Your new post is loading...
 Your new post is loading...
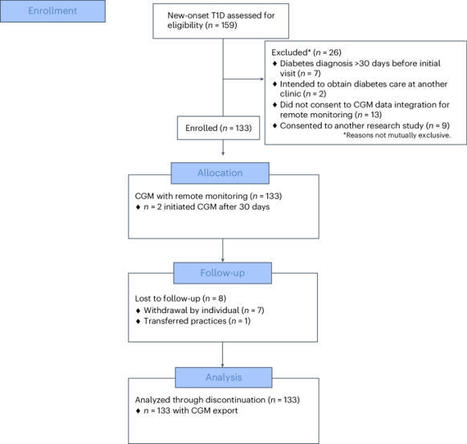
In a prospective study, a team-based approach combining continuous glucose monitoring with a technology-assisted remote patient monitoring program improved glycemia in a diverse cohort of children, adolescents and young adults with newly diagnosed type 1 diabetes.
You shouldn’t be so quick to trust your pregnancy app or others with your health data. The Ethical Tech Project’s Jonathan Joseph explains.
Traditionally, angle measurements have been performed using a goniometer, but the complex motion of shoulder movement has made these measurements intricate. The angle of rotation of the shoulder is particularly difficult to measure from an upright position because of the complicated base and...
Introduction: In today’s fast-paced world, technology continues to revolutionize every aspect of our lives, and healthcare is no exception. With the rise of telemedicine app development company, access to quality healthcare has become more convenient and efficient than ever before.
As technology evolves, we can expect blood health management tools to become even more integral to our approach to blood health.
SAN DIEGO--(BUSINESS WIRE)--Livara Health, a leader in value-based musculoskeletal (MSK) management, today announced that it has raised $15 million in Series B funding. The round was led by A1 Health Ventures, with participation from existing investors Polaris Partners, Providence Ventures, Martin Ventures, and a new strategic investor. A centralized musculoskeletal care plan is essential for enhancing patient outcomes, reducing overall care costs, ensuring equitable access to care, and optimiz
SAN DIEGO--(BUSINESS WIRE)--RevolutionEHR has been awarded Newsweek’s "World’s Best Digital Health Companies 2024." This recognition is presented by Newsweek and Statista Inc.
The PA Clinical Network has tapped health tech company Guidehealth for a multiyear partnership that will drive a greater push into value-based care.
The Apple Watch receives a special approval from the FDA.
Health leaders met at the 2024 Northern California State of Reform Health Policy Conference last month to discuss initiatives aiming to decrease barriers to...
The fee-for-service funding model for US emergency department (ED) clinician groups is increasingly fragile. Traditional fee-for-service payment systems offer no financial incentives to improve quality, address population health, or make value-based clinical decisions. Fee-for-service also does not support maintaining ED capacity to handle peak demand periods. In fee-for-service, clinicians rely heavily on cross-subsidization, where high reimbursement from commercial payors offsets low reimbursement from government payors and the uninsured.
Bethesda, MD – Aledade, the nation’s largest and most successful network of physician-led value-based care, announced today that it has acquired Michigan-based Medical Advantage, which since 2014 has operated as a wholly-owned subsidiary of The Doctors Company, the nation’s largest...
STRENGTHS AND LIMITATIONS OF THIS STUDYThe study included multiple populations with a large number of patients followed over a prolonged period.In the study, multiple clinical indicators and patient-reported outcomes were defined to calculate textbook and resulting outcome.To create a pragmatic framework, a binary outcome measure was defined. On a patient–physician level, this can lead to an overestimation or underestimation of value.IntroductionMedical costs have risen rapidly in recent decades, particularly in developed countries. This increase even exceeded the growth of the gross domestic product (GDP),1 implying that an increasing percentage of GDP has been spent on healthcare. Simultaneously, the gain in life expectancy was marginal and perceived health status remained approximately stable.2 Also changing population demographics, such as ageing2 and an increasing prevalence of multimorbidity3 and healthcare innovations4 contributed to the rise in healthcare costs. Therefore an improved health-related effectiveness evaluation model is required to achieve affordable, high-quality care in the future.Cost-effectiveness analysis (CEA) is the leading evaluation model to aid priority setting in healthcare budgeting5 on the macro, national, level.6 CEA quantifies differences in costs and outcomes for each new medical intervention compared with care as usual. CEA value is usually defined as health-related effectiveness, and operationalised using the Quality Adjusted Life Years (QALYs) metric, while costs include healthcare and societal expenditure.7 CEA is less suitable for priority setting on a meso, institutional, level.6 In CEA, the QALY model includes patients’ life span adjusted for health-related quality of life (HRQoL), which is based on patients’ generic health status.7 In daily practice however, these data are not available, nor easily obtained at the institutional level. Also, data regarding social expenditure are neither present nor manageable on an institutional level. Furthermore, results in CEA can be hard to interpret for clinicians and healthcare managers. This makes it difficult to manage healthcare costs and health outcomes using the CEA framework.In addition, because CEA analyses are based on the patients lifespan, either the remaining lifespan should be estimated, or the analysis can only be performed after the patient is deceased. Combining quality of life and quantity of life in a single metric can then be challenging. Both are different units, one qualitative and the other qualitative, and so are not easily summarised in a single statistic.In 2006, Porter and Teisberg proposed the concept of value-based healthcare (VBHC).8 VBHC describes value as patient-centred health outcomes per unit costs. CEA and VBHC both agree that decision-making in healthcare should be based on a trade-off between health outcomes and healthcare costs using a outcomes/costs ratio.9 However, in CEA, health outcomes are based on generic HRQoL measures whereas in VBHC relevant outcomes have been defined as disease or care path-specific indicators. The latter approach makes VBHC more feasible at the institutional level,6 because care paths are well defined and disease-specific clinical outcome measures are registered in the electronic medical records (EMR).For benchmarking between institutions and measuring outcomes within an institution over time, health outcomes need to be standardised.10 The International Consortium for Health Outcomes Measurement (ICHOM) has therefore published several sets of ‘patient-centred outcome measures’.11–14 Because health outcomes are anyhow disease specific, they are inherently multidimensional and can vary between patients and over time. Several VBHC studies applied or proposed a multicriteria analysis to summarise multiple outcome indicators into one metric.9 15–17 Yet, there is no standardised operational VBHC ‘common metric system’ that aggregates care path-specific outcomes over time. Also for most indicators, there is no clear criterion when such a relevant outcome is either fully achieved, failed or partially achieved. However, if a single VBHC metric produces understandable results, it could support managerial decision-making on an institutional level.Because current frameworks have a high complexity and limited applicability for priority setting on an institutional6 level, we propose a more pragmatic framework that includes costs and outcomes of care paths over time. Such a framework can be used for monitoring care paths, identification of suboptimalities within care paths, and serve as reference for quality improvement programmes and quality improvement reports at the institutional level. Furthermore, we will investigate if the framework can be used for clinical and managerial decision-making and/or quality-of-care assessments in daily clinical practice. Finally, we will analyse which (combination of) health outcomes are associated with increases in healthcare costs.MethodsPatient populationThis proof-of-concept study was a retrospective, real-world cohort study, performed in two use cases, namely: bariatric surgery and breast cancer surgery in Franciscus Gasthuis & Vlietland Hospital, a large medical teaching hospital in Rotterdam, The Netherlands.Bariatric populationFor the bariatric population, all aged ≥18-year older patients diagnosed with morbid obesity (body mass index (BMI) ≥40), treated with gastric bypass or a gastric sleeve resection surgery in 2019 or 2020, were included. Patients who received bariatric surgery in previous years were excluded because it was unclear if/ when a new primary treatment started and the previous treatment stopped.Breast cancer