 Your new post is loading...
 Your new post is loading...
Introduction One of the many muscles that help stabilize the shoulders and provide movement when the arms are in motion. The tricep muscles are one of the most underrated muscles that many people don’t seem to take care of when working out. The other muscles in the upper arms and shoulders are more likely to be worked on when it comes to being physically active. The deltoids, biceps, and brachialis muscles are some of the muscles that get much more attention when working on shoulder mobility. Still, the triceps provide the functionality to the shoulders as well. When the shoulders or the upper arms are injured and develop pain-like symptoms in the muscle groups, it can develop trigger points along the affected muscle. Today’s article looks at the tricep muscles, how trigger points affect them, and ways to manage trigger points along the tricep muscles. We refer patients to certified providers who specialize in arm pain treatments to aid individuals suffering from trigger points associated with the tricep muscles along the upper arms and elbows. We also guide and inform our patients by referring them to our associated medical providers based on their examination when appropriate. We established that education is a great solution to asking our providers profound questions the patient requests. Dr. Jimenez DC takes note of this information as an educational service only. Disclaimer What Do The Tricep Muscles Do? Do you experience pain underneath your forearm? How about feeling a dull ache on your elbows? Or do you feel a numbing sensation on your ring and pinky fingers? Individuals experiencing these symptoms in their arms could potentially develop trigger points along their tricep muscles. The tricep muscles are located under the upper arm and are a large, thick horseshoe-shaped muscle at the end of the arm. As stated earlier, the tricep muscles are one of the most underrated muscles in the arm that no one tends to work on during a workout, so they can be easily overlooked. However, the tricep muscles help in providing stability to the shoulders and help strengthen the arms. One of the main functions the triceps offer is that they allow the extension of the elbow joints. Studies reveal that the three head tendons that make up the triceps can influence elbow extension torque. The three heads of the triceps have different patterns of force when it comes to various activities during different shoulder evaluations. To that point, multiple combinations of the shoulder and elbows at different angles can affect the tricep’s shoulder extensions. Since many individuals don’t work on their triceps often, it can potentially develop issues that can make this underrated muscle weak. How Trigger Points Affect The Tricep Muscles? When the triceps don’t get worked on during a workout, it can lead to muscle weakness when doing pushups or when someone suffers from an injury with direct trauma in the elbows. When the tricep muscles become affected, it can lead to chronic conditions that are associated with myofascial pain or trigger points. Trigger points in the triceps can be formed when there are restrictions in extending the elbow joints. Studies reveal that when the triceps become overloaded from overusing the forearms from normal activities, it could potentially lead to tricep tendon rupture. To that point, which leads to the development of trigger points to invoke pain in the triceps and elbow joint. According to Dr. Janet Travell, M.D., trigger points associated with the tricep muscles could potentially involve referred pain in the vicinity of the elbow joints. What this refers to is that trigger points can mimic other chronic conditions so in this case, referred pain caused by trigger points associated with the tricep muscles can be mistakenly attributed to arthritis on the elbow joints. All is not lost, as there are ways to manage trigger points affecting the tricep muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The upper arms allow the individual to move the arms, hands, and fingers, enabling them to do everyday activities without feeling pain or injuries. Different muscles in the upper arms allow precise movements, from threading a needle to throwing a ball across the field. These muscles also work with the shoulders, allowing a full range of motion and flexion. One of the muscles that help the upper arms is the bicep brachii, which provide flexion to the arm. However, like all the muscles in the body, they can succumb to pain caused by trigger points. Today’s article looks at the bicep muscles’ function, how trigger points affect the muscles, and how to manage trigger points associated with the bicep muscles. We refer patients to certified providers who specialize in arm pain treatments to aid individuals suffering from trigger points associated with the bicep brachii muscles along the upper arms. We also guide and inform our patients by referring them to our associated medical providers based on their examination when appropriate. We established that education is a great solution to asking our providers profound questions the patient requests. Dr. Jimenez DC takes note of this information as an educational service only. Disclaimer What Are The Bicep Muscles Function? Have you been dealing with radiating pain down to your elbow? Do your upper arm muscle ache when carrying items from place to place? Or have you experienced muscle spasms in your arms and hands? Many people experiencing these symptoms might risk developing trigger points along their bicep muscles. The bicep brachii is a large, thick muscle that covers the joints and is located in the upper arms. The bicep muscle consists of two attachments: the short head (caput breve) and the ling head (caput longum). It works together with the coracobrachialis muscle to support stability to the shoulders. Studies reveal that these two muscle bands work together to provide multiple actions between the shoulder and elbow joints by being in conjunction with the other muscles. The main function of the bicep muscles is that it is one of the three muscles that can flex the elbow and shoulders. The biceps also allow flexion and supination or outward rotation of the forearms at 90 degrees. This muscle is very important for athletes that require lifting, carrying, or throwing and can make the individual stronger. To that point, the bicep muscle can also succumb to injuries that can cause pain to the upper arms and shoulders. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The shoulders help stabilize the upper extremities of the body and provide a wide range of movements for the arms. The shoulders have many muscles, ligaments, and tendons that help support the joints from injuries and utilize the motor function to do everyday actions like throwing a ball or stretching for long distances. Even though the shoulders help stabilize the upper extremities, they are still prone to injuries since the shoulder muscles are constantly used throughout the day. One of the shoulder muscles that are continuously utilized is the deltoid muscle, which can lead to the development of trigger points when it becomes injured. Today’s article examines the deltoid muscles, how trigger points affect the deltoids and shoulders, and managing trigger points associated with the deltoid muscles. We refer patients to certified providers specializing in shoulder pain treatments to aid individuals suffering from trigger points associated with the deltoid muscles along the shoulders. We also guide and inform our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure that education is a great solution to asking our providers insightful questions the patient requests. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Deltoid Muscle? Have you been feeling pain on the top of your shoulders? Do your shoulders feel stiff when rotating them? Or do you feel radiating pain along your upper arms? Individuals with shoulder pain may be experiencing trigger points affecting their deltoid muscles. The deltoids are large triangular-shaped muscles that are associated with the shoulder girdle. The deltoids sit on top of the shoulder girdle and have anterior and posterior sections that work together with the rotator cuff muscles that provide a full range of motion to the arms. Studies reveal that the deltoid muscles have a more complex structure since the intramuscular tendons from the deltoids help provide different functions when it comes to the shoulders and arms’ motor function. According to Dr. Janet G. Travell, M.D., the anterior sections of the deltoid muscles are used in sports activities. In contrast, the posterior section works with the rotator cuff muscles for mobility. Injuring the deltoid muscles can lead to the development of trigger points associated with shoulder pain. How Do Trigger Points Affect The Deltoids & Shoulders? Regarding the shoulders, they can succumb to various injuries that can become an issue over time, lead to the development of trigger points in the shoulder muscles, and cause referred pain to the upper arms. Trigger points or myofascial pain syndrome along the deltoid muscles may invoke referred pain to the shoulders. Studies reveal that myofascial pain syndrome is often described as the sensory, motor, and autonomic symptoms caused by trigger points that cause tender spots on the hardened muscle to produce pain. Trigger points are a bit tricky to diagnose since they mimic other chronic conditions in the body. The deltoid muscles are superficial, and trigger points can cause referred pain to the muscles that mimic arthritis in the shoulder joints. Some of the other symptoms associated with trigger points along the shoulders and deltoids include: - Limited range of mobility
- Tenderness in the shoulder muscles
- Muscle spasms
- Muscle pain
- Stiffness in the deltoid muscles
