 Your new post is loading...
 Your new post is loading...
By integrating AI-based tools into discharge planning, hospitals can achieve a seamless care continuum—one where ever
A study from AHA finds that patients and healthcare workers report improvements in hospital safety, care quality, and resilience.
Interview published by agendaNi Harmonious data exchange across healthcare systems should unify “disparate data” from "diagnostic systems, public health records, laboratories, pharmacies, and hospitals", whilst being verified between each party. The healthcare sector is embracing digital systems and patient portals to make appointments, store data and inform patients about their medical journeys, but there is
What industry specific factors are fueling the growth of the case management market The use of rectification strategies by healthcare companies for diverse case management is gradually broadening the case management market s horizon The primary motivation behind employing thes
By adopting innovative approaches and prioritizing flexibility, organizations can create sustainable benefits strategies that support both their workforce and their long-term goals.
A shocking Royal College of Nursing report reveals the toll chronic underfunding has taken on staff, and rings alarm bells for the future
Erica S. Doubleday, MS, FNP-C, BSN, RN, illustrated the importance of consistent care to identify AEs like interstitial lung disease in patients with cancer.
A CNA unknowingly worked while infectious with mpox, exposing 56 residents. Yet, no secondary infections occurred, highlighting the power of standard precautions in healthcare settings.
High-quality data drives efficiency, can help improve costs and outcomes, and fosters innovation in the evolving healthcare landscape.
Roadmap Not all claims follow a straightforward path in workers' compensation. Some cases are inherently more complex, requiring additional attention, resources, and strategy to achieve successful outcomes. These high-risk claims—characterized by prolonged recovery times, potential litigation, or unusual circumstances—demand a proactive and vigilant approach from employers. This article examines the red flags that may indicate | WorkersCompensation.com
As we wrap up another year and get ready for 2025 to begin, it is once again time for everyone's favorite annual tradition of Health IT Predictions! We reached out to our incredible Healthcare IT Today Community to get their insights on what will happen in the coming year and boy did they deliver. We
As we wrap up another year and get ready for 2025 to begin, it is once again time for everyone's favorite annual tradition of Health IT Predictions! We reached out to our incredible Healthcare IT Today Community to get their insights on what will happen in the coming year and boy did they deliver. We
The murder of a health care insurance executive has brought scrutiny to the ways that insurance companies can make it difficult for insured patients to get the care they need.
|
Employers have a role to play in lowering the cost of healthcare and improving quality.
Increased access to behavioral health care was associated with significant cost reductions, suggesting a financially viable buyer strategy.
Industry analyst outlines how Medicare made a noteworthy inclusion in its 2025 rule.
Case Management Focus Ponder this statement: One in four nurses face workplace violence, a rate higher than police and correctional officers. As the result of two recent catastrophic events last week, where two nurses were critically injured – WE the nursing workforce must demand action to prevent this from happening. Just like other events like | WorkersCompensation.com
Please also review AIHCP's Case Management Education Program and Case Management Courses for healthcare professionals.
Healthcare is at a turning point, with persistent challenges threatening the system's sustainability. Workforce shortages – projected to exceed 100,000 healthcare workers by 2028 – and increasing clinician burnout highlight the urgent need for a more sustainable and effective approach to care delivery. Integrated care models are emerging as a vital solution, blending advanced technologies,
Democrats and Republicans both want to see federal lawmakers address critical public health concerns. However, they were split on which concerns were most important.
In this digital era, artificial intelligence (AI) is transforming healthcare, ushering in a new era of efficient and personalized case management. Narendra Maddukuri, a key contributor to this revolution, highlights how AI-driven innovations streamline processes, improve patient outcomes, and reshape traditional healthcare delivery approaches. Reimagining Healthcare with Predictive Analytics AI-driven case management relies heavily on […]
The Population Health Management Market Growth is Driven by Rapid Adoption of Value-Based Care Models and Technologica
CCM provides hospitals and health systems with a framework for promoting better chronic disease outcomes that fit into the context of patients' lives.
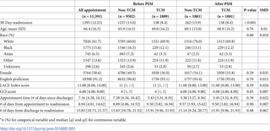
Transitional care management (TCM) visits have been shown to reduce 30-day readmissions, but it is unclear whether the decrease arises from the TCM visit itself or from clinic-level changes to meet the requirements of the TCM visits. We conducted a cross-sectional analysis using data from Northwell Health to examine the association between the type of post-discharge follow-up visits (TCM visits versus non-TCM visits based on billing) and 30-day readmission. Furthermore, we assessed whether being seen by a provider who frequently utilizes TCM visits or the TCM visit itself was associated with 30-day readmission. We included adult patients hospitalized to Medicine service and subsequent follow-up visits within two weeks of discharge between February 24, 2018, and February 24, 2020. We examined 1) post-discharge follow-up visit type (TCM visit versus non-TCM visit) and 2) provider characteristics (frequent TCM visit utilization or not). The primary outcome was unplanned hospital readmission within 30 days following hospital discharge. After propensity matching, TCM follow-up visits were associated with decreased 30-day readmissions (hazard ratio = 0.74 [0.63–0.88]) compared to non-TCM visits. Among patients with non-TCM follow-up visits, those seen by a provider who frequently used TCM visits had decreased odds (OR = 0.84 [0.71–0.99]) of 30-day readmission compared to those seen by providers who did not use TCM visits regularly. Among patients who followed up with providers who frequently use TCM visits, TCM visits were associated with decreased 30-day readmission compared to patients with non-TCM visits (OR = 0.78 [0.62–0.98]). The study has limitations, including the health system database not capturing all out-of-network follow-up visits. The reduction in 30-day readmission associated with TCM visits likely arises from both the visit itself and being seen by a provider who frequently uses TCM visits.
Hospitals across the country are employing virtual nurses to care for patients alongside bedside nurses—here's how one virtual nurse spends her shifts and why a virtual nurse expert is encouraging all nurses to help lead the future of the virtual nursing care model.
|




 Your new post is loading...
Your new post is loading...

























Care Coordination: How AI Is Transforming Hospital Discharge
Hospital discharging and AI
Please also review AIHCP's Case Management Program