populationFor the breast cancer population, all patients aged ≥18 years older diagnosed with malignant mammary neoplasm and treated with a mastectomy, wide local excision and possibly a breast reconstruction in 2019 or 2020 were included. Patients with stage IV breast cancer at the start of the care path were excluded, because they received palliative care. Also, patients with any breast cancer diagnosis prior to the study were excluded because it was unclear if/ when the new primary treatment started and the previous treatment stopped.Quality cost indicator (QCI) modelIn collaboration with physicians, patient representatives and healthcare managers, we developed a model to support managerial decision-making based on VBHC principles: the QCI model. This model was built on five concepts: textbook outcome (TO) resulting outcome (RO), average total costs (ATC), QCI date and QCI period. Each of these concepts is described below.Textbook outcomeTO18 is accomplished when patients meet all health outcome indicators, as defined for a specific care path. For example, survival should and HRQoL can be a part of TO.Resulting outcomeThe RO rate refers to the number of patients who achieved TO divided by the total number of patients included in the care path. RO varies between 0 and 1.Average total costsTotal costs (TC) are calculated as the sum of the healthcare utilisation costs incurred at the healthcare provider. These costs include the costs of the primary treatment plus any costs following the treatment of symptoms, adverse events or comorbidities of the evaluated patients. The (ATC) equals the TC divided by the total number of patients included in the care path.QCI dateThe TO, RO and ATC parameters are attributed to a QCI date. This is a specific date for each patient, such as the surgery date or date of diagnosis depending on the intervention that will be evaluated.QCI periodThe QCI period is a follow-up period in which the outcomes (TO and RO) and costs (ATC) should be determined. All costs, RO and TO should be considered from the start of the care path (which can occur before the QCI date) until the end of the QCI period. The length of the QCI period can vary according to the goal of the analysis. For example, short-term cost analysis and managerial decisions often require a short QCI period while treatment effectiveness from the patients’ and/ or physicians’ perspective can require a longer QCI period.With these five concepts in mind, QCI values can be calculated as follows: <img class="highwire-embed" alt="Embedded Image" src="https://bmjopen.bmj.com/sites/default/files/highwire/bmjopen/14/5/e080257/embed/mml-math-1.gif">; Outcome indicatorsThe following outcome indicators were defined to calculate RO over time. Data regarding outcome indicators were extracted from the EMR.Bariatric outcomesBecause there is no VBHC standard outcome indicator set for bariatric surgery, outcome indicators were defined by physicians in consultation with patient representatives. This was achieved via flow tables in which patients provided feedback to physicians on what they found high-quality care. Table 1 summarises the outcome indicators for the bariatric population (online supplemental appendix 1 shows the full definitions).Supplemental material [bmjopen-2023-080257supp003.pdf] View inline View popup Table 1 Description of the clinical outcome indicators per populationQCI values for the bariatric population were calculated twice, once including and once excluding the HRQoL indicator. QCI values including HRQoL were only calculated for surgery dates in 2019 due to data availability.Breast cancer outcomes Table 1 also shows the clinical outcome indicators for the breast cancer population, which were based on the ICHOM set11 (again online supplemental appendix 1 shows the full definitions). Because patient–reported outcome measures (PROMs) have only been incorporated in breast cancer care since 2021, we were unable to include the HRQoL indicator.Healthcare utilisation costsFor each patient, TC were calculated as number of activities of care * costs per unit of each activity. For example, the number of MRI scans * costs per MRI scan. Activities of care are specified according to the nationwide Dutch cost price model19 which covers all hospital-based costs (not reimbursement fees). The Dutch cost price model relates cost per units of specific activities to the diagnosis for which the activity is performed. At one point in time, one activity can be used to treat one diagnosis. Therefore, the primary and follow-up diagnosis needed to be included for all populations. All data regarding healthcare utilisation costs were extracted from the financial module of the EMR.Bariatric utilisation costsFor the bariatric population, all healthcare utilisation costs based on a morbid obesity diagnosis in the surgery department and on an adiposity/obesity diagnosis in the internal medicine department were included. Moreover, costs related to readmissions or ED visits within the bariatric population were included when one of the diagnoses in online supplemental appendix 1 was present.Breast cancer utilisation costsFor the breast cancer population, all healthcare utilisation costs based on a malignant mammary neoplasm diagnosis in the surgery department and based on a mammary malignancy diagnosis in the internal medicine department were used.Reference prices from 2019 were used to calculate costs for both populations throughout the entire QCI period. Finally, for calculating additional costs of expensive medication, average billing prices per medication were calculated and multiplied by the number of times these were administered per patient. These costs were then added to the utilisation costs of the patient to complete the full hospital-based costs of care.QCI date and periodFor all populations, the QCI date was selected as the surgery date. The QCI follow-up period was set at 1 year. To include all costs of the treatment for all patients, all costs from 1 year prior to the QCI date (2019 or 2020) until the end of the QCI period (2020 or 2021) were included.Outcome categorisationFor analysing the association between outcome indicators and costs, outcome indicators need to contain a minimum number of patients per outcome status (achieved/failed). Because some indicators were failed only a few times, indicators were categorised. The categories were defined such that they contained at least five patients.Bariatric outcome categoriesThe bariatric population contained the following outcome indicator categories:Admission time after the primary surgery failed.Deficiency failed.ED visit failed.Total weight loss (TWL) failed.Other failed.TO.Each category except Other failed category contained patients who only failed the respective indicator, or passed all indicators (TO). The Other failed category contained patients who either failed the reoperation or readmission indicator or a combination of indicators.Due to differences in outcomes (achieved/failed outcome indicators) between the bariatric population including and excluding HRQoL, the admission time failed category was replaced by the HRQoL failed category, containing patients who only failed the HRQoL indicator, in the population including HRQoL. The Other failed category therefore contained patients who either failed the reoperation, admission time or readmission indicator or a combination of indicators. All other outcome categories remained the same.Breast outcome categoriesFor the breast cancer population, the outcome categories were as follows:Positive Margins failed.Reoperation failed.Other failed.TO.Again all categories except the Other failed category contained patients who only failed the respective indicator, or passed all indicators (TO). Patients in the Other failed category either failed the recurrence or survival indicators or failed multiple indicators.AnalysisStratificationTo increase comparability of QCI values, we adjusted ATC and RO values for patient characteristics using stratification.Bariatric populationThe bariatric population was stratified according to:Gender.Age (</≥40 years).BMI at the start of the treatment (BMI ≥45, or BMI <45).National guidelines indicated that gender, BMI and age impact the costs and outcomes of the treatment.20 Data of the bariatric population also showed that patients over 40 had relatively higher costs than patients under 40.Breast cancer populationThe breast cancer population was stratified for:Age (</≥70 years).Tumour, nodule, metastasis score/ductal carcinoma in situ.Oestrogen receptor status.Human epidermal growth factor receptor 2 status.As per national guidelines, these patient and disease-specific characteristics indicate whether new (expensive) medication will be