Your new post is loading...
 Your new post is loading...
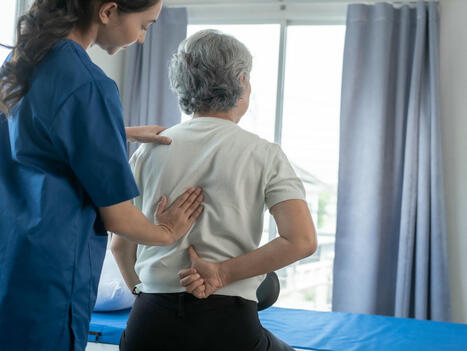
Introduction: Why Chiropractic Care Matters After a Car Accident Car accidents can cause more than just vehicle damage—they can leave people with hidden injuries that affect their quality of life. Many of these injuries don’t show up right away. Pain in the neck, back, or joints can start days after the crash. That’s where chiropractic care becomes essential. Chiropractors specialize in identifying and treating musculoskeletal problems, especially those involving the spine. They use hands-on techniques to realign joints, reduce inflammation, and relieve pain without drugs or surgery. Chiropractic care has become a key part of rehabilitation after motor vehicle accidents (MVAs) because of its effectiveness in treating injuries like spinal misalignment, whiplash, and soft tissue damage. Chiropractors not only help people feel better—they also help prevent long-term problems by addressing injuries early on. 🔗 Miami Chiropractors, 2024 Spinal Misalignment and the Role of Chiropractic Adjustments When the body experiences the sudden jolt of a car crash, the spine often gets pushed out of alignment. This misalignment can affect how the nerves communicate with the rest of the body, causing pain, stiffness, or numbness. Chiropractors use a technique called spinal adjustment to gently move the vertebrae back into place. This helps restore proper joint motion and improve nerve function. Spinal adjustments are quick, precise, and typically cause little to no discomfort. Over time, they can help reduce inflammation and allow the body to heal naturally. Many people report immediate relief after an adjustment, and consistent chiropractic care can speed up recovery and improve overall mobility. 🔗 Tradition Health, 2025 Healing Soft Tissue Injuries With Chiropractic Techniques Soft tissue injuries—like strains, sprains, and bruises—are very common after a car crash. These injuries affect muscles, ligaments, and tendons, often leading to pain and limited movement. While they may not appear on X-rays, they can still cause serious discomfort. Chiropractors use several non-invasive techniques to support soft tissue healing. These may include: -
Trigger point therapy to relax tight muscles -
Stretching and strengthening exercises -
Ultrasound therapy to reduce inflammation -
Cold laser therapy to promote cell repair By addressing these injuries early, chiropractic care can help avoid scar tissue buildup and long-term stiffness. 🔗 Liott Back and Neck Center, 2024 Supporting Natural Healing and Pain Relief The human body is designed to heal itself, but after an accident, that process sometimes needs a little help. Chiropractic care supports the body’s natural ability to recover. Rather than covering up pain with medication, chiropractors work to find and fix the root cause of the discomfort. Adjustments improve blood flow, reduce nerve interference, and decrease inflammation. This leads to better healing outcomes. People who receive early chiropractic treatment often report faster recovery and less reliance on pain medications. 🔗 Colorado Health Clinic, 2024 Early Intervention: Why Timing Matters Getting chiropractic care soon after a car accident can make a big difference. The earlier an injury is treated, the better the chances of preventing long-term damage. Delaying treatment can allow inflammation to worsen and injuries to become chronic. According to Dr. Kal’s clinic, early chiropractic care can reduce the chance of complications like nerve damage or post-traumatic arthritis. Immediate treatment helps with pain management and makes it easier for patients to return to daily activities. 🔗 Dr. Kal, 2024 Comprehensive Assessments and Customized Treatment Plans Every car accident is different, and so is every person’s body. That’s why chiropractors begin with a thorough evaluation, which may include: Once they understand the full picture, chiropractors create personalized treatment plans. These may include regular spinal adjustments, physical therapy, massage therapy, and advice on lifestyle changes. 🔗 Dr. Kal, 2024 Holistic Rehabilitation: Mind, Body, and Function Chiropractic care is about more than just the spine. It supports total wellness by restoring physical function and promoting emotional well-being. After an accident, many people feel overwhelmed by stress, trauma, and physical pain. Chiropractic therapy can help calm the nervous system and improve mental clarity by relieving pressure on the spine. This whole-body approach makes it easier for patients to return to work, drive again, and enjoy everyday activities. 🔗 Creekside Chiropractic, 2024 Cost Savings and Long-Term Benefits Motor vehicle accidents often come with high costs—medical bills, lost wages, car repairs, and more. Chiropractic care can actually reduce healthcare costs in the long run by helping people avoid surgery and long-term medication use. Some insurance providers, including auto and personal injury protection (PIP) plans, may cover chiropractic treatment. Seeking chiropractic care early can also create important medical records that help with legal claims and compensation. 🔗 MVA MVP, 2024 Long-Term Recovery and Prevention of Chronic Conditions Some injuries from car accidents can linger for months or years. Without proper treatment, issues like chronic back pain, neck stiffness, and migraines can develop. Chiropractic care focuses on long-term healing by keeping the spine and joints healthy and flexible. Regular adjustments and follow-up care can prevent minor issues from becoming major problems. Patients often continue chiropractic care even after their pain is gone to maintain wellness and reduce the risk of future injury. 🔗 The Neck and Back Clinics, 2024 Detecting Hidden Injuries Early Not all injuries are obvious right after an accident. Whiplash, for example, can take days to develop symptoms. Chiropractic assessments help find these "hidden" problems before they worsen. Chiropractors are trained to detect misalignments and nerve issues that don’t always show up on basic scans. Early detection and treatment are key to preventing chronic issues like spinal degeneration or nerve entrapment. 🔗 Pioneer Chiropractic, 2024 Chiropractic Support for Headaches and Migraines Many accident victims report headaches and migraines that stem from neck strain or tension in the spine. Chiropractic care can reduce the frequency and intensity of these headaches by realigning the cervical spine and relieving nerve pressure. Adjustments to the upper neck can help improve circulation and reduce tension, leading to fewer headaches and better sleep. 🔗 Apex Orthopedic and Sports Medicine, 2024 Dr. Alexander Jimenez: A Dual-Scope Approach in El Paso Dr. Alexander Jimenez, DC, APRN, FNP-BC, is a well-known chiropractor and nurse practitioner in El Paso who specializes in helping people recover from motor vehicle accidents. His unique combination of chiropractic and medical training allows him to diagnose injuries, order imaging, treat musculoskeletal problems, and handle legal documentation for personal injury cases. Dr. Jimenez uses advanced diagnostic tools, like MRI and digital motion X-rays, to assess internal damage. He connects the dots between symptoms and root causes—a process known as dual diagnosis. Whether the problem is whiplash, nerve damage, or spinal instability, Dr. Jimenez creates customized plans that may include chiropractic adjustments, rehabilitation exercises, massage, and nutritional guidance. Dr. Jimenez’s dual role also allows him to complete legal paperwork accurately, which helps patients file injury claims and receive fair compensation. His integrative approach makes it easier for patients to recover both physically and financially. 🔗 Dr. Alex Jimenez – Clinical Insights
🔗 LinkedIn – Dr. Alexander Jimenez
🔗 Instagram
🔗 Threads
🔗 Pinterest
🔗 Facebook
🔗 WellnessDoctorRx
🔗 Twitter/X Conclusion: The Value of Chiropractic in Car Accident Recovery Chiropractic care offers a safe, natural, and highly effective way to heal after a motor vehicle accident. From spinal adjustments that restore joint function to soft tissue therapies that reduce inflammation, chiropractic treatment focuses on addressing the root causes of pain. It also helps patients recover faster, avoid long-term problems, and regain their independence. With professionals like Dr. Alexander Jimenez leading the way in dual-scope care, patients can benefit from both medical and chiropractic expertise. Whether it’s reducing pain, improving mobility, or preparing legal documents, chiropractic care plays a vital role in full-body recovery after a crash. Understanding Ligamentous Injuries | El Paso, Tx References Apex Orthopedic and Sports Medicine. (2024). Should I see a chiropractor after a car accident? Colorado Health Clinic. (2024). Benefits of chiropractic care after a car accident Creekside Chiropractic. (2024). Auto injuries care Dr. Kal. (2024a). Early chiropractic care after car crashes: Why it matters Dr. Kal. (2024b). Chiropractic care after a car accident: What to expect Liott Back and Neck Center. (2024). Top chiropractor for auto accident recovery: What to know Miami Chiropractors. (2024). The role of chiropractic care in rehabilitation after a car accident MVA MVP. (2024). Why chiropractic care is essential after a motor vehicle accident Pioneer Chiropractic. (2024). Benefits of chiropractic care after a car accident The Neck and Back Clinics. (2024). Long-term recovery Tradition Health. (2025). Chiropractic treatment after car accidents General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, and physical medicine, as well as wellness, sensitive health issues, and functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and the jurisdiction in which they are licensed to practice. We utilize functional health and wellness protocols to treat and support care for injuries or disorders affecting the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters and issues that relate to and directly or indirectly support our clinical scope of practice. Our office has made a reasonable attempt to provide supportive citations and identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, please contact Dr. Alex Jimenez or us at 915-50-0900. Dr. Alex Jimenez, DC, MSACP, CCST, IFMCP*, CIFM*, ATN* Email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
🚗 Healing Beyond the Collision: Functional Medicine and MVA Recovery Introduction: The Ripple Effects of MVAs Motor vehicle accidents often leave victims with visible injuries—like whiplash or fractures—but they can also trigger hidden trauma. Beyond physical impact, MVAs can disrupt the body’s balance, triggering pain in the back, neck, and even digestive system, while leaving emotional scars behind. Functional medicine offers a holistic, personalized plan that treats not just symptoms, but identifies and heals the root causes. This article explores: -
Indirect trauma & neck/back pain -
Hidden gut damage from MVAs -
Emotional and neurological consequences -
The functional medicine toolkit -
Dr. Alexander Jimenez's El Paso model, blending clinical care with legal needs 1. Indirect Trauma: The Hidden Force from MVAs Even without visible injury, the abrupt forces of a crash stretch neck muscles and ligaments. This is called whiplash, which often leads to chronic neck and back pain if untreated. According to Baystate Physical Therapy, whiplash “stretches spinal ligaments and muscles,” causing lingering discomfort (healthcoach.clinic, elpasobackclinic.com, personalinjurydoctorgroup.com). Dr. Alexander Jimenez (DC, APRN, FNP‑BC) emphasizes that “indirect trauma” from vehicle collisions frequently results in persistent joint pain and muscular stiffness long after the event (elpasobackclinic.com). These injuries may not show up on initial scans, but pain and dysfunction persist, affecting posture, flexibility, and daily performance (elpasobackclinic.com). 2. Neck & Back Pain: When Muscles Lose Balance Crash impacts can misalign vertebrae, inflame discs, and irritate nerves, leading to muscle spasms and sensitivity. Dr. Jimenez often treats: -
Cervical spine misalignments from whiplash -
Lumbar strain due to compensatory movement -
Sciatica risks from disc pressure or nerves (dralexjimenez.com) He uses spinal decompression, manual adjustments, targeted rehab exercises, and acupuncture to reduce pain and restore function, aiming to prevent chronic joint degeneration (dralexjimenez.com). 3. Gut Health: The Overlooked System Did you know that MVAs can harm your digestive system? These accidents may: -
Cause direct abdominal trauma -
Trigger stress-related changes in gut flora (the “gut–brain axis”) -
Include medications like NSAIDs that irritate the intestine A recent blog says the gut is “often referred to as the ‘second brain,’” and MVAs impact it via trauma, stress, and drug side effects (dralexjimenez.com). Dr. Jimenez confirms that teens using NSAIDs for whiplash pain often report stomach pain or diarrhea—hidden effects frequently missed in accident assessments (personalinjurydoctorgroup.com). By focusing on diet, stress reduction, and safe supplements, functional medicine helps protect and heal the GI system, restoring nutrient balance and reducing inflammation. 4. Emotional & Nervous System Trauma MVAs are not just physical events—they cause psychological stress too. Emotional shock triggers an increase in adrenaline, cortisol, and nervous tension. These changes contribute to pain amplification, slowed healing, fatigue, and “brain fog” (dralexjimenez.com). Dr. Jimenez utilizes mindfulness, stress management, gentle exercise, and nervous system calming therapies—including acupuncture and chiropractic care—to enhance autonomic nervous system function and promote healing. (chiromed.com). 5. Functional Medicine: A Root-Cause Healing Path Functional medicine aims to achieve lasting health by identifying the underlying causes of symptoms, rather than merely masking them. Here’s how it applies to MVAs: Functional Medicine Strategy Purpose in MVA Recovery Functional Nutrition Reduces inflammation, supports gut and tissue repair ( healthcoach.clinic, chiromed.com) Manual & Spinal Therapies Corrects alignment issues to restore nervous system function Physical Rehabilitation Exercises Enhances strength, movement, posture, and injury prevention Stress Management Supports autonomic healing (reducing “freeze/fight” states) Diagnostics & Imaging Identifies ligament injuries, nerves, tissue damage—guides treatment 6. The El Paso Model: Dr. Jimenez’s Clinical‑Legal Integration a) Dual Credentials for Comprehensive Diagnosis Dr. Jimenez is both a chiropractor and board-certified nurse practitioner (FNP‑BC). This enables: b) Advanced Diagnostics in MVA Cases He employs: Functional panels reveal nutritional and genetic weaknesses that impede healing. (healthcoach.clinic). c) Structured Clinical Biography & Documentation For personal injury claims, Dr. Jimenez documents: -
Detailed history of trauma, timing, and symptoms -
Objective findings over time -
Quantitative metrics like range-of-motion scores -
Prognosis & treatment plans (elpasobackclinic.com, dralexjimenez.com) This level of documentation is critical in El Paso MVA legal claims, ensuring accurate injury assessment & support for compensation (healthcoach.clinic). d) Patient-Centered Treatment Approach He integrates: 7. Treatment Results: Real Progress Patients under Dr. Jimenez’s model often show: -
Improved range of motion & pain relief within weeks (elpasobackclinic.com) -
Restored gut comfort when NSAIDs are replaced with diet & mild herbs -
Reduced stress and fatigue, enhancing morale and healing capacity 8. Why Functional Medicine Works for MVAs -
Holistic: Treats body as a system, not just neck/back -
Custom: Uses labs & imaging to target root causes -
Evidence-based: Integrates proven interventions—manual therapy, nutrition, exercise -
Legal clarity: Produces detailed records that doctors, insurance, and lawyers trust 9. Tips for MVA Survivors & Families -
Early assessment: Even mild pain should be professionally evaluated. -
Choose holistic care: Look for practitioners skilled in diagnostic imaging and natural therapies. -
Track progress: Keep logs and pictures to show changes over time. -
Customize nutrition: Focus on anti-inflammatory, gut-healing meals and supplements. -
Include stress relief: Build rest, mindfulness, or counseling into routines. -
Pay attention to gut symptoms: Bloating, cramps, or diarrhea matter and impact healing. -
Document everything: Dates, pains, treatments—key for future claims. 10. Conclusion: From Collision to Complete Healing MVAs can cause far more than bruises or soreness—they may disrupt joint stability, gut health, stress balance, and quality of life. Functional medicine, championed by experts like Dr. Alexander Jimenez in El Paso, offers a powerful and personalized recovery path that combines clinical excellence with comprehensive documentation. By addressing root causes and treating patients as whole beings, this model delivers lasting health, reduced pain, and empowered healing. 📝 References (APA 7) -
Jimenez, A. D. (2025, June 13). El Paso Motor Vehicle Accident Physical Therapy Insights. HealthCoach. -
Jimenez, A. D. (2025, June 16). Motor vehicle accidents and gut health concerns. PersonalInjuryDoctorGroup. -
Jimenez, A. D. (2025). Motor vehicle accident gut health trauma solutions. DrAlexJimenez.com. -
Jimenez, A. D. (2025). Auto injuries and their consequences on the nervous system. DrAlexJimenez.com. -
Jimenez, A. D. (2025). Ligamentous injuries after motor vehicle accidents. HealthCoach. -
Jimenez, A. D. (2025, June 16). Motor vehicle accidents and gut health concerns. PersonalInjuryDoctorGroup. -
Jimenez, A. D. (n.d.). Motor vehicle accidents and gut health concerns. PersonalInjuryDoctorGroup. -
Jimenez, A. D. (2025). Post-automobile accident nutrition for quick recovery. HealthCoach. -
Jimenez, A. D. (2025). Dr. Jimenez injury rehabilitation: effective MVA care. ElPasoBackClinic. -
Jimenez, A. D. (2025). The hidden impact of motor vehicle accidents on gut health. ChiroMed. -
Jimenez, A. D. (n.d.). Dr. Alex Jimenez, DC, APRN, FNP‑BC, CFMP, IFMCP. A4M. -
Baystate Physical Therapy. (2025). Whiplash biomechanics and treatment. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, and physical medicine, as well as wellness, sensitive health issues, and functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and the jurisdiction in which they are licensed to practice. We utilize functional health and wellness protocols to treat and support care for injuries or disorders affecting the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice. Our office has made a reasonable attempt to provide supportive citations and identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, please contact Dr. Alex Jimenez or us at 915-50-0900. Dr. Alex Jimenez, DC, MSACP, CCST, IFMCP*, CIFM*, ATN* Email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Children walking with their toes pointed in may be pigeon-toed. What are the causes, conditions associated with it, and treatments? Pigeon-toed Walking If a child walks with their feet turned inward at the toes, it is usually described as being pigeon-toed. This pointing inward of the feet occasionally occurs as a child learns to walk and may continue through toddlerhood. It is noticed more often in children than adults, but older individuals can experience it. Pigeon-toed walking is rarely a major orthopedic problem and usually disappears without treatment. However, there are times when it may impact a child's lower extremities and hips. Bracing or surgery may be necessary in these cases to correct the problem. (Paramanandam V. et al., 2019) This condition is common and typically is caused by abnormal birth positions in utero. Sometimes, slight issues may lead to noticeable functional characteristics. Mild changes in bone shape and positioning usually cause pigeon toes. Often, it subsides in a few years as the child continues to develop. What Does It Mean? There is usually no need to worry, as this condition is likely not permanent and will disappear in a few years. (Paramanandam V. et al., 2019) However, it is recommended that you check in with your healthcare provider to ensure the child is developing normally. Some adults walk with their toes turned in. This may be due to a birth defect, a weakness, or a rare case of pigeon-toed walking as a youth that was left untreated or did not go away. Causes There are various reasons for pigeon-toed walking. To determine the cause, a healthcare provider can assess the child's condition and make a diagnosis, including: Metatarsus Adductus - A condition where the front part of the foot is turned inward.
