Your new post is loading...
 Your new post is loading...

|
Scooped by
nrip
|
The face of medical care is rapidly changing thanks to major advancements in the capture, proliferation, and analysis of medical data. Technologies like the electronic health records (EHRs) and personal health records (PHRs) are drastically improving the way data is aggregated and shared.
Now the hope is that big data analytics will help to make sense of seemingly endless streams of medical information.
As many doctors are painfully aware, outcome-oriented care is no longer a buzzword but a reality. The Center for Medicare and Medicaid Services has started to implement a program where payments are based on the ability of providers to meet key National Quality Strategy Domains (e.g. care criteria). Public payers are testing this new methodology, and private payers are expected to soon follow.
These big data analytics applications can also be relevant for the FDA, which may want to see how drugs perform in a non-test environment to ensure the appropriate patient populations are receiving the drug. I also expect pharmaceutical companies to actively scour this data to track drug efficacy post-release or identify markets that could “benefit” from increased penetration.
I am eager to see how the data evolution improves outcomes for doctors and patients.

|
Scooped by
nrip
|
As Ebola continues to ravish Sierra Leone, Guinea and Liberia, people from all around the world are working together to stop the disease. In addition to the life saving work of medical staff, logisticians and community organizers, information and communication technology (ICT) is also playing a vital part in supporting their work. Below are six examples showing how ICT is already making a difference in the current Ebola crisis.
1. Tracing outbreaks with mapping and geolocation
2. Gathering Ebola information with digital data collection forms
3. Connecting the sick with their relatives using local Wi-Fi networks
4. Sharing and receiving Ebola information via SMS text messages
5. Mythbusting for diaspora communities via social media
6. Supporting translations of Ebola information remotely online
read more at http://techchange.org/2014/10/08/ebola-technology-ict/

|
Scooped by
nrip
|
Called Baseline Study, Google's project will gather anonymous genetic and molecular information to create a full picture of what a healthy human is.
The early-stage project is run by Andrew Conrad, a 50-year-old molecular biologist who pioneered cheap, high-volume tests for HIV in blood-plasma donations.
Dr. Conrad joined Google X—thecompany's research arm—in March 2013, and he has built a team of about 70-to-100 experts from fields including physiology, biochemistry, optics, imaging and molecular biology.
Other mass medical and genomics studies exist. But Baseline will amass a much larger and broader set of new data. The hope is that this will help researchers detect killers such as heart disease and cancer far earlier, pushing medicine more toward prevention rather than the treatment of illness.
"With any complex system, the notion has always been there to proactively address problems," Dr. Conrad said. "That's not revolutionary. We are just asking the question: If we really wanted to be proactive, what would we need to know? You need to know what the fixed, well-running thing should look like."
The project won't be restricted to specific diseases, and it will collect hundreds of different samples using a wide variety of new diagnostic tools. Then Google will use its massive computing power to find patterns, or "biomarkers," buried in the information. The hope is that these biomarkers can be used by medical researchers to detect any disease a lot earlier.
The study may, for instance, reveal a biomarker that helps some people break down fatty foods efficiently, helping them live a long time without high cholesterol and heart disease. Others may lack this trait and succumb to early heart attacks. Once Baseline has identified the biomarker, researchers could check if other people lack it and help them modify their behavior or develop a new treatment to help them break down fatty foods better, Dr. Conrad said.
Google has already built one of the world's largest networks of computers and data centers to serve online-search results quickly and run other data-hungry services like the video website YouTube. This computing muscle can now be used to store and crunch medical information and let other researchers access it more easily.