Pain in the shoulders can cause the body to become unstable and cause many individuals to develop a hunched position over time to reduce the pain they are feeling; fortunately, there are various ways to manage the pain associated with trigger points along the shoulders and deltoid muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body has various muscle groups that work together to make each section of the body move. The arms, shoulders, and neck muscles in the upper half of the body allow mobility and range of motion without discomfort. The muscles in the midsection protect the vital organs and spine while assisting in rotation. And the low half of the body, which includes the hips, legs, and feet, helps the body to move from place to place. However, just like all muscles, injuries can occur to the body and cause issues if they are not taken care of immediately. This allows the muscle fibers to develop myofascial pain syndrome or trigger points, causing overlapping risk profiles at risk of developing pain in the affected area. For the upper body, when trigger points affect the shoulders, it can lead to referred pain that can affect the arms. Today’s article examines the shoulder muscle known as the subscapularis muscle, how trigger points are associated with the subscapularis, and ways to manage trigger point pain on the subscapularis muscle in the shoulder. We refer patients to certified providers specializing in musculoskeletal pain treatments to aid individuals suffering from trigger points associated with the subscapularis muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure that education is a great solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Subscapularis Muscle? Have you been feeling a constant ache in your shoulder muscles? Does your wrist seem to hurt, making it hard to grasp objects? Or Do you feel pain in your triceps or shoulder muscles? Individuals experiencing these symptoms might risk developing trigger points associated with shoulder pain along the subscapularis muscle. The subscapularis is the largest, strongest muscle of the rotator cuff that lies in the anterior or front of the scapular surface and provides shoulder movement while helping maintain glenohumeral joint stability. The best way to describe how it looks is that it seems like a chicken wing. The subscapularis is also part of the rotator cuff muscles, which includes the teres minor, supraspinatus, and infraspinatus muscles, and is active when a person swings their arms forward. When issues affect the shoulders, it can lead to referred pain affecting the upper extremities, including the hands, arms, and even the shoulders. Trigger Point Associated With The Subscapularis Muscle When injuries affect the shoulders, the muscle fibers that help stabilize the shoulders begin to develop small nodules, known as trigger points, that can invoke pain from the shoulders to the wrist, causing referred pain. The subscapularis and its tendons become affected when it becomes injured and can be prone to tearing. Studies reveal that when the subscapularis tendon has partial tears in the rotator cuff, it would be considered forgotten with “hidden lesions” that can overlap pain symptoms in the shoulders. Active trigger points in the subscapularis muscle can mimic other pre-existing conditions affecting the shoulders. Once the subscapularis tendon has partial tears in the muscle, it can develop trigger points along the subscapularis muscle and become active, causing various shoulder conditions. One of those conditions is frozen shoulders, and studies reveal a strong association between the subscapularis trigger points and the frozen shoulder. The “frozen shoulder” or adhesive capsulitis of the body is a common shoulder condition often characterized by pain, restricted range of motion, and a high morbidity rate. When a person is dealing with a frozen shoulder, it is often mistaken for shoulder stiffness as it doesn’t respond to non-invasive treatments. All is not lost, as there are various ways of manage active trigger points associated with the subscapularis muscle. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction As the body’s most mobile joints, the shoulders are surrounded by muscles, tissues, and ligaments that help support the shoulders and the rotator cuff in mobility function, thus ensuring the shoulders remain in a stable, normal position. As a complex structure that is made up of three bones: the humerus (upper arm bone), the scapula (shoulder blades), and the clavicle (collarbone), the shoulders provide a wide range of motion without feeling pain. When injuries affect the muscles, tissues, and joints of the shoulders, they can potentially develop tiny knots along the muscle fibers and invoke pain-like symptoms on the upper extremities of the body. To that point, it affects not only the shoulders but also the arms and the hands. Today’s article looks at the infraspinatus muscle, how shoulder joint pain is associated with trigger points, and various treatments to manage trigger points related to the shoulder joint. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger points related to the shoulder joints and the infraspinatus muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Infraspinatus Muscle? Do you feel stiffness along your shoulders or upper arms? Does it hurt when you rotate your shoulders? Or have you been experiencing a tingling or numbing sensation traveling down your arms? Many people who experience shoulder pain might be due to trigger points affecting their infraspinatus muscles. The infraspinatus muscle is a muscle that looks like a thick triangle that covers the front of the scapula. The infraspinatus is a part of the rotator cuff muscles or commonly referred to as SITS: - Supraspinatus
- Infraspinatus
- Teres minor
- Subscapularis
These four muscles provide the functionality to the rotator cuffs in the shoulders to allow the arms full range of motion. Studies reveal that rotator cuff activity from these muscles is crucial for normal shoulder motion. To that point, the infraspinatus plays a vital role by providing dynamic stability while producing external rotation at the shoulder. However, traumatic forces can affect the infraspinatus muscles causing lesions and other conditions to affect the shoulders and rotator cuffs, causing pain-like symptoms to the upper half of the body. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body is a functional machine that requires many muscles, organs, ligaments, joints, and tissues that provide everyday movements. In the upper extremities, the head, neck, and shoulders have many muscles, ligaments, and tissues that work together with the nerve roots from the nervous system that provides sensory-motor function to make the fingers move, the shoulders rotate, and the head turns from side to side. When injuries or common issues affect the muscles in the head, neck, or shoulders, it can cause small nodules to form along the muscle fibers of the affected muscle area and cause referred pain in different locations of the body. Today’s article looks at the scalene muscles, how trigger points affect the scalene muscles while mimicking shoulder pain, and how to manage chronic pain associated with trigger points. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger points related to the shoulders affecting the scalene muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Are The Scalene Muscles? Have you been experiencing tingling sensations running down your fingertips? Do you feel stiffness when rotating your neck or shoulders? Or do you feel muscle soreness in your shoulders? Many individuals who are feeling any of these symptoms affecting their neck or shoulders could be dealing with trigger point pain along the scalene muscles. The scalene muscles play a crucial part in the head and neck as they are deep muscles positioned laterally on the cervical tract of the spine. These muscles have three different branches: the anterior, medius, and posterior, which play the role of being accessory breathing muscles while being an important contributor to head and neck movement. To that point, it allows stability to the cervical spine. The scalene muscles even help support and elevate the upper rib cage when a person is lifting, pulling, or carrying heavy objects. However, like most muscles in the body, the scalene muscles can be prone to injury and can develop issues that can affect the upper extremities of the body. Trigger Points Affects The Scalene Muscles Mimicking Shoulder Pain When common injuries like pulling a muscle when carrying a heavy object or even a traumatic injury like being involved in an auto accident can cause pain in the affected area, over time, if not treated, can cause various symptoms to overlap and affect the muscles. When the scalene muscles are affected by injuries, they can develop tiny nodules along the taut muscle fibers and become hyperirritable to the surrounding areas of the upper half of the body. This is known as trigger point pain and can mimic other chronic issues that affect different body areas. To that point, trigger points affecting the scalene muscles may mimic shoulder pain in the upper half of the body. Studies reveal that scalene myofascial pain is a regional pain syndrome that originates pain in the neck area and radiates pain down to the arm. Since trigger points mimic other chronic issues, it is often misdiagnosed as another neck pain associated with radiculopathy when the scalene muscles are affected. When this happens, the muscles become stiff and weak, causing a reduction in the range of movement. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The lower jaw of the body has the mastication muscles surrounding the mandible and provides functionality to the jaw through chewing, moving the lower jaw up, down, left, and right, and speaking. The jaw also has joints known as the temporomandibular joints that slide back and forth to provide movement also. The jaw is also home to the teeth and tongue, which play a role in the mouth by consuming and grinding food into smaller bites to travel down to the gut system. Just like every joint and muscle in the body, common issues or injuries can affect the jaw and cause pain symptoms associated with the problem. Sometimes normal wear and tear can affect the joints in the jaw, or traumatic events can affect the surrounding muscles causing soreness in the jaw area. If the issue involving the jaw is not treated over time, it can lead to chronic disorders and overlap with other chronic disorders that can affect the whole body and the jaw. One of the jaw disorders is TMJ dysfunction, which can cause overlapping symptoms in the jaw and the body. Today’s article examines what TMJ dysfunction is, the signs and symptoms, and ways to manage TMJ dysfunction in the jaw. We refer patients to certified providers who specialize in musculoskeletal and oral treatments to aid individuals suffering from TMJ dysfunction affecting their jaws. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is TMJ Dysfunction? Have you been experiencing muscle pain in your neck, shoulders, and jaw? What about tenderness in your cheek when you lightly touched it? Or do you have difficulty chewing or moving your jaw when speaking? Many of these symptoms are signs that you could be experiencing TMJ dysfunction in your jaw. TMJ dysfunction, or temporomandibular dysfunction, is part of a group of orofacial pain conditions that affects the jaw joint and muscle, thus causing overlapping issues in the lower jaw. TMJ dysfunction also affects the mastication muscles that help move the jaw by making the muscles hyperactive and causing referred pain to the rest of the body. Studies reveal that about 25% of the population does get affected by TMJ dysfunction since it is a degenerative musculoskeletal condition associated with morphological and functional jaw deformities. The Signs & Symptoms Of TMJ Dysfunction On The Jaw TMJ dysfunction may potentially not only cause jaw pain but can also affect the neck and shoulders connected to the cervical spine. Studies reveal that TMJ dysfunction is correlated with neck disability, jaw dysfunction, and muscle tenderness in many individuals that suffer pain with or without TMJ dysfunction. TMJ dysfunction is associated with these issues because the jaw structures are affected by trigger points along the neck and jaw. To that point, TMJ dysfunction is often accompanied by back, joint, and abdominal pain. But how would TMJ dysfunction correlate with these pain issues? Studies reveal that disturbances in the upper body extremities may cause an increase in muscle tension associated with the whole-body imbalance that is potentially causing TMJ dysfunction. Some of the related symptoms of TMJ dysfunction in the jaw include: - Pain in neck and shoulders
- The jaw becomes “locked” in an open or closed position
- Headaches
- Earaches
- Muscle tenderness in the jaw
- Having difficulty chewing
- Swelling on the side of the face
- Body imbalance
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The jaw has a primary function in the head as it allows the muscles to move up and down, helps chew food, and allows the host to speak. Each of the muscles and organs inside the jaw has its functions that will enable the head to function correctly. The mouth, part of the gut system, allows air to travel into the lungs so the body can breathe and consume food to be swallowed and digested to be turned into energy for the rest of the body to move around. The mouth, the tongue, and the teeth have a casual relationship as the teeth can grind the food into small pieces to be digested, while the tongue can taste the food. When issues begin to cause an effect on the jaw, it can lead to symptoms that can, over time, be painful to the surrounding muscles, organs, and even nerve endings along the jaw’s skeletal structure. Today’s article looks at the medial pterygoid muscle, how trigger point pain affects this muscle, and ways to manage trigger point pain on the medial pterygoid muscle. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger point pain associated with the medial pterygoid muscle along the inside of the jaw. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Medial Pterygoid Muscle? Do you have any problems or issues chewing your food? What about throat soreness from swallowing something hard? Or have you noticed stiffness along your jawline? Individuals experiencing these symptoms might be dealing with pain along the medial pterygoid muscle in their jaw. The medial pterygoid muscle is part of the mastication muscles, which includes the temporalis, lateral pterygoid, and masseter muscles of the jaw. The medial pterygoid is a rectangular-shaped muscle that lies inside the lateral pterygoid muscle. The medial pterygoid muscle works together with the masseter muscle as a sling to help stabilize the mandible or the lower jaw. In contrast, the medial pterygoid nerves provide sensory-motor functions to make the lower jaw move and promote chewing action, thus sending nerve signals to travel through the trigeminal nerve and send the information to the brain. Just like any of the different muscles in the body, the medial pterygoid muscle may succumb to injuries that can affect the sensory-motor function of the jaw while triggering various issues to cause more pain to the jaw and the body. How Does Trigger Point Pain Affect The Medial Pterygoid Muscle? When various issues begin to affect the muscles of the body, it can be something simple like repetitive motions that causes the muscles to be overused or injuries that can cause the muscles to become inflamed and, if not treated, can become sensitive to the touch. To that point, tiny knots known as trigger points are formed along the taut muscle fibers that can make the muscle become sensitive and overlap various issues that can cause pain in different body locations. Since the medial pterygoid and the masseter muscle work together, studies reveal that muscle hypertrophy may associate with the masseter, medial pterygoid, or both and can potentially be involved with the risk of dental problems or other issues that are affecting the oral-facial region. Trigger points along the medial pterygoid muscle may be challenging to diagnose due to the referred pain that affects different body areas while mimicking various pain symptoms that become the causes. An example would be a person experiencing ear pain associated with jaw pain. Now how would these two correlate when the person is dealing with ear pain? Since trigger points can mimic other symptoms, the jaw muscles (which include the medial pterygoid) become aggravated and overused, causing referred pain to the teeth overlapping with ear pain. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The head has many functions that provide the body with functionality. The head consists of the skull, which protects the brain, the eyes to make the host see, and the jaw, which has teeth and the tongue to taste and chew food. The neck supports the head to ensure that it is stabilized and functions appropriately. Below the eyes, the jaw has muscles and joints that help stabilize the jaw from hyperextending out while providing motor function. To that point, factors that can affect the jaw could potentially affect the surrounding muscles and joints on the head and neck, causing the individual to be in pain. Today’s article looks at the masseter muscles, how myofascial pain affects the masseter muscles, and ways to relieve myofascial pain associated with the masseter muscles. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from myofascial pain associated with masseter muscle pain along the jaw. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Masseter Muscle? Have you been experiencing headaches located near your temples? Does your jaw feel sore throughout the entire day? Or have tooth pain or ear pain seems to bother you constantly? Some of these symptoms may affect your jaw joints, especially in the masseter muscles. The masseter muscles are powerful quadrangular muscles on each side of the jaw with three divisions: superficial, intermediate, and deep. The masseter muscles are also part of the mastication muscles in the jaw which include: - Temporalis
- Medial pterygoid
- Lateral pterygoid
- Masseter muscles
The masseter muscles also help the jaw function properly, as studies reveal that this quadrangular muscle participates in various activities like mastication (chewing), swallowing, and talking. To that point, the masseter muscles have a relationship with the trigeminal nerve, which provides sensory-motor stimulation for the jaw to move. However, when factors (traumatic or ordinary) begin to affect the masseter muscles and the surrounding muscles associated with the neck and head, pain can either slowly or quickly depending on the severity the muscles have endured. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body incorporates different muscles that have specific jobs to help mobilize the skeletal joints while providing function to the arms, neck, legs, and back. Many individuals use their muscles for everyday uses like lifting and carrying objects, moving from one place to another, and protecting vital organs from damage. To that point, issues like traumatic events, injuries, and environmental factors can affect the body and cause damage to the muscles. When the muscles are affected by these factors, tiny knots can form along the taut muscle band that can cause painful symptoms that affect specific areas in the body. One of the muscles affected by pain is the trapezius muscle, known as the “coat hanger” muscle, which can be associated with chronic symptoms of myofascial pain syndrome. Today’s article examines the trapezius muscle, how myofascial pain affects the trapezius muscle, and how to manage myofascial trapezius pain. We refer patients to certified providers specializing in musculoskeletal treatments to aid individuals suffering from trapezius muscle pain associated with myofascial pain. We also guide our patients by referring them to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC provides this information as an educational service only. Disclaimer What Is The Trapezius Muscle? Have you experienced pain in your neck, shoulders, or mid-upper back? Do you feel headaches occurring near your temples? What about tenderness in certain areas of your body? Some of these symptoms may appear in your trapezius muscles. The trapezius muscle is located across the back that looks like a simple trapezoid with upper, middle, and lower muscle fibers that have different functions for the upper-middle back, shoulders, and neck. While the entire trapezius muscle helps rotates, elevate, and retract the scapula while extending the head and neck, and turning the chin by itself. At the same time, the entire muscle can help with assisting the extension of the cervical and thoracic spine. - Upper Trapezius muscles: allow the shoulders to rise, bend the head and neck, and help support the weight of the upper extremities of the body, including the arms.