- The metatarsals are the long bones of the forefoot.
- This is when the bones of the foot point inward, leading to pigeon-toed walking.
- A clinical examination and X-ray can confirm the metatarsus adducts as a cause of pigeon-toed walking.
Tibial Torsion - A twisted shinbone (tibia) can cause the feet to turn inward in younger children.
- The shinbone/tibia in some children may be slightly twisted.
- The tibia can either turn outward or inward.
- When it twists inward, it may manifest as a pigeon-toed gait.
- Tibial torsion may accompany femoral anteversion.
- It is diagnosed with an X-ray.
- Children with tibial torsion typically grow out of the problem, and the pigeon-toed disappears by age 4. (Uden H., & Kumar S. 2012)
Femoral Anteversion - A common cause, especially in older children, is when the thighbone/femur is twisted inward.
- If the femur turns inward and forward unnaturally, where the femoral neck meets the body of the femur, it is called femoral anteversion.
- An outward and backward rotation of the femur is called femoral retroversion.
- This occurs in about 10% of children. (Scorcelletti M. et al., 2020)
- Many children with femoral anteversion appear knock-kneed with a large gap between their feet when standing with knees together, and when they walk, they appear pigeon-toed.
- A clinical examination and X-ray diagnose it.
Symptoms In most cases, the child does not complain of any pain. However, if pain is felt, it can include: - Tightness in the calf muscles
- Aching on the outer edges of the feet
- Knee pain
Usually, parents will notice pigeon-toes when their child is first learning to walk. Rest assured, the child most likely is not experiencing pain. They have feet and knees that turn inward when they walk and run. (Uden H., & Kumar S., 2012) A pediatrician or primary care provider can assess the situation and make recommendations. Most pigeon-toed children begin walking and running normally after age 3 or 4, so a watch-and-wait approach is used. Parents may have to take their child to a specialist, like an orthopedic surgeon, if they complain of pain while walking. A specialist may be referred if the child cannot walk due to the inward turn of their feet. Risk Factors Pigeon-toed walking is not a preventable condition but rather one that develops during pregnancy. Causes may include: (Scorcelletti M. et al., 2020) - A pregnancy with twins or multiple births
- Large fetus
- Breech position in utero when the baby is positioned feet first.
- Not enough amniotic fluid
Muscle Weakness in Adults Adolescents or adults who notice their knees turn in and walk pigeon-toed may have weakness in the hip and leg muscles that control the position of their legs when they walk. Strengthening those muscles can help. (Scorcelletti M. et al., 2020) Treatment Typically, a normal gait will appear by age 3 or 4. Other treatments may include: Physical Therapy Exercises and Gait Training - Exercises to stretch tight lower extremity muscles and strengthen hip and leg muscles can help improve walking gait.
- See a pediatric specialist before starting, as research shows that parental stretching of a newborn with metatarsus adductus offers little benefit. (Eamsobhana P. et al., 2017)
Bracing or Casting - Braces
- Serial casting is a procedure that helps children improve their range of movement and may be done to place their lower extremities in an optimum position as they develop. (Uden H., & Kumar S., 2012)
Surgery - For cases in which tibial torsion is the cause, osteotomy surgery, which involves cutting and/or removing bone, may be recommended to correct the structural deformity of the shinbone.
Injury Medical Chiropractic & Functional Medicine Clinic Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, and physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice. Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, please contact Dr. Alex Jimenez or us at 915-50-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Paramanandam, V., Lizarraga, K. J., Soh, D., Algarni, M., Rohani, M., & Fasano, A. (2019). Unusual gait disorders: a phenomenological approach and classification. Expert review of neurotherapeutics, 19(2), 119–132. https://doi.org/10.1080/14737175.2019.1562337 Uden, H., & Kumar, S. (2012). Non-surgical management of a pediatric "intoed" gait pattern - a systematic review of the current best evidence. Journal of Multidisciplinary Healthcare, 5, 27–35. https://doi.org/10.2147/JMDH.S28669 Scorcelletti, M., Reeves, N. D., Rittweger, J., & Ireland, A. (2020). Femoral anteversion: significance and measurement. Journal of Anatomy, 237(5), 811–826. https://doi.org/10.1111/joa.13249 Eamsobhana, P., Rojjananukulpong, K., Ariyawatkul, T., Chotigavanichaya, C., & Kaewpornsawan, K. (2017). Does the parental stretching programs improve metatarsus adductus in newborns?. Journal of Orthopaedic Surgery (Hong Kong), 25(1), 2309499017690320. https://doi.org/10.1177/2309499017690320
Get insights into GI disorder treatment strategies that can help restore balance and improve overall gastrointestinal health. What Are GI Disorders? How often do you feel bloated after eating a large meal? Do you experience constipation or inflammatory effects in your gut? Or do you experience stiffness in your joints and muscles? Many people don’t realize that environmental factors can affect their gut system and cause numerous overlapping risk profiles in the body by extending their impact onto the musculoskeletal system, thus causing pain-like symptoms that often mimic musculoskeletal disorders. Gastrointestinal (GI) disorders are usually common, depending on the severity, and can be a challenge to manage while having significant medical and social effects. (Malone et al., 2018) Some common GI disorder conditions include irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), and small intestinal bacterial overgrowth (SIBO). GI disorders can contribute to chronic pain, joint stiffness, and muscle dysfunction within the musculoskeletal system. By understanding the gut-musculoskeletal connection, many individuals can look for functional, non-surgical options that can relieve and improve their quality of life. How GI Disorders Affect The Gut & Musculoskeletal System Environmental factors play a key part in developing GI disorders, and many people wonder how they can affect their guts and muscles. Stress is one environmental factor that can affect the gut and muscles. Stress can affect a person physically and psychologically, causing the gut bacteria to respond differently and leading to GI disorders. (Konturek et al., 2011) Inflammation & Systemic Effects When GI disorders start to affect the body, they cause inflammation to develop and attach themselves to the affected area, causing issues to the gut. When inflammation begins to affect the gut system, it can induce low-grade inflammation and affect the gut barrier integrity while disrupting regular nutrient and food digestion. (Casini et al., 2024) This can lead to chronic GI conditions that incorporate inflammatory components like Crohn’s disease or ulcerative colitis. This, in turn, can trigger systemic inflammation in the musculoskeletal system by releasing cytokines and inflammatory mediators into circulation, causing symptoms of muscle pain, joint stiffness, and fatigue. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Can individuals experiencing difficulty with functional mobility benefit from physical therapy to help them return to normal activities? Outcome Measurement Tests Outcome measurement tests assess the effects of a treatment plan on a patient. They can be used to determine a patient's baseline function, monitor their progress, and evaluate the effectiveness of treatment. They also give the therapy team an effective way to measure mobility, flexibility, and range of motion. Function and Purpose Outcome measurement tests serve various purposes. These include: (American Physical Therapy Association, N.D.) - To assist in goal-setting
- Provide motivation
- To guide treatment
- To give a prognosis for the specific condition
- To justify the treatment
The physical therapist may use other functional outcome measurements to help assess physical therapy progress. - They may measure your strength and range of motion.
- Balance and posture may be evaluated.
Effective functional outcome measurement tests must meet certain criteria to be useful in a physical therapy clinic. First, they must be reliable, meaning the results must be consistent with each patient and within groups of patients. They must also be valid to measure exactly what they are intended to measure. An effective measurement test must also be easy to administer, so it must be practical and simple. Outcome measurement tests must also be purposeful. For example, a balance test must reflect a patient's current function and be related to their balance ability. Common Outcome Measurement Tests Used Common functional outcome measurement tools that a physical therapist may use include: - The timed up-and-go or TUG test is a simple assessment used to evaluate a person's mobility and balance by measuring how long it takes them to stand up from a chair, walk a short distance, turn around, walk back, and sit down again; it's often used to identify potential fall risks in older adults, particularly those with mobility concerns, as a longer time to complete the task may indicate increased fall risk. (Centers for Disease Control and Prevention, 2017)
- The Tinetti balance and gait evaluation, also known as the Performance-Oriented Mobility Assessment (POMA), is a clinical test used to assess balance and gait abilities, particularly in older adults. It evaluates stability during various standing and walking tests and provides a score that indicates a person's fall risk potential.
- The Berg Balance Scale (BBS) is a standardized test for adults that measures balance and the risk of falling. It's widely used and can be performed in various settings.
- The six-minute walk test (6MWT) is a medical assessment in which a person walks as far as they can in a designated area for exactly six minutes. This allows healthcare providers to evaluate their functional exercise capacity. It is particularly useful for assessing patients with lung or heart conditions where walking ability might be compromised. The distance covered during the six minutes is the key measurement used to interpret the test results. (Ferreira M. B. et al., 2022)
- The functional reach test (FRT) is a clinical assessment that measures an individual's dynamic balance by determining the maximum distance they can reach forward while standing in a fixed position. It assesses their risk of falling by evaluating how far they can extend their arm before losing stability. The FRT is often used to assess older adults or individuals with potential balance issues.
- The Oswestry low back pain disability questionnaire is a self-administered questionnaire used to measure the level of disability a person experiences due to low back pain. It assesses how the pain impacts their daily activities in various aspects of life, such as personal care, work, and social life; a higher score indicates greater disability.
- The functional independence measure (FIM) assesses a patient's ability to perform daily activities independently. It also measures the patient's disability level and how much assistance is needed.
Functional outcome measurement tests provide a starting point for developing physical therapy goals. For example, if the TUG test takes 19 seconds, individuals may aim for 10 seconds. A TUG score that falls at or over 10 seconds indicates reduced physical capacity (Kear B. M., Guck T. P., & McGaha A. L. 2017). This can be the motivation needed to reach physical therapy goals. Injury Medical Chiropractic and Functional Medicine Clinic Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References American Physical Therapy Association. (N.D.). Outcome Measures in Patient Care. https://www.apta.org/your-practice/outcomes-measurement Centers for Disease Control and Prevention. (2017). Timed Up & Go Assessment. Retrieved from https://www.cdc.gov/steadi/media/pdfs/steadi-assessment-tug-508.pdf Ferreira, M. B., Saraiva, F. A., Fonseca, T., Costa, R., Marinho, A., Oliveira, J. C., Carvalho, H. C., Rodrigues, P., & Ferreira, J. P. (2022). Clinical associations and prognostic implications of 6-minute walk test in rheumatoid arthritis. Scientific reports, 12(1), 18672. https://doi.org/10.1038/s41598-022-21547-z Kear, B. M., Guck, T. P., & McGaha, A. L. (2017). Timed Up and Go (TUG) Test: Normative Reference Values for Ages 20 to 59 Years and Relationships With Physical and Mental Health Risk Factors. Journal of primary care & community health, 8(1), 9–13. https://doi.org/10.1177/2150131916659282
Could regular daytime naps help individuals slow the aging process from natural brain shrinkage? Taking Naps Research and experts suggest that a short nap between 10 to 40 minutes provides the most benefits, including: - Improved mood
- Cognitive performance
- Alertness
A study suggests that daytime napping might prevent the brain from shrinking with age. (Paz V., Dashti H. S., & Garfield V. 2023) Optimal Nap Time A small study of young adults found that naps lasting 10 to 60 minutes immediately improved mood and alertness. However, most research shows that naps under 30 minutes offer the most benefit because individuals are less likely to enter the deep sleep stage or experience sleep inertia - a period of impaired alertness right after waking. A meta-analysis also suggested that short naps reduce fatigue, increase productivity, and enhance physical performance. (Dutheil F. et al., 2021) A 10-minute nap is the most effective at improving: - Sleep latency or sleep onset latency (SOL)
- Fatigue
- Vigor
- Cognitive performance
Some sleep specialists recommend that patients not take naps longer than 40 minutes, as too much napping could be unhealthy. Studies have shown that excessive daytime sleepiness and napping for over 60 minutes might increase the risk of type 2 diabetes and heart problems. (Yamada T, Nobuhiro S, Takashi K. 2016) Health In the study published in Sleep Health, researchers used data from over 30,000 participants aged 40 to 69 from the U.K. Biobank. Researchers examined genetic variants associated with taking naps regularly. (Paz V., Dashti H. S., & Garfield V. 2023) The researchers found a link between regular daytime napping and larger brain volume. The difference in brain volume between individuals who nap regularly and those who don't was equivalent to 2.6 to 6.5 years of aging. However, no association was found between napping and cognitive performance reaction time or visual memory. The brain naturally shrinks with age, but this process is accelerated in individuals with neurodegenerative diseases and cognitive decline. How To Avoid Napping for Too Long Taking naps is good for you. But there's a difference between healthy daytime sleep and counterproductive excessive sleeping. - Sleep specialists recommend setting an alarm for a nap or asking a family member, friend, or coworker to wake you up.
