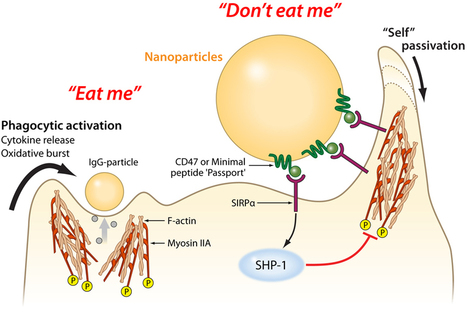
Macrophages — literally, "big eaters" — are a main part of the body's innate immune system . These cells find and engulf invaders, like bacteria, viruses, splinters and dirt. Unfortunately, macrophages also eat helpful foreigners, including nanoparticles that deliver drugs or help image tumors.
Along with members of his lab, Dennis Discher, professor of chemical and biomolecular engineering in the School of Engineering and Applied Science, has developed a "passport" that could be attached to therapeutic particles and devices, tricking macrophages into leaving them alone.
Taking a cue from a membrane protein that the body's own cells use to tell macrophages not to eat them, the researchers engineered a the simplest functional version of that protein and attached it to plastic nanoparticles. These passport-carrying nanoparticles remained in circulation significantly longer than ones without the peptide, when tested in a mouse model.
In 2008, Discher’s group showed that the human protein CD47, found on almost all mammalian cell membranes, binds to a macrophage receptor known as SIRPa in humans. Like a patrolling border guard inspecting a passport, if a macrophage’s SIRPa binds to a cell’s CD47, it tells the macrophage that the cell isn’t an invader and should be allowed to proceed on.
“There may be other molecules that help quell the macrophage response,” Discher said. “But human CD47 is clearly one that says, ‘Don’t eat me’.” Since the publication of that study, other researchers determined the combined structure of CD47 and SIRPa together. Using this information, Discher’s group was able to computationally design the smallest sequence of amino acids that would act like CD47. This “minimal peptide” would have to fold and fit well enough into the receptor of SIRPa to serve as a valid passport. After chemically synthesizing this minimal peptide, Discher’s team attached it to conventional nanoparticles that could be used in a variety of experiments. “Now, anyone can make the peptide and put it on whatever they want,” Rodriguez said.
The research team’s experiments used a mouse model to demonstrate better imaging of tumors and as well as improved efficacy of an anti-cancer drug-delivery particle.
As this minimal peptide might one day be attached to a wide range of drug-delivery vehicles, the researchers also attached antibodies of the type that could be used in targeting cancer cells or other kinds of diseased tissue. Beyond a proof of concept for therapeutics, these antibodies also served to attract the macrophages’ attention and ensure the minimal peptide’s passport was being checked and approved.
Video is here: http://tinyurl.com/b6dthgb
Via Dr. Stefan Gruenwald



 Your new post is loading...
Your new post is loading...