|
Scooped by
nrip
|
What would a medical device suite from Apple look like? More importantly, how would it feel?
When we think about the “why” of how we design products and services, our best work usually makes this planet a better place for all of us to live. Of course, not every product can make that claim, but with the design of medical products it’s almost built in. That said, especially with the constraints imposed by regulations, it’s to claim that our hands are tied and settle for a design compromise instead of looking for the best possible and most poetic answer. One day a hospital room will need to have the equivalently delightful experience of shopping in an Apple store. It’s coming soon.
Hard to picture? Maybe so in the short term, but as we progress, patients no longer will be willing to accept a care system or the products within it that view them as passive recipients of treatment. Patient loyalty can mean the difference between success and failure for healthcare organizations. Gaining patient loyalty comes down to one core factor: the ability of healthcare organizations to consistently deliver positive patient experiences. Organizations that can do so will own the future of healthcare.
The adoption of a patient-centered care model is becoming the main focus of innovative healthcare organizations as accountability for clinical patient satisfaction continues to grow. Positive patient experiences are no longer a nicety for healthcare systems; they are an absolute necessity. We are seeing an industry wide consciousness shift of this understanding with the steady increase of CXOs (customer experience officers) being appointed to C-suite positions across major healthcare organizations.
The future of healthcare will be won by those who put patients first, who think about patients as customers of healthcare. Again, this core value— always put your users first—is long understood in the design community.
A good way to think about it is to design these experiences looking through three lenses: beauty, ingenuity and charisma.
While we may not often think of medical products as beautiful, there is no reason not to; their expression in form and detail have the power to inspire and comfort.Ingenuity solves for problems of use and manufacture, and charisma draws people to a product because of a true understanding of need.
The trick is an uncompromising commitment to all three lenses in every solution and product designed.
With the widespread consciousness shift seen in healthcare organizations toward understanding the importance of focusing on positive patient experience, I believe that this is incredibly exciting time for design leadership to be brought to the table.
Let me pose a final question, hinted at in the first paragraph: Suppose instead of computers, Apple decided to make medical devices. What would a medical device suite from Apple look like?

|
Scooped by
nrip
|
The U.S. military has chosen two universities to lead a program to develop brain implants to restore memory to veterans who have suffered brain injuries, officials said at a news conference Tuesday.
The Restoring Active Memory (RAM) program is a project of the Defense Advanced Research Projects Agency (DARPA), the branch of the U.S. Department of Defense charged with developing next-generation technologies for the military. The initiative aims to develop wireless, fully implantable "neuroprosthetics" for service members suffering from traumatic brain injury or illness, DARPA Program Manager Justin Sanchez said at the news conference.
DARPA has selected two teams of researchers to develop the implants: The University of California, Los Angeles (UCLA) and the University of Pennsylvania, in Philadelphia. Currently, few treatments for TBI-related memory loss exist, but DARPA is trying to change that, Sanchez said. Deep brain stimulation, the use of implanted electrodes to deliver electrical signals to specific parts of the brain, has already demonstrated success in treating Parkinson's disease and other chronic brain conditions. Building on these advances, "we're developing new neuroprosthetics to bridge the gap in an injured brain to restore memory function," Sanchez said.
The UCLA team will focus on studying memory processes in the entorhinal cortex, an area of the brain known as the gateway of memory formation. Researchers will stimulate and record from neurons in patients with epilepsy who already have brain implants as part of their monitoring and treatment. The researchers will also develop computer models of how to stimulate the brain to re-establish memory function.
The University of Pennsylvania team will focus more on modeling how brain circuits work together more broadly, especially those in the brain's frontal cortex, an area involved in the formation of long-term memories. The university is collaborating with Minneapolis-based biomedical device company Medtronic to develop a memory prosthesis system.