administered. These characteristics therefore have a large effect on costs of care.21 Case mix adjusted valuesFor each stratum, the expected RO is the average RO of that stratum over all quarters. For each quarter, the expected RO is the weighted average of the stratum-specific expected RO values in that quarter. The observed RO per quarter is the average observed RO of all the patients in that quarter. The average observed RO is the average RO over all the quarters. Therefore, case-mix adjusted RO values are calculated as follows:22 <img alt="Embedded Image" src="https://bmjopen.bmj.com/sites/default/files/highwire/bmjopen/14/5/e080257/embed/mml-math-2.gif"; class="highwire-embed"> The ATC are calculated as follows: <img src="https://bmjopen.bmj.com/sites/default/files/highwire/bmjopen/14/5/e080257/embed/mml-math-3.gif"; alt="Embedded Image" class="highwire-embed"> Missing dataMissing indicator data could indicate an increased likelihood of failing or succeeding the indicator. With this in mind, we could not estimate TO for patients with missing indicator data. Therefore, all patients missing one or more clinical indicators were excluded from all analyses.Supplementary analysisBecause extreme cost outliers may influence QCI values, results were calculated with and without outliers. The cut-off value was selected at P95.Statistical testingThe Kruskal-Wallis test with an alpha value of 0.05 (two sided) was used to determine whether costs were significantly different across outcome categories within populations.Patient and public involvementAs previously mentioned, patients were involved in the development of the outcome measures via flow tables. Patients were not involved in the design or conduct of this registry-based study.ResultsPatient populationBariatric populationIn total, 1172 patients had bariatric surgery between 2019 and 2020. Due to missing clinical data, 316 patients (27%) were excluded. Of the 856 remaining patients, 639 had a BMI lower than 45 at the start of the treatment (table 2). Regarding the bariatric HRQoL population, 270 patients were included of which 203 were diagnosed with a BMI lower than 45 at the start of the treatment.View inline View popup Table 2 Characteristics of the breast cancer population and bariatric population with and without health-related quality of life (HRQoL) (number of patients and percentages of total)Breast cancer populationIn 2019–2020, a total of 671 patients underwent breast cancer surgery. Eight patients had cancer stage IV at the start of the treatment and were excluded. Of the remaining 663 patients, 208 received a mastectomy and 455 received a lumpectomy.Outcome indicators over time Table 3 describes the crude percentages of patients achieving the health outcome indicator and RO per year quarter and in total within the different populations.View inline View popup Table 3 Number (successful/not successful) and percentage of patients achieving the respective health outcome indicator per year, quarter within the different populationsBariatric outcomesIn the bariatric population, all clinical indicators scored above 90% except the deficiency indicator (73%). RO was 0.61 (range 0.51–0.73). For the bariatric population including HRQoL RO was 0.61, range (0.54–0.68). During the same period, RO was 0.59 in the bariatric population. The higher RO values in the bariatric population including HRQoL were mainly based on a higher percentage of patients achieving the TWL and deficiency indicators.Breast cancer outcomesIn the breast cancer population, RO was 0.87, range (0.82–0.93). The surgical margins indicator was least successful, with 92% of patients achieving it. The recurrence indicator was the most successful.QCI values Figure 1 displays case-mix adjusted RO (panels 1A, 1B), ATC (panels 2A, 2B) and QCI values (3A and 3B). Supplementary results comparing RO, ATC and QCI values including and excluding cost outliers are attached in online supplemental file 1 (breast cancer) and 2 (bariatric population).Supplemental material [bmjopen-2023-080257supp001.pdf] <img alt="Figure 1" class="highwire-fragment fragment-image" width="440" height="305" src="https://bmjopen.bmj.com/content/bmjopen/14/5/e080257/F1.medium.gif">Download figure Open in new tab Download powerpoint Figure 1 Case mix adjusted resulting outcome (panels 1A, 1B), average total costs (ATC) (panels 2A, 2B) and quality cost indicator (QCI) values (panels 3A, 3B) over time for both populations. HRQoL, health-related quality of life.Bariatric RO, ATC and QCI valuesFor the bariatric population, RO, ATC and QCI values are presented twice, once including the HRQoL indicator and once for the total bariatric population. As presented in panel 1A, RO values of the bariatric population including HRQoL are higher compared with the total bariatric population. Because ATC of both groups are similar (panel 2A), QCI values of the bariatric population including HRQoL are higher in 2019 Q2 and Q3. Overall, because ATC of the bariatric population has a low variance (SD = €230.42), deviations in QCI values are mostly due to changes in RO values. Excluding outliers had little impact on RO and QCI (online supplemental file 1) values for both groups. ATC values were slightly lower (AVG €8388.26 instead of €8833.55) and less variable (a decrease in IQR of €253.31).Breast cancer RO, ATC and QCI valuesThe results of the breast cancer population show that QCI (panel 3B) values can be impacted by a combination of both ATC (panel 2B) and RO (panel 1B). For the breast cancer population, this is especially true in 2019 Q3 and 2020 Q1. In 2019, Q3 QCI values were highest due to a combination of low costs and high RO values. The opposite is true for 2020 Q3 where a combination of high ATC and low RO values resulted in the lowest QCI value. Excluding outliers impacted the ATC of the breast cancer population predominantly in 2020 (online supplemental file 2), producing higher average QCI values (8.08 instead of 6.70) in that period.Supplemental material [bmjopen-2023-080257supp002.pdf] Costs per population per outcome category Table 4 describes the characteristics of the cost distributions per outcome category for each population.View inline View popup Table 4 Descriptive measures of the total costs per outcome category for each populationCosts of care per outcome category for the bariatric populationFor the bariatric population, patients in the Other failed and Admission time failed categories had high average costs of care, compared with the other categories. The Other failed category also had the highest SD and IQR. For the bariatric population including HRQoL, patients in the Other failed category had the highest average costs of care whereas patients in the TWL failed category had the lowest average costs. TC by outcome category differed significantly for both populations.Costs of care per outcome category for breast cancer populationFor patients with breast cancer, the average costs of the Reoperation failed and Other failed outcome categories were comparable. Patients in the TO category had the lowest average costs of care. Again TC by outcome category differed significantly.DiscussionIn this proof-of-concept study, we developed the QCI model in collaboration with physicians, patient representatives and healthcare managers based on VBHC principles. The QCI model suits the need for monitoring healthcare costs and health outcomes, and thereby the evaluation and quality assessment of healthcare interventions or quality improvements on an institutional level. The framework provides management information on (patient perceived) health outcomes and costs in a single metric and underlying components, for clinicians and healthcare management.The results show that the QCI framework is sensitive to changes in ATC and RO. A strength of the QCI framework is that routinely collected cost and outcome data from EMR and PROMs software are directly available for QCI analysis. Furthermore, the QCI framework has a high level of flexibility because health gains can be based on a large variety of outcomes, preferably those outcomes that cover all main health effects associated with the care path. This flexibility in outcomes also makes the QCI framework applicable for a variety of medical conditions. These findings indicate that the framework is suitable for monitoring the performance of care in terms of outcomes and costs in clinical practice, on an institutional level. Using the framework in a plan-do-act-check cycle, with or without using the underlying indicator and cost data, should help evaluate results and guide continued improvement processes.23 Not all outcome categories equally affected hospital-based costs of care. Failure of outcome indicators with regard to surgery was