- Individuals can place their phones or alarm clocks far away, so they must move them to turn them off.
- Individuals are recommended to stand up immediately to wake the body through movement and light exposure to avoid feeling groggy after a nap.
- One study suggests consuming caffeine before a nap may be an effective countermeasure for sleep inertia. (Hilditch C. J., Dorrian J., & Banks S. 2016)
- Engaging in physical activities before and after naps can also help promote wakefulness.
Sometimes, people feel exhausted for various reasons, such as stress and nutrition, rather than a lack of sleep. In these cases, sleeping more than the body needs will only worsen sleep quality at night. When individuals are experiencing daytime fatigue, rather than lying back down or sitting in bed, sleep specialists suggest walking around. This allows the fatigue to pass, and the patient can sleep better at night. Injury Medical Chiropractic and Functional Medicine Clinic Chiropractic's goals are to help individuals enhance movement with less pain due to a condition after injury or surgery. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body heal itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Paz, V., Dashti, H. S., & Garfield, V. (2023). Is there an association between daytime napping, cognitive function, and brain volume? A Mendelian randomization study in the UK Biobank. Sleep health, 9(5), 786–793. https://doi.org/10.1016/j.sleh.2023.05.002 Dutheil, F., Danini, B., Bagheri, R., Fantini, M. L., Pereira, B., Moustafa, F., Trousselard, M., & Navel, V. (2021). Effects of a Short Daytime Nap on the Cognitive Performance: A Systematic Review and Meta-Analysis. International journal of environmental research and public health, 18(19), 10212. https://doi.org/10.3390/ijerph181910212 Yamada T, N. S., Takashi K. (2016). Daytime napping, daytime sleepiness and the risk of metabolic diseases: dose-response meta-analysis using restricted cubic spline model. J Am Coll Cardiol., 67(13), 1951. https://doi.org/https://doi.org/10.1016/S0735-1097(16)31952-0 Hilditch, C. J., Dorrian, J., & Banks, S. (2016). Time to wake up: reactive countermeasures to sleep inertia. Industrial health, 54(6), 528–541. https://doi.org/10.2486/indhealth.2015-0236
Can individuals dealing with psoriatic arthritis find non-surgical treatments to reduce joint pain and improve skin health? Introduction The body is a complex machine with a communal relationship with the joints, organs, bones, muscles, and tissues, each of which has a specific function to ensure the host is alive. The brain is the main control system that gives each body’s systems, organs, muscles and joints a job. When environmental factors or pathogens enter the body, the immune system is the first one to defend the body and eliminate the pathogens to initiate the natural healing process. However, when the immune system is attacking the body constantly, over time, it can lead to autoimmunity and cause overlapping risk profiles in the body. This, in turn, can lead the development of chronic conditions and cause individuals pain and discomfort. In today’s article, we look at an autoimmune disorder known as psoriatic arthritis, its causes and symptoms, and how treatment can help reduce its pain like effects. We discuss with certified medical providers who inform our patients how psoriatic arthritis can affect the joints. While asking informed questions to our associated medical providers, we advise patients to incorporate various non-surgical treatments to reduce psoriatic arthritis symptoms and help manage joint pain that affects a person’s quality of life. Dr. Alex Jimenez, D.C., encompasses this information as an academic service. Disclaimer. What Is Psoriatic Arthritis? Do you experience swelling in your joints that causes pain and discomfort when moving? Do you feel your skin itchier and warmer than usual? Or have you noticed that everyday tasks are more difficult now than before? Many of these pain-like scenarios are associated with joint pain associated with an autoimmune or musculoskeletal condition. Since autoimmunity is developed when environmental factors cause the immune system to attack healthy cells, it can envoke pain and discomfort to the body. When a person is dealing with an autoimmune condition, it can impact not only the individual but also the rest of the body’s system. For instance, if a person is dealing with an autoimmune condition, they could be dealing with skin issues that can cause them to develop scaly, itchy, red skin patches known as psoriasis. If they have joint pain combined with psoriasis, it can develop into psoriatic arthritis. (Skornicki et al., 2021) Now psoriatic arthritis is a heterogeneous autoimmune condition with musculoskeletal involvement that can manifest various symptoms including inflammation and arthritis. (Hackett et al., 2022) This in turn causes many individuals to think they are dealing with rheumatoid factors. Causes & Symptoms As a multifactorial pathology, psoriatic arthritis causes care often influenced by a complex interplay of immunological, environmental, and genetic factors that cause its development. (Zalesak et al., 2024) When the immune system starts to attack the healthy cells in the body, the inflammatory cytokines can become haywire and attack the “problem,” causing the development of autoimmunity. Within this integration, some of the causes can include predisposing genetic backgrounds with the presence of environmental factors that can activate the innate immune system precipitate the onset of psoriatic arthritis. (Azuaga et al., 2023) Some of the symptoms can many individuals with psoriatic arthritis can include: - Tendon tenderness
- Joint pain
- Stiffness
- Fatigue
- Joint swelling
- Skin rash
- Musculoskeletal pain
However, there are ways to manage psoriatic arthritis, reduce joint pain from affecting a person, and help them manage the symptoms. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Can beginner workouts help individuals who want to improve their health by helping them lose weight and improve their quality of life? Beginner Workouts Individuals new to exercise do not need to go through intense workout sessions to gain the benefits of physical activity. Basic exercises and beginner workouts that can be done at home or outdoors, whichever is better or more convenient, are recommended when starting a fitness regimen to lose weight and improve overall health. Health Benefits Basic exercise sessions are the building blocks of a fitness program. They encourage habits that lead to significant weight loss and lifelong weight management skills. Here are a few workouts considered easy because they don't require gym equipment, their intensity can be adjusted to match an individual's physical activity level, and some can be done from a chair or bed for those who have trouble standing for long periods. Exercising offers immediate benefits, including increasing brain health and improving mood and long-term effects like decreased disease risk. (Centers for Disease Control and Prevention, 2024) Easy Exercises For individuals who are completely new to exercise, low-intensity activity sessions can help burn more calories so long as they don't compensate for the hunger that the physical activity creates by eating more. Combining diet with exercise is essential if weight loss is the goal. This can involve learning to eat lean protein, fruit, and vegetables and watching portion sizes. Studies of low-intensity exercise show the body burns fat when performing basic exercise and physical activities. (Lee D. et al., 2021) Another study looked at the effect of beginner workouts on cortisol levels. Cortisol is a hormone associated with abdominal weight gain when levels stay elevated for long periods. The study found that low-intensity exercise decreased circulating cortisol levels. (Gerber M. et al., 2020) Beginner exercises to lose weight also help individuals (Vina J. et al., 2012) - Increase self-confidence
- Decrease stress levels
- Improve sleep
- Establish healthy habits
- Burn calories to stimulate weight loss and sustain weight management.
- Develop strong muscles
Basic exercise remains a core component of fitness programs for many. This includes individuals with type 2 diabetes, metabolic syndrome, and cardiovascular disease. (Apostolopoulos V. et al., 2014) Easy Workouts Types of beginner workouts include: - Bodyweight training
- Chair workouts
- Dancing workouts
- Online workouts
- Shadowboxing
- Stairclimbing
- Aqua jogging
- Biking
- Walking
- Gardening and yard work
At-Home Set short-term goals to complete three workouts during the first week, then gradually add workout days until you can perform some form of physical activity on most days. The type of exercise chosen is less important than the consistency of the program. Bodyweight Training - No special gym equipment is needed to burn calories and build stronger muscles.
- Take 10 to 15 minutes for five incline push-ups against a surface that allows the body to be at an incline, such as a countertop, bathroom sink, etc.
- Five chair squats
- Five walking lunges or stationary lunges, holding on to a countertop for support.
- Repeat the sequence two to three times.
Chair Workout - Individuals who are uncomfortable standing for long periods use a sturdy chair and complete 10 to 15 minutes of movement with a seated workout several times weekly.
Dancing - Put on music and dance for 15 to 30 minutes.
- No choreography is necessary.
- The important thing is to move to the music.
Online Workouts - Many online workouts are free, and most offer easy workouts for beginners.
Shadowboxing - Shadowboxing is easy, with no equipment required, and it helps to decrease stress.
Stairclimbing - Take 10 minutes to walk up and down a flight of steps.
- Those who don't have a staircase available can use a step or platform.
Outdoors Exercising outside provides extra perks. There are stress-relieving benefits to breathing fresh air and enjoying the outdoors. Aqua Jogging - Try pool running or aqua jogging for those with joint pain when walking for long periods.
- Floatation devices keep the upper body afloat.
- Once in the water, walk without letting your feet touch the bottom of the pool.
- If no floatation device is available, individuals can walk in the water with their feet on the pool floor.
Biking - Take a leisurely spin around the neighborhood
- Ride on a continuous path or track requiring 20 to 30 minutes of pedaling.
Walking - A 30-minute walk workout can be counted as daily exercise.
- Walk slowly for five minutes.
- Pick up the pace for 20 minutes
- Cool down and walk slowly for five minutes.
Gardening or Yard Work - Spending time in the garden or yard is a great way to work muscles and burn calories.
- Digging, weeding, raking, and mowing are all recommended activities that count as exercise for beginners.
Injury Medical Chiropractic and Functional Medicine Clinic Remember, as a beginner, the point is to get the body moving, establish a workout routine, and gradually build confidence to increase exercise enjoyment and health benefits. Workouts for beginners, especially those who still need to maintain an exercise program, are designed to develop life-long habits of well-being. At Injury Medical Chiropractic and Functional Medicine Clinic, we focus on what works for you and strive to develop fitness and better the body through research methods and total wellness programs. These natural programs use the body’s ability to achieve improvement goals, and athletes can condition themselves to excel in their sport through proper fitness and nutrition. Our providers use an integrated approach to create personalized programs, often including Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine principles. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Centers for Disease Control and Prevention. (2024). Benefits of Physical Activity. Retrieved from https://www.cdc.gov/physical-activity-basics/benefits/?CDC_AAref_Val=https://www.cdc.gov/physicalactivity/basics/pa-health/index.htm Lee, D., Son, J. Y., Ju, H. M., Won, J. H., Park, S. B., & Yang, W. H. (2021). Effects of Individualized Low-Intensity Exercise and Its Duration on Recovery Ability in Adults. Healthcare (Basel, Switzerland), 9(3), 249. https://doi.org/10.3390/healthcare9030249
Gerber, M., Imboden, C., Beck, J., Brand, S., Colledge, F., Eckert, A., Holsboer-Trachsler, E., Pühse, U., & Hatzinger, M. (2020). Effects of Aerobic Exercise on Cortisol Stress Reactivity in Response to the Trier Social Stress Test in Inpatients with Major Depressive Disorders: A Randomized Controlled Trial. Journal of Clinical Medicine, 9(5), 1419. https://doi.org/10.3390/jcm9051419 Vina, J., Sanchis-Gomar, F., Martinez-Bello, V., & Gomez-Cabrera, M. C. (2012). Exercise acts as a drug; the pharmacological benefits of exercise. British journal of pharmacology, 167(1), 1–12. https://doi.org/10.1111/j.1476-5381.2012.01970.x Apostolopoulos, V., Borkoles, E., Polman, R., & Stojanovska, L. (2014). Physical and immunological aspects of exercise in chronic diseases. Immunotherapy, 6(10), 1145–1157. https://doi.org/10.2217/imt.14.76
Fans of almonds may have noticed that they can go stale and taste awful. Can knowing how to store almonds help extend their shelf life? Almonds Almonds are a healthy, satisfying snack rich in nutrients, including fiber and protein. However, they can go stale and should not be eaten. Whole almonds stay fresh the longest because chopped, roasted, or ground almonds release their oils, which are exposed to more oxygen and go rancid more quickly. Storage They should be stored in an airtight container in the refrigerator or freezer for extended life. They are not recommended to be stored at room temperature for long periods, so storing them in the pantry is not recommended. However, enough for a snack can be taken from storage for a day or two while keeping the rest safe and fresh. Shelf-Life The shelf-life depends on how they're produced, processed, and packaged. (Almond Board of California, 2024) - Natural almonds can be stored in the refrigerator or freezer for two years or more.
- Roasted almonds can stay fresh for up to a year in an airtight container in the refrigerator or freezer.
- Almond paste is recommended to be refrigerated and can stay fresh for 2 to 2 1/2 years.
Rancidity Almonds are rich in omega-3 and monounsaturated fats, so they are recommended for heart health. (Cleveland Clinic, 2023) However, the fats become rancid if the almonds are exposed to oxygen, especially at room temperature. Rancid oil gives the stale almonds a bad taste. Spoiled almonds are not poisonous, but the fats no longer benefit health. It is possible that rancid fat could contribute to chronic health problems if consumed regularly. (Estévez M. et al., 2017) Almonds last longer than other nuts because they contain some phytochemical antioxidants that protect the nuts. So, if they taste bad, it's time to throw them out. (University of California Agriculture and Natural Resources, 2010) Salmonella Salmonella is a bacteria that causes symptoms of food-borne illness, including upset stomach, vomiting, diarrhea, and fever. Almonds are generally safe from salmonella. However, raw almonds were responsible for two salmonella outbreaks in the United States and Canada. Salmonella outbreaks have also been reported in Australia. In response to those cases, the nuts now must be roasted, blanched, processed, steamed, or treated with a gas called propylene oxide. And none of these treatments remove the nutritional benefits. Injury Medical Chiropractic and Functional Medicine Clinic Injury Medical Chiropractic and Functional Medicine Clinic providers use an integrated approach to create customized care plans for each patient and restore health and function to the body through nutrition and wellness, chiropractic adjustments, functional medicine, acupuncture, Electroacupuncture, and sports medicine protocols. If the individual needs other treatment, they will be referred to a clinic or physician best suited for them. Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, nutritionists, and health coaches to provide the most effective clinical treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Almond Board of California. (2024). Shelf Stability and Shelf Life. https://www.almonds.com/tools-and-resources/food-safety-and-quality/shelf-stability-and-shelf-life Cleveland Clinic. Clinic, C. (2023). Nutrition: Nuts & Heart Health. https://health.clevelandclinic.org/benefits-of-nuts Estévez, M., Li, Z., Soladoye, O. P., & Van-Hecke, T. (2017). Health Risks of Food Oxidation. Advances in food and nutrition research, 82, 45–81. https://doi.org/10.1016/bs.afnr.2016.12.005 University of California Agriculture and Natural Resources. (2010). Nuts: Safe Methods for Consumers to Handle, Store, and Enjoy. https://ucfoodsafety.ucdavis.edu/sites/g/files/dgvnsk7366/files/inline-files/44384_0.pdf
Can electrolyte chewing gum help physically active individuals, fitness enthusiasts, and athletes experiencing extreme heat and dehydration? Electrolyte Chewing Gum Electrolyte powder mix and drinks have been marketed as efficient and time-saving for fast-paced lives. Now, electrolytes are in chewing gum form. These gums work by activating salivary glands and making the mouth water. Manufacturers claim the gum's sour taste makes the mouth water, quenches thirst, and replenishes some electrolytes. Some brands don’t list the percentages or amounts of ingredients, making determining each gum’s electrolyte content difficult. However, electrolyte chewing gum is designed to eliminate feelings of thirst and is not meant to hydrate the body. This can be dangerous because it gives the individual a false sense of hydration. When the thirst mechanism is impaired, an individual may not drink enough fluids, leading to dehydration. The Food and Drug Administration has not studied the effectiveness of electrolyte gum. Signs The Body Is Not Getting Enough Electrolytes Electrolyte deficiency can result from insufficient fluids or excessive sweating (National Library of Medicine, 2024). Signs that the body is not getting enough electrolytes can vary because the body needs each electrolyte for specific functions. The symptoms can range from neurological symptoms such as headaches and seizures in the case of low sodium to muscle cramps and weakness when there are low potassium levels. (National Library of Medicine, 2023) (National Library of Medicine, 2023) However, individuals can still have electrolyte imbalances even if they do not have symptoms. This is why proper hydration and intake of electrolytes through water and food are important. Ingredients The ingredients listed on electrolyte chewing gum include: - Sugar
- Gum base
- Corn syrup
- Citric acid
- Glycerin
- Natural flavors
- Soy lecithin
- Artificial sweeteners
- Artificial color
- Electrolytes in sodium citrate and potassium citrate
However, gum brands fail to include the percentages of the ingredients, making it hard to figure out the actual electrolyte content. The amount can determine their effectiveness. Given their size, estimates point to very little electrolyte content, possibly around 10 milligrams of sodium per piece, which is insufficient to hydrate the body. Rehydrating the Body Food and fluids are reliable sources of electrolytes that the body can absorb. Sources include: - Fruits like bananas and oranges contain potassium and magnesium.