|
Scooped by
nrip
|
Coordinated care for chronic diseases in kids is now part of the school nurse's terrain. In some states, nurses are getting access to EHR data.
Although the school nurse is a familiar figure, school-based health care is unfamiliar territory to many medical professionals, operating in a largely separate health care universe from other community-based medical services.
Now, as both schools and health care systems seek to ensure that children coping with chronic conditions such as diabetes and asthma get the comprehensive, coordinated care the students need, the schools and health systems are forming partnerships to better integrate their services. In these projects, some funded by the health law, school health professionals gain access to students' electronic health records and/or specialists and other health system resources. Such initiatives currently exist or are on the drawing board in Delaware, Miami and Beaverton, Ore., among other locations.
School nurses today do a lot more than bandage skinned knees. They administer vaccines and medications, help diabetic students monitor their blood sugar, and prepare teachers to handle a student’s seizure or asthma attack, among many other things.
A 2007 study found that 45 percent of public schools have a full-time nurse on site, while 30 percent have one who works part time. In addition to school nurses, 12.5 percent of school districts have at least one school-based health center that offers both health services and mental health or social services, according to the federal Centers for Disease Control and Prevention’s 2012 Schools Health Policies and Practices Study. School nurses often work closely with school-based health centers, referring students there as needed.
Read more: http://medcitynews.com/2014/06/pilot-programs-give-school-nurses-access-ehrs-can-help-kids-manage-chronic-diseases/#ixzz34HCgGmsp

|
Scooped by
nrip
|
Information that may offer medical insights has been locked away in the filing cabinets of doctors' offices.
Researchers at IBM, Berg Pharma, Memorial Sloan Kettering, UC Berkeley and other institutions are exploring how artificial intelligence and big data can be used to develop better treatments for diseases
But one of the biggest challenges for making full use of these computational tools in medicine is that vast amounts of data have been locked away — or never digitized in the first place.
The results of earlier research efforts or the experiences of individual patients are often trapped in the archives of pharmaceutical companies or the paper filing cabinets of doctors’ offices.
Patient privacy issues, competitive interests and the sheer lack of electronic records have prevented information sharing that could potentially reveal broader patterns in what appeared to any single doctor like an isolated incident.
When you can analyze clinical trials, genomic data and electronic medical records for 100,000 patients, “you see patterns that you don’t notice in a couple,” said Michael Keiser, an instructor at the UC San Francisco School of Medicine.
Given that promise, a number of organizations are beginning to pull together medical data sources.
more at http://recode.net/2014/06/07/medicines-big-problem-with-big-data-information-hoarding/

|
Scooped by
nrip
|
Who knew the loud dot matrix printers of the 1980s, complete with their perforated-edge paper, would give way to sleek 3D printers that can create items ranging from weapons to medical equipment? Let’s take a look at how 3D printing works and how far the technology has come since its recent inception.

|
Scooped by
nrip
|
While smartphones still beat tablets in numbers and frequency of use, physicians generally prefer to do their reading and research on the bigger screen.
Tablets are taking over as a tool of choice for physicians, says a survey by Kantar Media, with just over half of medical professionals using the hand-held computers to read up on the latest journal articles, conduct research on patient care, and email with colleagues.
51% of physicians say they use a tablet during their daily work, while nearly the same amount also use the device for personal tasks.
The survey of more than 3000 physicians found that nearly a third of respondents use tablets to read up on medical publications and 16% watch webcasts or listen to podcasts on professional topics using their tablets which have been making their way into hospitals and offices at a steady pace, through patient-oriented telehealth pilots and monitoring programs intended to engage patients and give providers an edge over chronic diseases
“As physicians continue to shift their work-related tasks to mobile devices, they must overcome technological hurdles challenging them from completing some of their most important tasks, namely interacting with EHRs and recording clinical notes.” An unrelated CDW survey adds that physicians can gain more than an hour of productivity by using tablets to help them multitask, with 84% of physicians saying that the devices make them more efficient and happier doing necessary paperwork.

|
Scooped by
nrip
|

|
Scooped by
nrip
|
Implications of integrating technology:
Under increasing pressure to keep costs down, providers should promote technologies that help manage patients’ health outside of costly care settings.
Shouldering more of their medical costs, health-conscious consumers may be more willing to pay for mobile and other technologies to help manage their health.
Drug and device companies must understand consumer behavior and satisfaction in the social media era.
Reimbursing non-traditional, mobile-enabled therapies may allow insurers to reduce medical costs.

