 Your new post is loading...
 Your new post is loading...
For wrestling athletes or those thinking about getting into the sport, can knowing about common injuries help in rehabilitation and prevention? Wrestling Injuries Wrestling is an intense and demanding sport. Studies have found that football and wrestling are the two high school sports with the highest risk of serious injury to athletes (Center for Injury Research and Policy, 2009). The injury rate for college wrestlers is 9 injuries per 1,000 athlete exposures. (Kroshus, E. et al., 2018) While most wrestling injuries include strains and sprains, there can also be serious traumatic and unusual injuries. Using proper safety gear and learning correct techniques can significantly reduce the risk of injuries. The majority occur during competition. Common The most common wrestling injuries are similar to those in other sports and include: Muscle Soreness - Muscle soreness that is experienced 12 to 48 hours after an intense workout or competition.
- Resting is often all that is needed to recover.
Bruises and Contusions - Sparring, take-downs, and hard landings can result in various bruises and contusions.
Sprains and Strains - Rest, ice, compression, and elevation are recommended to treat sprains and strains immediately.
Ankle Sprains - Ankle sprains occur when surrounding ligaments stretch and tear around the joint.
Wrist Sprains - Typically, it occurs when stretching or tearing the ligaments.
- Falling or landing on the hands is a common cause.
Overtraining Syndrome - Frequently occurs in athletes who train beyond the body's ability to recover.
Dehydration - When trying to make weight, dehydration can be a serious health problem that many wrestlers experience.
Other Injuries Other injuries common in wrestling: - Wrist tendinitis
- Finger fractures
- Iliotibial band syndrome
- Meniscus tears
- Groin pull
- Hamstring pull or tear
- Pulled calf muscle
- Achilles tendonitis
- Achilles tendon rupture
- Clavicle/Collarbone fracture
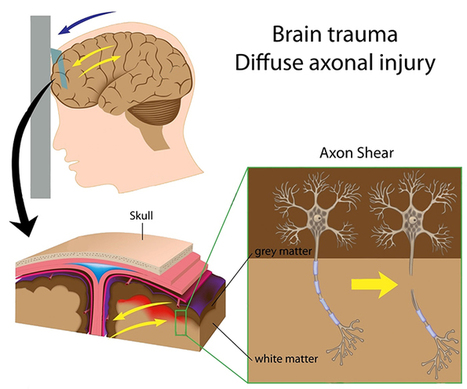
- Concussion
Serious The forcing of a joint beyond its normal range of motion is the most common cause of serious injuries. The most serious wrestling injuries affect the neck, shoulder, elbow, and knee and include: Neck - The cervical vertebrae are often forced into vulnerable positions during various techniques and movements, which can result in a neck injury. Common types include:
- Neck Strain
- Whiplash
- Cervical Fracture
Shoulder - A combination of leverage and twisting causes most upper body and shoulder injuries during competition. Types of shoulder injuries include:
- Rotator cuff injury
- Shoulder separation
- Shoulder dislocation
Elbow Dislocation - Elbows are under tremendous strain when maneuvering.
- Dislocations of the radial head are often related to the athlete bracing for a fall on an outstretched arm during take-downs.
Knee - Most knee injuries occur to the ligaments of the knee joint.
- These include anterior and posterior cruciate ligament or ACL/PCL injuries.
Safety Wrestling requires flexibility, strength, and proper technique to prevent injury, combined with thorough instruction and coaching and following basic safety precautions. Some tips include. Safety Gear - Wear appropriate headgear and mouthguards during practices, meets, and tournaments.
Improving Joint Flexibility - Wrestlers with a high degree of shoulder flexibility have fewer injuries.
- The flexibility of the lower back, hamstrings, elbows, and cervical spine should also be worked on.
Gain or Lose Weight Safely - Avoid dramatic weight loss and weight-gaining strategies by maintaining healthy nutrition and hydration during the season.
Avoiding Dangerous Holds and Slam Moves - Safe wrestling techniques need to be followed as these can generate severe injuries.
