Your new post is loading...
 Your new post is loading...

|
Scooped by
Jana Pearce
|

|
Scooped by
Jana Pearce
|
Deciphera Pharmaceuticals, Inc.(Nasdaq:DCPH), a clinical-stage biopharmaceutical company focused on addressing key mechanisms of tumor drug resistanc...

|
Scooped by
Jana Pearce
|
Safety and Efficacy of Subcutaneous Sarilumab in Improving the Quality of Life in People With Indolent Systemic Mastocytosis - Full Text View.

|
Scooped by
Jana Pearce
|

|
Scooped by
Jana Pearce
|
Types of Blood Cancers...

|
Scooped by
Jana Pearce
|
Targeting a diverse spectrum of cancers.

|
Scooped by
Jana Pearce
|
No matter what I'm feeling or experiencing, there's someone else out there going through the same thing. Probably multiple someones. So I'm going to try something I find really terrifying—being vulnerable on the internet.

|
Scooped by
Jana Pearce
|
New research by NIH investigators demonstrates for the first time that a bone marrow-derived cell, the mast cell, can cause disease in a solid organ through the transmission of small sacs of molecules through the bloodstream.

|
Scooped by
Jana Pearce
|
The NCCN has introduced the nation’s first-ever guidelines for systemic mastocytosis, a rare, complex and sometimes aggressive hematologic disease.

|
Scooped by
Jana Pearce
|
By Margaret Aranda, MD, Columnist I saw them do it to our veterans. Now they were going to do it to me. I heard the veterans scream decades ago, when I was president of a pre-med club at a VA hospital in Los Angeles. There was a little local anesthetic, no oxygen, no vital signs and no anesthesiologist. The hematologist-oncologist did the bone marrow extraction herself. Now I was about to have the same procedure myself, to get an early diagnosis of mastocytosis, an orphan disease. No one was going to tell me that I won’t hurt. The veterans fought in a war, yet they screamed. After taking my vital signs, the intake nurse interrogated me, eyes peering over her bifocals. “When was the last time you took OxyContin?” she asked. My thoughts: We never asked such a scrutinizing question. They could draw an opioid blood level, to “check” and see if I was telling the truth. Sure, my blood levels would be low, because it’s been a week. I’m not a drug addict. Big breath. Don’t let your thoughts get negative. Just get through this day. Postoperative pain was a big concern for me. “What will I get for post-op pain?” I asked the anesthesiologist. My thoughts: I don't want to cry. I don't want to hurt. I've had a lifetime of pain, and I live with it daily. Sores pervade me. They are all over my head, itchy ones that feel like cold sores mixed with chicken pox. If I scratch one, they all itch, including the sores on my arms and back. How much worse is my life about to get? "Tylenol. No post-op opioids for pain," was his reply. You bet my world crashed. "I can't do Tylenol. I need to save my liver. Everyone knows the smallest dose of Tylenol can hurt the liver. Besides, I don’t want to lose my empathy. Studies show acetaminophen causes a lack of empathy,” I said. “Ibuprofen,” was his answer. My thoughts: How much lower can my world crash? What the heck? Do you really know I’m a doctor, too? Do you know how many patients I’ve personally intubated through a GI bleed so they could breathe? “I can’t do ibuprofen,” I told him. “I can’t have a GI bleed. Or a heart attack. Or a stroke.” “Oh, okay! Morphine and fentanyl, a mixture. Morphine lasts longer," the anesthesiologist said. My thoughts: I can breathe again. Now I have to be the perfect patient. The pathologist was cheery, polite and smiled a lot. We went over the pathology of mastocytosis, WHO classifications, the systemic vs. cutaneous forms, early diagnosis, and the bone marrow procedure I was about to have. He asked if I had enough opioids for post-op pain. I did. I concluded that he does not write his own pain prescriptions. Once on the operating table, the surgeon caressed my head, patting it before I fell asleep. I inwardly smiled as I laid straight on my right side. Cold prep solution dripped down my lower back as I sunk into sleep. The surgeon bore into the ileum, then sucked out the bone marrow with a syringe. When I woke up, my butt was numb and I did not need any more pain medication. But I was not given a prescription for postoperative pain for when I went home. I was told to use my existing opioid prescription for pain, which is reasonable, as long as my doctor doesn't "count" them against me. My thoughts: How do patients defend themselves to get opioids for during and after surgery? I mean, I’m a doctor and I had to stick up for myself. What if the patient does not even know to ask about postoperative pain at all? They must wake up screaming, an insult to any anesthesiologist. What has happened to patient care? They profession of anesthesiology has changed. Dr. Margaret Aranda is a Stanford and Keck USC alumni in anesthesiology and critical care. She has dysautonomia and postural orthostatic tachycardia syndrome (POTS) after a car accident left her with traumatic brain injuries that changed her path in life to patient advocacy. Margaret is a board member of the Invisible Disabilities Association. She has authored six books, the most recent is The Rebel Patient: Fight for Your Diagnosis. You can follow Margaret’s expert social media advice on Twitter, Google +, Blogspot, Wordpress. and LinkedIn. The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.