|
Scooped by
nrip
|
What does 2014 hold? According to Eric Schmidt, Google's executive chairman, it means smartphones everywhere - and also the possibility of genetics data being used to develop new cures for cancer. Schmidt says there's a big change - a disruption - coming for business through the arrival of "big data": "The biggest disruptor that we're sure about is the arrival of big data and machine intelligence everywhere - so the ability [for businesses] to find people, to talk specifically to them, to judge them, to rank what they're doing, to decide what to do with your products, changes every business globally."
But he also sees potential in the field of genomics - the parsing of all the data being collected from DNA and gene sequencing. That might not be surprising, given that Google is an investor in 23andme, a gene sequencing company which aims to collect the genomes of a million people so that it can do data-matching analysis on their DNA.
(Unfortunately, that plan has hit a snag: 23andme has been told to cease operating by the US Food and Drug Administration because it has failed to respond to inquiries about its testing methods and publication of results.)
Here's what Schmidt has to say on genomics: "The biggest disruption that we don't really know what's going to happen is probably in the genetics area. The ability to have personal genetics records and the ability to start gathering all of the gene sequencing into places will yield discoveries in cancer treatment and diagnostics over the next year that that are unfathomably important."
It may be worth mentioning that "we'll find cures through genomics" has been the promise held up by scientists every year since the human genome was first sequenced.
So far, it hasn't happened - as much as anything because human gene variation is remarkably big, and there's still a lot that isn't known about the interaction of what appears to be non-functional parts of our DNA (which doesn't seem to code to produce proteins) and the parts that do code for proteins.

|
Scooped by
nrip
|
While much is made of the mHealth app market for consumers, a growing segment is being tailored for clinicians. Doctors are becoming as mobile as their patients, and they need the tools to access medical information as well.
Vendors are already moving in that direction, too. Take Orca Health, for instance, which has developed a platform of iOS 7 apps designed to help clinicians educate patients about certain conditions or medical procedures. The Patient Education for Healthcare Professionals platform, which currently features 10 apps, allows physicians to choose and edit medical content, capture photos and videos and securely send that information to the patient — in essence, enabling the physician to prescribe an app.
"Patient education is a monster, monster problem," said Matt Berry, Orca Health's founder and CEO, in an interview with mHealth News. Berry said the Orca Health apps (the company also has a line of iBooks through a partnership with Harvard Medical School) enable clinicians to personalize patient education, rather than relying on generic handouts. The physician sends the patient an e-mail with a link to a HIPAA-compliant web portal, where the patient can create a secure account and view that information. Subsequent prescriptions — videos, photos, links to information, histories of medical encounters and resolutions — can be added to the patient profile by the physician.
Apps currently available in the Apple App Store are Spine Decide, Knee Decide, Heart Decide, Eye Decide, Shoulder Decide, Foot Decide, Hand Decide, Dental Decide and Ear, Nose and Throat Decide (a Kids dental app is available for the Apple iPad).
Company officials said physicians using the Orca Health platform have improved patient retention rates by as much as 15 percent.
"Physicians are asking for these tools," Berry said. "They want to be able to prescribe that content for their patients."
|

|
Scooped by
nrip
|
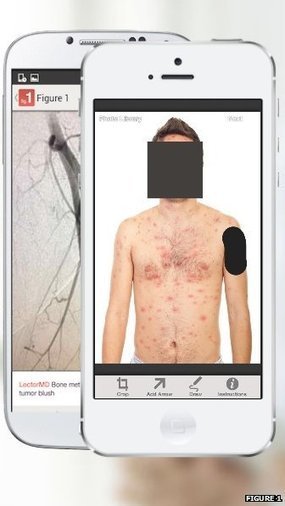
An app which enables healthcare professionals to share photos is to be rolled out across western Europe by the end of the year. The app was designed to enable doctors to share pictures of their patients, both with each other and with medical students.
So far, more than 150,000 doctors have uploaded case photos with the patient's identity obscured.
However, some experts have expressed concern about patient confidentiality.
Patients' faces are automatically obscured by the app but users must manually block identifying marks like tattoos.
Each photo is reviewed by moderators before it is added to the database.
more at: http://www.bbc.com/news/technology-29521986

