post-op. Sesamoid InjuryThe sesamoid bones are two oval-shaped bones inserted in the flexor hallucis brevis tendon, at the distal end of the first metatarsal. These bones function to lengthen the first metatarsal and assist with weight change and toe off through gait. As such, they suffer great stress in athletes that repeatedly 'push off' with the ankle in plantar flexion and the forefoot dorsiflexed, such as runners, dancers, football lineman, and golfers. Of all sesamoid accidents, stress fracture happens 40 percent of the time, whilst sesamoiditis and acute fracture appear in just 30 percent and 10% of cases, respectively(5). As with other repetitive stress injuries, the onset of pain using a stress fracture could be insidious and vague. Passively bending the big toe can reproduce the pain. X-ray evaluation isn't always conclusive in such harms; therefore, a bone scan or MRI may be necessary for diagnosis. Treatment consists of rest from the offending activity together with custom orthotics or a metatarsal pad to eliminate weight bearing directly to the bones. For athletes using sesamoiditis, an inflammatory condition caused by repeated stress to the bones, treat with rest, ice hockey and protection, and gradually initiate a return to action once they bear weight without pain. For those who have actual fracture, six months of non-weight bearing is necessary. If the fracture does not heal adequately following this time, consult with surgery. Athletes possibly return to sport within six months after surgery, which either partly or entirely eliminates the bone, or even fixes the fracture. 'Turf Toe'Dancers, football lineman, rugby players, golfers, and wrestlers often assume a position of MTP joint dorsiflexion with ankle plantar flexion (see Figure 3). More and more flexible shoes, along with artificial turf surfaces, have been implicated in the greater incidence of this harm. Participants present following an acute event with pain and tenderness over the joint, accompanied by swelling and bruising when the injury is categorized as Grades II (partial tear of the ligaments) or III. Conservative therapy with immobilization of the MTP joint through taping or bracing; protection with steel shoe inserts; progressive weight bearing; and restricted activity is the normal treatment course for all MTP harms. Initiate progressive sports instruction after three to six weeks as tolerated, and monitor for a recurrence of symptoms. Surgery is warranted only in the most extreme injuries with joint dislocation or harm to the sesamoid bones. Morton's NeuromaMore common in women than men, Morton's neuroma is a nerve entrapment disease of the nerve between the toes. The nerve becomes thick and painful because of chronic friction together with the adjacent ligaments, for example happens when pivoting in tennis or dancing. Abnormal foot body is thought to contribute to the problem. Athletes whine of burning pain between the feet, at the metatarsal heads. The pain can improve with rest and worsen with activity. A clinical diagnosis can be made with the lateral squeeze evaluation (see Figure 4). Since not a true neuroma, but instead a result of entrapment or compression, sneakers with a large toe box generally improve symptoms. Conservative physiotherapy modalities are sometimes helpful. Therapeutic exercises may also help fortify the foot and reduce strain to the injured nerve. When all else fails, surgical decompression or resection of the nerve eliminates the pain, but results in a level of numbness to the area. ConclusionInjuries into the mid and forefoot result in a significant number of lost playing time in all sports. By some reports, sports- related injuries to the toes comprise 2% to 18 percent of all athletic injuries(6). While many of those mid and forefoot accidents occur needlessly, they do so in regions already exposed, due to either a decreased blood supply and also the biomechanics of the foot structure. To minimize these injuries, use orthotics, taping, and therapeutic exercise to correct biomechanical and structural abnormalities inside the foot. Guide your athletes at proper shoe selection, eschewing whatever the shoe business rep could possibly be telling them is so popular. Look closely at functional deficits in gait and regions of relative weakness or strength imbalance. 1 weak gluteus medius muscle sends ripples down the biomechanical string that could leave a participant pivoting on a foot under more pressure than necessary. References
1. Am Fam Physician. 2003 Jan 1;67(1):85-91.
2. BMJ. 2013 July;3,347:f4561.
3. Clin Sports Med. 1997 July;16(3):435-65.
4. Am Fam Physician. 1999 May 1;59(9):2516-22.
5. Curr Sports Med Rep. Sept/Oct 2011;10(5):249-55.
6. Sports Health. 2012 Nov;4(6):518-34.
|



 Your new post is loading...
Your new post is loading...



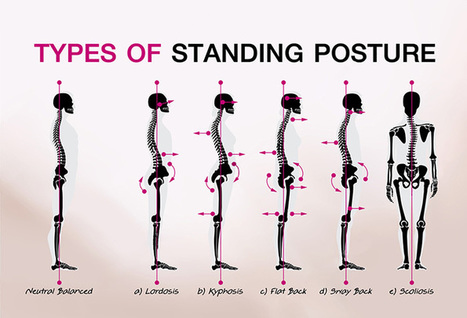


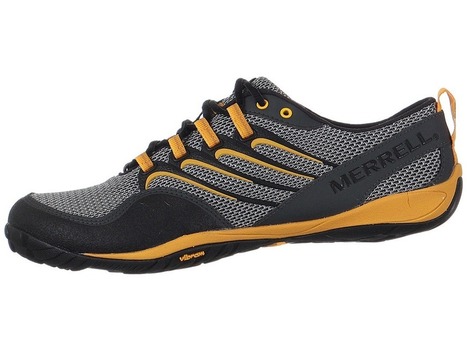









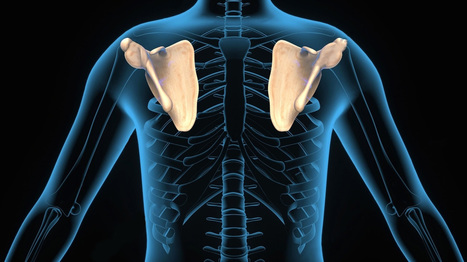





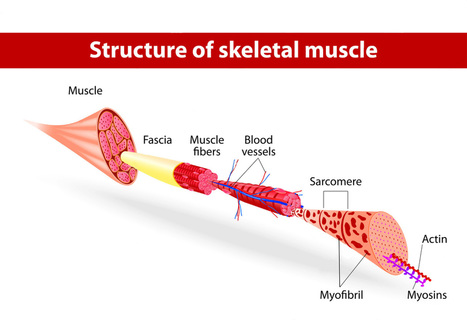

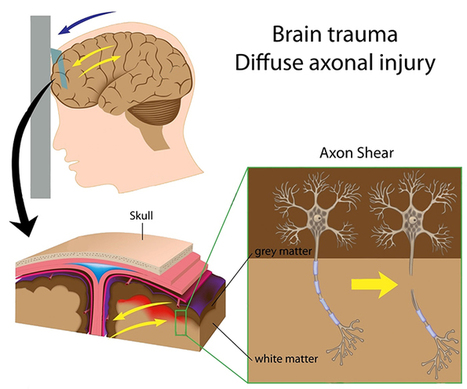


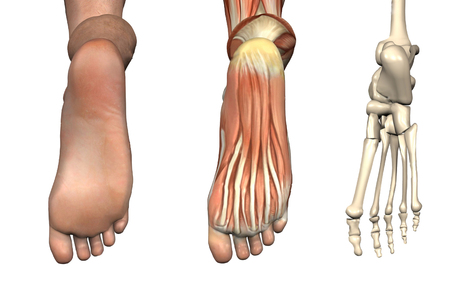





When a body part is not sufficiently mobile or strong to control the forces involved in the client’s chosen activity. For Answers to any questions you may have please call Dr. Jimenez at 915-850-0900