- Vegetables also contain potassium and magnesium.
- Dairy for calcium.
Electrolyte supplements are generally unnecessary if you eat a balanced diet. However, these products could be useful during exercise, especially for their sodium content (National Library of Medicine, 2024). When exposed to the heat, consider a rehydration solution like sports drinks or making your own. The presence of sugar increases the absorption of sodium by the intestine. Sugar in electrolyte solutions does not add calories; it helps the intestine absorb the sodium faster and holds water in the bloodstream, helping maintain blood pressure. While chewing a piece of electrolyte gum might make it easy to get balanced electrolytes, it is not enough to replenish the body. Individuals who need more electrolytes should talk to their healthcare provider about the best way to meet their body's needs. They may recommend drinks or powders specially formulated to provide an electrolyte boost. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop highly effective treatment plans through an integrated approach for each patient and restore health and function to the body through nutrition and wellness, functional medicine, acupuncture, Electroacupuncture, and integrated medicine protocols. If the individual needs other treatment, they will be referred to a clinic or physician best suited for them. Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, nutritionists, and health coaches to provide the most effective clinical treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, don't hesitate to contact Dr. Alex Jimenez or us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References National Library of Medicine, MedlinePlus. (2024). Fluid and electrolyte balance. Retrieved from https://medlineplus.gov/fluidandelectrolytebalance.html National Library of Medicine, MedlinePlus. (2023). Low blood sodium. Retrieved from https://medlineplus.gov/ency/article/000394.htm National Library of Medicine MedlinePlus. (2023). Low blood potassium. Retrieved from https://medlineplus.gov/ency/article/000479.htm
High temperatures can disrupt the body's sleep cycles, leading to health problems. Can knowing strategies and remedies help manage sleep quality? Hot Weather Sleep Sleep is important for refreshing the mind and body and being productive in school, work, relationships, and overall health. With record-breaking temperatures becoming the norm, consistently sleeping healthy is becoming difficult as forecasters predict another scorching summer with above-average temperatures. 2023 was the hottest year ever recorded. (National Oceanic and Atmospheric Administration. 2024) Studies show that high temperatures make it hard to fall asleep and stay asleep, which can negatively affect the immune system, cardiovascular system, cognitive performance, and mood. (Zheng, G., Li, K., and Wang, Y. 2019) (Obradovich, N. et al., 2017) Throughout the night, the body cycles through different sleep stages. (National Heart, Lung, and Blood Institute, 2022) Because the body’s temperature regulation is less effective during certain stages, a hot environment can cause waking so the body can thermoregulate. The right temperature is imperative for a healthy night’s sleep. For optimal sleep, it is recommended that the bedroom temperature be between 65 and 69 degrees Fahrenheit. However, this isn’t always possible without air conditioning, which increases electricity bills. Here are other strategies to help keep the body cool for better sleep in hot weather. Cooler Sleeping Environment Thinking creatively about sleeping arrangements can help. Try to find the place that is the coolest and has the most airflow. Shutters or curtains during the day can help keep the room dark and cooler, and opening the windows can increase airflow. (Fergus Nicol, 2019) Using a fan can help improve air circulation, and putting ice behind the fan can blow cooler air for improved sleep. Cooling Pillows and Breathable Pajamas Pajamas and bedding made from breathable fabrics can help keep the body cool, and cooling mattress toppers or pillows can also help. Cooling pillows have gel overlays that absorb body heat and cool the head and neck. Keep an ice pack on the bedside table and a towel and ice to keep the body cool. Take a Slightly Warm Shower Taking a cold shower can cool the body down quickly, but studies have shown that showering in warm water before bed can make it easier to fall asleep. (Tai, Y. et al., 2021) The warm shower signals the body into cooling mode, which can help promote sleep as the body temperature falls at night. However, the water shouldn’t be too warm, which could exacerbate sweating. Sleep Hygiene It can be difficult to create the perfect sleep environment in hot weather. A healthy going-to-bed routine is essential in the summer, as stress and anxiety can significantly affect sleep quality. Avoid eating close to bedtime, avoid alcohol, and add some time to relax and unwind before going to bed. Sleep experts suggest general sleep hygiene habits like keeping a consistent bedtime and turning off screens an hour before bed can help improve sleep, even in hot weather. (Baranwal, N., Yu, P. K., and Siegel, N. S. 2023) Chiropractic Treatment Chiropractic care, massage, and decompression therapy can help improve sleep. Treatment retrains the body to relax; stretching and pulling the muscles increases blood circulation and advanced and improved brain signals telling the body to relax. A chiropractor will evaluate the individual's sleeping patterns and recommend various strategies. Benefits include: - Muscle tension relief.
- Stimulates nerve and blood circulation.
- Relaxes the whole body.
- Enhances central nervous system function.
- Relieves pain and discomfort.
- A chiropractor will also provide:
- Sleeping position recommendations.
- Postural stretches and exercises.
- Recommendations on supportive mattresses.
- Ergonomics for work, home, and bed.
Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution through an integrated approach to treating injuries and chronic pain syndromes, improving flexibility, mobility, and agility programs to relieve pain and help individuals return to normal. Our providers create personalized plans for each patient. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References National Oceanic and Atmospheric Administration. (2024). April 2024 was Earth’s warmest on record. Retrieved from https://www.noaa.gov/news/april-2024-was-earths-warmest-on-record Zheng, G., Li, K., & Wang, Y. (2019). The Effects of High-Temperature Weather on Human Sleep Quality and Appetite. International journal of environmental research and public health, 16(2), 270. https://doi.org/10.3390/ijerph16020270 Obradovich, N., Migliorini, R., Mednick, S. C., & Fowler, J. H. (2017). Nighttime temperature and human sleep loss in a changing climate. Science advances, 3(5), e1601555. https://doi.org/10.1126/sciadv.1601555 National Heart, Lung, and Blood Institute. (2022). Sleep phases and stages. Retrieved from https://www.nhlbi.nih.gov/health/sleep/stages-of-sleep Nicol F. (2019). Temperature and sleep. Energy and Buildings, 204. https://doi.org/https://doi.org/10.1016/j.enbuild.2019.109516. Tai, Y., Obayashi, K., Yamagami, Y., Yoshimoto, K., Kurumatani, N., Nishio, K., & Saeki, K. (2021). Hot-water bathing before bedtime and shorter sleep onset latency are accompanied by a higher distal-proximal skin temperature gradient in older adults. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 17(6), 1257–1266. https://doi.org/10.5664/jcsm.9180 Baranwal, N., Yu, P. K., & Siegel, N. S. (2023). Sleep physiology, pathophysiology, and sleep hygiene. Progress in cardiovascular diseases, 77, 59–69. https://doi.org/10.1016/j.pcad.2023.02.005
For individuals who are getting older, can increasing bone strength help prevent fractures and optimize bone health? Bone Strength Bone strength is important, as a fractured hip can be serious for older individuals. A study found that for individuals in their 60s who had a hip fracture, 6.5% of women and 9.4% of men died within a year. Among individuals in their 80s, 13.1% of women and 19.6% of men died within a year. (Dimet-Wiley, et al., 2022) Increasing bone strength can help prevent various issues. A small increase in bone mineral density has been shown to help reduce the risk of fractures, especially hip fractures. A decades-long study found that just a 3% increase in bone strength helps lower the chance of breaking a hip. Researchers enrolled two groups of individuals aged 60 and older, one in 1989 and the second in 1999. - The bone mineral density of each subject’s femoral neck joint at the top of the thigh bone near the hip was measured.
- They then followed the subjects for years to see who experienced hip fractures.
- While the bone mineral density of the second group was only 3% higher than the first group, these subjects experienced a 46% reduction in hip fractures. (Tran, T. et al., 2023)
Bone Loss Bone loss is progressive in men and women and increases as the body ages. Osteoporosis is a condition in which bone tissue deteriorates. (Department of Health and Human Services Office of Disease Prevention and Health Promotion. 2020) Bones constantly break down and reform as a normal remodeling process. If the balance of this process is impaired, osteoporosis develops, resulting in more bone breakdown than formation. While men and women experience bone loss, it’s more common in females. (National Institute of Arthritis and Musculoskeletal Diseases. 2022) Menopause is a risk factor because of the decline of estrogen (National Library of Medicine, Medline Plus, 2022). Estrogen reinforces bone strength by protecting against bone breakdown; with estrogen loss, bone breakdown increases. However, anyone of any age or background can experience bone loss due to the following: - Endocrine disorders.
- Gastrointestinal diseases.
- Inflammatory diseases like rheumatoid arthritis.
- Certain cancers.
- Medication taken to treat these conditions, like steroids or oncology meds, can also accelerate bone loss. (National Library of Medicine. Medline Plus, 2022)
Exercise While some loss of bone strength is common, several strategies exist to maintain bone health. Exercise, specifically weight-bearing activities, can increase bone strength. When bones and muscles are used to hold a position against gravity, this mechanically stresses the bone, causing it to reform stronger. Movement and physical exercise as medicine and the forces transmitted through the bones generate mechanical signals that tell the cells to increase bone formation relative to breakdown. Exercises focusing on posture, balance, gait, and coordination are recommended for individuals with osteoporosis to strengthen the core, quadriceps, and hip flexors. Different types of exercises can include: - Walking to strengthen the spine and hips.
- Walking outside or on a treadmill provides more loading force to the bone.
- Planks and push-ups can strengthen the forearm and wrist bones.
- Holding a water bottle in each hand and lifting up and down 10 times together or alternating a few times a day.
- Side leg lifts can strengthen the hip and forearm bones simultaneously.
- Weight training provides the bones with a workout by having them support a weight load.
- Any exercise therapy program should be designed by a healthcare provider, physical therapist, and trainer according to the individual's condition and appropriate for them.
Diet What goes into the body definitely affects bone health. Calcium and vitamin D are key to bone building, but both are needed as vitamin D is needed to absorb the calcium ingested. Calcium can be found in: - Dairy
- Dairy products and non-dairy alternatives are fortified with calcium.
- Leafy greens.
- Beans.
- Almonds.
- The recommended daily calcium intake for adults over 50 is 1,200 milligrams.
Vitamin D can come from: - Sunlight
- Fish.
- Mushrooms.
- Fortified milk.
- Supplements.
- The recommended daily vitamin D intake for adults aged 70 is 15 micrograms and 20 micrograms for individuals over 70.
Studies have found that increasing calcium and vitamin D intake with supplements can help maintain bone health. Talk to a healthcare provider about whether supplements could be beneficial. Hormone Therapy Females also naturally produce testosterone, which promotes bone formation. As levels drop with age and negatively impact bone strength, hormone therapy could be recommended. Declining testosterone levels start with women in their 20s and men in their 30s. The typical drop in women is 1% to 3% yearly before menopause and stabilizes somewhat afterward. Female patients at risk of bone loss may be prescribed testosterone in various forms that continuously emit the hormone. The dosage is low, so patients do not experience unwanted hair growth or skin changes. Combined with estrogen, testosterone effectively increases bone growth in female patients. Not everyone is a candidate for hormone therapy, like individuals with a history of breast cancer, heart disease, blood clots, or liver disease. (National Library of Medicine. Medline Plus, 2019) Making small adjustments can optimize bone health and overall well-being At Injury Medical Chiropractic and Functional Medicine Clinic, we passionately focus on treating patients’ injuries and chronic pain syndromes to create personalized care plans that improve ability through flexibility, mobility, and agility programs tailored to the individual. Using an integrated approach, our goal is to relieve pain naturally by restoring health and function to the body through Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine protocols. If the individual needs other treatment, they will be referred to a clinic or physician best suited for them, as Dr. Jimenez has teamed up with the top surgeons, clinical specialists, medical researchers, and premier rehabilitation providers to provide the most effective clinical treatments. We focus on what works for you and strive to better the body through researched methods and total wellness programs. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Dimet-Wiley, A., Golovko, G., & Watowich, S. J. (2022). One-Year Postfracture Mortality Rate in Older Adults With Hip Fractures Relative to Other Lower Extremity Fractures: Retrospective Cohort Study. JMIR aging, 5(1), e32683. https://doi.org/10.2196/32683 Tran, T. S., Ho-Le, T. P., Bliuc, D., Center, J. R., Blank, R. D., & Nguyen, T. V. (2023). Prevention of Hip Fractures: Trade-off between Minor Benefits to Individuals and Large Benefits to the Community. Journal of bone and mineral research: the official journal of the American Society for Bone and Mineral Research, 38(11), 1594–1602. https://doi.org/10.1002/jbmr.4907 Department of Health and Human Services Office of Disease Prevention and Health Promotion. (2020). Osteoporosis Workgroup. Retrieved from https://health.gov/healthypeople/about/workgroups/osteoporosis-workgroup National Institute of Arthritis and Musculoskeletal Diseases. (2022). Osteoporosis. Retrieved from https://www.niams.nih.gov/health-topics/osteoporosis National Library of Medicine. MedlinePlus. (2022). What causes bone loss? Retrieved from https://medlineplus.gov/ency/patientinstructions/000506.htm National Library of Medicine. MedlinePlus. (2019). Hormone replacement therapy. Retrieved from https://medlineplus.gov/hormonereplacementtherapy.html
For individuals dealing with eczema, can incorporating acupuncture into a treatment plan help manage and reduce symptoms? Acupuncture for Eczema Eczema is a chronic skin disorder that causes intense itching, dry skin, and rashes. Common treatment options for eczema include: - Moisturizers
- Topical steroids
- Prescription medications
Some research suggests that acupuncture may also help individuals with eczema. In recent years, researchers have looked at acupuncture as a possible treatment option and found that it can reduce symptoms. Acupuncture Acupuncture involves inserting thin metallic needles in specific acupoints in the body. It is believed that by stimulating specific points, the body’s central nervous system activates and releases certain chemicals designed to enable healing. Ailments that are treated using acupuncture include: (Johns Hopkins Medicine. 2024) - Headaches
- Back pain
- Nausea
- Asthma
- Osteoarthritis
- Fibromyalgia
Treatment Studies have found that acupuncture could be a treatment option depending on the severity of the condition and the intensity of the itching sensations. (Ruimin Jiao et al., 2020) The needles are placed at various points associated with relieving the condition. These points include: (Zhiwen Zeng et al., 2021) LI4 - Located at the base of the thumb and index finger.
- It has been shown to help reduce inflammation and irritation.
LI11 - This point is located within the elbow to reduce itchiness and dryness.
LV3 - Located on the top of the foot, this point reduces stress on the nervous system.
SP6 - The SP6 is on the lower calf above the ankle and can help reduce inflammation, redness, and skin irritation.
SP10 - This point is located adjacent to the knee and reduces itchiness and inflammation.
ST36 - This point is located below the knee on the back of the leg and is used to improve overall well-being.
Benefits There are various benefits of acupuncture, including (Ruimin Jiao et al., 2020) - Dryness and itchiness relief.
- Itchiness intensity reduction.