|
Scooped by
Jana Pearce
|
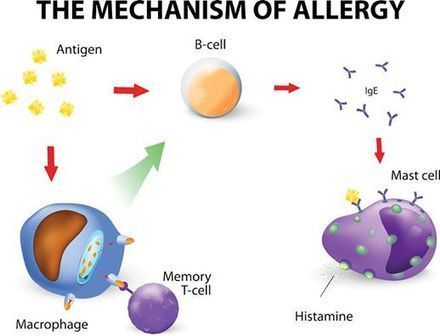
There are many products on the market that promise to relieve, control, manage or attack allergies. These products work by interfering with biochemical responses that happen in the body. One example is antihistamines. These medications may relieve symptoms by stopping histamine from being released by certain cells in the body. Though antihistamines are the most common drugs used to treat allergic symptoms, they are not short of side effects. A major side effect is sleepiness. Driving a car or working equipment is not suggested while under the influence of antihistamines. Further common side effects are dryness of the mouth, nose and throat, blurry vision, faintness, loss of appetite, biliousness, upset stomach, low blood pressure, headache, anxiety, agitation, sleeplessness and loss of coordination. With all those side effects, you may be looking for other options? FREE Download: Get your FREE 7 Day Gut Healing Meal Plan including recipes to make every meal. Click here now and receive instant access! Continue reading to discover my top natural antihistamine foods with benefits... Quick Navigation As a naturopath with 15 years of experience, I have a special interest in the treatment of allergic conditions. I love using natural remedies and food. Histamine is a biochemical that the body makes on its own. We can also eat diets that are rich in histamine. Histamine plays a key role in allergy related inflammation in the body. It also regulates sleep and stomach acid. Your body might experience histamine intolerance to food when it is no longer able to break it down. Histamine intolerance is a food intolerance. So, it should come as no surprise that the gut microbiome has a large part to play in its pathogenesis. Upon histamine digestion, enzymes work to metabolise histamine. This decreases the quantity absorbed into the blood stream. The inflammation, as a result of a disturbed gut microbiome, might be an underlying powerful influence behind histamine intolerance. Here are some of the top antihistamine foods that you can incorporate in your diet: 1. Apples Apples contain quercetin. Quercetin can help steady the release of histamines from certain immune cells. Quercetin reduces symptoms like coughs, watery eyes, runny noses, rash, puffy lips or tongue, and dyspepsia. Like many other bioflavonoids, quercetin has anti-oxidant, anti-atherogenic, and anti-carcinogenic properties. You know the old saying – an apple a day keeps the doctor away! Apples are also one of my top foods to buy organic. If you haven't switched to organic apples I recommend it, they are super crisp and tasty! 2. Thyme Thyme essential oil has antimicrobial activity against a multitude of diverse microorganisms and yeasts. It is a natural antihistamine. Thyme essential oil has sterile properties to help fight infections. It is an herbal antibiotic particularly armed to challenge lung infections. Thyme is sterile, antiviral, antihistamine, anti-inflammatory, antispasmodic, nervine, and antitussive. Unlike antibiotics, thyme works on microbial or virus-related contagions (not just bacteria). It has a soothing effect on the nervous system, and might help you get some much-needed time out. Including fresh thyme in your meals is helpful, but for a more therapeutic dose, thyme essential oil can be found in a number of antimicrobial supplements. 3. Watercress Investigation tells us that compounds removed from this hot herbal can stop histamine release from cells exposed to an allergen. Watercress helps to reduce high blood pressure. Watercress compounds lower cancer risk and can protect from the side-effects of radioactivity and chemotherapy. Watercress is one of the most nutrient-rich foods. It has the capability to constrain 60% of the histamine released from mast cells. I use watercress all the time as a garnish for salads to make them extra tasty. The spicy and nourishing greeneries of watercress have been used to treat bronchitis and adenoidal illnesses in children. 4. Onion Consistent onion eating can steady mast cells . Onions also lower down the histamine levels in blood plasma cells. What makes the health benefits of onions so abundant is the presence of the polyphenol quercetin compound. Polyphenols are phytochemicals, antioxidants that defend vegetations against microorganisms and worms. Quercetin halts your immune system from releasing histamines, easing allergen symptoms such as runny nose and watery eyes. The health benefits of onions aren’t only due to quercetin. Onions are salt and fat free, low in calories and plentiful in vitamins C, B6, A and E. The copper found in onions protects your bones and joints, firms your skin and stops osteoporosis in women. Your intestines will also thank you, since onions boost the development of good gut bacteria that helps in digestion. 5. Parsley Testing displays Parsley’s antihistamine action which indicates it to be helpful for individuals with hay fever or rash. It’s anti-inflammatory and can patch-up liver damage. As it turns out, further investigation proposes that parsley, that once-ignored garnish, is a star when it comes to 'food as medicine'. This herb is a key source of vitamin A, vitamin C, and lutein and zeaxanthin, recognised as the macular carotenoids for their key role in protecting eye strength. Shopping for parsley is like purchasing a bunch of fresh-cut rosettes: Freshness is important. The greeneries must be bright green, the stalks stable, nothing floppy. At home, take them out of the plastic so they can breathe a little. Once you are ready to enjoy, first give them a decent rinse in warm water. 6. Broccoli A reliable source of vitamin C, broccoli is an easy-to-find antihistamine and is a faultless answer for treating a stuffy nose and other symptoms of allergies brought on by irritation. It is a true superfood and is a particularly rich source of the flavonoid kaempferol, which is why it is such a strong anti-inflammatory. Investigation has exposed that eating a lot of cruciferous vegetables is linked with a reduced risk of heart disease and cancer. This might be connected to the anti-inflammatory effects of the antioxidants they contain. Broccoli is rich in sulforaphane, an antioxidant that fights inflammation by dropping your levels of cytokines and NF-kB, which drive swelling. Broccoli is one of the finest sources of sulforaphane, an antioxidant with anti-inflammatory, anitcancer, antimicrobial, anti-diabetic properties and helps promote liver detoxification. 7. Peach Peaches are a seasonal fruit, that are sugary and juicy. A study found that they repressed mast cell derivative allergic irritation. Ending the histamine response in cells is the first line of defense in ending irritation in the body. Besides being full of fibre and water, peaches are also very high in beta carotene. One of the utmost qualities in peach nutrition is the high number of antioxidants found in these delightful fruits. When free radicals can bounce around in your many body systems, they can cause all kinds of injury, known as oxidative stress, and contribute to illness and cell breakdown on many levels. 8. Black Rice Bran Black rice is supposed to have many distinguished health benefits. Academics have found that a 10% diet of black rice reduced irritation and repressed the release of histamine from mast-cells by around 32%. Brown rice did not have the same benefits. Anthocyanins found in black rice bran stop circulatory illness, melanoma and are anti-inflammatory and can help purify the liver of noxious build up. Bran is the outside shell of the grain, which is detached throughout the processing of brown rice to yield the familiar white rice. A 2010 study established the possible worth of black rice bran as an anti-inflammatory and anti allergic food element and as a healing agent for the handling and deterrence of illnesses linked with chronic inflammation. 