associated with higher costs. These results can be explained by the direct impact of surgical procedures on hospital-based costs.24 However, no direct impact of the deficiency and TWL indicators on hospital-based costs of care was visible. On the other hand, deficiencies can lead to the development of metabolic bone diseases in the long term25 and obesity is a known risk for coronary heart disease.26 The follow-up period of 1 year might not have been sufficient to investigate the expected increase in cost due to these complications. Investing in adherence to follow-up could result in a higher percentage of patients passing the TWL and deficiency indicators thereby possibly preventing these long-term costs.27 Investing in adherence to follow-up could therefore, in short-term QCI analysis, lead to higher costs and a higher RO. This indicates that short-term QCI values can either improve or decrease depending on whether the gain in RO outweighs the gain in costs. In a long-term QCI analysis, QCI values could improve as additional costs to treat the aforementioned complications could be avoided and RO increases. Different follow-up periods could therefore result in different QCI values.VBHC, CEA and QCI all agree that decision-making in healthcare should be based on a trade-off between health outcomes and healthcare costs using a outcomes/costs ratio.9 However, both VBHC and CEA require complex calculations to summarise outcomes.7 9 15–17 In contrast, in QCI, the RO parameter is an understandable statistic summarising outcomes. Also, in the basis, VBHC and CEA include social as well as direct healthcare costs. QCI, in this analysis, is limited to costs incurred at the healthcare provider. This matches the clinician and managerial perspective. Alternatively, the model could also include out-of-hospital and non-medical costs if this is relevant for hospital management. Finally, both CEA and VBHC recommend analysis of the full cycle of care. In QCI, different follow-up periods are available. Short-run or medium-term analysis can provide valuable information for managerial purposes.The definition of TO as ‘all clinical outcome indicators are met’ gives healthcare providers a pragmatic method to summarise outcomes. However, a limitation of this binary scoring model is that value is only created when all health indicators are met (1), and no value is created ‘when at least one of the indicators is failed’ (0). In the first case, when all indicators are passed, the patient can still perceive the treatment as less then optimal. In the latter case, the patient can view the treatment (at least partially) as a success. The binary scoring rule could therefore result in an overestimation of value, but is more likely to lead to an underestimation of value. An alternative approach could be to define an outcome measure with a continuous score that varies between completely suboptimal outcome (0) and completely optimal outcome (100), with or without assigning different weights to different outcome indicators. Another limitation is missing data. When data from one indicator is missing and the other indicators are passed, QCI values are not defined. Because the QCI framework can give an underestimation as well overestimation (or no estimation in the case of missing data) of value on the microlevel (physician–patient encounter),6 the framework is not applicable at this level. The QCI model can give valuable information on an institutional level as it summarises group outcomes and costs in an understandable fashion.Areas of future research include defining upper and lower margins for outcome, costs and QCI values to guide continued improvement processes. Because as time passes chances of failing or succeeding an indicator can vary,28 future research should investigate RO and TO values over multiple follow-up periods. Comparing hospital performance using the QCI framework could be helpful for optimising QCI values and underlying costs and outcome results.29 Finally, the QCI framework should be applied to more medical conditions, in chronic and acute settings to study the generalisability of the properties of the QCI model.ConclusionsThis proof-of-concept study showed that the QCI framework is effective for monitoring the performance of care paths in terms of costs and health outcomes on an institutional level. An overall impact of health outcome indicators on hospital-based costs of care is found. Also, some indicators, or combination of indicators, impact costs more than others.Data availability statementData are available upon reasonable request. The datasets used in this study are not publicly available under the Dutch privacy legislation. Anonymised datasets can be made available from the corresponding author on reasonable request.Ethics statementsPatient consent for publicationNot applicable.Ethics approvalBecause the study evaluated care as usual a METC review is not obliged under Dutch Legislation. The Institutional Review Board of the Franciscus Gasthuis & Vlietland hospital, named Advies Commissie Wetenschap (ACW) reviewed and waived the study protocol (ref. 2023-002). The study was conducted in accordance with the Declaration of Helsinki exempted this study. The ACW stated that retrospective collection of informed consent was not required for this registry-based study. The effort to do so would be disproportionate due to the number of patients in the study and the fact that the treatment occurred some time ago.AcknowledgmentsWe would like to thank M. Dunkelgrün, MD PhD, and J. Wiebolt, MD PhD, for providing the health outcome indicators for the bariatric population and reviewing the article. We would also like to thank N. Honig with whom we had some inspiring debates on priority setting in healthcare.References↵OECD/European Union. Health at a Glance: Europe 2022: State of Health in the EU Cycle. Paris: OECD Publishing, 2022.↵Organization for Economic Co-operation and Development. Healthcare Quality Indicators from 2011 to 2020. Paris: Organization for Economic Co-operation and Development, 2021. Available: https://stats.oecd.org/Index.aspx?QueryId=51879 ↵ Álvarez-Gálvez J , Ortega-Martín E , Carretero-Bravo J , et al . Social determinants of Multimorbidity patterns: a systematic review. Front Public Health 2023;11:1081518. doi:10.3389/fpubh.2023.1081518 ↵ DiMasi JA , Grabowski HG , Hansen RW . Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ 2016;47:20–33. doi:10.1016/j.jhealeco.2016.01.012 OpenUrlCrossRefPubMed↵ Neumann PJ , Ganiats TG , Russell LB , et al . Siegel: Cost-Effectiveness in Health and Medicine. 1st Edition. Oxford: Scholarship Online, 1996.↵ Al Sayah F , Lahtinen M , Bonsel GJ , et al . A multi-level approach for the use of routinely collected patient-reported outcome measures (Proms) data in Healthcare systems. J Patient Rep Outcomes 2021;5:98. doi:10.1186/s41687-021-00375-1 ↵ Weinstein MC , Torrance G , McGuire A . Qalys: the basics. Value Health 2009;12 Suppl 1:S5–9. doi:10.1111/j.1524-4733.2009.00515.x OpenUrlPubMed↵ Porter ME , Teisberg EO . Redefining Health Care: Creating Value-Based Competition on Results. 1st Edition. Harvard Business Press, 2006.↵ Walraven J , Jacobs MS , Uyl-de Groot CA . Leveraging the similarities between cost-effectiveness analysis and value-based Healthcare. Value in Health 2021;24:1038–44. doi:10.1016/j.jval.2021.01.010 OpenUrl↵ Porter ME , Larsson S , Lee TH . Standardizing patient outcomes measurement. N Engl J Med 2016;374:504–6. doi:10.1056/NEJMp1511701 OpenUrlCrossRefPubMed↵ Burns DJP , Arora J , Okunade O , et al . International Consortium for Health Outcomes Measurement (ICHOM): standardized patient-centered outcomes measurement set for heart failure patients. JACC Heart Fail 2020;8:212–22. doi:10.1016/j.jchf.2019.09.007 OpenUrlAbstract/FREE Full Text↵ Nano J , Carinci F , Okunade O , et al . Diabetes working group of the International Consortium for Health Outcomes Measurement (ICHOM). A standard set of person-centred outcomes for diabetes mellitus: results of an international and unified approach. Diabet Med 2020;37:2009–18.OpenUrlPubMed↵ Seligman WH , Das-Gupta Z , Jobi-Odeneye AO , et al . Development of an international standard set of outcome measures for patients with atrial fibrillation: a report of the International Consortium for Health Outcomes Measurement (ICHOM) atrial fibrillation working group. Eur Heart J 2020;41:1132–40. doi:10.1093/eurheartj/ehz871 OpenUrlPubMed↵ Ong WL , Schouwenburg MG , van Bommel ACM , et al . A standard set of value-based patient-centered outcomes for breast cancer: the International Consortium for Health Outcomes Measurement (ICHOM) initiative. JAMA Oncol 2017;3:677–85. doi:10.1001/jamaoncol.2016.4851 OpenUrl↵ Parra E , Arenas MD , Alonso M , et