- Affected area reduction.
- Improved quality of life.
- Eczema flare-ups are also linked to stress and anxiety. Acupuncture has been shown to reduce anxiety and stress, which can also help relieve eczema symptoms (Beate Wild et al., 2020).
- Acupuncture helps repair skin barrier damage or the outer part of the skin designed to protect the body. (Rezan Akpinar, Saliha Karatay, 2018)
- Individuals with eczema tend to have a weakened skin barrier; this benefit can also improve symptoms. (National Eczema Association. 2023)
- Individuals with eczema often have an overactive immune system contributing to the disorder.
- According to research, acupuncture can also help in regulating the immune system. (Zhiwen Zeng et al., 2021)
Risks Acupuncture is generally considered safe, but there are some risks to be aware of. These risks include: (Ruimin Jiao et al., 2020) - Swelling where the needles are inserted.
- Red spots on the skin.
- Increased itchiness.
- A rash known as erythema - occurs when small blood vessels are injured.
- Hemorrhages - excessive bleeding.
- Fainting
Individuals Who Should Avoid Acupuncture Not all individuals can be treated with acupuncture. Individuals who should avoid acupuncture treatment include individuals who (National Eczema Association. 2021) (Johns Hopkins Medicine. 2024) - Are pregnant
- Have a bleeding disorder
- Have an increased risk of infection
- Have a pacemaker
- Have breast implants
Effectiveness Most studies on acupuncture for eczema show positive results that prove it can aid in relieving symptoms. (SeHyun Kang et al., 2018) (Ruimin Jiao et al., 2020) However, individuals should talk to their healthcare provider to see if it's a safe option. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Johns Hopkins Medicine. (2024). Acupuncture (Health, Issue. https://www.hopkinsmedicine.org/health/wellness-and-prevention/acupuncture Jiao, R., Yang, Z., Wang, Y., Zhou, J., Zeng, Y., & Liu, Z. (2020). The effectiveness and safety of acupuncture for patients with atopic eczema: a systematic review and meta-analysis. Acupuncture in medicine: journal of the British Medical Acupuncture Society, 38(1), 3–14. https://doi.org/10.1177/0964528419871058 Zeng, Z., Li, M., Zeng, Y., Zhang, J., Zhao, Y., Lin, Y., Qiu, R., Zhang, D. S., & Shang, H. C. (2021). Potential Acupoint Prescriptions and Outcome Reporting for Acupuncture in Atopic Eczema: A Scoping Review. Evidence-based complementary and alternative medicine: eCAM, 2021, 9994824. https://doi.org/10.1155/2021/9994824 Wild, B., Brenner, J., Joos, S., Samstag, Y., Buckert, M., & Valentini, J. (2020). Acupuncture in persons with an increased stress level-Results from a randomized-controlled pilot trial. PloS one, 15(7), e0236004. https://doi.org/10.1371/journal.pone.0236004 Akpinar R, Karatay S. (2018). Positive Effects of Acupuncture on Atopic Dermatitis. International Journal of Allergy Medications 4:030. doi.org/10.23937/2572-3308.1510030 National Eczema Association. (2023). Skin barrier basics for people with eczema. What is my skin barrier? https://nationaleczema.org/blog/what-is-my-skin-barrier/ National Eczema Association. (2021). Get the facts: acupuncture. Get the facts: acupuncture. https://nationaleczema.org/blog/get-the-facts-acupuncture/ Kang, S., Kim, Y. K., Yeom, M., Lee, H., Jang, H., Park, H. J., & Kim, K. (2018). Acupuncture improves symptoms in patients with mild-to-moderate atopic dermatitis: A randomized, sham-controlled preliminary trial. Complementary therapies in medicine, 41, 90–98. https://doi.org/10.1016/j.ctim.2018.08.013
|
Introduction: The Silent Damage of MVAs A motor vehicle accident (MVA) can change a person's life in an instant. While visible injuries like cuts and bruises are easy to spot, many people walk away from accidents unaware that deeper musculoskeletal injuries have occurred. Musculoskeletal injuries affect muscles, bones, joints, ligaments, tendons, and nerves. These injuries may not show symptoms right away, but can cause serious problems over time. Pain, stiffness, reduced mobility, and long-term damage are just some of the outcomes if left untreated. A common question many people ask after an accident is: "Will I recover fully, and how long will it take?" The answer depends on the injury type, severity, and treatment plan. Chiropractic care has become a trusted, non-invasive approach for treating these hidden injuries and helping people return to their everyday lives. (Advantage Healthcare Systems, n.d.; Aguiar Injury Lawyers, n.d.) Understanding Musculoskeletal Injuries After a Car Accident When the body is suddenly jolted during a collision, it experiences forces beyond normal limits. Even in minor fender-benders, the body can be thrown forward and backward quickly. This whiplash motion often injures soft tissues like muscles and ligaments in the neck, back, and shoulders. Additionally, joints can be pushed out of alignment, and discs between vertebrae can be damaged. Musculoskeletal injuries may include: These injuries can affect daily functioning, including walking, working, sleeping, and participating in hobbies or sports. Without proper treatment, musculoskeletal injuries can lead to chronic pain, arthritis, and mobility issues. (Florida Physical Medicine, n.d.; Tortslaw, n.d.) The Recovery Timeline: Will It Be Full, and How Long Will It Take? Recovery time depends on several factors: -
The type and location of the injury -
The severity of tissue damage -
The timeliness of seeking treatment -
The overall health and age of the person Some people recover in a few weeks with minimal care, while others may need months of therapy. The goal of treatment is not just to relieve pain but also to restore mobility, prevent future problems, and improve quality of life. According to Dr. Alexander Jimenez, DC, APRN, FNP-BC, a dual-licensed chiropractor and nurse practitioner in El Paso, the most accurate recovery predictions come from dual-scope diagnosis, which includes orthopedic exams, neurological assessments, and advanced imaging. By combining chiropractic insight with medical knowledge, providers like Dr. Jimenez can create a personalized recovery roadmap. (JS Berry Law, n.d.; Lonseth Pain, n.d.; Jimenez, n.d.) Chiropractic Care: A Non-Invasive, Whole-Body Approach Chiropractors specialize in diagnosing and treating neuromusculoskeletal problems. After an accident, they examine the spine, joints, muscles, and nerves for signs of misalignment, inflammation, and nerve compression. Through manual spinal adjustments, chiropractors help realign joints and reduce pressure on nerves. This process can: -
Improve blood flow -
Enhance nerve function -
Reduce inflammation -
Promote natural healing Unlike medications that only mask symptoms, chiropractic care aims to correct the root cause of pain and dysfunction. Techniques may include spinal adjustments, soft tissue therapy, therapeutic stretching, and lifestyle counseling. (Tradition Health, 2024; Uptown Denver Chiropractor, n.d.) The Role of Chiropractic Adjustments in Post-Accident Care One of the most important tools in chiropractic care is the spinal adjustment. When joints are misaligned due to trauma, they can press on nerves and restrict movement. A chiropractor uses controlled force to reposition the joint, relieving pressure and restoring balance to the body. Adjustments are especially helpful for treating: -
Neck and back pain -
Headaches -
Whiplash symptoms -
Limited range of motion Dr. Jimenez explains that spinal realignment can reduce pain without the side effects of medication. It also improves coordination between the brain and the body by restoring healthy nerve communication. (Hogan Chiropractic, 2024; Clearway Pain, n.d.) Soft Tissue Therapy and Inflammation Reduction Injuries often trigger inflammation, which causes swelling, heat, pain, and stiffness. While inflammation is a natural part of healing, chronic inflammation can damage tissues and prolong recovery. Chiropractors use techniques such as myofascial release, trigger point therapy, and instrument-assisted soft tissue mobilization to reduce inflammation and break up scar tissue. These therapies improve: -
Muscle flexibility -
Circulation -
Joint range of motion -
Overall healing time Reducing inflammation also helps patients return to daily activities faster and with less discomfort. (Brookdale Health, n.d.; Artisan Chiropractic Clinic, n.d.) Restoring Mobility and Preventing Long-Term Complications In the aftermath of an MVA, patients often experience stiffness, reduced mobility, and muscle guarding (a protective tightening of muscles). If untreated, these symptoms can lead to muscle atrophy, joint degeneration, or even permanent disability. Chiropractic care includes guided rehabilitation exercises and postural correction strategies to restore normal movement. These therapies reduce the chance of long-term complications like: -
Chronic pain -
Spinal disc degeneration -
Poor posture -
Functional limitations Dr. Jimenez emphasizes combining chiropractic adjustments with rehabilitative exercises tailored to each patient’s injury and lifestyle to ensure sustainable improvement. (The Neck and Back Clinics, n.d.; Wirth Chiropractic, n.d.) Dual-Scope Diagnosis: Medical and Chiropractic Integration What sets providers like Dr. Jimenez apart is their ability to perform a dual-scope assessment. As both a nurse practitioner and chiropractor, he understands how to: -
Order diagnostic imaging like MRIs and CT scans -
Interpret neurological and orthopedic findings -
Document injuries for legal and insurance purposes -
Coordinate referrals to physical therapists, orthopedic surgeons, or pain management specialists when needed This comprehensive approach streamlines care and ensures that patients receive both therapeutic treatment and appropriate medical documentation. Through his clinics in El Paso, Dr. Jimenez uses this model to help injured individuals heal physically while also supporting their legal cases with detailed reports, diagnostic codes, and insurance-compliant records. (Jimenez, n.d.; Personal Injury Doctor Group, n.d.) Chiropractic Care and the Legal-Medical Connection After an MVA, patients often need legal assistance to receive compensation for their injuries. Chiropractors like Dr. Jimenez play a crucial role in this process by: -
Documenting the timeline and severity of injuries -
Recording treatment progress and outcomes -
Providing expert testimony when needed These detailed medical records support personal injury claims, demonstrating the connection between the accident and the resulting injuries. When chiropractic care is initiated early, the documentation is more accurate and timely, leading to better outcomes both medically and legally. (Advantage Healthcare Systems, n.d.; Aguiar Injury Lawyers, n.d.) Whole-Person Healing Through Integrative Medicine Many chiropractic clinics now offer integrative care, combining: -
Chiropractic adjustments -
Acupuncture -
Functional medicine -
Nutritional counseling -
Lifestyle changes This approach recognizes that healing goes beyond pain relief. It addresses inflammation, stress, sleep quality, and gut health, all of which can be impacted by trauma. Integrative treatments are especially helpful in restoring emotional well-being, which often suffers after an accident. Dr. Jimenez integrates functional assessments and supportive therapies to help patients not only recover from physical trauma but also regain their overall wellness. (Recovery Chiro Med, n.d.; Jimenez, n.d.) Conclusion: Chiropractic Care as a Trusted Partner in Recovery Musculoskeletal injuries from motor vehicle accidents can range from mild strains to serious disc and nerve damage. They affect not only the body but also daily activities, work, mental health, and financial well-being. Chiropractic care offers a safe, drug-free path to recovery by addressing the root causes of pain, improving joint and nerve function, and supporting long-term healing. With advanced diagnostics and dual-scope assessment, providers like Dr. Alexander Jimenez help patients get back on their feet while also guiding them through the complex legal and insurance landscape. By choosing chiropractic care, accident survivors can trust they are receiving thorough, personalized treatment that promotes total-body wellness and protects their future. Personal Injury Rehabilitation References Advantage Healthcare Systems. (n.d.). The questions you should always ask a doctor after a car crash. https://www.advantagehcs.com/the-questions-you-should-always-ask-a-doctor-after-a-car-crash/ Aguiar Injury Lawyers. (n.d.). Most common car accident injuries in Louisville. https://aguiarinjurylawyers.com/most-common-car-accident-injuries-in-louisville/ Artisan Chiropractic Clinic. (n.d.). The comprehensive guide to chiropractic care for car accident survivors. https://www.artisanchiroclinic.com/the-comprehensive-guide-to-chiropractic-care-for-car-accident-survivors/ Brookdale Health. (n.d.). Why chiropractic care is essential after a car accident. https://www.brookdalehealth.com/blog/why-chiropractic-care-is-essential-after-a-car-accident.html Clearway Pain. (n.d.). Should I get a chiropractic adjustment after my car accident? https://clearwaypain.com/should-i-get-a-chiropractic-adjustment-after-my-car-accident/ Florida Physical Medicine. (n.d.). Musculoskeletal injuries. https://floridaphysicalmedicine.com/musculoskeletal-injuries/ Hogan Chiropractic. (2024, October 31). See a chiropractor after auto accident. https://hoganchiropractic.com/2024/10/31/see-chiropractor-after-auto-accident/ Jimenez, A. [Dr. Alexander Jimenez]. (n.d.). Injury diagnosis and treatment after auto accidents. https://www.dralexjimenez.com/ Jimenez, A. [Dr. Alexander Jimenez]. (n.d.). Legal-medical integration in personal injury. https://www.personalinjurydoctorgroup.com/ Jimenez, A. [Dr. Alexander Jimenez]. (n.d.). LinkedIn profile. https://www.linkedin.com/in/dralexjimenez/ JS Berry Law. (n.d.). Long-term effects of whiplash. https://jsberrylaw.com/long-term-effects-of-whiplash/ Lonseth Pain & Spine. (n.d.). Minimally invasive treatments after car accidents. https://www.lonsethpain.com/news/minimally-invasive-treatments-car-accidents/ Personal Injury Doctor Group. (n.d.). Chiropractic-medical support for auto accident injuries. https://www.personalinjurydoctorgroup.com/ Recovery Chiro Med. (n.d.). Healing from car accidents: The impact of chiropractic care on auto injuries. https://recoverychiromed.com/healing-from-car-accidents-the-impact-of-chiropractic-care-on-auto-injuries/ The Neck and Back Clinics. (n.d.). Long-term recovery. https://theneckandbackclinics.com/long-term-recovery/ Tortslaw. (n.d.). Long-term effects of whiplash. https://www.tortslaw.com/car-accident-lawyers/injuries/whiplash/long-term-effects/ Tradition Health. (2024, November 26). Chiropractic care for auto accident injuries. https://traditionhealth.com/2024/11/26/chiropractic-care-for-autoaccident-injuries/ Uptown Denver Chiropractor. (n.d.). How chiropractic care helps auto accident injury victims. https://uptowndenverchiropractor.com/blog/how-chiropractic-care-helps-auto-accident-injury-victims Wirth Chiropractic. (n.d.). What is the value of using a chiropractor after an accident? https://www.wirthchiropractic.com/accident-injury/what-is-the-value-of-using-a-chiropractor-after-an-accident/ General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, and physical medicine, as well as wellness, sensitive health issues, and functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and the jurisdiction in which they are licensed to practice. We utilize functional health and wellness protocols to treat and support care for injuries or disorders affecting the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice. Our office has made a reasonable attempt to provide supportive citations and identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, please contact Dr. Alex Jimenez or us at 915-50-0900. Dr. Alex Jimenez, DC, MSACP, CCST, IFMCP*, CIFM*, ATN* Email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Why do the muscles retighten days or weeks later for individuals who have received massage or chiropractic adjustments? Muscles Retighten Muscles can retighten again days or weeks after chiropractic treatment and/or a massage. A few factors may cause this. - Muscle memory: The body's natural tendency to return to its previous state of tension.
- This includes all the unhealthy postures/positioning
- Delayed inflammatory response.
- The body's natural healing process
- How muscles respond to manipulation
- The need for ongoing maintenance of muscle health
After a massage, muscles can experience a temporary increase in soreness or tightness as the body heals from any minor damage or inflammation caused by the massage. Additionally, if the underlying issue causing muscle tightness is not addressed, the muscles may revert to their original state over time. (Cleveland Clinic, 2024) Causes Causes for muscles to retighten. Underlying Issues - If the root cause of the muscle tightness is not addressed, such as unhealthy posture, injuries, repetitive motions, or muscle imbalances, it can lead to further complications.