- Middle Trapezius muscles: assist with flexion and abduction of the arms around the shoulders at a nearly full range.
- Lower Trapezius muscles: Helps retract the scapula while rotating the glenoid fossa upwards by decompressing the vertebral borders of the scapula. These fibers help assist the flexion and abduction of the arms.
When traumatic forces or injuries affect the trapezius muscles, painful symptoms begin to affect the muscles, causing them to be tender to the touch and affecting different areas in the body. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body is a functional machine that consists of muscles, organs, and skeletal joints that play different parts in making the body healthy as possible. Each section has a casual relationship as they work together and do their jobs separately. The muscles provide protection and movement from daily activities. The organs supply hormones, oxygen, and nutrients, so the body’s internal functions work correctly. And finally, the skeletal joints help with mobility and stabilization for the body to stay upright. When environmental factors or traumatic injuries affect the body, many issues over time may cause damage, and the body may develop pain-related symptoms. Today’s article examines how the musculoskeletal system works in the body, how trigger points affect the musculoskeletal system, and how chiropractic care can help alleviate trigger point pain. We refer patients to certified providers specializing in musculoskeletal treatments to aid individuals suffering from muscle pain associated with trigger points. We also guide our patients by referring them to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer How Does The Musculoskeletal System Works? Have you been experiencing muscle stiffness in specific areas located in your body? Do you feel tenderness in your neck, shoulders, or back? Or do you feel knots along your muscles that are causing you pain? Some of these symptoms are associated with muscle pain in the musculoskeletal system. The musculoskeletal system in the body has muscles, ligaments, and connective tissues surrounding the skeletal joints. Studies reveal that the structure of the musculoskeletal system shows how the surrounding muscles protect the joints and help provide the body functionality. The various muscles in the body offer a range of motion, sensory-motor functions, reflexes, and strength when functioning normally. However, when environmental factors begin to affect the body over time, it can lead to musculoskeletal disorders associated with pain. Studies reveal that when the body succumbs to pain related to musculoskeletal disorders. Musculoskeletal disorders are a common issue that has affected many individuals worldwide and causes various disabilities and symptoms that affect the body. Some of the musculoskeletal disorder symptoms that affect the body include: - Burning sensations
- Muscle twitches
- Fatigue
- Stiffness and aching
- Myofascial trigger pain
How Do Trigger Points Affect The Body? One of the musculoskeletal symptoms associated with muscle pain is trigger points or myofascial pain. Myofascial pain is a common condition involving the muscles and surrounding connective tissues that may be acute or chronic depending on where the pain is located. While trigger points refer to hard palpable nodules in the taut bands of the skeletal muscle that can be active (causes spontaneous pain or abnormal sensory symptoms) or latent (causes no spontaneous pain but shows operational myofascial trigger points characteristics). Studies reveal that myofascial pain can be associated with muscle dysfunction, weakness, and limited range of motion that affects the body. A knot in the muscle in certain body areas can make the muscle hyperirritable, causing painful compression while invoking characteristic referred pain and autonomic phenomena in the body. To that point, it can be difficult for doctors to diagnose since trigger points are caused by traumatic events in the body and can occur in different spots in different people. Trigger points can form all over the body, including: One common characteristic when trigger points affect the body is that they can travel or even spread to the surrounding muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body has a defensive response known as the immune system that comes to the rescue when traumatic events or injuries impact certain areas of the body. The immune system releases inflammatory cytokines to the affected area and begins the healing process to repair the damage while also getting rid of the foreign intruders in the body. Inflammation can be potentially beneficial and harmful to the body, depending on how severe the injury has potentially impacted the area. When inflammation begins to cause an impact on the surrounding muscles, ligaments, and joints, it can lead to chronic issues associated with pain. To that point, it causes the body to be dysfunctional while mimicking other symptoms. Today’s article examines how chronic inflammatory responses affect the joints, their associated symptoms, and how to manage chronic joint inflammation. We refer patients to certified providers specializing in anti-inflammatory treatments to help many individuals dealing with chronic inflammation of the joints. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer How Does Chronic Inflammatory Response Affect The Joints? Have you been experiencing pain in some regions of your body? What about experiencing tenderness in your muscles? Do your joints ache when you are doing everyday activities? If you have been dealing with these issues, it might be due to chronic inflammatory responses affecting your musculoskeletal joints. As stated earlier, inflammation can be both beneficial and harmful to the body, depending on the severity of the impact the body has taken. In its beneficial form, the body activates the immune system and eliminates pathogens from bacteria, viruses, and other environmental triggers to promote healing and tissue repair. This potentially makes the affected area red and inflamed, thus repairing the damaged cells. However, in its harmful form, studies reveal that chronic inflammatory responses can break down immune tolerance, causing significant alterations to all the tissues, organs, and joints. To that point, the residual effects of high inflammation can cause harm to the joints and cartilage, making them potentially involved with pain and possibly deformity over time. The joints help keep the body moving, surrounded by connective muscle tissue that helps stabilize the body; when chronic inflammatory responses start to affect the joints, they can become a mediator for pain and discomfort while triggering musculoskeletal disorders. Studies reveal that inflammation in the joints can cause damage to the cartilage and result in degenerative changes to the body. This includes functionality loss, joint instability, and other symptoms associated with chronic joint inflammation. The Symptoms Associated With Chronic Joint Inflammation When it comes to chronic joint inflammation, it can mimic other chronic conditions that present joint instability while overlapping different chronic disorders. This makes diagnosing difficult, especially if the person is dealing with inflammation on one side of their body, but it affects another part. This is known as referred pain, and studies reveal that most inflammatory forms that affect the joints are sometimes arthritic and have systemic symptoms that may occur in different body areas. Some of the symptoms associated with chronic joint inflammation can include: - Swelling
- Stiffness
- Grinding sounds
- Difficult mobility
- Numbness
- Joint deformity
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The muscles, tissues, and ligaments help stabilize the joints and structure of the spine so that the body can function. These muscles are layered and interwoven in the spine and joints that help facilitate movement. When the body suffers from injuries or traumatic events, the muscles, tissues, and ligaments become affected, causing muscle pain and discomfort. This causes the muscles to be tender to the touch and sensitive. This is known as myofascial pain syndrome. Today’s article looks at myofascial pain syndrome, how it is linked with central sensitization, and ways to manage myofascial pain syndrome. We refer patients to certified providers specializing in musculoskeletal treatments to help many individuals with myofascial pain syndrome associated with central sensitization. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer What Is Myofascial Pain Syndrome? Have you been experiencing muscle tightness in different areas of your body? Have you felt your muscles tender to the touch? Or have you been having trouble sleeping? Many of these overlapping risk factors are signs that you might have myofascial pain syndrome. The term “myofascial” is split into two parts. “Myo” refers to the muscles, while “fascia” refers to the connective tissues found throughout the body. So myofascial pain syndrome is where there is muscle pain in various forms, which includes the muscle tissues, connective tissues, or both. Studies reveal that myofascial pain syndrome originates from trigger points in the skeletal muscle, causing the affected muscle to be in pain. The trigger points in the body’s skeletal muscles are the “knots” people feel when their muscles feel tight. These trigger points are challenging to identify because they occur in different areas causing referred pain (pain in one place but in another body area). How Central Sensitization Link To Myofascial Pain Syndrome? Studies reveal that central sensitization in the body is represented as an enhancement in neuron function and circuits in the nociceptive pathways that increases membrane excitability and synaptic efficacy. To that point, it reduces inhibition and manifests the remarkable plasticity of the somatosensory nervous system. The nociceptor inputs can trigger and manifest central sensitization as pain hypersensitivity when the body suffers from an injury. So how is central sensitization linked to myofascial pain syndrome? Let’s use fibromyalgia as an example. Many individuals dealing with myofascial pain may be potentially involved with fibromyalgia. This is due to fibromyalgia being a chronic condition that features widespread pain, and this causes the body to be more sensitive to pain. Central sensitization linked to myofascial pain syndrome can mimic fibromyalgia symptoms in the body, causing muscle pain and discomfort. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