9. Mung Bean Sprout Mung bean sprouts are concentrated with flavonoids, the phytonutrients in flowers. Mung beans constrain the release of the activating histamine enzyme in mast cells and help stop histamines from being released. Mung beans can control cholesterol levels since their antioxidants act like strong free-radical foragers, withdrawing injury done to blood vessels and dropping irritation. Oxidized LDL cholesterol is one of the main dangers of lethal cardiac events, such as heart attacks or stroke. LDL cholesterol can add inside the internal lining of blood vessels, named the endothelium, and block blood flow, causing cardiac arrest. Mung beans are a terrific addition to any anti-inflammatory diet thanks to their capacity to keep veins strong and to recover flow. 10. Turmeric Turmeric is the spice that gives curry its shade, and on its own it has a pungent, cheddar like sense of taste. The fresh rhizomes are obtainable and can be frozen and grated over most salty dishes as a condiment. Turmeric has influential anti-inflammatory and anti-oxidant properties. A study found that it repressed mast cell activation. It also acts as an anti-inflammatory, calming the reddened air route of the oesophagus following an allergic response. Turmeric contains a compound known as curcumin. This acts as a decongestant and this action in turn aids in reducing the many symptoms that come with allergies. This spice acts as a natural antihistamine. This means that it can decrease the release of histamines in your body, or stop mass cell degranulation. It is also a powerful detoxifier. 11. Fennel Fennel is anti-inflammatory, antihistamine, painkilling and antioxidant. Fennel is a natural relief for skin care. Fennel seeds, stems, bulbs, and greeneries are all crammed with nutrition and are an outstanding source of B vitamins. These vitamins, with vitamin C, are vital for upholding good skin health and even promote collagen synthesis to keep the skin strong and body-hugging. Fennel extracts are valued as an anti-aging element in many supplementary skin care goods. Fennel contains many nutrients that play a dynamic part in shielding you from melanoma. The herb contains an anti-inflammatory phytonutrient called anethole, which occurs in fennel, recognised to have anti-cancer effects by stopping breast cancer cells from growing. Colicky babies cry hard at around the same time each day for at least three days a week. Breastfeeding mothers can sip on fennel tea to help releive their baby's discomfort. This will cool the digestive tract and help release gas and indications of indigestion. Fennel seed oil can decrease duodenal contractions and upsurge motility of the small intestine. It eases stomach discomfort and uneasiness linked with dyspepsia, stomach swelling, biliousness, burping, and flatulence. Fennel and celery with a sprinkle of slithered almonds makes a delicious and refreshing salad. 12. Pomegranate Pomegranates have a sugary but acerbic sense of taste and are used in both salty and sugary foods. They contain polyphenols, such as tannins and anthocyanins, and are higher in antioxidants than green tea. A study displayed that they act as mast cell stabilisers. Pomegranates are of great therapeutic use for the body. Pomegranate is delicious in its natural form, juice or herbal tea. In vivo studies done on the whole fruit or extract, skin, and florae reveal antiulcer effect in a diversity of animal models. Ellagic acid was the chief accountable for this effect, though other separate ellagitannins might contribute to the biotic activity of the mixture. Diverse preparations of pomegranate, including cuttings from skins, florae, kernels, and juice, display a noteworthy anti-inflammatory activity in the gut. 13. Ginger Ginger is a rhizome that constrains allergic responses. It has been used as an H2 inhibitor, but then again, a 2009 study displays that it also acts as a mast cell stabiliser. Investigation has exposed that ginger has many health benefits including antioxidant, anti-viral, anti-inflammation, and anti-tumor effects. So, it can help treat many commonplace problems such as peptic illnesses, biliousness, motion sickness, abdominal spasms, temperatures, and chills as well as major diseases such as high blood pressure, high cholesterol, and even malignant tumors. Ginger acts as an anti-histamine and can help in the handling of allergies. Ginger is a natural anti-viral and anti-histamine. It can help promote healthy perspiring, which is often accommodating when suffering from a cold or temperature. 14. Holy Basil Holy basil’s activity as an anti-histamine has been found to affect histamine’s H2 receptor, great news for those with histamine intolerance/histaminosis/mastocytosis/mast cell activation disorders with stomach grievances. Holy Basil is also known as Tulsi, one of my favourite herbal supplements and teas. Its anti-inflammatory effects are in part owing to it’s high vitamin K content. Holy basil is a herb in the basil family. It has a delicate taste that is minty, and flowery, with a natural sugariness. It is an adaptogen to help reduce feelings of stress, as well as anti-anaphylactic, antihistamine, and mast cell stabilising properties. 15. Sweet Potato This delicious, nourishing food is one of the highest antihistamine type foods. The root vegetable contains a diverse range of vitamins, minerals, phytonutrients, and antioxidants that stop the histamine response in cells. A key source of complex carbs, fibre, beta-carotene, manganese and vitamin B6 and C, these potatoes help rectify inflammation in the body. Beta carotene is the nutrient accountable for giving sweet potatoes that typical attractive carroty hue. It’s also helpful in exfoliating your skin. Cyanidin is one more antioxidant extra of sweet potatoes. Found in the flesh of purple sweet potatoes, this phytonutrient compound has been related to shielding us from pollutants in the digestive system. It helps the body decrease inflammation that contributes to long term chronic disease including diabetes, arthritis and asthma. 16. Amaranth Amaranth greeneries are delicious. The greeneries are crammed with anti inflammatory vitamin K and they have such robust antihistamine action that they’ve been exposed to stop anaphylactic shock. The kernels are not grains, like wheat or rice. It contains a higher protein concentration than any other grain on the market. Furthermore, even the greeneries of the amaranth contain helpful proteins. The proteins are particularly of high nutritional value owing to the outstanding balance of vital amino acids. Still, further investigation proposes that extra nutrients such as phytochemicals of amaranth might also have possible health beneficial effects. The emollients and phytosterols in amaranth help lower cholesterol levels, including LDL and triglycerides. The anti-inflammatory properties of peptides and emollients in amaranth can ease pain and decrease irritation. This is particularly significant for chronic conditions where inflammation corrodes your health, such as diabetes, heart disease, and stroke. Did you enjoy finding out which of your favourite antihistamine foods are also helping your allergies? As a Naturopath, I focus on two features: prevention and addressing the root cause of disease. I practise a holistic, evidence-based approach to care. I use the best of natural and conservative treatment – which includes diet! Over to you... Do you think you can integrate some of these antihistamine foods into your diet? Challenge yourself to make the step. If you would like help, I’m here to support you. I can help you integrate these antihistamine foods into your diet. Don’t be a stranger - let me know how you add these natural antihistamine foods into your diet in the comments. If you liked this article and think it could benefit your friends, please share it � How is Your Gut Health? Click the button below to take our short quiz and discover your results: Yes, take the quiz now!

