The co-founder of German company BioNTech, which successfully delivered the first widely distributed coronavirus vaccine, said that the mRNA technology it used will soon be put to work tackling cancer.
Özlem Türeci, who started BioNTech alongside her husband, said that she had been working to use the body's immune system to combat cancer tumors before the coronavirus pandemic stopped the world.
“We have several different cancer vaccines based on mRNA,”
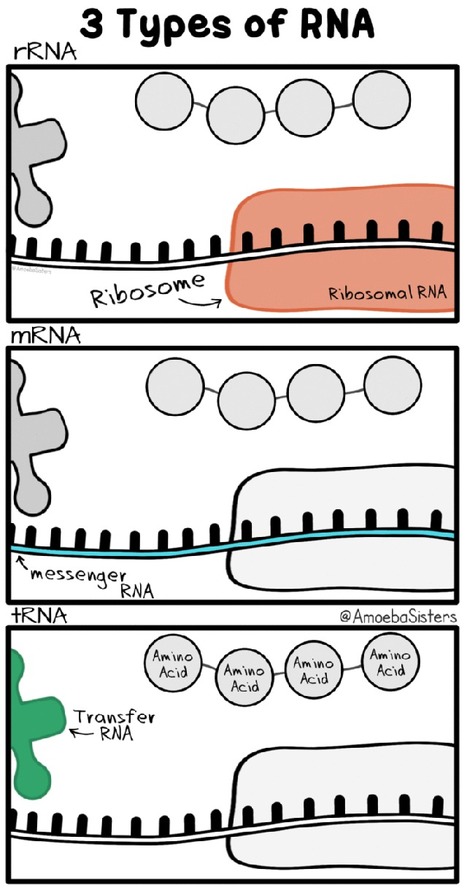
The coronavirus vaccine made by BioNTech(and also Pfizer) uses messenger RNA, or mRNA, to deliver instructions to the body to make proteins that will alert it to attack a certain virus. The same technology can in theory be used for cancer tumors.
What is mRNA ?
Messenger RNA (mRNA) is a single-stranded RNA molecule that is complementary to one of the DNA strands of a gene. The mRNA is an RNA version of the gene that leaves the cell nucleus and moves to the cytoplasm where proteins are made. During protein synthesis, an organelle called a ribosome moves along the mRNA, reads its base sequence, and uses the genetic code to translate each three-base triplet, or codon, into its corresponding amino acid.
The mRNA Approach to Vaccines
mRNA vaccines are a new type of vaccine to protect against infectious diseases. To trigger an immune response, many vaccines put a weakened or inactivated germ into our bodies. Not mRNA vaccines. Instead, they teach our cells how to make a protein—or even just a piece of a protein—that triggers an immune response inside our bodies. That immune response, which produces antibodies, is what protects us from getting infected if the real virus enters our bodies.
mRNA vaccines have been studied before for flu, Zika, rabies, and cytomegalovirus (CMV). As soon as the necessary information about the virus that causes COVID-19 was available, scientists began designing the mRNA instructions for cells to build the unique spike protein into an mRNA vaccine.
Future mRNA vaccine technology may allow for one vaccine to provide protection for multiple diseases, thus decreasing the number of shots needed for protection against common vaccine-preventable diseases.



 Your new post is loading...
Your new post is loading...