al . Assessing value-based health care delivery for Haemodialysis. J Eval Clin Pract 2017;23:477–85. doi:10.1111/jep.12483 OpenUrlPubMed↵ Reed SD , Dubois RW , Johnson FR , et al . Novel approaches to value assessment beyond the cost-effectiveness framework. Value Health 2019;22:S18–23. doi:10.1016/j.jval.2019.04.1914 OpenUrl↵ Thokala P , Duenas A . Multiple criteria decision analysis for health technology assessment. Value Health 2012;15:1172–81. doi:10.1016/j.jval.2012.06.015 OpenUrlCrossRefPubMedWeb of Science↵ Roh CK , Lee S , Son SY , et al . Textbook outcome and survival of robotic versus Laparoscopic total gastrectomy for gastric cancer: a propensity score matched cohort study. Sci Rep 2021;11:15394. doi:10.1038/s41598-021-95017-3 ↵ Oostenbrink JB , Rutten FFH . Cost assessment and price setting of inpatient care in the Netherlands. The DBC case-mix system. Health Care Manag Sci 2006;9:287–94. doi:10.1007/s10729-006-9096-y OpenUrlCrossRefPubMed↵Federatie medisch specialisten. Guideline Surgical Treatment Obesity. Utrecht: Federatie medisch specialisten, 2022. Available: https://richtlijnendatabase.nl/richtlijn/chirurgische_behandeling_van_obesitas/startpagina_-_chirurgische_behandeling_van_obesitas.html ↵Federatie medisch specialisten. Guideline Treatment Breast Cancer. Utrecht: Federatie medisch specialisten, 2022. Available: https://richtlijnendatabase.nl/richtlijn/borstkanker/algemeen.html ↵ Sibert NT , Pfaff H , Breidenbach C , et al . Different approaches for case-mix adjustment of patient-reported outcomes to compare healthcare providers-methodological results of a systematic review. Cancers (Basel) 2021;13:3964. doi:10.3390/cancers13163964 ↵ Roll C , Tittel S , Schäfer M , et al . Continuous improvement process: ortho-geriatric co-management of proximal femoral fractures. Arch Orthop Trauma Surg 2019;139:347–54. doi:10.1007/s00402-018-3086-7 OpenUrl↵ Schutzer ME , Arthur DW , Anscher MS . Time-driven activity-based costing: A comparative cost analysis of whole-breast radiotherapy versus balloon-based Brachytherapy in the management of early-stage breast cancer. J Oncol Pract 2016;12:e584–93. doi:10.1200/JOP.2015.008441 OpenUrlAbstract/FREE Full Text↵ Bal BS , Finelli FC , Shope TR , et al . Nutritional deficiencies after Bariatric surgery. Nat Rev Endocrinol 2012;8:544–56. doi:10.1038/nrendo.2012.48 OpenUrlCrossRefPubMed↵ Katta N , Loethen T , Lavie CJ , et al . Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr Probl Cardiol 2021;46:100655. doi:10.1016/j.cpcardiol.2020.100655 OpenUrl↵ Spaniolas K , Kasten KR , Celio A , et al . Postoperative follow-up after bariatric surgery: effect on weight loss. Obes Surg 2016;26:900–3. doi:10.1007/s11695-016-2059-6 OpenUrl↵ Seo DC , Lee CG , Torabi MR , et al . The longitudinal trajectory of post-surgical % total weight loss among middle-aged women who had undergone Bariatric surgery. Prev Med Rep 2017;5:200–4. doi:10.1016/j.pmedr.2016.12.021 OpenUrl↵ Dale KD , Tay EL , Trauer JM , et al . Comparing tuberculosis management under public and private healthcare providers. BMC Infect Dis 2017;17. doi:10.1186/s12879-017-2421-x Coulman KD , Abdelrahman T , Owen-Smith A , et al . Patient-reported outcomes in Bariatric surgery: a systematic review of standards of reporting. Obes Rev 2013;14:707–20. doi:10.1111/obr.12041 OpenUrl
|
CaranX Medical, an innovative medical technologies company, announced the successful completion of the world's first robotic Transcatheter Aortic Valve Implantation (TAVI) procedure.
At My Assessment Help, we recognize the transformative potential of telehealth in empowering nurses to deliver quality care and improve patient outcomes.
Switzerland-based Ikerian AG and its subsidiary, RetinAI U.S. Inc, a developer of software solutions to accelerate healthcare workflows has closed $6.18M (approximately €5.7M).
Background: To overcome knowledge gaps and optimize long-term follow-up (LTFU) care for childhood cancer survivors, the concept of the Survivorship Passport (SurPass) has been invented. Within the European PanCareSurPass project, the semiautomated and interoperable SurPass (version 2.0) will be...
See who joined the panel of 44 health system leaders shaping the definition of a "smart hospital" with CHIME and care.ai, with survey results coming this fall.
Where we’ve been, where we’re going, and how healthcare organizations can protect themselves from privacy risks caused by the Meta pixel and other third-party trackers...
The number of papers presenting machine learning (ML) models that are being submitted to and published in the Journal of Medical Internet Research and other JMIR Publications journals has steadily increased.
Kaiser Permanente is deploying Innovaccer’s healthcare AI platform and population health management tools to support better value-based care — starting with its Washington market and potentially expanding to new markets in the future.
Streamline patient referrals and improve care with a referral management solution. Learn how specialty healthcare practices can benefit from this comprehensive approach.
Looking at some of the chief opportunities and challenges for digital health providers in implementing and scaling technological solutions in the UK...
Navina, the AI-driven primary care platform revolutionizing the interpretation of intricate patient data into actionable guidance during…...
STRENGTHS AND LIMITATIONS OF THIS STUDYThis study originates from a database rich in georeferenced information for each patient.The study uses actual costs of public and intermunicipal transportation for each individual in the dataset.Individual preferences for public or private transportation were not accounted for in this study.Productivity loss estimation did not consider the employment status of participants.The measured calculations are indirect since there is no validated instrument available to measure individuals’ expenditure costs.IntroductionIn the last decade, there have been significant technological advances in healthcare. Telemedicine is a modality of healthcare services delivery, where patients and providers are separated by distance. Telehealth uses information and communication technology for the exchange of information, related to the diagnosis and treatment of diseases and injuries, and to strengthen research and continuing education of health professionals.1 This care model can be especially helpful for outpatient consultations, where barriers related to travel time and cost are constantly inherent for patients.2 3 Positive results regarding patient satisfaction and outcomes of telemedicine care have been reported in the literature.4 This tool has reduced costs in the health system of several countries.5 6 From the patient’s perspective, despite its inherent limitations, telemedicine has been well-received and has generated excellent patient satisfaction.6 7 Telemedicine led savings for patients and their companions, mainly those related to care, including travel time, distance and costs.8–10 However, most of the studies about patient savings related to telemedicine use had been conducted in high-income countries, providing information on the teleconsultation offered for a single state, locality or city.The development and enhancement of telemedicine in Colombia have been under discussion since 2010. However, it was not until 2020, during the COVID-19 pandemic’s public health emergency, that the government began to actively promote its utilisation; this was driven by the enforcement of mandatory lockdown measures and the imperative to ensure continuous medical care. In this circumstance, Fundación Valle del Lili (FVL), a highly complex Colombian teaching hospital, quickly introduced a telemedicine service. Implementing this service encountered significant challenges, the availability of resources and the cultural resistance exhibited by patients towards this modality of attention.11 Our aim was to estimate the hypothetical transportation-related savings in time, distance and costs assumed for the patients due to outpatient care by the FVL telemedicine programme during April–December 2020.MethodsDesign and populationA retrospective study focused on the time and transportation cost savings experienced by the patients as a result of telemedicine interventions. Our study included patient who resided in Colombia and received outpatient teleconsultation through the FVL Telemedicine programme between April and December 2020. We excluded patients residing in countries other than Colombia, as well as those lacking residence information or address details. The study population was categorised based on their place of residence into the following three groups (figure 1):Cali: people who live in the city of Cali, Valle del Cauca.Valle del Cauca excluding Cali: people who live in other cities in Valle del Cauca, different to Cali.Outside of Valle del Cauca: people who live in other departments, different to Valle del Cauca.