|
Introduction When it comes to the human body in motion, the arms can carry, lift, and move items from one place to another without pain. The arms have different muscles that work together to protect the arm and shoulder joints while providing mobility and movement. One of the muscles that help the arms carry items is the brachialis muscles, which work together with the bicep and tricep muscles. As part of the forearm, it can succumb to various injuries affecting the muscle, tendons, and ligaments. When this happens, referred pain can affect the arm and develop trigger points to overlap chronic conditions that can potentially cause more pain. Today’s article looks at the brachialis muscle’s function, how trigger points affect the muscle, and various ways to manage brachialis trigger points. We refer patients to certified providers who specialize in arm pain treatments to aid individuals suffering from trigger points associated with the brachialis muscles along the upper arms. We also guide and inform our patients by referring them to our associated medical providers based on their examination when appropriate. We established that education is a great solution to asking our providers profound questions the patient requests. Dr. Jimenez DC takes note of this information as an educational service only. Disclaimer What Is The Brachialis Muscle Function? Have you been experiencing muscle strain in your forearms? What about stiffness in your wrist? Or do your arm muscles begin to spasm out of nowhere? Many people who have experienced these pain symptoms might be caused by trigger points associated with the brachialis muscle. The brachialis is an important muscle that flexes the forearm at the elbow. This muscle works with the biceps as it can carry heavy items, like the deltoid, and is the opposite of the tricep muscles. However, it can become overused and succumb to injuries that can invoke pain in the arm muscles, thus leading to the development of trigger points along the brachialis muscle. How Does Trigger Points Affect The Brachialis Muscle? When the brachialis muscle becomes injured, many people will experience pain when flexing their elbows inward or outward. According to Dr. Travell, M.D., these pain symptoms may be due to referred pain and tenderness from brachialis trigger points or radial nerve entrapment. During heaving lifting, the forearm flexion stress overload activates trigger points along the brachialis. Studies reveal that excessive sudden physical stress or repetitive activities may result from a muscle sprain or tear in the brachialis muscle. To that point, these symptoms associated with trigger points can cause overlapping risk profiles that can mask the condition. Some of the conditions that can overlap and activate trigger points include: - Carrying heavy groceries
- Holding power tools
- Tennis elbow
- Playing a string instrument
Studies also reveal that active trigger points along the affected muscle can increase weight coefficients and alter motor control without co-contraction patterns. This is due to trigger points becoming tricky to diagnose and mimic other conditions affecting the arms’ muscle group. Many people with pain-like symptoms associated with trigger points often complain about numbness or deep pain in their arms and hands. To that point, trigger points can also be involved with nerve entrapment in the brachialis muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The upper extremities of the body, which include the head, neck, shoulders, chest, and arms, all have a specific job of keeping the body functioning and helping move from place to place. The head and neck work together to allow the host to have the mobility to turn, rotate from side to side, and lean from one side. The shoulders work with the arms to let the muscles have a full range of motion and even help stabilize the upper body. The shoulders have various muscles, tendons, and ligaments to protect the skeletal joints and even work to do everyday activities like carrying or lifting items. When injuries begin to affect the muscle groups of the upper body, it can lead to pain-like symptoms that can lead to chronic conditions developing over time if not treated right away. One of the muscles in the upper body is called the coracobrachialis muscle, which can be affected by injuries. Today’s article observes the coracobrachialis muscle, how trigger points affect the upper arm muscles, and how to manage trigger points associated with the coracobrachialis muscle. We refer patients to certified providers who specialize in shoulder pain treatments to aid individuals suffering from trigger points associated with the coracobrachialis muscles along the upper arms. We also guide and inform our patients by referring them to our associated medical providers based on their examination when appropriate. We established that education is a great solution to asking our providers profound questions the patient requests. Dr. Jimenez DC takes note of this information as an educational service only. Disclaimer What Is The Coracobrachialis Muscle? Have you been dealing with pain from the upper arms to the hands? Do simple arm and shoulder stretches seem to be difficult to do? Or have you been dealing with symptoms of pain, stiffness, or tenderness in your upper arms? Experiencing these pain-like symptoms could overlap other conditions affecting the upper arms and develop trigger points along the muscles, including the coracobrachialis. The coracobrachialis is the smallest muscle located in the front of the upper arm’s anterior that originated in the shoulder coracoid process. This small muscle is connected to the tendon located at the short head of the bicep brachii, and according to Dr. Janet Travell, M.D., the coracobrachialis muscle function helps flex and adduct the arms at the shoulders while working together with the surrounding muscles of the upper arm and shoulders. This allows the arms to move forward slightly and inward. This means that the coracobrachialis muscle will enable individuals to place their arms behind their back without pain. However, like any muscle in the body, injuries can occur in the upper arms and lead to the development of trigger points along the upper arm muscles affecting the coracobrachialis muscle. How Trigger Points Affect The Upper Arm Muscles? When the upper arm and the coracobrachialis muscle suffer from pain, tiny nodules along the muscle fiber bands known as trigger points can cause referred pain to the upper arms. Now trigger points are tricky to diagnose due to mimicking overlapping conditions affecting the upper arms. Studies reveal that non-specific arm pain could potentially be one of the causes that trigger points mimic due to strenuous physical activities or work-related activities that can overuse the upper arm muscles. Studies reveal that individuals with idiopathic arm pain deal with high variable upper-extremity dysfunction, which could play a factor in pain-like symptoms along the surrounding muscles of the arms and shoulders. Many people often experience pain when reaching behind their back for the coracobrachialis affected by trigger points. Since the coracobrachialis works with the surrounding muscles in the shoulders and upper arms, trigger points associated with the coracobrachialis correspond to those muscles causing overlapping risk profiles. Trigger points affecting the coracobrachialis muscle can also mimic nerve entrapment since the coracobrachialis helps the bicep muscles when flexing. Pain associated with trigger points could potentially irritate the surrounding nerves in the muscle fibers, which causes radiating pain along the arms. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction Many individuals do not realize they are in pain until they begin to feel symptoms of stiffness or tenderness in certain areas of their body. Many people have two most common complaints: back and shoulder pain. The shoulder and the back have a casual relationship that stabilizes the upper body and protects the spine’s thoracic region. When injuries or ordinary factors affect not only the shoulders but the back, it can lead to symptoms of pain and stiffness along the muscles, causing the development of trigger points along the upper back and shoulder muscles. One of the muscles affected by trigger points is the rhomboid muscles located in the upper back behind the scapula (shoulder blades). Today’s article looks at the rhomboid muscle, how superficial backaches and round shoulders can affect the rhomboid muscle, and managing trigger points associated with the rhomboid muscle. We refer patients to certified providers specializing in back pain treatments to aid individuals suffering from trigger points associated with the upper back along the rhomboid muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure that education is a great solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Rhomboid Muscle? Do muscle stiffness in your shoulders seem to be causing you pain? Have you noticed that your shoulders seem more rounded than usual? What about the unexplainable upper backaches after being in a hunched position for a long period? Many individuals with these pain symptoms could be associated with the rhomboid muscles. The rhomboid muscles are a collective group of muscles important for upper limb movement and stability for the shoulder’s girdle and scapula. The rhomboid muscles consist of two separate muscles: the rhomboid minor and the rhomboid major, deep within the trapezius muscle and behind the scapula (shoulder blades). The functionality of the rhomboid is that they provide stability to the shoulder and when they are active, the upper arms move back and forth while walking. How Superficial Backaches & Round Shoulders Affect The Rhomboid While the rhomboid muscles provide stability to the shoulders, they can succumb to pain like any muscles in different body sections. Ordinary factors like a bad sitting posture can cause the upper back and shoulder muscles to contract and strain. Studies reveal that the effects of bad sitting posture can lead to the development of a forwarding head posture with rounded shoulders, causing pain in the rhomboid muscles. When the shoulder muscles, like the rhomboid muscles, experience this sort of change over time, it can increase muscle tone and continuous stress in the neck and shoulders. To that point, it can lead to various symptoms like pain, numbness, loss of functionality in the upper limbs, and nerve root symptoms. Other issues like back pain can also be one of the symptoms that can lead to referred pain in the rhomboid muscles and can potentially lead to the development of trigger points along the shoulders and rhomboid muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The rotator cuff works together with the shoulder, providing movement and a full range of motion. The shoulders are one of the largest and most complex joints that can succumb to injuries that can make the shoulders unstable and cause unwanted pain-like symptoms to affect not only the shoulders but also the arms and the neck. These pain-like symptoms are caused by myofascial pain syndrome or trigger points. Trigger points can create small knots along the muscle fibers in any muscle group and causes referred pain to different locations in the upper body. One of the muscles that can be affected by trigger points is the teres minor muscle. Today’s article examines this muscle, how trigger points affect the teres minor muscle, and managing trigger points associated with the teres minor muscle. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger points associated with shoulder joints and the teres minor muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Teres Minor Muscle? Have you been experiencing shoulder pain? Do you feel a tingling sensation that runs down to your fingertips? What about spasms or stiffness in your shoulders? Most of these symptoms are caused by trigger points associated with shoulder pain along the teres minor muscles. The teres minor muscles are part of the muscle group that supports the rotator cuffs. These muscles include the subscapularis, teres minor, supraspinatus, and infraspinatus and together assist in stabilizing the shoulder joint and even help perform arm movement. For the teres minor, this muscle is a narrow intrinsic shoulder muscle that extends from the lateral border of the scapula (shoulder blade). The teres minor is deep to the deltoid muscle as it has functions parallel to the other rotator cuff muscles, especially the infraspinatus. Studies reveal that even though the teres minor is often overlooked in normal shoulder function. To that point, the teres minor muscle becomes a key component for maintaining shoulder function when the other rotator cuff tendons fail from pathology that affects the shoulder and the rotator cuff joint. How Do Trigger Points Affect The Teres Minor Muscle? When pathology begins to affect the body, it affects the shoulders and the rotator cuffs. When pain affects the rotator cuffs, trigger points can develop and cause associated pain-like symptoms along the shoulders. Shoulder pain is the third common disorder in the musculoskeletal system. When the corresponding muscles in the shoulder are affected, trigger points can mimic other conditions that make it difficult to diagnose. According to Dr. Janet G. Travell, M.D., many patients often complain more of the pain rather than the restricted motion of their shoulders. This is due to the infraspinatus muscle being affected by active trigger points, causing referred shoulder pain. To that point, infraspinatus-referred pain dominates and releases tension to the parallel muscle fibers, the teres minor. Other issues like hypertrophy can also affect the teres minor when there are rotator cuff tears. Studies reveal that when the rotator cuff suffers damage and begins to tear, it could potentially lead to teres minor hypertrophy and cause referred pain-like symptoms along the upper arm. Fortunately, there are ways to manage trigger points associated with the teres minor to alleviate the pain. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The shoulder muscle functionality allows support and stability to the flexible joints in the body. The shoulders allow a full range of motion without feeling pain or discomfort, like throwing a ball or reaching an item on the shelf. The shoulders are also supported by many muscles, tendons, and ligaments surrounding the rotator cuffs that allow the shoulders to remain stable. The rotator cuffs consist of four muscle groups that allow the arms to be mobile. However, the range of motion from the shoulders and the rotator cuff can be prone to injuries and become unstable. To that point, the shoulders and their associated muscles are often the sites for many issues to develop. Today’s article looks at the supraspinatus muscles in the rotator cuffs, how trigger points affect the rotator cuffs and various therapies for rotator cuff injuries. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger points related to the shoulders affecting the rotator cuffs and the supraspinatus muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer The Supraspinatus Muscles In The Rotator Cuffs Do you feel stiffness along your shoulders? Does it hurt when you rotate them? Or have you been experiencing numbness and tenderness traveling your upper arm? Individuals experiencing these symptoms in their shoulders could be dealing with trigger points along the supraspinatus muscles. The supraspinatus muscle resides in the supraspinous fossa of the scapular spine and is superiorly located in the rotator cuff muscles. The supraspinatus muscle is associated with the other muscles that surround and support the rotator cuffs in the shoulder, which include: - Infraspinatus
- Teres Minor
- Subscapularis
These four muscles closely relate to the deltoid muscles to provide stability, movement, and rotation to the upper arm joint. When issues affect the shoulders or the rotator cuffs, it can cause the rotator cuff muscles to develop trigger points and other associated symptoms along the upper arm. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction Everyone in the world has various expressions that reflect how they are feeling. From being excited, worried, sad, angry, and disgusted, facial expressions defy people who they are, what they eat, and how they look. Each of the different muscles that make up the face has other jobs to work at the various locations of the upper extremities. The muscles on the forehead and near the eyes help people see while opening, closing, and raising their eyebrows. The muscles around the nose help take in air to breathe. The muscles located in the jaw help people chew food and speak. The neck muscles help support the head and provide mobility. All these muscles have specific jobs, and when issues affect the upper body extremities, they can potentially lead to different problems. When environmental factors like stress, anxiety, or depression begin to affect the body, it can also affect its facial features, causing unwanted symptoms to develop. Today’s article focuses on myofascial trigger pain on the face, the signs and symptoms associated with myofascial facial pain, and how to manage myofascial facial pain. We refer patients to certified providers who specialize in musculoskeletal and oral treatments to aid individuals suffering from myofascial trigger pain affecting their facial muscles. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer How Does Myofascial Trigger Pain Affect The Face? Have you been experiencing pain-like symptoms in your jaw? What about feeling constant pressure around your nose or cheeks? Do you feel tenderness in certain body areas around your face? Many of these symptoms you are experiencing could potentially involve myofascial trigger pain affecting the facial muscles. Having myofascial trigger pain in the upper extremities of the body can be challenging, as studies reveal that myofascial pain syndrome is a muscular pain disorder that is often misunderstood as it involves referred pain from small, tender trigger pain within the muscle fibers causing pain in different locations of the body than the actual source. Myofascial trigger pain often mimics other chronic conditions that cause doctors to be confused when patients mention that they have been experiencing symptoms and it’s affecting their daily lives. For myofascial trigger pain affecting the face, studies reveal that facial pain associated with myofascial trigger pain can be classified in various ways that affect the nasal, orbital, and oral cavities, the temporomandibular joint, and the sinuses from underlying pathologies. Myofascial pain correlating with the face can have many trigger points that can make a person feel miserable and affect their daily lives. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The jaw allows the host to chew, speak, and move while being stabilized by the surrounding muscles that help the jaw structure. The other surrounding muscles that support the jaw are the neck muscles when food is consumed and swallowed. The lower jaw has joints on each side that connect to the upper part of the skull, while the surrounding muscles provide the motor function to the jaw. To that point, normal wear and tear or various factors can not only affect the joints and the surrounding muscles, but they can cause overlapping pain profiles to the tendons, organs, and jaw muscles that may potentially affect a person’s quality of life. Today’s article examines the lateral pterygoid muscle, how TMJ dysfunction and trigger points affect this muscle, and ways to manage TMJ dysfunction and trigger points in the jaw. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger point pain associated with TMJ dysfunction affecting the lateral pterygoid muscle. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Lateral Pterygoid Muscle Have you heard popping sounds in your jaw when you open or close your mouth? Does your jaw feel stiff, and the pain travels down the neck? Does your jaw lock up, causing difficulty for you to open or close your mouth? Some of these symptom overlap with pain associated with the lateral pterygoid muscle. As part of the mastication muscles, the lateral pterygoid muscle is also a craniomandibular muscle that has a crucial role in the inferior temporal region. The lateral pterygoid muscle works together with the medial pterygoid muscle to provide functionality to the mandible or the lower jaw. The lateral pterygoid muscle also has nerves that branch off the trigeminal nerve and sends information to the brain. This information causes the muscles to move and function when food is consumed; however, when injuries or traumatic events affect the lateral pterygoid, it can disrupt the lower jaw structure and the surrounding muscles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction Headaches are one of the common issues that affect anyone worldwide. Different issues can cause headaches and affect other individuals depending on the issue. The pain can range from being dull to sharp and affect a person’s mood, sense of belonging, and body. Different headaches can have different effects on people since headaches can be acute or chronic and overlap with other issues affecting the body. To that point, the surrounding muscles and organs around the face may be involved with other conditions where headaches are a symptom rather than a cause. Today’s article examines the temporalis muscle, how trigger pain affects the temporalis muscle, and how to manage the pain associated with trigger points. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from trigger point pain associated with the temporal muscle pain along the side of the head. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Temporalis Muscle? Have you been dealing with a dull or sharp ache on the side of your head? What about the tension that is along your jawline? Or have you been dealing with tooth pain throughout the entire day? Encountering these symptoms can be difficult as they affect the facial region of the head and might overlap with the temporal muscle. The temporalis muscle is part of the mastication muscles, which includes the medial pterygoid, lateral pterygoid, and masseter muscles. The temporalis muscle is a flat, fan-shaped muscle that spans from the temporal fossa to the inferior temporal line of the skull. This muscle converges to form a tendon that surrounds the jaw bone and helps stabilize the jaw and its function by extending and retracting. Studies reveal that the temporalis muscle has two tendons: superficial and deep, in the back of the molars to aid chewing and are attached to the coronoid process (the skin and subcutaneous tissues that cover the superficial tendon of the temporalis muscle and the masseter muscle.) To that point, traumatic and ordinary factors can affect the temporalis muscle and cause symptoms associated with the muscle. How Do Trigger Points Affect The Temporalis Muscle? When traumatic or ordinary factors begin to affect the body, including the oral-facial region, it can cause unwanted symptoms to develop over time and, if not treated, make a person’s life miserable. Studies reveal that individuals dealing with chronic tension-type headaches have intense pain from the temporalis muscle. When the temporalis muscle becomes sensitive to the touch, the pain can travel to different body areas. These are known as myofascial or trigger points, and they can be a bit challenging for doctors to diagnose because they can mimic various pain symptoms. Trigger points along the temporalis muscles may potentially affect the teeth and cause headaches to form. Active trigger points in the temporalis muscle could potentially evoke local and referred pain while constituting one of the contributing sources of headache pain. Now how can the temporalis muscle induce chronic tension-type headaches? Well, trigger points are caused when the muscles are overused and can develop tiny knots along the muscle fibers. Trigger points along the temporalis muscle could potentially induce abnormal dental pain. Studies reveal that abnormal dental pain can be referred to as neurovascular headaches associated with tension on the temporalis muscle. Since trigger points often mimic other chronic conditions that confuse many people about why they are experiencing pain from one section of their body, there are no signs of traumatic encounters. Since trigger points can cause pain to travel from one area of the body to another, many individuals try to find therapeutic ways to alleviate their pain. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The neck is vital in keeping the head upright in a casual relationship with the cervical spine. The neck is home to the thyroid organ and the surrounding muscles that help support the neck to the rest of the body. One of the muscles that help support the neck is the sternocleidomastoid muscle. When traumatic forces begin to affect the neck, over time can lead to the development of chronic conditions associated with pain. When individuals start to feel pain affecting their neck, it can cause them to be miserable and find ways to relieve the pain they are experiencing. Today’s article focuses on the sternocleidomastoid muscle, how trigger pain affects this muscle, and ways to relieve SCM pain. We refer patients to certified providers who specialize in musculoskeletal treatments to aid individuals suffering from SCM associated with trigger pain along the neck. We also guide our patients by referring them to our associated medical providers based on their examination when appropriate. We ensure to find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC observes this information as an educational service only. Disclaimer What Is The Sternocleidomastoid Muscle? Have you been experiencing pain along the sides of your neck? What about limited mobility when you turn your neck from side to side? Or do headaches seem to worsen throughout the entire day? Some of these symptoms are associated with pain along the neck and could affect the surrounding muscles that are connected. One of the surrounding muscles that sit behind the thyroid is known as SCM or sternocleidomastoid muscle. The sternocleidomastoid muscle is a long muscle with dual innervation and multiple functions in the neck. The SCM is connected to the trapezius muscle that helps flex the neck, pulling the head forward while bringing the chin down to the chest. The SCM and the trapezius muscle work together to help stabilize and fix the head position while the host is talking or eating. When factors affect the neck over time, the SCM also gets involved. How Does Trigger Pain Affect The Sternocleidomastoid? When factors affect SCM associated with the neck, many issues will start to affect the neck and overlap pain near the eyes, ears, sides of the cheeks, and forehead. Studies reveal that SCM may develop myofascial trigger points in the head, causing referred pain. Trigger points are usually formed when traumatic forces affect certain areas in the body. For SCM to be affected by trigger pain, tiny knots along the taut band of the SCM muscle fibers become sensitive to pressure when compressed, and many people often describe the pain as deep and dull. To that point, the symptoms associated with SCM trigger pain may appear in numerous combinations or together depending on how severe the pain is on the person. Some of the symptoms related to SCM trigger pain include: - Headaches (sinus, cluster, or tension)