|
Scooped by
nrip
|
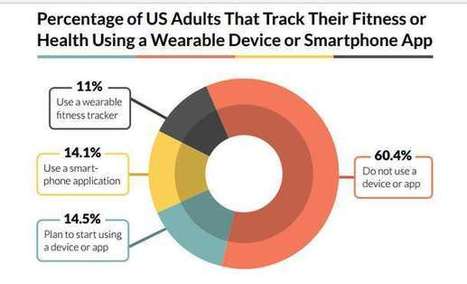
Late last month, TechnologyAdvice released an interesting study looking at whether most people want to use health wearables such as fitness trackers and other tools for health purposes.
Here are the top-line results of this study:
- 75 percent of U.S. adults do not track their weight, diet, or exercise using a health tracking apps or devices
- 43.7 percent had no specific reason for not tracking their fitness
- 27.2 percent won’t use these devices due to lack of interest - 25.1 percent of adults are currently using either a fitness tracker or a smartphone app to monitor their health, weight, or exercise.
This sounds like pretty bad news for those who believe the era of health wearables is here. But, this study also raises another question: Are health wearables evangelists fools?
Fard Johnmar, Founder of Enspektos explains why relevancy is the key to boosting the adoption of health wearables.
Read more at http://hitconsultant.net/2014/10/08/are-health-wearables-evangelists-fools/

|
Scooped by
nrip
|
As tech giants like Apple, Google and Samsung compete over dominance in the healthcare market, with their latest platforms and apps, the question remains will any or all of these innovations truly tap into the greater realm of consumer health? Aside from the buzz now emanating from consumers’ pockets, is there a real signal being sent out here about how to change healthcare, or will these latest consumer-concentric technologies add nothing more than noise?
Welltok's Scott Rotermund explains that what we really need from Google Fit and HealthKit is an integrated approach that not only collects data, but also meshes with the current healthcare ecosystem.
What lessons learned from the disappointments associated with the consumer use of FitBit and others tell us about behavior change? We’ve learned two things:
1. A cool gadget is not enough – The novelty will wear off along with the use of the wearable. In my experience, most people lose interest in their tracking device after a month – they learn their sleep patterns, know average steps, etc. To maintain usage, we’ve tied tracking devices to challenges, participatory incentives and personalized action plans with defined goals.
2. Relying on the consumers to take action – With the startling statistics associated to preventable diseases like obesity and diabetes, it’s safe to say that we cannot expect consumers to take action on their own. These big tech giants are treating health activities as they would consumer electronics – the same rules don’t apply. To move beyond early adopters, they need to tie into programs that provide personalized guidance on how to use the trackers and the resulting data, and align those defined actions with the right incentives to get people moving.
more at http://hitconsultant.net/2014/07/22/is-integration-the-key-to-google-fit-and-healthkits-success/

|
Scooped by
nrip
|
Wearables, devices used to sense data and process it into information, are generating quite the buzz in healthcare these days. But down the line, does that buzz come with a sting?
In Wearable Tech News, Tony Rizzo reports wearable technology spending predictions of $50 billion by 2018. He also reports on a ground-breaking, glucose-sensing contact lens for diabetics that will be a “true solution for a very real medical problem that affects hundreds of millions of people.”
By 2016, wearable wireless medical device sales will reach more than 100 million devices, according to a Cisco blog on the future of mobility in healthcare. The importance of these devices is that healthcare professionals can access critical data via mobile apps before, during and after a patient’s hospitalization, thus boosting the speed and accuracy of patient care, the blog says.
The Age of Wearables has a few caveats, though – note that a doctor “can,” “could,” “may” or “potentially” be able to monitor a patient from a wearable, as the products are still under development. One product cites unpublished research as support, and another uses a modality, thermography, that the National Cancer Institute states has no additional benefit for breast cancer screening.
The new, intense focus on wearables is the engagement of the general public, both the ill and the well, and how they collect and transmit patient information to physicians and EHRs. This presents two challenges:
1. Are physicians prepared for this tidal wave of data and information? 2. What is the true cost of the data surge versus its benefits?
Like all healthcare information technology, wearables have huge potential – married to massive challenges.