<img src="https://bmjopen.bmj.com/content/bmjopen/14/5/e084447/F1.medium.gif"; class="highwire-fragment fragment-image" width="386" height="440" alt="Figure 1">Download figure Open in new tab Download powerpoint Figure 1 Study area map with locations of patient residences. Grey-shaded area refers to the region of Valle del Cauca. Black point indicates Fundación Valle del Lili (FVL). Grey points represent areas of teleconsultation in Cali, Valle del Cauca excluding Cali and areas outside of Valle del Cauca.Overview of FVL Telemedicine ProgramIn Colombia, hospitals are categorised into four levels based on their degree of specialisation, subject to evaluation and approval by the national government. Level I hospitals primarily have low-complexity technology and provide care by general practitioners, offering outpatient consultations, hospitalisation, emergency services and essential diagnostic and treatment support. Level II hospitals expand their services to include gynaecology and obstetrics, surgery, internal medicine and paediatrics, incorporating technology of moderate complexity. Level III hospitals feature subspecialised personnel, adult and neonatal intensive care units, and advanced technology. At the highest level of care, level IV hospitals cater to patients in critical condition, offering highly complex subspecialties and the potential for organ transplantation.12 Moreover, it is noteworthy that the three largest cities in Colombia, Bogotá, Medellín and Cali, concentrate the majority of levels III and IV hospitals in the country, providing comprehensive medical services to the surrounding population. Additionally, Colombia boasts only 16 government-accredited teaching hospitals, representing hubs of specialist concentration. Access to specialist care in Colombia’s healthcare system requires authorisation from the patient’s healthcare plan, as patients cannot freely choose their own specialist. The patient healthcare plan assigns the care location based on contractual agreements, with telemedicine services typically included within the health plan. Conversely, smaller cities and towns may house levels 1 and 2 hospitals, offering care of basic to moderate complexity.12 FVL is a private, non-profit, high-complexity hospital located in Santiago de Cali, serving as a referral centre in the southwest region of Colombia. In 2019, the institution provided 511 124 outpatient visits, 75 890 emergency room visits and 26 878 inpatient stays. FVL’s telemedicine service, promoted and strengthened in March 2020 in response to the declaration of a health emergency by COVID-19 by the Ministry of Health, ensures the continuity of ambulatory health services throughout the Colombian territory. This initiative aims to address accessibility challenges, particularly in rural regions, by extending high-level medical services to remote areas. Through a robust referral and counter-referral mechanism, eligible patients requiring outpatient or home-based management can access specialised consultations, facilitating consultation scheduling and ensuring necessary care irrespective of geographic location.FVL’s telemedicine service facilitates outpatient care across 64 medical specialties, employing an interactive modality that establishes remote communication between patients and healthcare professionals through real-time video calls. FVL’s telemedicine service is meticulously organised to ensure seamless access to outpatient care for patients. The process begins with appointment scheduling via telephone, available from Monday to Friday between 07:00 and 17:00, and on Saturdays from 08:00 to 13:00. Patients are carefully guided through administrative procedures, supplemented by instructional emails detailing telemedicine processes. Appointment confirmations are diligently conducted 24 hours in advance by verifying the submission of requisite documents to the designated email address. Teleconsultations and real-time video calls are facilitated through the Microsoft Teams platform. Patient data are recorded in the Enterprise Resource Planning systems of the hospital (SAP-IS-H Software), which host the electronic medical record. Following the consultation, a PDF containing consultation details, medical directives and prescriptions is dispatched to the patient’s email address. Patients who have difficulty due to low technology literacy or cognitive issues are assisted by the appointment agent during the booking process. Additionally, the receptionist provides support during the teleconsultation setup, including guidance on using the application for initiating the call.Outcome measuresThe following outcome measures were taken into consideration:Travel distance savings: the distance in kilometre of round trip that the patient would have travelled for an in-person consultation at the FVL.Travel time savings: the time in hours of round trip that the patient would have wasted for an in-person consultation at the FVL; it represents the patient work time loss due to the travel for an in-person consultation.Measurements of car transportation were performed using Google Maps, taking the main FVL centre as the destination and the patient’s place of residence as the origin. The patient’s home address was defined by the address (for Cali residents) or the registered municipality of residence in the electronic medical record system. The car transport option and the quickest route were selected. The estimated distance and travel time were doubled to encompass the round-trip travel to and from the FVL.Travel cost savings: the expenses related to round trip that the patient would have spent for an in-person consultation at the FVL. For all cases, two modes of transportation were considered: (1) private transportation, for which round-trip fuel expenses were calculated for; and (2) public transportation, for which taxi costs (Cali group) or intermunicipal bus costs (Valle del Cauca and Colombia groups) were calculated based on 2020 fare rates.Fuel cost calculation: we took as a reference the cost per gallon of fuel reported by the Ministry of Mines and Energy for the year 2020 that was $8268 COP (US$2.24); and an average consumption of 40 km travelled per gallon <img src="https://bmjopen.bmj.com/sites/default/files/highwire/bmjopen/14/5/e084447/embed/mml-math-1.gif"; alt="Embedded Image" class="highwire-embed"> Calculation of public transportation cost savings: to calculate the cost public transportation for the population living in Cali, we considered the cab fare reported by the Cali Municipal Hall for the year 2020, which was $84 COP for each 80 m travelled. For residents in other areas of Valle del Cauca and Colombia, we searched on the virtual platforms of the country’s public transportation terminals to determine the fare cost of intermunicipal bus travel from the different localities to the city of Cali.It should be highlighted that for the municipalities where river transportation is necessary, the travel cost and time required for each municipality were consulted, in addition to the cost and time of land transportation. For the municipalities that do not have land access, estimates were made of the airfare costs; these were excluded in the calculations of distance and time savings.Potential loss of productivity: it pertains to the value of work time that the patient would have lost due to the round-trip travel required for in-person consultations.Calculation of the potential loss of productivity: in Colombia, the legal minimum wage in force for the year 2020 was $877 803 COP (US$640.31), the workday corresponds to 48 hours/week, which is adjusted to 8 hours/day. The value of 1 hour worked was $3657 COP (US$2.67). With the above, the value that the patient would have lost due to lost work time secondary to the round trip to attend an in-person consultation was calculated <img class="highwire-embed" alt="Embedded Image" src="https://bmjopen.bmj.com/sites/default/files/highwire/bmjopen/14/5/e084447/embed/mml-math-2.gif">; All costs were calculated with the purchasing power parity exchange rate of 1370.9 COP per USD as per CCEMG–EPPI Centre Cost Converter’ (v.1.7 last update: January 2024) (https://eppi.ioe.ac.uk/costconversion/) designed to facilitate international comparison of costs.13 To estimate distance per patient per trip for patients outside the city of Cali but with land access to the city we used the distance between the centre of the town and the exact address at FVL using available free software. For patients without land access, distance was not computed. For patients