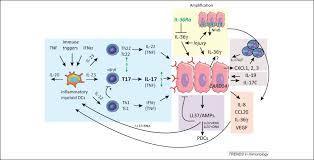
One-third of patients with Crohn's disease (CD) or ulcerative colitis (UC) receiving anti-TNFs do not respond to treatment, and a relevant proportion experience loss of response or intolerance.
AimTo investigate the efficacy and safety of a second anti-TNF agent after primary/secondary failure or intolerance to a first drug.
MethodsInclusion criteria: studies evaluating the efficacy of infliximab (IFX), adalimumab (ADA) and certolizumab-pegol (CZP) as the second anti-TNF in CD or UC. Search strategy: Bibliographical searches (PubMed/Embase). Data synthesis: percentage of response/remission; the meta-analysis was performed using the inverse variance method.
ResultsWe included 46 studies (37 CD, 8 UC, 1 pouchitis). The CD studies comprised 32 switching IFXADA, 4 IFXCZP and 1 ADAIFX. Overall, the second anti-TNF after the failure of IFX in CD induced remission in 43% and response in 63% of patients. The remission rate was higher when the reason to withdraw the first anti-TNF was intolerance (61%) than after secondary (45%) or primary failure (30%); response rates were, respectively, 72%, 62% and 53%. All UC studies switched IFXADA, six of them reporting remission rates ranging from 0% to 50%. Adverse events rate ranged from 0% to 81% in CD, most of them mild (serious adverse event 0–21%, discontinuation rate <20%).
ConclusionsThe efficacy of a second anti-TNF in CD patients largely depends on the cause for switching. The remission rate is higher when the reason to withdraw the first anti-TNF is intolerance (61%), compared with secondary (45%) or primary failure (30%). Further studies of switch ADAIFX are needed to evaluate this strategy. PROSPERO-registry-number: CRD42014012943.
Via Krishan Maggon



 Your new post is loading...
Your new post is loading...









Article first published online: 4 FEB 2015
DOI: 10.1111/apt.13083
© 2015 John Wiley & Sons Ltd
Issue
Alimentary Pharmacology & TherapeuticsVolume 41, Issue 7, pages 613–623, April 2015