|
Scooped by
Jana Pearce
|
![Figure][1]</img>
An 83-year-old man presented with hematuria and bone pain. Computed tomography–scan imaging demonstrated multiple osteolytic lesions and vertebral collapse.A complete blood count showed anemia with hemoglobin of 9.1 g/dL and normal white blood count and platelets, 4.95 × 109/...

|
Scooped by
Jana Pearce
|
ALL PATIENTS: Self-Injectable Epinephrine (two doses; e.g., EpiPen®/EpiPen Jr®) should be carried by all patients with a mast cell disorder at all times, even if previous anaphylaxis has not occurred.
|

|
Scooped by
Jana Pearce
|
https://pubmed.ncbi.nlm.nih.gov/32981062/ Australas J Dermatol. 2020 Sep 27. doi: 10.1111/ajd.13469. Online ahead of print. Álvaro Iglesias-Puzas, Alberto Conde-Taboada, Beatriz Aranegui-Arteaga, Eduardo López-Bran (Dermatology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain;...

|
Scooped by
Jana Pearce
|
![Figure][1]</img> [1]: pending:yes...

|
Scooped by
Jana Pearce
|
https://www.ncbi.nlm.nih.gov/pubmed/30545997 J Natl Compr Canc Netw. 2018 Dec;16(12):1500-1537. doi: 10.6004/jnccn.2018.0088.Gotlib J, Gerds AT, Bose P, Castells MC, Deininger MW, Gojo I, Gundabolu K, Hobbs G, Jamieson C, McMahon B, Mohan SR, Oehler V, Oh S, Padron E, Pancari P, Papadantonakis N,...

|
Scooped by
Jana Pearce
|

|
Scooped by
Jana Pearce
|
Systemic Mastocytosis Stem Cells Therapy in Ukraine...

|
Scooped by
Jana Pearce
|
Tryptase is an enzyme that is released, along with histamine and other chemicals, from mast cells when they are activated as part of a normal immune...

|
Scooped by
Jana Pearce
|
The majority of patients with advanced systemic mastocytosis (AdvSM) exhibit D816V mutations of the KIT gene, which presents a promising therapeutic target. Here, Daniel DeAngelo, MD, PhD, of Dana-Farber Cancer Institute, Boston, MA, discusses the clinical trial of avapritinib (previously BLU-285;...

|
Scooped by
Jana Pearce
|
![Figure][1]</img>
A 62-year-old woman was investigated for myeloproliferative neoplasm with splenomegaly.Complete blood count showed the following: hemoglobin, 123 g/L; leukocytes, 30.7 × 109/L; platelets, 273 × 109/L; myelocytes, 1.14 × 109/L; neutrophils, 23.72 × 109/L; eosinophils, 0.43...