|
Scooped by
nrip
|

|
Scooped by
nrip
|
Many recent headlines regarding DNA and genetic science have been complex and hard for the average person to relate to. When the technology saves a young person's life, such as what happened recently at the University of California, San Francisco, the science takes on human qualities, and as a public, we can truly grasp just how important and revolutionary this combination of biology and technology really is.
Dr. James Gern, a professor of pediatrics and medicine at the University of Wisconsin School of Medicine and Public Health in Madison, contacted Joseph DeRisi for help after his patient, a 14-year-old boy, was hospitalized with encephalitis. The prognosis was so severe that the young man had been hospitalized for six weeks and put into a medically induced coma, according to a press release.
None of the tests and procedures run so far had managed to point out the cause of the boy’s illness. Gern contacted DeRisi, chair of biochemistry and biophysics at UCSF, due to his expertise in new genomic techniques. These techniques involved identifying pathogens that were previously unknown, such as that which caused the young man's illness. According to DeRisi, with this new technology, essentially any pathogen can now be detected with a single test. Once the cause was found, correct treatment could be administered.
The case study can be found published online in the New England Journal of Medicine.
Using SURPI, a tool used in “next generation-sequencing,” a team of researchers quickly and efficiently found the cause of the young man’s illness. With the help of the technology, the team compared samples of the boy’s DNA to the GenBank databases maintained by the National Center for Biotechnology Information with awe-inspiring speed, doing in 96 minutes what before took at least a day. Researchers determined that 475 distinct DNA sequences among the three million DNA sequences obtained in the patient’s cereospinal fluid came from a type of bacteria called Leptospira.
The team was even able to pinpoint the exact strain of Leptospira that they boy had been contaminated with: one native to the Caribbean and warmer climates.
Based on these findings, researchers decided to treat the boy using penicillin without having the diagnosis validated with a clinically approved test.
The antibiotics treatment was successful in ridding the boy’s body of infection, and he was discharged and sent home shortly afterward.
Validation by a clinically approved test could have taken upward of five months to confirm, and by this time the boy may not have survived.
more at http://www.medicaldaily.com/dna-sequencing-test-saves-young-teens-life-technology-just-months-away-commercial-approval-286490
The case study can be read at http://www.nejm.org/doi/full/10.1056/NEJMoa1401268#t=article

|
Scooped by
nrip
|
With his Google Glass, Stanford University physician Dr. Homero Rivas pinpoints a target on the skin of an anatomical human model. The surgeon and his assistant then direct their Glass at the target to reveal an augmented reality display on their screens. To their eyes, looking through the Glass, they can see the procedure illustrated step by step with images superimposed over the skin of the model.
Stanford University live-streamed that demonstration to physicians around the world. It wasn’t a particularly complicated procedure, but it was one of the first times that augmented reality has been introduced to Glassware for the benefit of surgeons.
“You don’t need to go in blind anymore,” said Dr. Rivas in an interview with VentureBeat following the demonstration. “Now, we have an educated impression of where a mass is. We can better understand exactly where to make an incision so we can create less trauma.”
more at : http://venturebeat.com/2014/03/13/this-stanford-surgeon-shows-us-the-future-of-medicine-augmented-reality-google-glass-exclusive/