Regardless of how common or seemingly not serious an injury or medical condition is, it's important to rest and recover and tell a coach and health care professional, as some injuries and conditions can become serious if left untreated. Injury Medical Chiropractic and Functional Medicine Clinic focuses on and treats injuries and chronic pain syndromes through personalized care plans that improve ability through flexibility, mobility, and agility programs to relieve pain. Our providers use an integrated approach to create personalized care plans for each patient, including Functional Medicine, Acupuncture, Electro-Acupuncture, and Sports Medicine principles. Our goal is to relieve pain naturally by restoring health and function to the body. If other treatment is needed, Dr. Jimenez has teamed up with top surgeons, clinical specialists, medical researchers, and rehabilitation providers to provide the most effective treatments. General Disclaimer * The information herein is not intended to replace a one-on-one relationship with a qualified healthcare professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.* Our office has reasonably attempted to provide supportive citations and identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please get in touch with Dr. Alex Jimenez or contact us at 915-850-0900. Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, ATN* email: coach@elpasofunctionalmedicine.com Licensed in: Texas & New Mexico* References Nationwide Children’s Hospital. (2024). Center for Injury Research and Policy. https://www.nationwidechildrens.org/research/areas-of-research/center-for-injury-research-and-policy Kroshus, E., Utter, A. C., Pierpoint, L. A., Currie, D. W., Knowles, S. B., Wasserman, E. B., Dompier, T. P., Marshall, S. W., Comstock, R. D., & Kerr, Z. Y. (2018). The First Decade of Web-Based Sports Injury Surveillance: Descriptive Epidemiology of Injuries in US High School Boys' Wrestling (2005-2006 Through 2013-2014) and National Collegiate Athletic Association Men's Wrestling (2004-2005 Through 2013-2014). Journal of athletic training, 53(12), 1143–1155. https://doi.org/10.4085/1062-6050-154-17
Injury specialist, Dr. Alexander Jimenez looks at the latest study about concussion in sports, especially regarding early/on-field assessment and diagnosis of this condition. The proper medical definition of concussion is: a clinical syndrome characterized by immediate and transient change in brain function, including alteration of mental illness and level of consciousness, resulting from mechanical pressure or injury. But, it is more commonly described as an injury to the brain caused by a blow to the head (eg an uppercut in boxing, a clash of heads in soccer or a fisherman moving over the handlebars on the ground etc), which leads to temporary loss of normal brain function, including disturbances in memory, judgment, reflexes, speech, balance and muscle coordination. A less obvious cause is an indirect blow where the force is transmitted up to the head from a different portion of the body -- for example when a stationary rugby player is tackled from behind causing his head to abruptly flick back, with a number of the force of the tackle passing through his brain; the participant may end up concussed without ever taking a direct blow to the head. While bruises and cuts might be present on your face or head as a consequence of this blow, in most cases a person with a concussion never loses consciousness. Because of this, less experienced coaches and sports physicians may not immediately assume concussion, or if they do they presume that it's unlikely to be a cause for concern. But, though some concussions are less severe than others, there's absolutely no such thing as a 'minor concussion'; while a single concussion should not result in permanent damage, another concussion shortly after the initial one doesn't have to be very powerful for its consequences to be fatal or permanently disabling. Animal and human studies support the concept of this so-called 'post-concussive vulnerability', showing that a second blow before the mind has regained results in worsening metabolic changes within the cell(1). This explains the crucial importance of correctly and immediately identifying when a concussion has occurred because it affords the opportunity of this athlete to be taken out of the field of play, thereby ensuring a second concussion cannot happen. Initial Diagnosis Of ConcussionAs soon as an athlete suffers a blow to the head, the first priority should be that someone qualified is available to assess whether concussion has occurred. In an ideal world, this assessment could always be performed by a physician specifically trained in this area. In many sporting events (eg a small league football game), it is unlikely that such a individual will be there standing on the sidelines. However, as stated by the America Medical Society for Sports Medicine (AMSSM), the competence to execute this assessment also needs to be decided by training and experience and not purely dictated by specialty(1). To put it differently, with the right training and expertise, coaches, trainers and health care professionals are more than capable to perform a concussion examination. The AMSSM additionally points out that the identification of concussion is ideally created by a healthcare provider who is not only knowledgeable in the recognition and analysis of concussion but also familiar with the person concerned. The reason for this is that while standardized sideline tests are a useful framework for making an appraisal, the validity and reliability of these tests are greatly reduced without some type of individual baseline test result with which to compare, and some other baseline rating will vary based on the individual athlete concerned. AMSSM New GuidelinesThe primary recommendations were assembled by reviewing the evidence over a number of years and are summarized as follows: - Any athlete suspected of having a concussion should be stopped from playing and assessed by a qualified healthcare provider trained in the evaluation and management of concussion and ideally someone who is familiar with the athlete (for the reasons given above). The recognition and initial assessment of a concussion should be guided by a symptoms checklist, cognitive evaluation (which should include orientation, past and immediate memory, new learning and concentration), balance tests and further neurological and physical examination.