in the city of Cali, an exact street address to street address estimation was done with the help of specialised software that takes into account traffic and real routes. This however was costly to do for the 19 630 patients, so we estimated a sample of 753 using the formula for a minimum sample size for estimating a population mean with 95% level of confidence (parameter=1.96), a SD of 7 km and a marging of error (E) of 0.5 km. This calculation did not correct for the finite population correction factor as the population size was large relative to the sample size An extra 8% of patients were added to complete a sample of 814, allowed by the budget allocated to this task, increasing precision and accuracy. This resulted in a total of 1708 teleconsultations in the selected sample, indicating that a single individual may have undergone multiple consultations and follow-up appointments throughout the study period. These consultations represented 3.9% of the 44 182 teleconsultations conducted in this group. As a result, calculations for the total savings in this group were later extrapolated by multiplying the value obtained in the sample by 25.87.Patient and public involvementNone.ResultsA total of 296 170 outpatient care consultations were made from April to December 2020. Among these, 152 consultations were excluded due to patients residing outside of Colombia. Consequently, 296 018 consultations were included, out of which 62 258 (21.03%) were conducted via telemedicine, involving to 27 948 individuals (online supplemental table 1). The median age of the population was 41 years (IQR 21–61), the majority were female (62.95%) and the median of teleconsultations per person was 1 (IQR 1–2) (table 1). Further details regarding the distribution of the number of teleconsultations per patient can be observed in (figure 2). Telemedicine services were primarily provided by psychiatry (8891, 14.28%), endocrinology (6088, 9.78%) and psychology (4603, 7.39%).Supplemental material [bmjopen-2024-084447supp001.pdf] View inline View popup Table 1 Sociodemographic characteristics of the patients attended via telemedicine, between April and December 2020<img width="440" src="https://bmjopen.bmj.com/content/bmjopen/14/5/e084447/F2.medium.gif"; class="highwire-fragment fragment-image" alt="Figure 2" height="244">Download figure Open in new tab Download powerpoint Figure 2 Distribution of the frequency of teleconsultations per person.Total travel savings in terms of distance amounted to 4 514 903 km, and in terms of time, it reached 132 886 hours. The estimated travel cost savings were US$1 035 336 for private transportation (combining fuel cost savings and potential productivity gains) and US$1 442 335 for public transportation (cost of public transportation saved and potential productivity gains). The largest savings were in the rest of Colombia group, which are those people living in departments of Colombia other than Valle del Cauca. Table 2 shows the total and average savings per teleconsultation for each group. Furthermore, it was estimated that individuals residing in areas where access required air travel, could achieve savings of up to US$134 USD (SD 131.17) per teleconsultation.View inline View popup Table 2 Distance, time, fuel and public transportation savings observed by telemedicine consultation, between April and December 2020The mean number of teleconsultations per patient was 2.10 (SD2.54) in Cali, 2.23 (SD 3.14) in Valle del Cauca excluding Cali and 2.05 (SD 2.28) for the Outside of Valle del Cauca group. The estimated mean cost savings for private transportation round trip per patient was US$10.13 in Cali, US$66.79 in Valle del Cauca excluding Cali and US$205.65 in outside of Valle del Cauca; and mean cost savings for public transportation expenses per patient was US$28.98 in Cali, US$50.22 in Valle del Cauca excluding Cali and US$213.25 in outside of Valle del Cauca. In addition, the transportation cost savings for individuals residing in areas with exclusive air access amounted to US$658.52, with a SD of US$392.49 (table 3).View inline View popup Table 3 Distance, time, fuel and public transportation per patient (all visits), between April and December 2020DiscussionIn low-income and middle-income countries, the population at the base of the socioeconomic pyramid bears a disproportionately high burden of disease, often facing limited access to health services due to lower purchasing power and residence in underserved areas. In such contexts, there is an urgent need to identify innovative short, medium and long terms to achieve effective universal health coverage, giving special strength to programmes that allow access in the most remote and vulnerable areas.14 15 Strengthening telehealth systems has the potential to improve health and socioeconomic status of different population groups. Extending healthcare services to these remote areas through telemedicine helps bridge this gap and facilitates substantial reductions in both time and distance.16–19 In Colombia, 7.2% of the population lives in rural areas,20 with significant challenges and obstacles when accessing healthcare services, particularly specialised medical care.15 In 2020, as the COVID-19 pandemic spread worldwide, world poverty increased, and poverty induced by COVID-19.21 Colombia was significantly affected by this issue, with a noticeable deterioration in its economic growth indicators. In 2020, the pandemic led to a 6.8% decline in Colombia’s economy (gross domestic product), contributing to an increase in the national unemployment rate by at least 8 percentage points, resulting in an average rate of 15.9, a 5.4 percentage points rise from the previous year.22 23 Furthermore, the proportion of informal employment increased from 45% to 49%.24 Thus, savings achieved by the programme were very timely in the midst of the worst economic year in Colombian history. The introduction of telemedicine led to average potential loss of productivity savings of US$5.51 and US$34.25 per patient for the population of Cali and Valle del Cauca, equivalent to 26% and 75% of a full day’s salary, respectively. For the population of Colombia, US$56.63 was saved per patient, representing 9% of the minimum monthly salary.Transportation cost is a determining factor in access to healthcare, especially for those living in rural areas not having a tertiary or complex centre nearby that can provide services by medical specialties.25 However, the need for more training in the use of technologies and the difficulties in acquiring technology that allows remote connection limit the implementation of telemedicine in these areas.6 26 In our study, the telemedicine programme succeeded in extending its reach to remote locations facing geographical challenges. These areas are accessible solely by air or sea. Examples include municipalities such as Guapi, Timbiquí, Leticia and San Andres Island. Enhancing telecommunication networks in these regions could yield substantial savings in time, distance and travel expenses for their residents.27 For people living in those municipalities, savings in transportation costs estimated per patient exceeded the 2020 monthly minimum wage.Significant savings related to transportation and fuel expenses have been reported. These costs vary widely; studies have reported savings ranging from US$4.66 to US$150 per teleconsultation.4 28 Other studies have reported saved costs that encompass fuel expenses, insurance and maintenance, resulting in higher per-person savings. Few studies have addressed costs related to public transportation; given the importance of public transportation in Colombia, especially between and within cities, this variable was key for a more realistic measurement.29 When comparing the average public transportation expenses saved for the Cali, Valle del Cauca and rest of Colombia locations to the legal monthly minimum salary in Colombia for year 2020, it represents 3.67%, 5.08% and 24.19%, respectively, for the average patient.Limitations of the current study include the retrospective approach to data collection, which limited the depth of analysis possible. Prospective data collection would have allowed for a more comprehensive examination, including factors such as work absenteeism, wait times, appointment duration and associated costs. In addition, the absence of provider expenditures in the cost-effectiveness (CE) assessment of telemedicine represents a significant gap. On the other hand, the Colombian healthcare system fully covers diagnostic and treatment services, which may mitigate the cost impact on patients or hospitals. However, the study did not measure these consequences and costs, which is a limitation. Additionally, the potential loss of