|
Scooped by
Jana Pearce
|

|
Scooped by
Jana Pearce
|
Summary Adverse drug reactions are a cause of significant morbidity and mortality to patients and a source of financial burden to the healthcare system. Of the wide spectrum of adverse drug reactions, the most concerning to the anaesthetist remain anaphylaxis and malignant hyperthermia. Although the incidence of anaphylaxis under anaesthesia is difficult to ascertain, it occurs commonly enough that most anaesthetists will manage at least one case in their career. The wide range of drugs given in the peri-operative period and the variable presentation in the anaesthetised patient can delay diagnosis and treatment, and adversely affect outcome. Furthermore, despite improvements in testing, causative drugs can still be difficult to identify, as adverse reactions may be mediated by mechanisms other than IgE activation. With an increase in the reporting of anaphylaxis to newer anaesthetic drugs such as sugammadex, combined with change over the recent decades in the most likely causative peri-operative agents, it is imperative anaesthetists remain up to date on recent developments. In addition, they should be vigilant to patient characteristics, including pharmacogenetic variations that may predispose to adverse drug reactions, in order to help minimise risks of a reaction. The severity of adverse drug reactions to peri-operative drugs means morbidity and mortality remain high. Anaesthetists are the medical specialists most likely to witness adverse drug reactions. This is due, in part, to the nature of the peri-operative period, in which patients are exposed to a large variety of potential allergens. These include anaesthetic drugs, antiseptics, dyes, contrast, latex and antibiotics. Adverse drug reactions (ADR) are a source of significant morbidity and mortality, responsible for up to 6% of hospital admissions, carrying a mortality of 2% and costing the NHS £466 million per annum (€654 million, US$ 602 million) [1]. They not only impact on the patient's quality of life, confidence in the healthcare system and length of hospital stay, but failure to identify ADRs can lead to unnecessary investigations, potentially be detrimental to the patient and adding to the financial burden. The incidence of adverse drug reactions to anaesthetic drugs is often quoted as between 1 in 10,000 and 1 in 20,000 [2]. However, it is likely these numbers are a gross underestimate. Differences in methodology between studies make it difficult to predict the true figure, but it may be somewhere nearer 1 in 3000 [3]. Despite comprehensive guidelines on recognition and management of adverse drug reactions, mortality from ADRs associated with anaesthesia is in the order of 10% [4]. Peri-operative anaphylaxis was the subject of the Royal College of Anaesthetists’ 6th National Audit project, which aimed to establish the true incidence of anaphylaxis in the UK, its epidemiology, short- and long-term outcomes, management, referrals, investigation and follow-up [5]. It is hoped that dissemination of these results will impact diagnosis and management of anaphylaxis in the same manner as previous audits have on awareness under anaesthesia and airway complications [6, 7]. It is a patient safety imperative that, as peri-operative specialists, we remain vigilant to the possibility of ADRs and be familiar with their recognition, immediate treatment and follow-up. Definitions and classifications Adverse drug reaction The most commonly used definition of an ADR is a response to a drug that is ‘noxious, unintended and occurs at doses normally used in man’. This definition arose from the World Health Organization (WHO) report on International Drug Monitoring in 1972, and remains largely unchanged [8]. In contrast, the classification systems used and the nomenclature for allergy and anaphylaxis have changed considerably. There are now two commonly used systems for classifying adverse drug reactions. The original classifications known as type A or augmented (dose-dependent and predictable) and type B or bizarre (dose-independent and unpredictable) are the best known and are often applied to reactions occurring in anaesthesia or intensive care. Types C–F have since been added (Table 1) [9]. In 2003, Aronson and Ferner observed that some adverse drug reactions do not always fit well into just one of these classes and proposed a system based on dose-relatedness, time-relatedness and susceptibility of the patient (DoTS) (Fig. 1) [10]. However, many of the drug reactions seen in anaesthetics and critical care still fit comfortably in the original type A and type B classification, and it remains simple to use and is familiar to clinicians. As such, it is still used by the Medicines and Healthcare products Regulatory Agency (MHRA) in its ADR collection process. Table 1. Classification of adverse drug reactions. Adapted with permission [10] Types of reaction Features Example A – Augmented Dose-related Common Related to known pharmacological effect Predictable Hypotension with propofol B – Bizarre Non-dose-related Unpredictable Uncommon Not related to known pharmacological action of drug Anaphylaxis Malignant hyperthermia Suxamethonium apnoea C – Chronic Dose-related Time-related Uncommon Related to cumulative dose Propofol infusion syndrome D – Delayed Time-related Often dose-related Uncommon Fluoride nephrotoxicity E – End of use Uncommon Occurs after withdrawal of drug Rebound hypertension following cessation of clonidine infusion F – Failure Dose-related Uncommon May be caused by drug interactions Failure of oral contraceptive pill with sugammadex use Anaphylaxis In 2001, the European Academy of Allergy and Immunology (EAACI) redefined their nomenclature for allergy, including anaphylaxis. They defined anaphylaxis as a ‘severe, life-threatening generalised or systemic hypersensitivity reaction’. It can be subdivided into allergic or non-allergic anaphylaxis, with allergic anaphylaxis further subdivided into IgE-mediated and non-IgE-mediated. The term anaphylactoid is now obsolete, and all non-immune-mediated reactions should be referred to as non-allergic anaphylaxis [11]. This new nomenclature highlights difficulties in identifying potential anaphylaxis triggers, as skin prick testing will only identify IgE-mediated reactions, and attributing causality may require additional investigations such as intradermal testing, which carries the risk of precipitating further anaphylaxis [12]. In addition to drugs which cause ADRs by IgE or non-IgE-mediated mechanisms, there are others, such as non-steroidal anti-inflammatory drugs (NSAID) and neuromuscular blocking (NMB) agents, that can cause a reaction by both mechanisms, further complicating diagnosis (Table 2) [13]. Table 2. Mechanism causing hypersensitivity reactions for drugs commonly used in the peri-operative period IgE-mediated allergy Non-allergic drug hypersensitivity NSAID, non-steroidal anti-inflammatory drug; NMB, neuromuscular blocking agent. NSAID NSAID Antibiotics Opioids Latex Hypnotics NMB NMB Heparin Contrast media Contrast media Dyes, e.g. patent blue Disinfectants Hypnotics Factors contributing to adverse drug reactions Patient characteristics Age The physiological differences in children and the elderly make them more susceptible to ADRs. Differences in renal, hepatic and cardiovascular systems all increase the chance of an ADR [14]. Polypharmacy This increases the chance of an ADR secondary to drug interactions. Polypharmacy can also alter pharmacokinetics, and the underlying disease may affect pharmacodynamics [15, 16]. Sex Some drugs cause anaphylaxis more commonly in females; these include NMBs and latex. Females are almost twice as likely to experience an ADR. This may be attributable to pharmacokinetic differences related to body mass, hepatic clearance and hormones [17]. Smoking Anaphylaxis to antibiotics occurs more frequently in smokers and could result from sensitisation due to repeated courses for respiratory infections [18]. Atopy Latex allergy and anaphylaxis to contrast media are more common in patients with a history of atopy. They are also more common in patients with an allergy to fruits, especially banana, chestnut and avocado [19]. Previous exposure Healthcare professionals and patients undergoing multiple procedures, such as those with spina bifida, are at increased risk of latex allergy. This also applies to workers who have an occupational exposure to latex [18, 19]. However, unlike those high-risk patients where environmental sensitisation from a young age is the primary mechanism, there may be a genetic component predisposing healthcare workers in addition to prior exposure [20]. Possible environmental sensitising agents There is considerable variation between countries in the incidence of anaphylaxis, particularly to NMBs. Although variations in reporting rates may