- Coaches/physicians/healthcare providers should take note that while balance disturbance is a specific indication of a concussion, it isn't very sensitive. In particular, performing equilibrium testing about the touchline may yield substantially different results than baseline evaluations simply because of differences in shoe/cleat-type or surface, use of ankle tape or braces, or the presence of other lower extremity injuries that might have also happened during the episode involving the head injury.
Any athlete suspected or diagnosed with a concussion should be monitored for deteriorating physical or mental status. Importantly, there should be NO same day return to play for an athlete diagnosed with a concussion injury. Meanwhile, imaging should be reserved for athletes where intracerebral bleeding is suspected. - Even though most concussions can be managed appropriately without the use of neuropsychological (NP) testing, those with athletes in their maintenance ought to bear in mind that NP evaluations are an objective measure of brain- behavior relationships and, as such, are somewhat more sensitive for subtle cognitive impairment than a straightforward clinical examination. However, NP testing should be used only as part of a extensive concussion management plan and should not be utilized in isolation. Also, the ideal timing, frequency and type of NP testing have not been completely ascertained.
- Computerized NP testing should be translated by health care professionals educated and comfortable with the type of test and also the individual test limitations. Paper and pencil NP evaluations are both valuable and are able to test different domain names and assess for different conditions, which may masquerade as or reevaluate evaluation of concussion.
- Concussion symptoms must be resolved before returning to perform with (RTP) and RTP after concussion should happen just with medical clearance from an experienced health-care supplier trained in the analysis and management of concussions -- see Box 2. An RTP progression entails a gradual, step-wise increase in bodily demands, sports-specific activities and the danger of contact. If any signs recur using action, the progression ought to be stopped and resumed in the previous symptom-free step. In the brief term, the principal concern with early RTP is diminished reaction time resulting in an increased risk of a repeat concussion or additional injury and prolongation of symptoms. In the long run, there's a growing concern that head impact exposure and recurrent concussions can contribute to long-term neurological complications and a number of studies have indicated an association between previous concussions and chronic cognitive impairment.
- Physicians should be prepared to offer counseling regarding potential long-term consequences of a concussion and continuing concussions. However, there are currently no evidence-based guidelines for disqualifying/retiring an athlete from a game after a concussion. More commonly, greater efforts are needed to educate involved parties, such as athletes, parents, coaches, officials and school administrators and health care providers to boost concussion recognition, prevention and management.
Recent Findings: On-Field & Same Day AssessmentMake no mistake, but the first assessment of concussion in the mature athlete is tough, given that the elusiveness of harm, the sensitivity and specificity of their sideline assessment tools along with the evolving nature of concussive injury. A very current (2013) review newspaper systematically examined the evidence related to on-field concussion assessment and considered questions related to same day return to play, what to do if no doctor is available onsite, as well as the benefit of distant notification of future concussive events(3). It concluded that the on-field test of sport-related concussion is often a challenge, especially given the elusiveness and variability of presentation, the strain to create a quick diagnosis (as an instance, in the middle of an important match in which the concussed athlete was making a significant contribution), the specificity and sensitivity (or rather lack of) of this on-field assessment tools, along with the dependence on symptom presentation. However, they cautioned that a range of assessments over a brief time period tend to be necessary and, since signs and symptoms may be postponed, erring on the side of caution (ie maintaining an athlete from participation whenever there's a distress for harm) is important. In addition, they concluded that although a standardized evaluation of concussion is beneficial in the evaluation of the athlete with suspected concussion, it should NOT take the place of the clinician's conclusion. These findings have been very much in agreement with another 2013 review research on instruments currently utilized in the