|
Scooped by
nrip
|
Industry observers like myself have often painted the competitive mHealth landscape with a brush that wages computer manufacturer Dell and software behemoth Microsoft versus Apple--the reigning mobile healthcare champion. However, the real battle for the heart, mind and soul of the still-emerging mHealth market places Apple and search engine giant Google squarely in the commercial trenches.
Apple's iPhone and iPad have set the standard for other mobile devices in healthcare. Doctors, in particular, simply love their iPhones and iPads. But, now, the mHealth war between Apple and Google appears to be entering a new battlefield, namely wearable devices.
At the center of Apple's efforts in this area is its long-awaited iWatch, a wristwatch-like computing device with smartphone/tablet and health/activity tracking capabilities. Reportedly, iWatch includes a pedometer for counting steps and sensors for monitoring health-related data such as heart rate.
Apple is growing its team of medical sensor specialists by hiring some of the world's premiere experts in mobile medical technologies. Presumably, this expertise will be heavily leveraged by Apple in their development of the iWatch or some other device.
Simultaneously, Google has been working on its much-heralded Google Glass, high-tech glasses which contain a heads-up display, camera and a microphone, and can ostensibly support mobile health apps directly on the device. Google Glass, developed by the company's secretive Google X lab, has strong potential for healthcare, particularly in the ER where physicians could use the glasses to scroll through lab and radiology results and in the OR providing surgeons with hands-free access to critical clinical information.
In addition, earlier this month, Google unveiled its contact lenses, which use a tiny sensor and wireless transmitter, to monitor and measure glucose levels in tears, potentially replacing the self-administered blood tests from finger pricks that diabetics must endure on a daily basis. Not surprisingly, Google employees recently met with U.S. Food and Drug Administration officials at FDA headquarters who regulate eye devices.
Who will be first to market with these wearable devices--Apple or Google--remains to be seen. What is certain, however, is that the two technology leaders with track records for building strong brands will no doubt dazzle the marketplace with innovative, leading-edge products that put sensor-based devices in the hands of consumers and medical professionals. That kind of competition in mHealth can only serve to benefit us all as this nascent industry moves forward
More at http://www.fiercemobilehealthcare.com/story/apple-vs-google-mhealth-face/2014-01-27

|
Scooped by
nrip
|
With an eye on improving healthcare quality and efficiency, the U.S. Department of Health & Human Services and the U.K.'s National Health Service will share health IT information and tools with one another after signing an agreement Thursday at the Office of the National Coordinator for Health IT's annual meeting in Washington, D.C.
HHS Secretary Kathleen Sebelius and her British counterpart Jeremy Hunt signed the memorandum of understanding, the latter of whom was broadcast via a live feed from the U.K. The agreement focuses on four key areas, according to an HHS announcement, including:
- Sharing quality indicators: The collaboration now is identifying alignments across existing British and American repositories to identify best practices in the design and use of quality indicators. Future work will include mutually leveraging technical experts and data, and working on a standardized approach to quality indicator development.
- Liberating data and putting it to work: HHS and NHS will discuss and find areas of collaboration around open data and safe and secure data transparency of secondary stored data, as well as interoperability standards for improvement of data sharing and clinical care with a focus on patients accessing and sharing data.
- Adopting digital health record systems: Both organizations will work to maximize successful adoption of digital records across the health care spectrum and support the development of a robust health IT workforce.
- Priming the health IT market: Both organizations will work to support the Health IT Marketplace by identifying barriers to innovation, sharing individual certification approaches for patients and clinician-facing applications, and strategies to support small and medium enterprises/start-ups
more at http://www.fiercehealthit.com/story/us-uk-collaborate-health-it-sharing-initiative/2014-01-24

|
Scooped by
nrip
|
The medical industry is quickly adopting mobile technology as a means of connecting lay users with medical professionals. Increasingly, smartphone and tablet users are speaking to their doctors, scheduling medical appointments, and even receiving complex diagnoses via mHealth platforms.
mHealth makes it possible for consumers to receive personalized medical care that may otherwise be unavailable to these individuals.
In this article you can find cases that include some of the most successful mHealth developments to date.