account for some of this difference, it may be that environmental factors are involved. For example, many common chemicals found in domestic products contain allergenic epitopes similar to the quaternary ammonium ions thought to be responsible for adverse reactions to the NMBs [21]. The most well-known is the IgE sensitisation of patients to NMBs, particularly suxamethonium, from the use of pholcodine, a historical component of a popular cough medicine in Europe. The discrepancy between rates of anaphylaxis to NMBs between Scandinavian countries prompted a search for an environmental factor. The rate of reported anaphylaxis to NMBs dramatically reduced in Sweden since the withdrawal of pholcodine in the 1980s, and a recent review in Norway shows similar results since its withdrawal in 2007 [22]. A similar theory is postulated for the increasing amount of anaphylaxis seen to sugammadex, based on our ingestion of up to 4 g of cyclodextrins a day [23]. Pharmacogenetics Differences in pharmacogenetic diversity can help explain the differences seen in both pharmacokinetics and efficacy of many drugs used in the peri-operative period, including the varied responses to commonly used anaesthetic drugs such as propofol, fentanyl and ondansetron [24-26]. Genetic predispositions of particular relevance in anaesthesia include: suxamethonium apnoea; malignant hyperthermia; acute porphyria; and ADRs secondary to variations of the cytochrome P450 system (Table 3) [27]. With the cost of gene sequencing likely to fall, the pre-emptive identification of those of risk of ADRs secondary to pharmacogenetics may become an option. However, although this would allow for individually tailored peri-operative care, it raises practical, ethical and financial considerations. Table 3. Genetic variations with relevance to anaesthesia Genetic variation Effect Related drugs Plasma pseudocholinesterase Deficient enzyme activity, prolonged drug effect (suxamethonium apnoea) Suxamethonium, mivacurium Defective coding for ryanodine receptor Malignant hyperthermia Inhalational anaesthetics Suxamethonium CYP2D6 gene Poor, intermediate, extensive or ultrarapid metabolisers Diazepam Codeine Tramadol Ondansetron β-blockers Porphobilinogen deaminase deficiency Acute intermittent porphyria Barbiturates Clonidine Cephalosporins Benzodiazepines Phenytoin Immune response An immunological response, usually involving in the formation of antibodies, can lead to hypersensitivity reactions. These can be classified into four main types (Table 4). Table 4. Types of hypersensitivity reactions Mechanism Example Type I Immediate Anaphylaxis, angio-oedema Type II Cytotoxic Transfusion reaction Type III Immune complex-mediated Reactive arthritis Type IV Delayed, cell-mediated Contact dermatitis The ADRs of greatest significance to the anaesthetist in the peri-operative period are undoubtedly anaphylaxis and malignant hyperthermia. Much of the remainder of this article focusses on the recognition, management and investigation of these reactions. Management of other ADRs largely relies on avoidance of known precipitants and knowledge of any genetic predisposition likely to cause problems. Recognition of hypersensitivity reactions The first step to managing an adverse drug reaction is identifying it. This may not be straightforward in an anaesthetic setting. Simultaneous exposures to multiple potential allergens and the physiological effects of anaesthesia can muddy the waters. For example, although bronchospasm may be due to an ADR, it could simply be the response to irritation by a tracheal tube. As well as intravenous (i.v.) triggers, there are ‘hidden’ drugs such as latex and chlorhexidine to consider, so identification of the precipitant may not be possible at the time of reaction [2]. Peri-operative reactions can be severe or life-threatening, with the potential for a more severe reaction on repeated exposure to the allergen, making identification of the responsible agent extremely important for future avoidance. Clinical presentation can vary from skin and temperature changes to life-threatening cardiovascular collapse. Physiological changes related to anaesthesia or critical illness can delay recognition. The following is a brief guide, highlighting the wide variation in presentation that makes prompt recognition challenging. The commonest presentations of anaphylaxis under anaesthesia can be found in Table 5 [17, 28]. Table 5. Presentations of anaphylaxis under anaesthesia Cardiovascular 75–88% Hypotension 18% Cardiovascular collapse 50% Cardiac arrest 6% Bradycardia 2% Bronchospasm 36–40% Cutaneous signs 45–90% Angio-oedema 7–25% Skin changes These may be absent, hidden under drapes or coloured antiseptic or only appear in cases of profound circulatory collapse once perfusion has improved [2]. If the patient is on high-dose corticosteroids or antihistamines, skin changes may be masked. Patients with urticaria should be referred for investigation, but localised and transient rashes caused by local histamine release are unlikely to represent significant hypersensitivity. In particular, transient flushes or rashes secondary to known histamine-releasing drugs, such as NMBs and opioids, usually resolve spontaneously and do not warrant specific investigation [29]. Airway Bronchospasm as an isolated phenomenon may not be allergic in nature but a result of pre-existing disease such as asthma or due to inadequate depth of anaesthesia. When patients’ lungs are mechanically ventilated, bronchospasm may present as a prolonged expiratory phase, high airway pressures, decrease in oxygen saturation or audible wheeze/rhonchi on auscultation [2]. Cardiovascular changes Tachycardia may not always be present, or may be masked in patients on beta-blockers. In contrast, hypotension may commonly present as the only symptom, and can be prolonged and resistant to treatment with the usual vasopressors [2]. When there is significant hypotension associated with anaphylaxis, there is likely to be a significant increase in serum tryptase [30]. All cases of prolonged or difficult-to-treat hypotension in the peri-operative period should be considered for allergy investigation. It is important to consider all sources of a patient's exposure to allergens in the peri-operative period when referring patients. This should include all drugs (i.v. and oral), disinfectants, dyes, transfusions and the use of medicines containing polyethylene glycols and methylcellulose, such as pre-operative laxatives. The substances which cause anaphylaxis most commonly in the peri-operative period are listed in Table 6 [31]. Table 6. Agents most commonly responsible for hypersensitivity reactions in anaesthetic practice Neuromuscular blocking agents 38% Antibiotics 31% Chlorhexidine 18% Patent blue dye 7% Latex 6% Opioids 2% Local anaesthetics 2% Of interest is the addition to this list of patent blue dye. In recent years, there has been an increase in the number of cases of severe anaphylaxis reported it being commonly used for sentinel node mapping in breast surgery [32]. One multi-centre study put the incidence at 1:3000, considerably higher than other drugs administered in the peri-operative period [33]. This has led to the suggestion that pre-operative skin testing should be conducted before its use [34]. However, due to intradermal administration and cutaneous uptake, ADRs to patent blue dye often appear 15-30 min after injection and may produce prolonged, biphasic reactions resistant to treatment [35]. In all cases of suspected ADRs, careful documentation is essential, with attention to the timing of symptoms following drug administration or exposure to potential triggers. The possibility of missed allergens should be considered in patients before further differential diagnoses are considered. Such differentials may include an undiagnosed mast cell disorder, which can also present with severe hypotension triggered by pain, stress and extremes of temperature in the peri-operative setting [36]. Management of adverse drug reactions It is beyond the scope of this article to review the management of adverse drug reactions for each individual class. Detailed guidelines on the management of anaphylaxis and malignant hyperthermia can be found on the AAGBI website (https://www.aagbi.org). In broad terms, less severe ADRs may be managed by lowering the dose or ceasing the drug, and providing supportive therapy. Rocuronium and sugammadex Much interest has been generated in the possibility of using sugammadex, in addition to standard management strategies, for the treatment of rocuronium-induced anaphylaxis. This arose from the hypothesis that the cyclodextrin sugammadex encapsulates rocuronium and therefore prevents the allergenic groups of rocuronium from interacting with IgE, mast cells and basophils [37]. Molecular models and in vivo experiments, however, do not