evaluation of sport-related concussion on the day of injury -- consequently 'same day' assessment tools(4). In this review, a total of 41 research on sports concussion were pooled and their findings analyzed. The authors concluded that several well- supported tests are acceptable to be used in the evaluation of acute concussion from the athletic athletic environment and that these evaluations can provide significant data on the symptoms and functional impairments that clinicians can integrate in their diagnostic formula. But they also cautioned that such tests should not solely be used to diagnose concussion. SCAT3 Assessment ToolAs mentioned above, the first evaluation of an injured athlete with suspected concussion remains predominant in determining subsequent action. There are a number of diagnostic tools available, but undoubtedly among the most admired is when there is no one with medical training available to tend to an injured athlete, it is recommended that the ‘Sport Concussion Recognition Tool’ be used instead (seeBox 3). The SCAT3 assessment tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf. The SCAT3 is a standardized instrument for evaluating injured athletes for concussion, and is intended for use by medical professionals. SCAT3 supersedes the first SCAT and SCAT2 published in 2005 and 2009 respectively. Importantly, baseline testing together with the SCAT3 can be beneficial for translating post-injury test scores at a later date. The SCAT3 evaluation tool can be downloaded here: http://bjsm. bmj.com/content/47/5/263.full.pdf SCAT3 is a detailed tool that assesses the following areas: background, symptom evaluation, cognitive and physical function, neck trauma, balance and coordination. According to the SCAT guidelines, the first indications through a sideline evaluation are critical and any of the following warrants triggering emergency procedures and barbarous transport to the nearest hospital: - a Glasgow Coma score of less than 15 (see Box 4)
- deteriorating mental status
- potential spinal injury
- progressive, worsening symptoms or new neurologic signs.
It is important to highlight, but that scoring on the SCAT3 shouldn't be utilized as a stand-alone process to diagnose concussion, quantify recovery or make conclusions regarding an athlete's readiness to come back to competition after concussion. Additionally, since signs and symptoms can evolve over time, it's very important to consider repeat evaluation from the acute evaluation of concussion. Finally, it needs to be stressed that the identification of a concussion is a medical judgment, ideally created by a medical professional. The SCAT3 shouldn't therefore be used solely to make, or exclude, the diagnosis of concussion in the absence of clinical judgement. An athlete could have a concussion even if their SCAT3 score is 'normal'. References
1. Br J Sports Med. 2013 Jan;47(1):15-26. doi: 10.1136/bjsports-2012-091941
2. Am J Sports Med. 2012 Apr;40(4):747-55
3. Br J Sports Med. 2013 Apr;47(5):285-8
4. Br J Sports Med. 2013 Apr;47(5):272-84
5. Br J Sports Med 2013 47: 259
6. downloadable from: http://bjsm.bmj.com/content/47/5/267.full.pdf
|
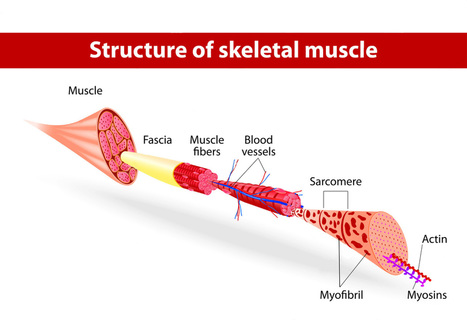
Chiropractic scientist, Dr. Alexander Jimenez has a look at this painful condition which can be the cause of a lot of lost playing time. Last year, rugby union player Anthony Allen of the Leicester Tigers endured what he believed was a reasonably straightforward blow to the exterior of his shin -- but it ended up being a nightmare which would keep him out for four weeks of rugby. In October 2013, he thought he'd sprained his ankle in a match, as he did not recall sustaining a direct blow to the surface of the shin. Over the ensuing days, he noticed that the pain was worsening and he was experiencing swelling and pain sensations further down the shin away from the website of the accident, with some minor paraesthesia into the top of the foot. He alerted the medical staff to his worsening illness and they immediately referred him to an orthopaedic surgeon who watched the leg using an ultrasound (to exclude a deep vein thrombosis), after which an MRI, which confirmed that the participant was suffering from an acute compartment syndrome in the lower leg. They conducted an operation to successfully alleviate the pressure from the leg, and he was told that the rehabilitation following this harm could be 3-4 weeks. What Is Compartment Syndrome?When a body part receives a direct blow because of an external object, muscle damage can ensue. The outcome is a hematoma, which is a swelling inside the muscle due to blood accumulation -- a consequence of the direct bleeding of this muscle as little venules and possibly arterioles are damaged and 'leak' blood to the region, which then collects into a mass. A hematoma can grow within the muscle or external to the true muscle