Clinical Outcomes of a Novel Therapeutic Vaccine with Tax Peptide-Pulsed DCs for ALL #Immunotherapy #Lukemia http://t.co/OK4Zgk42ki
Summary
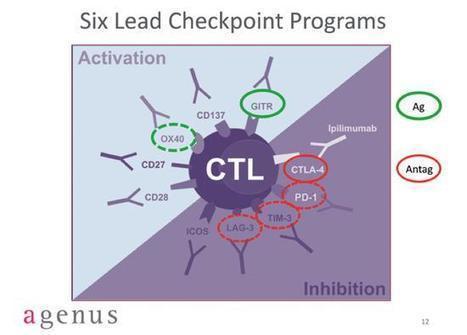
Adult T cell leukaemia/lymphoma (ATL) is a human T cell leukaemia virus type-I (HTLV-I)-infected T cell malignancy with poor prognosis. We herein developed a novel therapeutic vaccine designed to augment an HTLV-I Tax-specific cytotoxic T lymphocyte (CTL) response that has been implicated in anti-ATL effects, and conducted a pilot study to investigate its safety and efficacy. Three previously treated ATL patients, classified as intermediate- to high-risk, were subcutaneously administered with the vaccine, consisting of autologous dendritic cells (DCs) pulsed with Tax peptides corresponding to the CTL epitopes. In all patients, the performance status improved after vaccination without severe adverse events, and Tax-specific CTL responses were observed with peaks at 16–20 weeks. Two patients achieved partial remission in the first 8 weeks, one of whom later achieved complete remission, maintaining their remission status without any additional chemotherapy 24 and 19 months after vaccination, respectively. The third patient, whose tumour cells lacked the ability to express Tax at biopsy, obtained stable disease in the first 8 weeks and later developed slowly progressive disease although additional therapy was not required for 14 months. The clinical outcomes of this pilot study indicate that the Tax peptide-pulsed DC vaccine is a safe and promising immunotherapy for ATL.
Via
Krishan Maggon



 Your new post is loading...
Your new post is loading...

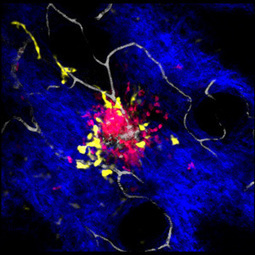









Immune cells interact in surprising ways when responding to skin injuries
Published online 10 June 2015
About A*STAR Research|DermatologyMobilizing the skin’s defense cells
Immune cells interact in surprising ways when responding to skin injuries
Published online 10 June 2015