- In that case, the muscles may return to their original state after a few days or weeks.
Delayed Onset Muscle Soreness (DOMS) - For example, muscles feel sore after intense exercise, and individuals can also experience DOMS after a massage, especially if they are particularly tight or if it's been a while since their last massage. (Healthline, 2020)
Delayed Inflammatory Response - Massage can sometimes cause microscopic tears or inflammation in muscle tissue, which triggers the body's natural healing process.
- This response can cause soreness and temporary tightness, as the body repairs the damaged tissue even after the initial massage. (Essential Chiropractic, 2025)
Muscle Memory - The body tends to revert to habitual patterns of muscle tension, especially if the underlying cause of the tightness isn't addressed.
- Muscles can retain how they were manipulated during the massage and may revert to their original tightness if they haven't been consistently relaxed.
Muscle Guarding - The individual and body can subconsciously tense muscles to avoid pain or soreness, even after the massage.
- This muscle guarding can counteract the benefits of the massage and lead to a renewed cycle of tension. (Bhimani R. H., & Soomar D. 2019)
Muscle Health Maintenance - Regular Maintenance
- Muscles need consistent care to maintain their optimal state of health and function.
- Regular massages and other lifestyle changes, such as stretching and strengthening exercises, can help maintain muscle flexibility and reduce the likelihood of muscle tightness returning.
Individual Variation - Factors like the type of massage received, the frequency of massages, and individual body responses can all influence how long a massage's benefits last. (Cleveland Clinic, 2024)
Massage Treatment Muscles can retighten after a massage due to the body's response to the pressure and manipulation during the treatment. This can include individual sensitivity to massage, the type of massage, and hydration levels, which can also play a role. Type of Massage - Deep tissue massage, which focuses on specific muscle groups and applies deeper pressure, may cause more soreness than other types of massage.
- Some individuals may be more sensitive to massage and experience soreness, even with a gentle massage. (Cleveland Clinic, 2024)
Muscle Fiber Manipulation - Deep tissue massage can break down spasms or microtears in muscle fibers, leading to soreness.
- This is similar to the microscopic tears that occur during exercise, which are necessary for muscle repair and growth.
Dehydration - Individuals who are not adequately hydrated may experience increased soreness after a massage. (Cleveland Clinic, 2024)
Lactic Acid Buildup - During an intense massage, particularly deep tissue, lactic acid can build up in the muscles, leading to soreness and tightness.
- (Healthline, 2020)
Muscle Tensions - If the muscles were particularly tense or knotted before the massage, the manipulation could lead to soreness as the knots get worked out.
Injury Medical Chiropractic and Functional Medicine Clinic As a Family Practice Nurse Practitioner, Dr. Jimenez combines advanced medical expertise with chiropractic care to address various conditions. Our clinic integrates Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine to create customized care plans that promote natural healing, mobility, and long-term wellness. By focusing on flexibility, agility, and strength, we empower patients to thrive, regardless of age or health challenges. At El Paso’s Chiropractic Rehabilitation Clinic & Integrated Medicine Center, we passionately focus on treating patients after injuries and chronic pain syndromes. We focus on improving your ability through flexibility, mobility, and agility programs tailored for all age groups and disabilities. We use in-person and virtual health coaching and comprehensive care plans to ensure every patient’s personalized care and wellness outcomes. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, and physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice. Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, don't hesitate to contact Dr. Alex Jimenez or us at 915-50-0900. Dr Alex Jimenez, DC, MSACP, CCST, IFMCP*, CIFM*, ATN* Email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Cleveland Clinic. (2024). How to Relieve Muscle Soreness After a Massage. https://health.clevelandclinic.org/why-does-my-body-feel-worse-after-a-massage Healthline. (2020). How to Relieve Sore Muscles After a Massage. https://www.healthline.com/health/sore-after-massage#causes-of-soreness Essential Chiropractic and Physiotherapy. (2025). Muscle Ache After Massage: Common Causes and Relief. https://essentialchiropractic.co.uk/muscle-ache-after-massage-common-causes-and-relief/#:~:text=Post%2Dmassage%20soreness%20is%20a,hours%20as%20the%20muscles%20recover. Bhimani, R. H., & Soomar, D. (2019). Understanding Symptoms of Muscle Tightness, Weakness, and Rigidity From a Nursing Perspective. Rehabilitation Nursing: The Official Journal of the Association of Rehabilitation Nurses, 44(5), 271–281. https://doi.org/10.1097/rnj.0000000000000151
For individuals experiencing musculoskeletal pain symptoms like lower back pain and shoulder pain, can incorporating cupping therapy help bring relief and manage pain? Cupping Therapy This ancient treatment is gaining public acceptance, and awareness has heightened, with various individuals and athletes being seen with round marks on their shoulders and backs. It is a pain treatment that, like acupuncture, comes from traditional Chinese medicine, or TCM. The therapy involves placing glass, silicone, or bamboo cups on the skin to create suction. The treatment is an alternative medicine technique used to relieve musculoskeletal pain. The suction is believed to promote healing (Cleveland Clinic, 2023) Increasing Blood Circulation - The suction draws blood to the area, which can help reduce inflammation and promote healing.
Releasing Muscle Tension - The suction can stretch and pull on muscles, which can help relieve pain and tightness.
Breaking Up Adhesions - The suction can help break up scar tissue and adhesions that can cause pain and restricted movement.
Detoxifying the Body - Some practitioners believe that cupping can help remove toxins from the body.
It is typically performed by a trained practitioner who places the cups on the skin and leaves them in place for several minutes. The cups can be placed on various body areas, including the back, neck, shoulders, and legs. (Cleveland Clinic, 2023) Benefits - Pain relief, especially for muscle and joint pain
- Reduced inflammation
- Improved circulation
- Increased range of motion
- Detoxification
Procedure The medical practice involves creating skin suction using glass, ceramic, or plastic cups. How it's done: Preparation - The practitioner cleans the area where the cups will be placed.
- They may apply oil or massage cream to the skin for easier movement of the cups.
Techniques Dry - The practitioner heats the inside of the cup with a flame or pump, creating a vacuum.
- The cup is then placed on the skin, which adheres due to the negative pressure.
- The cup remains on the skin for several minutes, allowing the suction to draw blood and tissue into the cup.
Wet - Like the dry technique, the practitioner makes small incisions in the skin before applying the cup.
- This allows blood to flow into the cup, creating a more intense suction.
Aftercare - The cups are removed, and the practitioner may apply pressure to the area to stop bleeding.
- The patient is advised to avoid strenuous activity and hot showers for a few hours after the treatment.
The benefits of therapy include opening pores, stimulating blood flow, filtration, and balancing energy flow through the body. It's often combined with massage and acupuncture. (Cleveland Clinic, 2023) It also aims to alleviate symptoms of systematic diseases like diabetes and hypertension. However, more research is needed to see and fully analyze the effects of the treatment. (Aboushanab T. S., & AlSanad S. 2018) Risks The therapy is generally safe when done correctly and by a licensed professional. However, there is some risk of side effects like skin discoloration and scarring. Reports of rare side effects include bleeding inside the skull from cupping on the scalp and anemia from repeated wet techniques. (National Center for Complementary and Integrative Health, 2018) Other side effects can include: Bruising - It can cause temporary bruising at the site of the cups.
Skin Irritation - Some people may experience skin irritation or burns from the suction.
Infection - There is a small risk of infection if the cups are not properly sterilized.
Who should avoid the therapy? Those with skin conditions like eczema and psoriasis should avoid cupping, as it may worsen them. (National Center for Complementary and Integrative Health, 2018) Injury Medical Chiropractic & Functional Medicine Clinic It is important to consult with a healthcare professional before trying any new treatment, especially if you have any underlying health conditions. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice. Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol. To discuss the subject matter above further, please contact Dr. Alex Jimenez or us at 915-50-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Cleveland Clinic. (2023). Cupping Therapy. https://my.clevelandclinic.org/health/treatments/16554-cupping Aboushanab, T. S., & AlSanad, S. (2018). Cupping Therapy: An Overview from a Modern Medicine Perspective. Journal of acupuncture and meridian studies, 11(3), 83–87. https://doi.org/10.1016/j.jams.2018.02.001 National Center for Complementary and Integrative Health. (2018). Cupping. Retrieved from https://www.nccih.nih.gov/health/cupping
For individuals experiencing periodic limb movements of sleep, can understanding how movements at night may relate to other sleep disorders help bring healthy sleep? Periodic Limb Movements of Sleep Periodic limb movements of sleep (PLMS) are involuntary, repetitive leg and sometimes arm movements during sleep. PLMS is one of the sleep disorders that may cause disruptive movement of the legs, like restless legs syndrome (RLS). It can lead to sleep disruption, insomnia, and daytime sleepiness. Causes The exact cause of PLMS is unknown, but it is thought to be related to: - Underlying medical conditions (e.g., restless legs syndrome, sleep apnea)
- Nerve dysfunction
- Neurochemical imbalances (e.g., dopamine, iron)
Symptoms - Repetitive leg and/or arm movements during sleep, typically lasting 0.5-5 seconds.
- It may be accompanied by sensations of tingling, crawling, or pulling in the legs.
- It can cause sleep disturbances, leading to daytime fatigue.
Type of Movements Periodic limb movements during sleep (PLMS) consist of sudden jerking movements of the legs that occur involuntarily during sleep, which the affected individual may not realize is happening. It can be kicking, twitching, or extension of the legs. - Restless legs syndrome (RLS) symptoms are noted when awake.
- PLMS occurs during sleep. (Walters A. S., & Rye D. B. 2009)
- The movements associated often consist of flexion or extension at the ankle.
- In some cases, this can also occur at the knee.
- It may occur on one side or alternate back and forth between the left and right sides. (Cleveland Clinic, 2023)
- It tends to increase with age and often but is not always accompanied by restless leg symptoms.
If PLMS causes daytime impairment, such as significant sleep disruption, excessive daytime sleepiness, and insomnia, it may be diagnosed as periodic limb movement disorder (PLMD). (Sleep Foundation, 2024) Diagnosis PLMS is diagnosed through a sleep study (polysomnography), which records brain waves, eye movements, muscle activity, and breathing patterns during sleep. As part of the study, superficial electrodes are placed on the legs and sometimes the arms to detect muscle contractions or movements. - In individuals with PLMS, repetitive movements at least four in a row may last from 1/2 second to 5 seconds.
- The movements may be more significant if they are associated with arousal or awakenings from sleep.
- They also may be deemed important if they become disruptive to a bed partner.
- No further treatment may be necessary when noted in isolation on a sleep study without associated symptoms or impacts.
- If another disorder cannot explain the movements, PLMS may be the likely diagnosis.
- Again, if the movements lead to sleep disruption, insomnia, and excessive daytime sleepiness, it is called PLMD.
- Isolated PLMS noted on a sleep study, without consequence, are insignificant and do not require treatment with medication.
Restless leg syndrome is diagnosed based on clinical criteria of having an uncomfortable feeling in the legs associated with an urge to move that occurs in the evening when lying down and is relieved by movement. (Stefani, A., & Högl, B. 2019) Treatment Treatment for PLMS depends on the underlying cause and severity of symptoms. Options include: - Medications (e.g., dopamine agonists, iron supplements)
- Lifestyle changes (e.g., exercise, avoiding caffeine before bed)
- Treating the underlying medical condition
In general, it is unnecessary to treat PLMS if the individual affected has no complaints of sleep disruption. Treatment can be considered if it causes: - Partial or total arousal from sleep
- Contributes to insomnia
- Undermines sleep quality
- Also, if the movements are disruptive to a bed partner, getting them under control may be desirable.
Prescription medications can be effective in treating PLMS. (Cleveland Clinic, 2023) Many of the meds used to treat RLS can be helpful. These may include benzodiazepines (clonazepam), Mirapex (generic name pramipexole), and ropinirole. Movements may also occur with obstructive sleep apnea events, and then the treatment would target the breathing disorder. Injury Medical Chiropractic and Functional Medicine Clinic Individuals who struggle with sleep or other sleep disorders that impact their ability to get restful sleep should consult with their healthcare provider about getting an assessment and treatment to restore health. Individuals can recover and regain the benefits of quality rest through healthy sleep practices and lifestyle accommodations. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to build optimal health and wellness solutions. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Walters, A. S., & Rye, D. B. (2009). Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep, 32(5), 589–597. https://doi.org/10.1093/sleep/32.5.589 Cleveland Clinic. (2023). Periodic limb movement disorder (PLMD). https://my.clevelandclinic.org/health/diseases/14177-periodic-limb-movements-of-sleep-plms Sleep Foundation. (2024). Periodic Limb Movement Disorder What it is, what it feels like, its possible causes, and how it's addressed. https://www.sleepfoundation.org/periodic-limb-movement-disorder Stefani, A., & Högl, B. (2019). Diagnostic Criteria, Differential Diagnosis, and Treatment of Minor Motor Activity and Less Well-Known Movement Disorders of Sleep. Current treatment options in neurology, 21(1), 1. https://doi.org/10.1007/s11940-019-0543-8
Can individuals with arthritis incorporate various natural remedies to reduce joint pain in their extremities and restore mobility? Introduction Regarding the body, joints allow the upper and lower extremities to be mobile. This allows the host to move, bend, flex, and rotate without feelings of pain and discomfort. However, as many people age, so do the body and joints, as wear and tear can cause limited movement and stiffen the body. When this happens, it can lead to inflammatory effects and joint disorders. When the joints develop limited mobility and have overlapping risk profiles, it can come in the form of arthritis. When it comes to arthritis can come into two forms: osteo and rheumatoid, and both forms can cause two different inflammatory effects on the joints, causing pain and discomfort to the individual. Luckily, there are natural ways to manage the overlapping pain profiles caused by arthritis. In today’s article, we will look at the difference between the two forms of arthritis and how various natural remedies can help reduce pain-like symptoms caused by arthritis. We associate with certified medical providers who inform our patients of how arthritis can affect the joints and cause pain-like symptoms to their extremities. While asking important questions to our associated medical providers, we advise patients to incorporate various natural remedies to reduce pain-like symptoms related to arthritis and restore joint health. Dr. Alex Jimenez, D.C., envisions this information as an academic service. Disclaimer. Osteoarthritis Vs. Rheumatoid Arthritis How often do you experience pain in your upper and lower extremities in the cold and feel better with the heat? Do you experience your fingers locking up constantly, making it difficult to grasp objects? Or do you notice swelling or redness in your joints, causing a decreased range of motion? When it comes to the joints dealing with these pain-like issues, it could be due to inflammation, causing the surrounding muscles, tissues, and tendons to become swollen. When it is not being treated, it can lead to the development of arthritis. Arthritis can come in two forms: osteoarthritis and rheumatoid arthritis. These two forms can affect the joints differently, confusing many individuals. Rheumatoid arthritis is a common autoimmune joint disease that causes hyperplasia of the joint tissue and synovial inflammation, which causes cortical bone loss and marginal bone erosion. (Liu et al., 2021) Osteoarthritis can develop when the cartilage between the bones wears down, and it causes the pain associated with inflammation that sensitizes the joint capsule. (Knights et al., 2023) At the same time, osteoarthritis is a well-known degenerative joint disease that is the main cause of disability in a person’s daily living. It has a multifactorial etiology affecting the joint structures. (Yunus et al., 2020) When dealing with either of these forms of arthritis, many people have found natural remedies to help manage the symptoms and reduce the pain. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Could learning to apply healthy sleep hygiene habits help improve sleep and overall health for individuals with sleeping difficulties? Primary Insomnia Insomnia affects most adults at some point in their lives. Primary insomnia is a fairly common condition characterized by difficulty sleeping, and sometimes, it can resolve without treatment. A diagnosis of primary insomnia means that there is no need to worry that a medical or psychological issue is causing sleep problems. Secondary insomnia is the result of medication side effects or medical or psychological issues. However, individuals may need a diagnostic evaluation, including blood tests or an overnight sleep study, to determine an underlying cause for persistent insomnia. Managing lifestyle habits is usually effective for the relief of primary insomnia. If that doesn’t work, medical treatment may be recommended. Symptoms Primary insomnia means not getting enough sleep. Individuals with primary insomnia average six hours of sleep per night (Flynn-Evans E. E. et al., 2017). They often toss and turn or get out of bed frequently. Typically, primary insomnia makes it hard to fall asleep and/or stay asleep. Individuals can wake up easily by triggers like noises or even without triggers. Sleep deprivation can lead to several health problems when awake. Symptoms of insomnia fatigue include: (Salisbury-Afshar E. 2018) - Trouble waking up in the morning
- Constant yawning
- Feeling tired and sleepy throughout the day
- Lack of energy for physical activity
- Lack of motivation
- Hunger
- Difficulty concentrating
- Irritability
- Headaches
- Hypersomnia or falling asleep during the day
- Sensitivity to noise or lights when awake
- Bouts of hyperactivity
- Jumpiness
- Being easily alarmed or frightened
Individuals can experience these symptoms for a few days in a row and resolve the day after a restful night of sleep or after a nap. There are times when fatigue can help with falling asleep, which helps to resolve insomnia. Complications Individuals can develop severe anxiety and distress about the fact that they are not getting enough sleep. This anxiety is usually more severe before going to bed or in the middle of the night, but the worry can continue during the day as well. Persistent insomnia and chronic lack of sleep can lead to depression and predispose the mind and body to health complications. (Sun, Q., & Tan, L. 2019) Insufficient sleep is associated with lowered immune system function, obesity, and heart disease. (Hung C. M. et al., 2018) Causes The conundrum of primary insomnia is that it does not have an identifiable cause, but certain risk factors predispose individuals to have primary insomnia. The condition persists throughout a person’s life, often worsening or improving for months or years. Primary insomnia can be more common among those who have family members with insomnia. Research has found that, while primary insomnia isn’t caused by psychiatric issues, tending to stress or a worry-prone personality might be predisposing factors. (Hung C. M. et al., 2018) Circadian Rhythm Research has found that primary insomnia is associated with circadian rhythm irregularities. It can result from individuals falling into deeper sleep phases earlier than those who don’t have the condition (Flynn-Evans E. E. et al., 2017). However, it can be challenging to know whether early deep sleep is a cause or an effect of primary insomnia. This is because sleep deprivation can also lead to abrupt or rapid onset of deep sleep. Diagnosis Getting enough sleep is a common concern throughout life. Diagnosing primary insomnia involves various steps. One of the main components of identifying insomnia is determining whether the individual needs more sleep than they are getting. For individuals who are unable to get the proper amount of sleep, the second aspect of primary insomnia diagnosis is focused on finding the reason for their lack of sleep. Diagnostic tests measure insomnia and its effects and include: Sleep Study - A polysomnogram is an overnight sleep study measuring brain activity, muscle activity, and breathing.