and involving the fascial sheaths that surround the muscle. The majority of those hematomas are benign and, although painful for 7-21 days, they finally resolve and the sufferer regains full purpose. The origin of the direct blow may be the sufferer contacting another person forcefully, as in being kicked in soccer or martial arts or a direct blow due to a tackle in football. These are commonly known as 'contusions', ' 'corks' or ' 'charley horses'. This is called the osteofascial compartment. This growth in volume within a enclosed space eventually compresses the blood vessels and nerves that run through the compartment and symptoms have been exacerbated. Who Can Get Compartment Syndrome?Most cases of compartment syndrome are a result of high velocity trauma like motor vehicle accident or falling out of a quick- moving bike/horse. These generally involve a bone fracture like the tibia in the upper leg or the radius in the forearm. The amount of blood discharged from the bone will collect in the osteofascial compartment. But, they may also be caused by lead high-force 'crush'-type injuries which do not break bones but do end up damaging a lot of muscle tissue. This can be because of a direct hefty blow that spreads the pressure across a wide region and does not violate any underlying bone. Severe burns may also lead to compartment syndromes. Young males are the most likely victims as ordinarily they're involved in sport and pastimes that may expose them to high velocity or high-force trauma that may cause this pathology. Individuals on anti-coagulant blood thinners are also more vulnerable. Because the fascia of the compartment does not stretch, a little increase in blood volume can result in large increases in pressure. This rapidly compresses the nerves and blood vessels (typically veins) and the normal late signs of compartment syndrome like needles and pins and deficiency of pulses may then result. Arteries are usually spared as the systolic blood pressure in the gut is usually too high to be compressed by the compartment pressure. Chronic compartment syndromes which are not medical emergencies may occur in athletes because of a slow growth in muscle size because of hypertrophy with an overlying fascia that doesn't stretch. This impacts runners, cyclists and even bodybuilders. Signs & SymptomsThe usual signs and symptoms of an acute compartment syndrome are called the 6 Ps: - Pain (out of proportion to expected tissue damage). Usually a deep pain and is aggravated by stretch of the muscle;
- Paralysis due to compression of motor nerves;
- Pallor due to blood vessel compression;
- Paraesthesia due compression of nerves.;
- Pressure elevation (measurable);
- Pulselessness (rare and usually only if severe compression).
The pain and neurological disorders (pins and needles) have been early signals; diminished or absent pulses and paralysis are late signs. Pallor may come with a swollen and tense muscle because of the collection of blood at the underlying muscle compartment. DiagnosisThe most direct measure for compartment syndrome is a compartment pressure test. In such examples, it has been recommended that the compartment decompression may be necessary. TreatmentThis involves an incision into the thoracic fascia, similar to how a sausage on the BBQ may be sliced to discharge juices from a swelling sausage since it is being heated. It is common place to perform a fasciotomy on all the compartments in the area affected. As a result of sudden onset of elevated compartment pressure, if the injury isn't dealt with immediately, catastrophic permanent damage to the muscle, nerves and blood vessels can result, leaving permanent scarring in these types of structures and generally rhabdomyolysis may ensue, leaking toxins into the blood stream that might result in kidney damage. RehabilitationFollowing operation, the time frame for return to straightforward activities like walking is generally quite quick and the individual might be functional with this particular capacity in 4-6 weeks. They might require gentle soft tissue massage to stop excessive scarring and adhesions, and gentle progressive strength training to recover lost muscle functioning. The athlete needs a longer time frame to return to perform as they will need a more systematic rehabilitation protocol which takes them from walking to running to sprinting and ultimately explosive movements such as jumps and take-off moves. They'll require longer to regain strength and full stretch in addition to other high-level capacities such as proprioception and balance control.
|



 Your new post is loading...
Your new post is loading...








Discover the risks and rewards of wrestling, an intense and demanding sport. Learn about common injuries and how to prevent them. For answers to any questions you may have, call Dr. Jimenez at 915-850-0900 or 915-412-6677