|
Scooped by
nrip
|
This year, when patients throughout the United States begin downloading the world’s first doctor-prescribed smartphone app, mobile health care will finally get what big-time medicine most requires: a way to get insurance companies to pay for it.
The app, called BlueStar, helps people with Type 2 diabetes (the most common kind) by suggesting, in real time, when to test their blood sugar and how to control it by varying medication, food, and exercise. That it requires a physician’s prescription is actually an advantage, because it means insurance companies will reimburse BlueStar’s fee.
“This is a piece of software getting the same treatment as a medical device,” says Sonny Vu, cofounder of Misfit Wearables in San Francisco, a maker of wearable computing devices. “It’s pretty world-changing.”
The U.S. Food and Drug Administration cleared BlueStar for market in 2010, in line with its recent determination to regulate devices that provide a diagnosis or recommend a treatment, not those that simply track activity, like calories consumed or steps taken. The success that WellDoc, the app’s manufacturer, has had with the FDA may inspire other mobile health companies to go the regulatory route. “It gives us hope that you can pull something like this off,” says Vu. The European Commission has also issued guidance on regulations for mobile health apps, but countries such as China and India have not.
The app addresses one of the toughest tasks a physician has: changing patient behavior.
Doctors ask diabetic patients to keep a daily record of glucose readings, food, exercise, and medications. If managed well, these factors keep patients’ blood sugar in a safe range, reducing their risk of complications from the disease. But only 15 to 20 percent of patients actually keep a log, says Philis-Tsimikas.
Diabetes apps that make activity tracking easier are available, but their effectiveness is limited. “No one does it, because you have to wait 90 days before you get feedback [at your next doctor visit],”

|
Scooped by
nrip
|
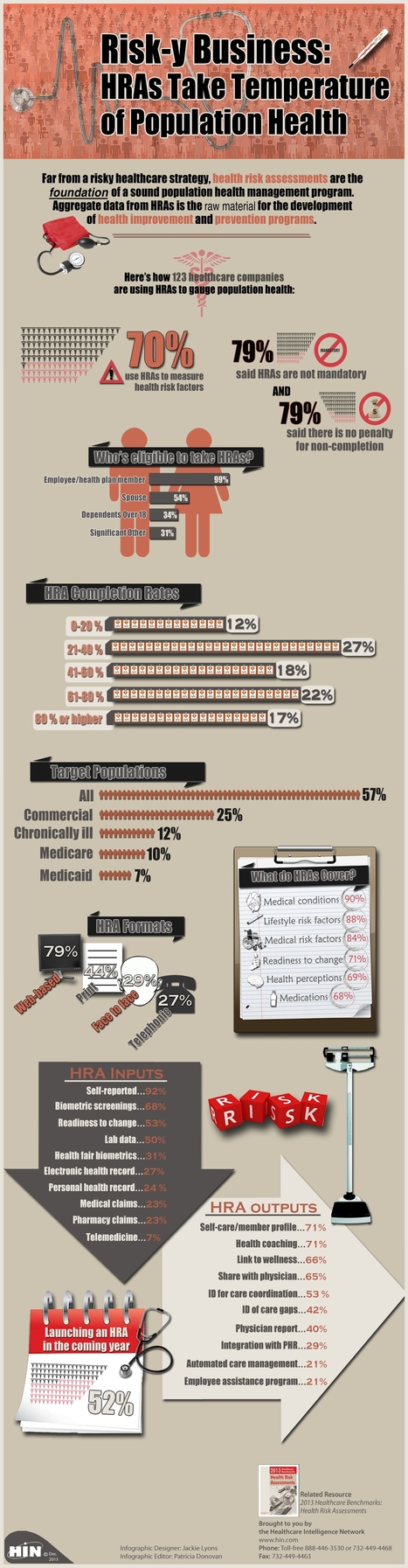
Health Risk Assessments (HRAs) are a powerful component of population health management strategies for healthcare organizations.
|



 Your new post is loading...
Your new post is loading...