support this theory [38]. Sugammadex has itself been shown to cause anaphylaxis [23, 39] and is not currently recommended in the treatment of rocuronium-induced anaphylaxis [40]. Reporting of adverse drug reactions In the UK, the Medicines and Healthcare products Regulatory Agency (MRHA) mediates the monitoring of adverse drug reactions through the yellow card scheme [41]. This has been in place for healthcare professionals since the thalidomide disaster in 1964. In 2003, the MHRA took primary responsibility for the collection and analysis of ADRs, and from October 2005, the scheme became accessible to both the general public and patients. Yellow cards can be found in the British National Formulary (BNF), Monthly Index of Medical Specialities (MIMS) and the Association of the British Pharmaceutical Industry (ABPI) Medicines Compendium. They can also be completed online at https://yellowcard.mhra.gov.uk. For drugs that are well established, only serious adverse effects should be reported (Table 7). For newer drugs, or those under additional surveillance, an inverted black triangle (▼) will appear in the product information, advertising material and the drug entry in the BNF, MIMS and ABPI Medicines Compendium. For these drugs, all ADRs should be reported, however minor (Table 7) [42]. Table 7. Adverse effects of well-established drugs to report to the Medicines and Healthcare products Regulatory Agency (MRHA) Serious adverse effects Fatal Life-threatening Disabling or incapacitating Congenital abnormalities Involved or prolonged hospitalisation Medically significant Many countries have comparable pharmaco-vigilance centres collecting data on ADRs and there are now 125 members of the WHO Programme for International Drug Monitoring. This information is collated by the ADR monitoring centre in Sweden and used to identify the first signs of danger posed by a drug. It was established in 1978 as a response to the global thalidomide disaster, and continues to have a significant role in the development of systems for drug safety worldwide [43]. For anaphylaxis, the anaesthetist who gave the anaesthetic, or the supervising consultant anaesthetist, is responsible for ensuring that the reaction is investigated. The patient should be referred to a specialist allergy or immunology centre. A list of centres can be found on the AAGBI (https://www.aagbi.org/safety/allergies-and-anaphylaxis) or British Society for Allergy and Clinical Immunology (http://www.bsaci.org/find-a-clinic/index.htm) websites. Reactions should be notified to the AAGBI National Anaesthetic Anaphylaxis Database via an allergy referral (https://www.aagbi.org/safety/allergies-and-anaphylaxis). The patient, surgeon and general practitioner should all be informed. Once the patient has been investigated and the causative agent determined, a yellow card should be completed [18]. The Yorkshire Allergy Pack can also be downloaded from the AAGBI website containing all the relevant forms and a useful checklist for the referral process. Malignant Hyperthermia assessment and monitoring is coordinated in the UK by a central unit at St James's Hospital In Leeds [44]. In addition to their screening service, they operate a 24-h hotline for medical practitioners, providing guidelines for referral criteria. Perhaps unsurprisingly, up to 50% of referrals can be attributed to other causes. The malignant hyperthermia unit also maintains a national registry of cases and genetically predisposed families. Such a registry helps provide advice on risk assessment to affected families and their relatives. Investigations of adverse drug reactions Those reactions referred for investigation from the peri-operative period are likely to be type B (hypersensitivity type-1 or anaphylaxis). About 60–70% of these reactions during anaesthesia are mediated by IgE, with more than 7000 cases published in the last 25 years [45]. It is important to have a systematic approach to the investigation of ADRs, and it requires a specialist allergist. Serum tryptase Tryptase is a peptidase made and stored in mast cells. It can be found in two forms, alpha and beta. Alpha tryptase is released constantly at low levels, but raised baseline levels can be found in systemic mastocytosis [46]. Symptoms of a hypersensitivity reaction and the presence of a raised beta serum tryptase increase the probability of anaphylaxis, but normal levels do not exclude it. As people have varying baseline levels of serum tryptase, it is important to collect more than one sample so comparisons can be made. In some individuals, it can take more than 24 h following a reaction for baseline levels to return to normal, and so a control sample should be taken after this time. There are timing guidelines for taking levels in the UK (Table 8) [18, 28, 47]. A significant increase in the concentration of serum tryptase (> 50 μg.l−1) suggests an IgE-mediated anaphylaxis [48]. Non-IgE-mediated reactions (such as complement-mediated reactions) may generate lower concentrations of 20–50 μg.l−1 [48]. Increased basal tryptase levels may be found in patients with systemic mastocytosis, mast cell activation syndrome or haematological diseases such as myelodysplastic syndromes and mast cell leukaemia [48]. These may or may not be known about before investigation and may complicate diagnosis. Table 8. Timings for serum tryptase sampling following suspected anaphylaxis Timing Sample 1 As soon as possible but do not delay resuscitation to take sample Sample 2 1–2 h after onset of symptoms Sample 3 24 h after onset of symptoms or in follow-up clinic (to measure baseline tryptase) Skin testing This takes the form of both skin prick testing and intradermal testing. These can be performed as soon as a patient has made a full recovery. Skin prick testing involves placing a drop of the drug on the volar surface of the forearm and pricking the skin through the drop with a lancet. The results are read after 15–20 min with histamine and saline solutions used as positive and negative controls. Drugs with antihistamine activity should be therefore discontinued several days before testing, but steroids (oral or inhaled) do not need to be stopped. Intradermal tests are usually performed on the forearm or back when skin prick tests are negative. They are more difficult to interpret with a higher false-positive rate and are more likely to precipitate a systematic reaction [18]. The European Network for Drug Allergy (ENDA) has published a list of non-irritant dilutions for skin prick and intradermal testing. It is notable that skin tests are not useful for non-IgE-mediated reactions, such as those caused by contrast media or NSAIDs [49]. As previously mentioned, anaesthetic drugs can cause IgE- or non-IgE- mediated reactions, with some causing anaphylaxis through either mechanism, adding to the difficulty in agent identification [13]. IgE assays There are IgE assays available for a limited number of drugs, including chlorhexidine, succinylcholine, latex and penicillin, but their sensitivity and specificity is variable. The presence of IgE is not necessarily proof the agent is the cause of a reaction, but indicates the individual has an allergic sensitization. However it does provide a possible mechanism if there is correlation with other clinical and laboratory information. The availability of these tests is variable depending on the country and speciality of the laboratory [18, 45]. Basophil activation test As well as mast cell activation, allergens stimulate histamine release and basophil surface activation of CD63 and CD203. The basophil activation test and histamine release test are not currently widely available to clinicians, but may be useful where hypersensitivity is highly suspected but not supported by skin testing or IgE assays. [2, 18]. Challenge testing In instances where skin tests are not diagnostic (such as NSAIDS and opiates) or where there is a clinical need to use a drug suspected of causing an ADR in the future, drug challenging may be considered. This should only be undertaken in a specialised centre given the risk of precipitating anaphylaxis. Patients should be consented, fully monitored and have i.v. access before a graded exposure to the drug orally, subcutaneously or intravenously [45]. Conclusion Adverse drug reactions, particularly those in the peri-operative period, can be severe and life-threatening. They impact on patient stay, healthcare costs, morbidity and mortality, and potentially affect future anaesthesia or drug exposure. Recognition of an ADR and identification of the causative agent can be challenging. As peri-operative specialists, anaesthetists must remain up to date with all aspects of ADRs, including possible clinical presentations, common causative agents, appropriate management and subsequent reporting. Acknowledgements No external funding or competing interests declared.