- The polysomnogram is expected to show decreased sleep and normal breathing patterns if it is primary insomnia. (Sun, Q., & Tan, L. 2019)
Pittsburgh Sleep Quality Index - The PSQI is a questionnaire that includes a self-assessment of sleep.
- It helps identify sleep patterns and issues like using the bathroom frequently at night.
Multiple Sleep Latency Test - An MSLT is a daytime nap study in which participants are monitored to determine how fast they fall asleep.
- The test results are a reflection of your sleep deprivation.
These studies help assess whether an individual is not getting enough sleep and what type of sleep interruption is experienced. Other tests might include screening questionnaires or other assessments of emotional issues like depression and anxiety. Sometimes, individuals are aware of these problems but may dismiss symptoms of depression and anxiety, and they instead manifest as insomnia. Ruling Out Underlying Causes Medical causes of insomnia can include: (Guo H. M. et al., 2017) - Thyroid disease
- Liver disease
- Dementia
- Restless leg syndrome
- Breathing problems.
Individuals might need to have tests to determine whether any of these underlying issues are contributing to their insomnia. Individual medical symptoms and physical examination would guide the diagnostic testing. Sleep Hygiene Habits Individuals can start making small lifestyle adjustments to help regulate their sleep. The key is to avoid things that prevent falling asleep when you want to. Healthy habits include: - Avoid caffeine in the afternoon or evening.
- Avoid alcohol.
- Avoid napping during the day.
- Don't turn on a phone, computer, or television screen in the bedroom before bed.
- Staying away from bright lights for several hours before sleep.
- Scheduling tasks so you feel caught up before going to sleep.
- Getting enough to eat so you aren’t hungry before going to bed.
- Not eating so much that you feel bloated before going to bed.
- Doing some light exercise several hours before going to bed.
Medical Treatment If lifestyle habits don’t help alleviate insomnia, talk to a healthcare provider about medical therapy. Some notice a benefit from treatment with non-prescription-based strategies like counseling, cognitive behavioral therapy for insomnia (CBT-I), or acupuncture. These approaches can have a longer-lasting effect without the risk of side effects. (Salisbury-Afshar E. 2018) A healthcare provider might recommend melatonin or may prescribe medication such as antidepressants, antihistamines, or benzodiazepines. Injury Medical Chiropractic and Functional Medicine Clinic Navigating insomnia can be challenging, but understanding the treatment process can significantly help the individual. A healthcare provider can determine the most effective treatment strategies. This can include physical therapy, rest, health coaching, and medication. Overcoming these limitations is possible. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, prevent injury, and help mitigate issues through adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal problems. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Flynn-Evans, E. E., Shekleton, J. A., Miller, B., Epstein, L. J., Kirsch, D., Brogna, L. A., Burke, L. M., Bremer, E., Murray, J. M., Gehrman, P., Rajaratnam, S. M. W., & Lockley, S. W. (2017). Circadian Phase and Phase Angle Disorders in Primary Insomnia. Sleep, 40(12), 10.1093/sleep/zsx163. https://doi.org/10.1093/sleep/zsx163 Salisbury-Afshar E. (2018). Management of Insomnia Disorder in Adults. American Family Physician, 98(5), 319–322. Sun, Q., & Tan, L. (2019). Comparing primary insomnia to the insomnia occurring in major depression and general anxiety disorder. Psychiatry Research, 282, 112514. https://doi.org/10.1016/j.psychres.2019.112514 Hung, C. M., Li, Y. C., Chen, H. J., Lu, K., Liang, C. L., Liliang, P. C., Tsai, Y. D., & Wang, K. W. (2018). Risk of dementia in patients with primary insomnia: a nationwide population-based case-control study. BMC psychiatry, 18(1), 38. https://doi.org/10.1186/s12888-018-1623-0 Guo, H. M., Liu, M., Xiang, Y. T., Zhao, J., Ungvari, G. S., Correll, C. U., Ng, C. H., Chiu, H. F., & Duan, Z. P. (2017). Insomnia in Adults With Chronic Hepatitis B, Liver Failure, and Cirrhosis: A Case-Control Study. Perspectives in psychiatric care, 53(1), 67–72. https://doi.org/10.1111/ppc.12138
Individuals who have been injured or ill or have a chronic disability may be having difficulty performing everyday activities. Can recreation therapy help rehabilitate injuries and manage chronic conditions? Recreation Therapy Living with a chronic disability or functional limitation due to an illness or injury can significantly impact an individual's quality of life. Working with a team of rehabilitation professionals can help improve mobility and the ability to complete everyday tasks comfortably. A recreational therapist is one professional who helps regain emotional and functional well-being. A recreational therapist is a healthcare professional who helps individuals maximize physical and emotional health through recreational activities. Also known as therapeutic recreation, the therapist will use activities to help move and feel better. A physical or occupational therapist uses exercises to improve functional mobility, and a recreational therapist uses recreational activities to help regain mobility and improve well-being. Activities can include: - Playing games
- Outdoor activities
- Hiking
- Puzzles
- Horseback riding
- Cooking
Therapy A healthcare specialist uses activity-based interventions to help individuals move and feel better after injury or illness or if they have a chronic disability. The interventions and therapies are based on recreational activities the individual likes and are designed to help recover physical, functional, and emotional health. Recreational therapists are trained to evaluate an individual's condition and intervene in ways that help maximize social, mental, and physical health. The main goal is to reduce depression and anxiety and to help individuals socialize comfortably. (American Therapeutic Recreation Association, 2024) Activities Therapeutic recreation involves engaging in specific activities to help individuals regain their confidence and independence. Examples of activities can include: (American Therapeutic Recreation Association, 2024) - Painting or drawing
- Dancing
- Sports programs
- Cooking
- Community outings
- Group exercise classes
The key to a positive experience is that the activity should be specific to the individual's emotional and physical needs and capabilities and something the individual would want to do as an activity. Other Types of Therapy Individuals may be familiar with other types of therapists, like physical and occupational therapists. These professionals help individuals regain pain-free functional mobility after injury or illness. For individuals who cannot move their upper extremities after falling, the physical therapist can measure their shoulder range of motion and strength and develop a personalized treatment program. Recreation therapists are similar; they meet with patients regularly to help them recover from injuries or positively socialize with their community. During the initial meeting, they will evaluate the individual's condition and learn how their emotional and physical needs prevent them from achieving maximal potential. (American Therapeutic Recreation Association, 2024) The patient and therapist will engage in activities to help move and feel better during therapy. During the activity, the therapist may suggest adjustments or ideas that improve movement and ability to interact with the environment. Who Can Benefit? Individuals of all ages and abilities with physical and psychological conditions can benefit from working with a recreational therapist. Children, teenagers, adults, and older individuals who have a disability, either temporary or permanent, can engage in recreation therapy as part of a rehabilitation and recovery program. (American Therapeutic Recreation Association, 2024) Benefits Whenever engaging in any healthcare activity or treatment, ask if that treatment can help your specific condition. A review of the use of recreational dance in children and young people ages 5 to 21 found evidence of the benefits of the therapy, which included: (Burkhardt J, Brennan C. 2012) - Decreased anxiety
- Improve self-image
- Improved cardiovascular fitness
- Decreased obesity
- Improved bone health
Another study examined health improvements in individuals injured in military service after a week-long recreational therapy wellness retreat. The participating service members' results showed significant improvement in outcome measures for post-traumatic stress disorder, stress, anxiety, and depression. The health improvements remained three and six months after completing the recreation therapy. This shows that therapeutic recreation may offer significant emotional and psychological benefits to injured military service members' long-term health and an effective treatment to improve the well-being of injured or disabled individuals with limited negative side effects. (Townsend J, Hawkins BL, Bennett JL, et al., 2018) Professional Background Most therapists have a bachelor's degree in recreational or leisure studies, focusing on art, psychology, and music classes. Upon graduation, students can take a national exam and become Certified Therapeutic Recreation Specialists/CTRS. (Hoss M.A.K, 2019) Once certified, therapists must regularly take continuing education classes and undergo a recertification process every five years. Receiving Therapy Services To start working with a recreational therapist, visit your healthcare provider and request a referral. They can ensure the treatment is appropriate for the specific injury and/or condition and should be able to help find a therapist. (American Therapeutic Recreation Association, 2024) Individuals in an inpatient hospital will likely spend time with a recreational therapist at some point. Just like working with a physical or occupational therapist to help individuals move better, working with a recreation therapist while in rehabilitation may be an everyday occurrence to help reintegrate into the community after discharge. Insurance Coverage One question regarding recreational therapy is, will my insurance cover the services of a recreational therapist? - For individuals with Medicare insurance, recreational therapy is a covered service for individuals with certain diagnoses and settings.
- Therapeutic recreation is a covered rehabilitation service for individuals in an inpatient rehabilitation facility.
- Individuals who receive outpatient recreational therapy should ensure they have a prescription and letter of medical necessity from a physician to qualify for Medicare reimbursement. (American Therapeutic Recreation Association, 2024)
- Individuals with private insurance should call their insurance provider and inquire about coverage for recreation therapy.
- Individuals who do not have insurance can expect to pay $100-$150 per session.
- Each session lasts around one to two hours. (De Vries D. 2014)
Injury Medical Chiropractic and Functional Medicine Clinic Working in therapeutic recreation may help decrease anxiety and depression, improve the sense of well-being, and improve function in daily tasks. (Townsend J, Hawkins BL, Bennett JL, et al., 2018) Always consult your healthcare provider before beginning new treatment methods. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution. We focus on what works for you to relieve pain, restore function, and prevent injury. Regarding musculoskeletal pain, specialists like chiropractors, acupuncturists, and massage therapists can help mitigate the pain through spinal adjustments that help the body realign itself. They can also work with other medical professionals to integrate a treatment plan to resolve musculoskeletal issues. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies that are available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References American Therapeutic Recreation Association. Association, A. T. R. (2024). What is Recreational Therapy? https://www.atra-online.com/about-rt American Therapeutic Recreation Association. Association, A. T. R. (2024). Who We Are. https://www.atra-online.com/who-we-are Burkhardt, J., & Brennan, C. (2012). The effects of recreational dance interventions on the health and well-being of children and young people: A systematic review. Arts & Health, 4(2), 148–161. https://doi.org/10.1080/17533015.2012.665810 Townsend, J., Hawkins, B. L., Bennett, J. L., Hoffman, J., Martin, T., Sotherden, E., … Duregger, C. (2018). Preliminary long-term health outcomes associated with recreation-based health and wellness programs for injured service members. Cogent Psychology, 5(1). https://doi.org/10.1080/23311908.2018.1444330 Hoss, PhD, CTRS, FACHE, FDRT, M. A. K. (2019). Recreational therapy workforce: An update. American Journal of Recreation Therapy, 18(3), 9–15. https://doi.org/10.5055/ajrt.2019.0191 De Vries, DHA, MPA, CTRS, D. (2014). Regulatory requirements for recreational therapy in nursing homes. American Journal of Recreation Therapy, 13(1), 25–30. https://doi.org/10.5055/ajrt.2014.0063
Can individuals reduce stress affecting their daily routine through treatments to restore their gut health? Introduction Everybody in the entire world has dealt with stress at some point in their lives and has experienced general aches and pains in their bodies. This is due to the hormone cortisol, which helps regulate the entire body’s response. Stress has two forms, acute and chronic, and depending on the scenario a person is under, it correlates with stress and can even impact the major body systems. When dealing with acute stress, the muscles start to tense up at the stressor and go into a fight-or-flight mode until the stressor is gone and the individual can begin to relax. However, if the individual is dealing with chronic stress, it can cause numerous overlapping issues that can lead to digestive issues affecting the gut system. When the gut system is acting up from the cortisol hormone in its chronic form, many people will begin to notice small changes that are affecting their health and well-being. Today’s article examines why gut issues induce stress, how individuals can reduce stress naturally, and how people can restore their gut health. We talk with certified associated medical providers who provide our patients’ information to assess gut issues associated with stress that is affecting their health and wellness. We also inform patients while asking their associated medical provider intricate questions to formulate customized treatment plans to reduce the effects of stress correlating to gut health. Dr. Alex Jimenez, D.C., includes this information as an academic service. Disclaimer. Why Gut Issues Induced Oxidative Stress? How often does your body tense up and slowly relax after a stressful situation? Do you experience general aches or pains in your muscles and joints? Or do you feel tenderness and discomfort in your gut? When people are experiencing chronic oxidative stress in their bodies, they sometimes don’t realize that their gut also plays a part. This is because the gut is known as “the second brain” and helps regulate the immune response while protecting the body from unwanted pathogens. However, dealing with a large amount of stress from environmental factors can cause alterations in the immune system’s response and disrupt the delicate balance between the individual and the gut microbiota. (Sharifa et al., 2023) Since gut issues can vary from person to person, it is important to note that when environmental factors cause overlapping risk profiles, it can modify or change the gut microbiota composition of the host.