productivity particularly affects the adult population aged between 21 and 61 years. The retirement age in Colombia for women is 57 years and for men is 62 years. Within the scope of the study, this constitutes a limitation as it was not measured.The study also overlooked critical factors like internet usage and telecommunications connectivity, impacting the assessment of cost savings achieved through telemedicine adoption. Failure to consider participants’ transportation mode and employment status hindered insights into socioeconomic dynamics influencing telemedicine utilisation. Methodologically, the indirect calculation of expenditures introduced ambiguity, compounded by the absence of a validated instrument for precise measurement. Our objective in this paper was measuring savings using TM in comparison to a regular visit by the patient to our location; we did not seek a full economic evaluation which will include a CE study. The CE literature has shown that from a health systems perspective telemedicine programmes remain cost effective, but from a societal perspective there is a gap, and we leave a full economic evaluation for further research.Future implicationsThe results encourage developing public policies and strengthening strategies incorporating digital health and telemedicine in Latin America’s countries. Our experience shows results aimed at reducing indirect patient costs related to providing health services and facilitating care by multiple specialties through teleconsultation.ConclusionTelemedicine brings to patients a significant travel savings, both in terms of time, distance, cost and potential loss of productivity; particularly in regions facing geographical and socioeconomic challenges. These findings emphasise the potential of telemedicine to bridge healthcare accessibility gaps in middle-income countries and the need to further develop and expand telemedicine services in such areas.Data availability statementData are available upon reasonable request. The data that support the findings of this study are available from the corresponding author [MFE], upon reasonable request.Ethics statementsPatient consent for publicationNot applicable.Ethics approvalThis study was conducted according to the Declaration of Helsinki guidelines; and was classified as a risk-free study according to resolution No. 008430 of 1993, article 11, numeral A of the Ministry of Health and Social Protection of Colombia. The institutional ethics committee reviewed and approved the protocol (Protocol No. 1742; IRB/EC No. 090–2021, Act No. 06-2021). This study did not require intervention or intentional modification of the biological, physiological, psychological or social variables of the participants. Therefore, no informed consent was necessary.AcknowledgmentsWe thank to the Fundación Valle del Lili, especially the department of cost and budget for providing and supporting this current research.References↵WHO-ITU global standard for accessibility of telehealth services. World health organization, international telecommunication union en Geneva. 2022. Available: https://www.who.int/publications-detail-redirect/9789240050464 ↵ Bynum AB , Irwin CA , Cranford CO , et al . The impact of telemedicine on patients’ cost savings: some preliminary findings. Telemed J E Health 2003;9:361–7. doi:10.1089/153056203772744680 OpenUrlCrossRefPubMedWeb of Science↵ Spaulding R , Belz N , DeLurgio S , et al . Cost savings of telemedicine utilization for child psychiatry in a rural kansas community. Telemed J E Health 2010;16:867–71. doi:10.1089/tmj.2010.0054 OpenUrlCrossRefPubMed↵ Dullet NW , Geraghty EM , Kaufman T , et al . Impact of a university-based outpatient telemedicine program on time savings travel costs, and environmental pollutants. Value Health 2017;20:542–6. doi:10.1016/j.jval.2017.01.014 OpenUrlPubMed↵ Snoswell CL , Taylor ML , Comans TA , et al . Determining if telehealth can reduce health system costs: scoping review. J Med Internet Res 2020;22:e17298. doi:10.2196/17298 ↵ Almathami HKY , Win KT , Vlahu-Gjorgievska E . Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients. J Med Internet Res 2020;22:e16407. doi:10.2196/16407 ↵ Eze ND , Mateus C , Cravo Oliveira Hashiguchi T . Telemedicine in the OECD: an umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One 2020;15:e0237585. doi:10.1371/journal.pone.0237585 ↵ Hussaini SMQ , Gupta A , Dusetzina SB . Financial toxicity of cancer treatment. JAMA Oncol 2022;8:788. doi:10.1001/jamaoncol.2021.7987 OpenUrl↵ Tuckson RV , Dzau VJ , Lurie N . Creating healthy communities after disasters. N Engl J Med 2017;377:1806–8. doi:10.1056/NEJMp1711834 OpenUrl↵ Patel KB , Turner K , Alishahi Tabriz A , et al . Estimated indirect cost savings of using telehealth among nonelderly patients with cancer. JAMA Netw Open 2023;6:e2250211. doi:10.1001/jamanetworkopen.2022.50211 ↵ Figueroa LM . Telehealth in Colombia, challenges associated with COVID-19. Biomedica 2020;40:77–9. doi:10.7705/biomedica.5594 OpenUrl↵ Escobar MF , Echavarría MP , Carvajal JA , et al . Hospital padrino: a collaborative strategy model to tackle maternal mortality: a mixed methods study in a middle-income region. Lancet Reg Health Am 2024;31:100705. doi:10.1016/j.lana.2024.100705 ↵ Shemilt I , James T , Marcello M . A web-based tool for adjusting costs to a specific target currency and price year. Evid & Pol 2010;6:51–9. doi:10.1332/174426410X482999 OpenUrl↵Departamento Administrativo Nacional de Estadística (DANE). Situación de las mujeres rurales desde las estadísticas oficiales, 2022. Available: https://www.dane.gov.co/files/investigaciones/notas-estadisticas/oct-2022-nota-estadistica-mujer-rural-presentacion.pdf ↵ Brundisini F , Giacomini M , DeJean D , et al . Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser 2013;13:1–33.OpenUrlPubMed↵ Speyer R , Denman D , Wilkes-Gillan S , et al . Effects of telehealth by allied health professionals and nurses in rural and remote areas: a systematic review and meta-analysis. J Rehabil Med 2018;50:225–35. doi:10.2340/16501977-2297 OpenUrlCrossRefPubMed↵ Carroll M , Cullen T , Ferguson S , et al . Innovation in Indian healthcare: using health information technology to achieve health equity for American Indian and Alaska native populations. Perspect Health INF Manag 2011;8:1d.↵ Lagomarsino G , Garabrant A , Adyas A , et al . Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet 2012;380:933–43. doi:10.1016/S0140-6736(12)61147-7 OpenUrlCrossRefPubMedWeb of Science↵ Balabanova D , Mills A , Conteh L , et al . Good health at low cost 25 years on: lessons for the future of health systems strengthening. Lancet 2013;381:2118–33. doi:10.1016/S0140-6736(12)62000-5 OpenUrlCrossRefPubMedWeb of Science↵Dirección de Epidemiología y Demografía. Análisis de Situación de Salud (ASIS) Colombia, 2020. Ministerio de Salud y Protección Social, 2020.↵ Moyer JD , Verhagen W , Mapes B , et al . How many people is the COVID-19 pandemic pushing into poverty? A long-term forecast to 2050 with alternative scenarios. PLoS One 2022;17:e0270846. doi:10.1371/journal.pone.0270846 ↵Departamento Administrativo Nacional de Estadística (DANE). Comunicado de Prensa Producto Interno Bruto (PIB) IV Trimestre y Año 2020. Bogotá D.C, 2021.↵Departamento Administrativo Nacional de Estadística (DANE). Boletín Técnico Gran Encuesta Integrada de Hogares (GEIH) Diciembre 2020. Bogotá D.C, 2021. Available: https://www.dane.gov.co/files/investigaciones/boletines/ech/ech/bol_empleo_dic_20.pdf ↵Departamento Administrativo Nacional de Estadísticas - DANE. Empleo Informal y Seguridad Social, 2023. Available: https://www.dane.gov.co/index.php/estadisticas-por-tema/salud/informalidad-y-seguridad-social/empleo-informal-y-seguridad-social-historicos ↵ Wolfe MK , McDonald NC , Holmes GM . Transportation barriers to health care in the United States: findings from the national health interview survey, 1997-2017. Am J Public Health 2020;110:815–22. doi:10.2105/AJPH.2020.305579 OpenUrlCrossRefPubMed↵ Zachrison KS , Boggs KM , Hayden EM , et al . Understanding barriers to telemedicine implementation in rural emergency departments. Ann Emerg Med 2020;75:392–9. doi:10.1016/j.annemergmed.2019.06.026 OpenUrlPubMed↵ Atmojo JT , Sudaryanto WT , Widiyanto A , et al . Telemedicine, cost effectiveness, and patients satisfaction: a systematic review. J Health Policy Manage 2020;5:103–7. doi:10.26911/thejhpm.2020.05.02.02 OpenUrl↵ Paquette S , Lin JC . Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg 2019;59:167–72. doi:10.1016/j.avsg.2019.01.021 OpenUrl↵Ministerio de Transporte. Transporte en Cifras 2021. Anuario Nacional de Transporte 2022;55–8.
|

 Your new post is loading...
Your new post is loading...
 Your new post is loading...
Your new post is loading...