|
Scooped by
Jana Pearce
|
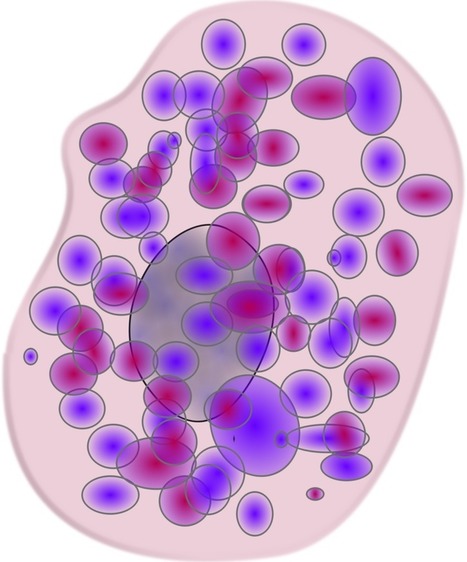
Many cancer and blood specialists will not have encountered systemic mastocytosis. A new drug targets the underlying defect of the disease and will help put doctors on the lookout. Keep reading below to learn more about this development, or follow the original story here. Dr. DeAngelo presented clinical data for a new drug agent at the annual meeting of the American Society of Hematology in 2017. The agent, known as avapritinib targets a specific mutation which occurs in 90% of mastocytosis cases. Results from an early trial show impressive results. Activity is high, and disease control was observed in all patients. Improvements in clinical symptoms also occurred rapidly. Dr. DeAngelo believes “once you have a therapy, patients will come.” He continues to explain that once an effective therapy is available, mastocytosis is a disease not to be overlooked. Dr. DeAngelo also mentioned that the amount of attention given to mastocytosis is already increasing. Last year, the FDA approved a new drug for mastocytosis called midostaurin When Dr. DeAngelo began taking an interest in mastocytosis he only saw one or two cases each year. Now he receives one to two each week. Current estimates show that 2000 cases of mastocytosis occur in the US each year. Dr. DeAngelo, on the other hand, suggests this is a low estimate and mentions how often the disease is missed. In today’s medicine, the most common way a mastocytosis patient reaches a hematologist is by referral from a dermatologist. This is usually as a result of skin lesions. Occasionally allergists or immunologists pickup on a patient who presents with recurring anaphylactic reactions. In both cases, symptoms could be signs of mast cells over producing as part of a pathology. Mast cells typically account for a few cells in every 1000. In a patient with mastocytosis, however, bone marrow may be flooded with mast cells at rates of 10-50%. Uncontrolled growth of mast cells often leads to distorted organs. In these cases, the spleen is swollen, leaving almost no room for the stomach. Mast cells may also build up in the small intestine and colon leading to malnutrition and loss of weight. In other cases, mast cells lead to impaired liver function and low blood counts. Sometimes mast cells even develop into a form of leukemia. Until the approval of midostaurin last year there was no treatment for mastocytosis. Other forms of therapy were limited and rarely successful. Even midostaurin sits only a step above though. The new results from avaprinitib are too early to call in full confidence, but have been markedly improved. In a small phase 1 study consisting of 18 evaluable patients, 72% experience an overall response, and every member of the group had their disease controlled. A phase 2 trial will test the drug on a larger number of patients. Success in the trial would mark a giant leap forward in the study and treatment of mastocytosis. The Secretary of the American Society of Hematology remarked that such a developmental leap would be something of a legend. He compared the new study to one 20 years ago in which new drugs had been discovered for the treatment of chronic myeloid leukemia. What are your thoughts about living with mastocytosis? Share your thoughts, and your hopes, withthe Patient Worthy community! Comments comments

|
Scooped by
Jana Pearce
|
Mast Cell Diseases are diseases that impact mast cells. A mast cell is a type of cell found in the connective tissues in the body. They are located in the skin, lining of the gastrointestinal tract, bone marrow, airway, and other organs.
|

 Your new post is loading...
Your new post is loading...
 Your new post is loading...
Your new post is loading...