The gut system, which harbors a large number of beneficial microbial cells, plays a crucial role in the human body. These cells help stimulate the immune system’s maturity and play a role in cognitive performance and stress tolerance. (Marttinen et al., 2020) However, when a person has a poor diet, not physically active, or leads a stressful lifestyle due to their jobs, these environmental factors can cause the development of gut issues over time and contribute to the increase of oxidative stress in the body. (Vasquez et al., 2019) Additionally, many people dealing with chronic stress will often notice their skin feeling a bit warmer, they feel bloated, they will often experience fatigue throughout the day, and experience weight changes. So when the gut system is experiencing high levels of stress from environmental factors, the intestinal epithelial permeability will begin to activate the T-cells that will destroy the immunosuppressive cytokines which leads to systemic inflammation to the body. (Ni et al., 2022) However, there are numerous ways to reduce stress and to help restore gut health naturally. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and is not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico*
Are there ways to make ramen noodles healthier for those who enjoy them? Ramen Noodles Instant ramen noodles are dehydrated noodles flavored with powders. They are inexpensive and easy to prepare by adding hot water. However, these packaged noodles are high in fat and sodium. One package of ramen noodles has around 1,330 milligrams of sodium. (U.S. Department of Agriculture, 2019) However, a ramen meal can be made healthier by adding a source of protein and a serving of vegetables. Nutrition Ramen noodles have about 190 calories, 27 grams of carbohydrates, and 7 grams of total fat, including 3 grams of saturated fat. Unfortunately, they do not have any health benefits other than containing iron, which is necessary for moving oxygen throughout the body and preventing fatigue and anemia or iron deficiency. (Miller J. L. 2013) Because these noodles are low in fiber and nutrients, which are important factors in losing weight, they do not help with weight loss. The high sodium content can lead to bloating and water retention, which is not helpful when losing weight. Healthy Ramen Makeover Individuals can improve their nutritional value by adding ingredients low in calories and high in nutrients. This way, individuals can still have an inexpensive meal that isn't entirely unhealthy while increasing the volume. Adding chicken and vegetables adds vitamins and protein without much fat. Although each serving is still around 200 calories, it contains only 4.5 grams and less than 2 grams of saturated fat. This also increases the fiber from 1 gram to about 2.5 grams, adding vitamin A, lutein, and B vitamins. (U.S. Department of Agriculture, 2019) Adding vegetables and lean meats adds volume to the meal and helps increase the feeling of being full. (Mayo Clinic, 2024) Recipe A recipe for noodles with healthy fats, vitamins, minerals, and fiber. - Package of ramen noodles or cup of noodles.
- One cup of cooked chicken breast.
- One cup of frozen mixed vegetables like peas, carrots, and onions or a combination.
- Prepare the noodles by cooking one package in three cups of boiling water until the noodles are soft.
- Add the flavor packet.
- Add cooked chicken breast meat and frozen vegetables.
- Stir until vegetables are heated thoroughly.
- Complete the meal with a small salad dressed with olive oil, vinegar, or light salad dressing.
Try out other Recipes Try other proteins, vegetables, and flavorings. Shrimp or cooked fish can add healthy omega-3 essential fatty acids (Swanson, D. et al., 2012), or vegetarian protein like tofu or legumes for added protein. Enhance the flavor with sesame oil, mushrooms, bean sprouts, etc. Reduce the amount of powder from the flavoring pack to reduce sodium even more. To compensate for the loss of flavor, try supplementing with garlic, pepper, or favorite herbs. For those who prefer the cups of noodles, remember each cup is two servings. Prepare a cup of hot water and place the noodles on top of cooked vegetables and meat. Injury Medical Chiropractic and Functional Medicine Clinic Injury Medical Chiropractic and Functional Medicine Clinic providers use an integrated approach to create personalized care plans for each patient and restore health and function to the body through nutrition and wellness, functional medicine, acupuncture, Electroacupuncture, and sports medicine protocols. If the individual needs other treatment, they will be referred to a clinic or physician best suited for them. Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, nutritionists, and health coaches to provide the most effective clinical treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References U.S. Department of Agriculture. FoodData Central. (2019). Nissin, Top Ramen, Ramen Noodle Soup, Chicken. Retrieved from https://fdc.nal.usda.gov/fdc-app.html#/food-details/410139/nutrients Miller J. L. (2013). Iron deficiency anemia: a common and curable disease. Cold Spring Harbor perspectives in medicine, 3(7), a011866. https://doi.org/10.1101/cshperspect.a011866 Mayo Clinic. (2024). Weight loss: Feel full on fewer calories. https://www.mayoclinic.org/healthy-lifestyle/weight-loss/in-depth/weight-loss/art-20044318 Swanson, D., Block, R., & Mousa, S. A. (2012). Omega-3 fatty acids EPA and DHA: health benefits throughout life. Advances in nutrition (Bethesda, Md.), 3(1), 1–7. https://doi.org/10.3945/an.111.000893
For individuals dealing with headaches, can utilizing self-care techniques help ease symptoms? Headaches Self Care There are different self-pain-relieving approaches to ease headache-related pain that use non-medication options. While headache self-care pain-relieving techniques can help temporarily, they are recommended to help ease headache symptoms until professional treatment is available. Individuals are encouraged to try multiple strategies to find the right treatment regimen that works for them, which is usually a process of trial and error. Self-care headache relief maneuvers can include temple massages, breathing exercises, exercise, or applying a cold pack to the head. Self-Care Relief Commonly used for tension headaches or migraine, a few examples of self-care techniques include (Espí-López G. V. et al., 2016) - Massaging the temples, neck, or scalp with the hand, fingers, or a massage tool.
- Applying a cold pack to the affected area.
- Heat can be used on the affected area, like a headband or a hot shower.
- Compression such as a handkerchief or belt wrapped tightly around the head or pressing firmly on the painful area.
Compression is more commonly utilized in migraineurs versus scalp massage in people with tension headaches. This is often due to the throbbing sensation caused by a migraine versus a tension headache, which feels like a tight grip or band around the head. Individuals with cluster headaches are more likely to utilize unique approaches, such as covering one ear, rotating the head, shallow breathing, moving around, or closing the nostril on the same side as the head pain. Other Complementary Options Other complementary therapies for headache and migraine care include: (Millstine D. et al., 2017) - Trigger point release massage
- Progressive muscle relaxation
- Aerobic exercise
- Yoga
- Deep breathing exercises
- Meditation
- Cognitive-Behavioral Therapy
Various scientific studies support the potential benefit of these complementary therapies. However, individuals should talk with a healthcare provider to choose the best strategy for their headache type and their unique needs/goals. Working with a chiropractic team can help expedite healing. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop a customized treatment plan through an integrated approach to treating injuries and chronic pain syndromes, improving flexibility, mobility, and agility, relieving pain, and helping individuals return to normal activities. If other treatments are needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Espí-López, G. V., Zurriaga-Llorens, R., Monzani, L., & Falla, D. (2016). The effect of manipulation plus massage therapy versus massage therapy alone in people with tension-type headache. A randomized controlled clinical trial. European journal of physical and rehabilitation medicine, 52(5), 606–617. Millstine, D., Chen, C. Y., & Bauer, B. (2017). Complementary and integrative medicine in the management of headache. BMJ (Clinical research ed.), 357, j1805. https://doi.org/10.1136/bmj.j1805
Can understanding the nucleus pulposus help in body positioning and prevention for individuals wanting to practice spinal hygiene and protect their discs from injury? Nucleus Pulposus The spinal discs are located between the spine's vertebrae and are the body's natural impact and shock absorbers. Within the disc is the nucleus pulposus, which plays a major role in providing the spine with shock absorption during movement. (Zhou Z. et al., 2014) The discs have a tough outer portion and a soft inner core. They are the: Annulus Fibrosus - The annulus fibrosus is the outer portion of the disc.(Nosikova, Y. S. et al., 2012)
- It forms the tough circular exterior and comprises concentric sheets of collagen fibers or lamellae surrounding the inner core.
- It has cartilaginous endplates that firmly attach to the vertebrae above and below.
Nucleus Pulposus - The nucleus pulposus is the inner core soft filling of the discs.
- It contains a network of fibers suspended in a mucoprotein gel with a water base to maintain strength and pliability.
- The near-liquid consistency makes it responsive to movement to handle the body's axial load.
- It helps maintain spinal suspension to prevent pressure on the bones and prevent bone-to-bone contact, reducing the potential for injuries and pain.
Shock Absorber Each intervertebral disc is a shock-absorbing cushion, with the nucleus pulposus providing shock-absorbing properties (Zhou Z. et al., 2014). The intervertebral discs move as the body moves. For example, when arching the back, the disc moves forward slightly, and when twisting, the disc twists as well. Spinal Action The intervertebral disc supports spinal movements. When bending, twisting, arching, or tilting the spine, the nucleus pulposus swivels to accommodate these actions. These repeated spinal actions, which occur throughout the day and night, contribute to shifting positions while sitting, working, playing sports, carrying groceries, performing house chores, etc. An example is bending forward to pick something up. This action involves forward spinal flexion, which is bending the spine forward, flattening, or rounding. When bending using flexion, the spinal bones come closer together, pushing the nucleus pulposus toward the back. Injuries The disc can be pushed too far back with persistent or excessive spinal flexion. If the fibers of the annulus fibrosus become weak, they can tear, causing the nucleus pulposus to leak out and disc herniation. Generally, the nucleus pulposus will leak to the side and back; however, this corresponds to the location of the very sensitive nerve root/s with which it can come into contact, causing pain and other symptoms. The most common causes of disc herniation are degenerative wear and tear changes of the disc and trauma. Disc degeneration occurs as the body ages; it weakens the annulus fibers, allowing the nucleus pulposus to distend, bulge, or herniate. Aging Disc degeneration occurs with age but can also occur with injuries to the area. In young individuals, the nucleus pulposus is mostly water. For this age group, a herniation from trauma is more likely than in older individuals. (Ucar, D. et al., 2021) But as the body ages, the discs, especially the nucleus pulposus, begin to dry out. This dehydration leads to a significant loss of disc height. (UCLA Health, 2024) By age 60 or 70, the discs may be composed entirely of fiber, which can cause the shock absorption function not to work and disappear. Chiropractic therapy is among the more conservative treatment options for a herniated disc and may be tried first before proceeding with more invasive treatments. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution that fully benefits the individual to get back to normal. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Zhou, Z., Gao, M., Wei, F., Liang, J., Deng, W., Dai, X., Zhou, G., & Zou, X. (2014). Shock absorbing function study on denucleated intervertebral disc with or without hydrogel injection through static and dynamic biomechanical tests in vitro. BioMed research international, 2014, 461724. https://doi.org/10.1155/2014/461724 Nosikova, Y. S., Santerre, J. P., Grynpas, M., Gibson, G., & Kandel, R. A. (2012). Characterization of the annulus fibrosus-vertebral body interface: identification of new structural features. Journal of anatomy, 221(6), 577–589. https://doi.org/10.1111/j.1469-7580.2012.01537.x Ucar, D., Duman, S., Bayram, Y., & Ucar, B. Y. (2021). Extruded disc herniations are experienced earlier by inactive young people in the high-tech gaming era. Journal of medicine and life, 14(3), 402–407. https://doi.org/10.25122/jml-2021-1059 UCLA Health. (2024). Degenerative disc disease (Conditions Treated, Issue. https://www.uclahealth.org/medical-services/neurosurgery/conditions-treated/degenerative-disc-disease
For individuals who are dealing with back pain and problems, could knowing how to improve and maintain intervertebral disc health help alleviate symptoms? Intervertebral Disc Health The spinal column comprises 24 movable bones and 33 bones called vertebrae. The vertebral bones are stacked on top of each other. The intervertebral disc is the cushioning substance between the adjacent bones. (Dartmouth. 2008) Bones The vertebral bones are small and round in an area called the vertebral body. In the back is a bony ring from which protrusions extend and arches and pathways are formed. Each structure has one or more purposes and includes: (Waxenbaum JA, Reddy V, Williams C, et al., 2023) - Stabilizing the spine.
- Providing a space for the connective tissue and back muscles to attach.
- Providing a tunnel for the spinal cord to pass through cleanly.
- Providing a space where nerves exit and branch out to all areas of the body.
Structure The intervertebral disc is the cushioning that sits between the vertebrae. The design of the spine allows it to move in various directions: - Flexion or bending
- Extension or arching
- Tilting and rotation or twisting.
Powerful forces act upon and influence the spinal column to produce these movements. The intervertebral disc absorbs shock during movement and protects the vertebrae and spinal cord from injury and/or trauma. Ability On the outside, strong woven fiber tissues form an area called the annulus fibrosis. The annulus fibrosis contains and protects the softer gel substance in the center, the nucleus pulposus. (Y.S. Nosikova et al., 2012) The nucleus pulposis provides shock absorption, flexibility, and pliability, especially under pressure during spinal movement. Mechanics The nucleus pulposus is a soft gel substance located in the center of the disc that allows elasticity and flexibility under stress forces to absorb compression. (Nedresky D, Reddy V, Singh G. 2024) The swivel action alters the tilt and rotation of the vertebra above and below, buffering the effects of spinal motion. The discs swivel in response to the direction the spine moves. The nucleus pulposus is made mostly of water, which moves in and out through small pores, acting as byways between the vertebra and disc bone. Body positions that load the spine, like sitting and standing, push the water out of the disc. Lying down on the back or in a supine position facilitates water restoration into the disc. As the body ages, the discs lose water/dehydrate, leading to disc degeneration. The intervertebral disc has no blood supply, which means that for a disc to receive necessary nutrition and for waste removal, it must rely on water circulation to stay healthy. Care Some ways of maintaining intervertebral disc health include: - Paying attention to posture.
- Changing positions frequently throughout the day.
- Exercising and moving around.
- Applying correct body mechanics to physical activities.
- Sleeping on a supportive mattress.
- Drinking plenty of water.
- Eating healthy.
- Maintaining a healthy weight.
- Drinking alcohol in moderation.
- Quitting smoking.
At Injury Medical Chiropractic and Functional Medicine Clinic, we treat injuries and chronic pain syndromes by improving an individual’s ability through flexibility, mobility, and agility programs tailored for all age groups and disabilities. Our chiropractic team, care plans, and clinical services are specialized and focused on injuries and the complete recovery process. Our areas of practice include Wellness & Nutrition, Acupuncture, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols. If other treatment is needed, individuals will be referred to a clinic or physician best suited to their injury, condition, and/or ailment. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, don't hesitate to contact Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Dartmouth Ronan O'Rahilly, MD. (2008). Basic Human Anatomy. Chapter 39: The vertebral column. In D. Rand Swenson, MD, PhD (Ed.), BASIC HUMAN ANATOMY A Regional Study of Human Structure. W.B. Saunders. https://humananatomy.host.dartmouth.edu/BHA/public_html/part_7/chapter_39.html Waxenbaum, J. A., Reddy, V., Williams, C., & Futterman, B. (2024). Anatomy, Back, Lumbar Vertebrae. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/29083618 Nosikova, Y. S., Santerre, J. P., Grynpas, M., Gibson, G., & Kandel, R. A. (2012). Characterization of the annulus fibrosus-vertebral body interface: identification of new structural features. Journal of anatomy, 221(6), 577–589. https://doi.org/10.1111/j.1469-7580.2012.01537.x Nedresky D, Reddy V, Singh G. (2024). Anatomy, Back, Nucleus Pulposus. In StatPearls. https://www.ncbi.nlm.nih.gov/pubmed/30570994
|



 Your new post is loading...
Your new post is loading...