- Sore throat
- Ear pain (popping sounds in the ears)
- Blurred vision
- Vertigo
- Dizzyness
- Balance issues
- Muscle soreness
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The neck ensures that the head is upright in the body while providing mobility to rotate, bend, and tilt in various directions. The neck is part of the cervical spine and provides sensory-motor functions from the nerve pathways spread out along the shoulders and upper back. When traumatic events or injuries affect the cervical spine and cause pain to the neck over time, however, if not treated, it can lead to problematic symptoms associated with muscle pain. Neck pain can lead to muscle stiffness and cause myofascial trigger pain associated with referred pain along the rest of the upper body. Today’s article looks at the effects of neck pain, how it is associated with myofascial trigger pain, and ways to manage neck pain associated with myofascial trigger pain. We refer patients to certified providers specializing in musculoskeletal treatments to aid individuals suffering from neck pain associated with myofascial trigger pain. We also guide our patients by referring them to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Jimenez DC provides this information as an educational service only. Disclaimer The Effects Of Neck Pain Have you been feeling muscle stiffness around your neck and shoulders? Do you experience random headaches that affect your day? What about feeling tingling sensations along your arms and hands? These symptoms are associated with neck pain and can affect many individuals if not treated over time. Many people who suffer from neck pain will feel muscle stiffness that affects not only the sides of the neck but around the shoulders and their upper back. Studies reveal that neck pain is a multifactorial musculoskeletal disorder that affects the worldwide population and can become a chronic problem. Risk factors associated with the contributing development of neck pain include: - Stress
- Poor posture
- Anxiety
- Sleep position
- Neuromusculoskeletal disorders
- Auto accidents
- Traumatic events
Many of these risk factors associated with neck pain can cause pain symptoms and cause pain in different locations of the body, making diagnosing the pain source problematic for doctors. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The skeletal joints can keep the body upright and stabilized while protecting the internal organs. The skeletal joints also are at risk of factors (normal and traumatic) that can impact the body, thus potentially causing painful symptoms to affect different body areas. Hip pain is among the most common complaints for many individuals, especially the elderly. To that point, when the body suffers from hip pain, it may involve pelvic pain and associated symptoms that mimic other issues within the body. Today’s article examines the causes of hip and pelvic pain, the symptoms related to hip and pelvic pain, and how chiropractic care may relieve hip and pelvic pain. We refer patients to certified providers specializing in osteopathic treatments to help many individuals with hip and pelvic pain. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer The Causes Of Hip & Pelvic Pain Do you experience stiffness located on your low back or hips? What about sciatic nerve pain that travels down your legs? Or have you been experiencing cramping around the pelvic regions of your body? Experiencing these symptoms may be the potential cause that you might be dealing with hip and pelvic pain. Even though hip pain is often associated with older individuals, it can affect many individuals of different ages. Studies reveal that the pathologies outside the hips may be the cause and referred pain, making diagnosing hip pain difficult. Hip pain causes could be overused joints and soft tissues that support the hips due to repetitive motions, strain from the multiple muscles that support the hips, or arthritic symptoms. Studies reveal that individuals who work in a desk job will potentially develop low back pain due to prolonged sitting, thus becoming associated with excessive mobility of the lumbar spine and decreased hip joint mobility. Individuals with hip pain could risk developing pelvic pain associated with the overuse of joints and soft tissues. Now how pelvic pain correlates with hip pain, and what’s the causation? Studies reveal that the stabilizing muscles (iliopsoas, pectineus, obturator externus, gluteus minimus, and piriformis muscles) are overworked and become consequent hip and joint destabilization. This causes the affected muscles to become tired and weak and triggers sciatic nerve compression along the piriformis muscle. Pelvic pain associated with hip pain may cause dysfunctional musculoskeletal symptoms along the lower abdominals, hips, and lumbosacral back. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Introduction The body is exposed to various environmental factors daily. Whether it is the environment that a person is living, the foods being consumed, or the level of physical activities a person has plays a part in the body. Many individuals that want to live a healthier lifestyle will start small by incorporating nutritious foods they can add, sticking to an exercise regime they might enjoy, and finding time to meditate. Those who don’t want to change their lifestyle habits will continue eating foods that are high in fats, not exercising enough, or have problems sleeping. Over time, the body will be at risk of developing autoimmune disorders associated with musculoskeletal symptoms when exposed to environmental factors that impact a person’s lifestyle. Today’s article looks at an autoimmune disorder that causes inflammatory effects on the joints, known as polymyalgia rheumatica, the symptoms associated with this disorder, and how chiropractic care can help manage the symptoms of polymyalgia rheumatica. We refer patients to certified providers specializing in autoimmune treatments to help many individuals with autoimmune diseases associated with musculoskeletal disorders. We also guide our patients by referring to our associated medical providers based on their examination when it’s appropriate. We find that education is the solution to asking our providers insightful questions. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer What Is Polymyalgia Rheumatica? Have you been experiencing pain along your shoulders, neck, hips, or thighs? Does your body feel stiff in the morning and better throughout the day? Or have you been experiencing a limited range of motion in certain areas of your body? Many of these symptoms are signs that you might be at risk of developing polymyalgia rheumatica in your joints. Polymyalgia rheumatica is defined as a rheumatic disorder that is common in elderly adults over the age of 50. Polymyalgia rheumatica is an inflammatory musculoskeletal disorder that induces muscle pain and stiffness around the joints, especially in the morning. Studies reveal that polymyalgia rheumatica is often characterized by aching muscle pain in the shoulders, pelvis, and neck; it can mimic other rheumatic diseases like RA (rheumatoid arthritis), SLE (systemic lupus erythematosus), and polymyositis. When the body is dealing with the inflammatory effects of polymyalgia rheumatica, many people believe they are dealing with a different disorder affecting their bodies. To that point, diagnosing polymyalgia rheumatica is difficult. The Symptoms Associated With Polymyalgia Rheumatica Since polymyalgia rheumatica can mimic other rheumatic diseases, some of the symptoms associated with this inflammatory musculoskeletal disorder are similar to other chronic common diseases in the body. Studies reveal that the cause of polymyalgia is unknown, but environmental and genetic factors contribute to this inflammatory disease. Another disease that shares similar symptoms with polymyalgia is a disease known as giant cell arteritis. Giant cell arteritis causes inflammatory effects along the lining of the arteries, and individuals with this disease may have polymyalgia rheumatica. Some of the symptoms associated with polymyalgia rheumatica include: - Shoulder pain
- Pelvic pain
- Limited range of motion
- Muscle stiffness
- Joint pain
- Inflammation
- Neck pain
General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
|



 Your new post is loading...
Your new post is loading...











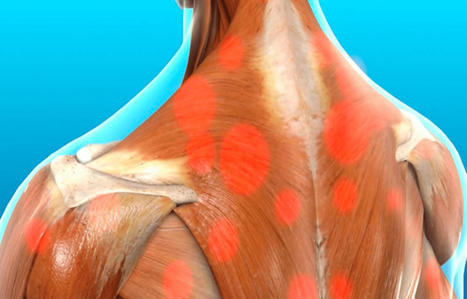




















Dr. Alex Jimenez gives an insightful overview of how the triceps muscles may be affected by trigger points other than pain. If you have any questions or concerns, please call Dr. Jimenez at 915-850-0900.